Translate this page into:
Correlation of Aortic Root Movement with Left Ventricular Function
*Corresponding author: Imran Shaik, Department of Cardiology, Nizam’s Institute of Medical Sciences, Hyderabad, Telangana, India. imran.omc93@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shaik I. Correlation of aortic root movement with left ventricular function. Indian J Cardiovasc Dis Women 2023;8:30-6.
Abstract
Objectives:
The motion of structures of the heart is the basis for cardiac function. Factors such as low image quality and low signal-to-noise ratio create hindrances in the adequate valuation of left ventricular (LV) systolic and diastolic function. Even in cases with poor image quality, the aorta being a large structure is well visualized. One of the unorthodox approaches to the assessment of heart function is the study of aortic root movement.
Materials and Methods:
We studied patients who came to the Nizam Institute of Medical Sciences. The ethics committee of the institute approved our study. We studied 85 patients who came to the emergency or outpatient department with or without various cardiovascular problems. We have included patients who presented with myocardial infarction, arrhythmia, and heart failure, cerebrovascular accident. We measured the constants pertaining to the aortic root motion and LV function with the standard parameters of echocardiography. Then, we aimed to check for a correlation between aortic root movement parameters and the LV function of the heart. Patients filling the inclusion criteria were enrolled in the study after taking informed consent. The data from the participants were collected prospectively. We recorded the echocardiography according to the standard guidelines. We used the Vivid E9 scanner (GE Vingmed Ultrasound AS) with the M5S-D (1.7–3.3 MHz) cardiac probe to acquire the data. We studied the echocardiographic 2D images and Doppler parameters. We used the parasternal long axis view as well as the parasternal short axis view to measure the aortic movement.
Results:
We included a total number of 85 patients as per the defined criteria among which 22 (25.88%) are females and 63 (74.11%) are males. The average age of enrolled participants was 56.30 years (±14.95 years). The mean age of the patients was 56.3 ± 14.9. About 75% of the subjects had LV dysfunction and the remaining had normal lv function. Sixty-five patients had LV dysfunction either due to ischemic or non-ischemic cardiomyopathy. We, then, checked for the relationship between the aortic root constants and the LV function parameters. We found the mean value of aortic root diastolic distance (ARDD) as 2.59 ± 0.43 cm and. The aortic root maximal diastolic velocity (ARDV) was 10.8 ± 2.4 cm/s. The aortic root systolic distance (ARSD) was 2.71 ± 0.65 cm. The aortic root maximal systolic velocity (ARSV) was 7.92 ± 2.26 cm/s. Mean aortic root excursion was 4.3 mm. Aortic root systolic excursion (ARSE) showed a parallel relation with LV function (r up to 0.7). We found ARSD and ARSV correlating weakly with systolic Doppler parameters, such as ejection fraction (EF), maximum annular plane systolic excursion (MAPSE), and s' medial. ARSE was an exception that it showed a good correlation with s’medial r = 0.746 (P < 0.001), EF r = 0.807 (P < 0.001), and MAPSE r = 0.68 (P < 0.001). The ARDD and ARDV related poorly with LV diastolic parameters such as e' mean, e' medial, e' lateral, E/A, and E/e’. E velocity, E/A, and E/e’mean showed a negative correlation with ARDV. ARDD (r up to 0.02) and ARSD (all r values < 0.40) did not correlate with the LV Doppler measurements. ARDV correlated (r up to 0.51) with some LV diastolic Doppler parameters and ARSV correlated in moderate range only with mitral annulus plane systolic excursion (r = 0.31). In fact, we found that ARDD is related better than ARDV with Doppler measurements.
Conclusion:
In our study, we included subjects with cardiovascular diseases and we conclude that systolic aortic root motion correlates significantly with systolic LV function, the most essential being the aortic root systolic velocity. We found that the diastolic root motion parameters correlated weakly with the diastolic LV function. In patients with poor echo windows, aortic root motion may be helpful in predicting LV function in patients with or without LV dysfunction.
Keywords
Aortic root movement
LV function
echo window
ABSTRACT IMAGE

INTRODUCTION
Measurement of the left ventricular (LV) function is an integral part of echocardiographic studies. Simpson’s method for assessment of LV function is considered a reliable way of measuring LV function. However, the accuracy depends on the image quality, echo window, and skill of the performer. Most of the measures of LV function depend on the volumes and contraction.[1] The aortic root is exposed to the same shearing force as the LV. Hence, the amplitude of aortic root movement is supposed to be directly proportional to the LV systolic function.[2] It is also well-visualized as being a highly echogenic structure in B-mode echocardiography.
M-mode was the first modality used to assess the aortic root motion. Using the m-mode in the parasternal short-axis view can help determine the aortic root systolic excursion (ARSE).[3] Apart from ARSE, we are studying novel parameters of aortic root systolic and diastolic distances, and aortic root systolic and diastolic velocities. This is measured in the parasternal long-axis view with tissue Doppler imaging. Our aim is to study these parameters of aortic root movement and check for the relation with regular LV function measures. In cases where it is difficult to use the standard measures of LV function, especially when there is a poor echo window one may use the parameters of aortic root motion to estimate LV function [Figures 1 and 2].[4]

- Aortic root maximal systolic velocity measured using tissue Doppler imaging.

- M-mode echo on aortic root to calculate aortic root systolic excursion.
Objectives
To study the aortic root systolic, diastolic distances and velocities.
To determine the relation between the aortic root motion parameters and LV function by standard echocardiographic measures.
MATERIALS AND METHODS
We studied patients who came to the Nizam Institute of Medical Sciences. The ethics committee of the institute approved our study. We studied 85 patients who came to the emergency or outpatient department with or without various cardiovascular problems. We have included patients who presented with myocardial infarction, arrhythmia, and heart failure, cerebrovascular accident. We measured the constants pertaining to the aortic root motion and LV function with the standard parameters of echocardiography. Then, we aimed to check for a correlation between aortic root movement parameters and the LV function of the heart. Patients filling the inclusion criteria were enrolled in the study after taking informed consent. The data from the participants were collected prospectively. We recorded the echocardiography according to the standard guidelines. We used the Vivid E9 scanner, (GE Vingmed Ultrasound AS) with the M5S-D (1.7–3.3 MHz) cardiac probe to acquire the data. We studied the echocardiographic 2D images and Doppler parameters. We used the parasternal long axis view as well as the parasternal short axis view to measure the aortic movement. We intended to determine the aortic root systolic distance (ARSD), aortic root diastolic distance (ARDD), aortic root systolic velocity (ARSV), and aortic root diastolic velocity (ARDV).
Statistical analysis
We cross-correlated the aortic root function parameters with each of the LV Doppler parameters. We calculated P-value and Spearman’s rank correlation coefficient r. Strength of relationship was defined as: |r| ≥ 0.80, very strong; |r| = 0.60–0.79, strong; |r| = 0.40–0.59, moderate; |r| = 0.20–0.39, weak, and |r| = 0.00–0.19, negligible.
RESULTS
We included a total number of 85 patients as per the defined criteria, of which 22 (25.88%) are female and 63 (74.11%) are male. The distribution according to gender is shown in [Figure 3].

- Gender distribution of the participants.
The average age of enrolled participants was 56.30 years (±14.95 years). The mean age of the patients was 56.3 ± 14.9. About 75% of the subjects had LV dysfunction and the remaining had normal lv function. Sixty-five patients had LV dysfunction either due to ischemic or nonischemic cardiomyopathy. The basic information about the participants is mentioned in [Table 1].
| Mean | Median | SD | |
|---|---|---|---|
| Age (yr) | 56.30588235 | 57 | 14.95789609 |
| Body weight (kg) | 58.30588 | 56 | 8.068197 |
| Body height (cm) | 154.0824 | 155 | 3.697527 |
| Body surface area (m2) | 1.576711972 | 1.556438242 | 0.117734386 |
| Systolic blood pressure | 104.3529412 | 100 | 20.37079251 |
| Diastolic blood pressure | 67.05882353 | 70 | 11.00038196 |
| Pulse pressure | 37.41176471 | 32 | 12.55397311 |
| Heart rate | 89.8 | 88 | 16.89589976 |
The distributions of the various aortic root movement parameters are shown in [Figures 4 and 5].

- Graphical representation of the distribution of aortic root systolic excursion in study participants.

- The graphical representation of distributions of aortic root movement parameters.
The statistical analysis of the various parameters that were studied is shown in [Table 2].
| Mean | Median | SD | |
|---|---|---|---|
| Aortic root motion parameters | |||
| ARSD | 2.710941176 | 2.7 | 0.658082756 |
| ARDD | 2.597411765 | 2.63 | 0.434621217 |
| ARSV | 7.928117647 | 7.3 | 2.26 |
| ARDV | 8.012352941 | 7.57 | 2.46 |
| ARSE | 5.074117647 | 4.7 | 1.562061591 |
| Regular parameters of LV function | |||
| EF | 37.57647059 | 38 | 14.58095339 |
| S’med | 7.325882353 | 6.5 | 2.990268062 |
| E | 111 | 68 | 18.38477631 |
| A | 71.5 | 56.6 | 0.707106781 |
| E/A | 1.553794992 | 1.294117647 | 0.272496158 |
| e’ mean | 11.325 | 7.22 | 1.661700936 |
| E/e’ | 10.02837438 | 8.292134831 | 3.094828734 |
| MAPSE | 8.06 | 8.00 | 2.93 |
ARSD: Aortic root systolic distance, ARDD: Aortic root diastolic distance, ARSE: Aortic root systolic excursion, LV: Left ventricular, EF: Ejection fraction, and MAPSE: Maximum annular plane systolic excursion
We, then, checked for the relationship between the aortic root constants and the LV function parameters. We used Spearman’s rank correlation coefficient for analysis in our study. Table 3 shows how much they correlate with the regular parameters.
| R (P value) | |||||
|---|---|---|---|---|---|
| ARSD | ARDD | ARSV | ARDV | ARSE | |
| EF | 0.036782496 (0.513) |
0.072458791 (0.194) |
0.317066434 (0.0001) |
0.306721426 (0.001) |
0.807763777 (0.0001) |
| S’ med | −0.010067041 (0.516) |
0.035813144 (0.270) |
0.333895317 (0.001) |
0.279921075 (0.001) |
0.746317231 (0.0001) |
| E | 0.023062839 (0.67) |
0.022297045 (0.709) |
−0.07499151 (0.339) |
−0.100334173 (0.246) |
0.015861648 (0.632) |
| A | 0.108024696 (0.621) |
0.036196732 (0.539) |
0.130630562 (0.299) |
0.076212977 (0.281) |
0.415318324 (0.0006) |
| E/A | 0.201638313 (0.003) |
0.398341723 (0.0005) |
−0.32146173 (0.002) |
−0.331756241 (0.0004) |
−0.752302036 (0.001) |
| e’ mean | −0.029568502 (0.365) |
0.047484822 (0.209) |
0.370611156 (0.0001) |
0.298308105 (0.0025) |
0.365767929 (0.002) |
| E/e’ | 0.002904438 (0.567) |
0.017774328 (0.666) |
−0.28065295 (0.002) |
−0.264280021 (0.004) |
−0.15311 (0.06) |
| MAPSE | −0.02 (0.4966) |
0.03 (0.388) |
0.35 (0.005) |
0.21 (0.013) |
0.68 (0.0001) |
ARSD: Aortic root systolic distance, ARDD: Aortic root diastolic distance, ARSE: Aortic root systolic excursion, EF: Ejection fraction, and MAPSE: Maximum annular plane systolic excursion
We found the mean value of ARDD as 2.59 ± 0.43 cm. The aortic root maximal diastolic velocity (ARDV) was 10.8 ± 2.4 cm/s. The aortic root systolic distance (ARSD) was 2.71 ± 0.65 cm. The aortic root maximal systolic velocity (ARSV) was 7.92 ± 2.26 cm/s. The mean aortic root excursion was 4.3 mm. ARSE showed a parallel relation with the LV function (r up to 0.7). We found ARSD and ARSV correlating weakly with systolic Doppler parameters, such as ejection fraction (EF), maximum annular plane systolic excursion (MAPSE), and s' medial. ARSE was an exception that it showed a good correlation with s’medial r = 0.746 (P < 0.001), EF r = 0.807 (P < 0.001), and MAPSE r = 0.68 (P < 0.001). The ARDD and ARDV related poorly with LV diastolic parameters such as e' mean, e' medial, e' lateral, E/A, and E/e’. E velocity, E/A, and E/e’mean showed a negative correlation with ARDV.
ARDD (r up to 0.02) and ARSD (all r values < 0.40) did not correlate with the LV Doppler measurements. ARDV correlated (r up to 0.51) with some LV diastolic Doppler parameters and ARSV correlated in the moderate range only with mitral annulus plane systolic excursion (r = 0.31). In fact, we found that ARDD is related better than ARDV with Doppler measurements.
Below is the summary of the results of the correlation between the newer parameters with the regular parameters of LV function:

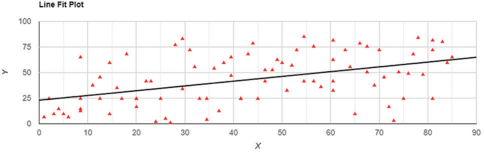
Above figure shows the significant medium positive correlation between EF and ARSV

Above figure shows the significant medium positive correlation between EF and ARDV

Above figure shows a large positive significant correlation between EF and ARSE

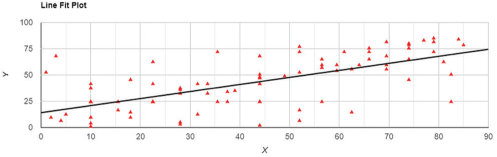
Above figure shows a significant large positive correlation between s’medial and ARSE

Medium positive correlation between s’medial and ARSV

The medium positive relation between S’medial and ARDV
The medium positive correlation between A velocity and ARSE

The medium positive correlation between e’mean and ARDV

Small positive relationship between e’mean and ARDD
The large positive relation between MAPSE and ARSE
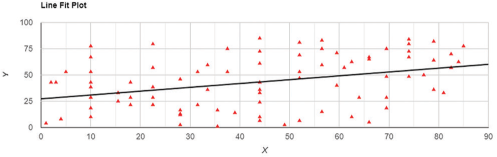
The medium positive relation between MAPSE and ARSV

The non-significant very small positive relation between MAPSE and ARSD
DISCUSSION
The results of our study showed that ARSE showed a significant correlation with EF, MAPSE, and s’medial. The systolic parameters recorded with Doppler flow and Doppler tissue imaging, like ARSD, and ARSV showed moderate correlation with s’medial, EF, and MAPSE. However, the new diastolic parameters showed a weak correlation with E, E/A, and E/e’mean. Aortic root maximum diastolic distance showed stronger correlations than diastolic velocity.
The most important finding is that the aortic root displacement is reduced in patients with LV dysfunction. Therefore, it can be especially useful in patients for assessing LV function even in patients with LV dysfunction. In our study, we found a strong correlation of ARSE with EF, s’medial, and MAPSE, whereas the new diastolic parameters showed a poor correlation with E, E/A, and E/e’mean. While interpreting the results, it is important to keep in mind that our study provides information about subjects affected by cardiovascular diseases. Hence, we can expect significant variability in physiology affected by various factors such as aging, hypertension, diabetes, myocardial infarction, and cerebrovascular accidents.
Jingi et al. also studied the aortic root motion and derived a formula to calculate EF based on ARSE, LVEF (%) = 29 × In [ARSE].[5] This formula is applicable even in patients with severe LV dysfunction. Hence, these findings are in agreement with the findings of our study. Even the measurement of aortic root angle showed a correlation with LV function by EF as well as global longitudinal strain as studied by Soltan et al.[6] However, we did not include GLS in our study.
Mahfouz et al. studied aortic root excursion in HfpEF patients and found that reduced ARSE predicts subclinical LV dysfunction as well as poor effort tolerance. However, they defined a higher cutoff of 7.5 mm for predicting exercise intolerance.[7] Whether the ARSE needs to be indexed to the body surface area is an issue that needs to be further clarified in future studies.
Karwat et al. studied the aortic root motion parameters in a healthy population and found a significant correlation with diastolic parameters of ARDD more than ARDV.[8]These findings are in contrast to our findings where systolic parameters correlated better than those of diastolic parameters. There may be several factors which need to be analyzed that are affecting the movement of the aortic root and we need to include them in the analysis. Tethering of myocardium in cases of MI, regional wall motion abnormalities, aortic stiffness, myocardial stiffness, cardiac remodeling, stunning, etc., are a few of them.
The factors which may influence the aortic root motion in systole have been studied by Aurich et al.[2] They found a weak association between stroke volume and systolic aortic root motion and no definitive relation with systolic blood pressure. However, Pratt et al. found a significant positive relation with stroke volume. Left atrial volume change was supposed to contribute to systolic aortic root motion by Strunk et al. that this study was focused on the posterior wall of the aortic root and left atrial angiograms were used to calculate LA volumes.[9,10] Biamino et al., further, refined this hypothesis by including sinus rhythm and the absence of mitral insufficiency and ASD as prerequisites for aortic root motion to reflect LV stroke volume.[11]
We believe that our study is the first one to study these newer parameters of aortic root motion in patients with LV dysfunction. We also found significant correlations between systolic aortic root motion and systolic LV parameters. However, diastolic parameters correlated weakly with the diastolic aortic root motion. With the methods we used in our study, we intend to provide vital information regarding the movement of the aortic root, especially in subjects with LV dysfunction. We conclude that in our subjects, the systolic aortic root motion parameters correlate significantly with established measurements of the LV function, most importantly the aortic root systolic distance and velocity. In patients with low ultrasound image quality, especially when there are no apical views available for routine LV function assessment aortic root motion parameters can be useful. However, we need more studies especially in diseased populations to analyze other factors which affect the aortic root motion parameters and their relation with the LV systolic and diastolic function.
CONCLUSION
In our study, we included subjects with cardiovascular diseases and we conclude that systolic aortic root motion correlates significantly with systolic LV function, the most essential being the aortic root systolic velocity. We found that the diastolic root motion parameters correlated weakly with the diastolic LV function. In patients with poor echo windows, aortic root motion may be helpful in predicting LV function in patients with or without LV dysfunction.
Limitations
Several limitations must be borne in mind before interpreting our results. The first one is the number of patients. Larger studies may be needed before we come to a definitive conclusion. Moreover, we have used 2D images for tracking the aortic root motion. 3D imaging would be better to track the volumetric data of the aortic root. Detailed analysis of the subjects’ pathophysiology may be needed to understand the relationship with the LV function.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Audio summary available at
Financial support and sponsorship
Nil.
References
- Limited bedside echocardiography by emergency physicians for diagnosis of diastolic heart failure. Emerg Med J. 2012;29:280-3.
- [CrossRef] [PubMed] [Google Scholar]
- Pathophysiological background and prognostic implication of systolic aortic root motion in non-ischemic dilated cardiomyopathy. Sci Rep. 2019;9:3866.
- [CrossRef] [PubMed] [Google Scholar]
- Echocardiography of the Aortic Root. Invest Radiol. 1968;3:356-66.
- [CrossRef] [PubMed] [Google Scholar]
- Correlations of left ventricular systolic function indices with aortic root systolic excursion (ARSE): A cross-sectional echocardiographic study. PLoS One. 2018;13:e0206199.
- [CrossRef] [PubMed] [Google Scholar]
- Systolic Aortic Root Motion and Angle as Novel Indices of Left Ventricular Systolic Function. Germany: ResearchGate; 2020
- [CrossRef] [Google Scholar]
- Aortic root systolic excursion and its association with exercise tolerance in patients with heart failure with preserved ejection fraction. J Cardiol Curr Res. 2021;14:155-61.
- [CrossRef] [Google Scholar]
- Aortic root movement correlation with the function of the left ventricle. Sci Rep. 2021;11:4473.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of left ventricular stroke volume on aortic root motion: An echocardiographic study. Circulation. 1976;53:947-53.
- [CrossRef] [PubMed] [Google Scholar]
- The posterior aortic wall echocardiogram, its relationship to left atrial volume change. Cardiovasc Res. 1976;54:744-50.
- [CrossRef] [PubMed] [Google Scholar]
- Echocardiographic pattern of motion of the aortic root as a correlate of left atrial volume changes. Am Heart J. 1980;100:191-200.
- [CrossRef] [PubMed] [Google Scholar]







