Translate this page into:
Unmasking of Exercise-Induced Diastolic Dysfunction in Symptomatic Post Coronary Angiogram Patients with Normal Coronaries
M.S. Harish Reddy, MD DM final year Resident, Department of Cardiology, Nizam's Institute of Medical Sciences Punjagutta, Hyderabad 500082 India sugunakar66@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract

Background Diastolic dysfunction is the cause in nearly half of cases of heart failure, the hemodynamic equivalent of which is elevated cardiac filling pressures. However, owing to its ubiquity, it is often diagnosed as an incidental finding, but an association with symptoms is not established in many of the patients. Most patients with hypertension or left ventricular (LV) hypertrophy have evidence of impaired diastolic function as a finding on Doppler echocardiography, but do not have any symptoms of heart failure at rest. However, these patients do have symptoms related to diastolic dysfunction only during exercise. In this study, we have contemplated to assess invasively, left ventricular filling pressures in patients with unexplained shortness of breath with normal systolic and diastolic function on echocardiography, on exercise and compare the level of rise in patients with established diastolic dysfunction.
Methods This is an observational prospective study, done over a span of 3 months, wherein patients with typical symptoms such as chest pain and shortness of breath, after ruling out systemic causes, and were subjected to coronary angiogram. If no coronary lesion identified, patients were subjected to invasive cardiac catheterization during coronary angiogram. Patients were divided into two groups, one without diastolic dysfunction and the other with established diastolic dysfunction. Simultaneous left ventricular end diastolic pressures (LVEDP) were measured at rest and after 3-minute manual handgrip exercise and readings were noted.
Results The mean age of the population (n = 30) was 55.8 ± 7.538 and 20 were males. The mean value of LVEDP in patients with no diastolic dysfunction at resting was 4.4 ± 3.169 and after exercise was 8.40 ± 4.169. The mean value of LVEDP in patients with established diastolic dysfunction at resting was 5.30 ± 3.948 and after exercise was 8.75 ± 4.506. Paired t-test among two groups revealed a significant p-value of 0.001 after exercise among both groups, suggesting a significant increase in LVEDP in patients with exercise. Unpaired t-test comparing both groups revealed that the elevation of LVEDP in no diastolic dysfunction group was comparable with patients with diastolic dysfunction (p = 0.432).
Conclusion The increase in LVEDP with exercise is a well-established fact in patients with diastolic dysfunction. Our study adds to the fact that patients with unexplained shortness of breath can have raised LVEDP after exercise, thereby unmasking the underlying diastolic dysfunction. Our study stresses the importance of inclusion of exercise as a provocative test for the assessment of diastolic function, either invasively or non-invasively, in patients presenting with exertional dyspnea.
Keywords
LVEDP
diastolic dysfunction
diastolic dysfunction after exercise
elevated LV filling pressures
Introduction
Diastolic dysfunction is the cause in nearly half of cases of heart failure, the hemodynamic equivalent of which is increased cardiac filling pressures.1 However, owing to its ubiquity, it is often diagnosed as an incidental finding, but an association with symptoms is not established in many patients. Most patients with hypertension or left ventricular (LV) hypertrophy have evidence of impaired diastolic function as a finding on Doppler echocardiography, but do not have any symptoms of heart failure at rest.2 Diagnosis of HFpEF is easily made, when patients present as acutely decompensated heart failure. However, among people presenting with long-standing dyspnea, diagnosis solely relies on identifying a direct or indirect evidence of elevated left ventricular (LV) filling pressures. Further, many patients with HFpEF display normal LV filling pressures at rest, but abnormal pressures that develop only during physiological stresses such as exercise.3 It is becoming evident that diastolic dysfunction plays a major role in precipitating heart failure and in determining prognosis, after ruling out pulmonary and obvious cardiac causes.
Patients with dyspnea on exertion, who do not have abnormal systolic or diastolic function, would have a steeper LV pressure–volume relation in diastole, during exercise, when compared with those who have no symptoms of dyspnea on exertion, despite similar LV diastolic functions at rest.4 5 In a patient with diastolic dysfunction, initially only LV end-diastolic pressure is the only abnormally elevated pressure, whereas mean PCWP and LA pressure remain normal. With tachycardia and/or increased LV afterload, mean PCWP and LA pressure tend to increase, forming the basis for isolated diastolic stress test. Recent ESC 2021 guidelines on heart failure have recommended right heart catheterization in selected patients with HFpEF as class IIb recommendation for diagnosis of heart failure. In this study, we have contemplated to assess invasively, LV filling pressures in patients with unexplained shortness of breath with normal systolic and diastolic functions on echocardiography and compare the level of rise in patients with established diastolic dysfunction.
Materials and Methods
This was an observational prospective study done over a span of 3 months. The study population included patients between 18 and 65 years of age, presenting with shortness of breath of unexplained etiology to Nizams Institute of Medical Sciences, Hyderabad, a tertiary care multi-specialty hospital in South India, during Feb2021 to Apr 2021. These patients were then subjected to coronary angiogram to rule out shortness of breath as an angina equivalent, and those patients, with normal systolic and diastolic functions at rest or established diastolic dysfunction on echocardiography and with normal coronaries or mild coronary artery disease during coronary angiogram were included under our study. Patients with acute coronary syndrome or significant CAD, which can explain the symptoms, patients with acute decompensated heart failure, established systolic and diastolic heart failure, and patients with alternative causes of clinical syndrome of HF such as primary cardiomyopathies (hypertrophic, infiltrative, or restrictive), constrictive pericarditis, high-output heart failure, significant valvular heart disease (>moderate regurgitation or > mild stenosis), pulmonary embolism and right ventricular myopathies or patients with other systemic causes of shortness of breath are excluded from the study. Patients satisfying the inclusion and exclusion criteria were enrolled in the study after taking a duly informed consent. Patients were then divided into two groups. Group A included patients with normal diastolic function at rest on echocardiography. Group B included patients with grade I, II, and III diastolic dysfunction on echocardiography at rest. After assigning into groups, patients were subjected to coronary angiogram and if no coronary lesion identified, patients were subjected to LV filling pressure assessment invasively, during coronary angiogram by left heart catheterization, at rest and after exercise for 3 minutes. LV diastolic pressures at rest and during exercise were obtained by introducing a Judkins Right catheter into the LV from a radial arterial or femoral arterial access site. The exercise protocol employed is manual handgrip exercise by hand gripper exercise tool for 3 minutes to maintain uniformity in study. LVEDP were noted at rest and at exercise and subjected for statistical analysis.
Statistical Analysis
Data were collected, compiled using Microsoft Excel, and statistical analyses were done using SSPS v20.0. Results on continuous variables are presented as mean and standard deviation. Results on categorical variables are presented as percentages. Chi square test was used to find the significance of study parameters on a categorical scale between the two groups. Continuous variables were analyzed using independent t-test for normal distribution. Binomial regression analysis was applied for subgroup analysis for comparison across different groups across controls versus cases. All p-values are two-tailed and p < 0.05 was considered statistically significant.
Results
The mean age of the population (n = 30) was 55.83 ± 7.58 years and there were 22 males and 8 females. The demographics of the population among groups was as follows: The mean age of patients in patients with diastolic dysfunction was 56.50 ± 8.569 years. The mean age of patients in patients without diastolic dysfunction was 54.50 ± 5.233 years.
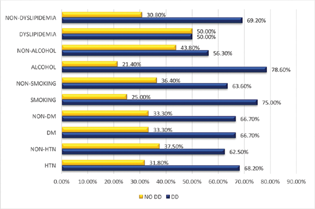
Among risk factor distribution between the two groups, there was a higher prevalence of hypertension, diabetes mellitus, smoking, and alcohol consumption in patients included in the group with diastolic dysfunction; however, these differences were not statistically significant (Table 1 and Fig. 1). Dyslipidemia was equally distributed across both groups. Only patients with mild CAD and normal coronaries were included in the study, and out of patients with mild CAD, 75% had diastolic dysfunction and 25% were patients without diastolic dysfunction. Out of those with normal coronaries, 60% were had diastolic dysfunction and 40% were without diastolic dysfunction.
-
Fig. 1 Risk factors distribution between diastolic dysfunction and non-diastolic dysfunction groups.
Fig. 1 Risk factors distribution between diastolic dysfunction and non-diastolic dysfunction groups.
|
Risk Factor |
Gender |
DD |
NO DD |
p-Value |
|---|---|---|---|---|
|
Hypertension |
Male |
13(81.3%) |
3(18.8) |
1.00 |
|
Female |
2(33.3%) |
4(66.7) |
||
|
T2 DM |
Male |
8(80.0%) |
2(20.0%) |
1.00 |
|
Female |
2(40.0%) |
3(60.0%) |
||
|
Smoking |
Male |
6(75%) |
2(25.0%) |
0.682 |
|
Female |
3(37.5%) |
5(62.5%) |
||
|
Alcohol |
Male |
11(78.6%) |
3(21.4%) |
0.260 |
|
Female |
3(37.5%) |
5(62.5%) |
||
|
Dyslipidemia |
Male |
2(66.7%) |
1(33.3%) |
0.584 |
|
Female |
0(0%) |
1(100%) |
The mean HbA1c of patients with diastolic dysfunction was 6.645 ± 1.1 and that in group without diastolic dysfunction was 6.660 ± 1.29. The NT-ProBNP in patients with diastolic dysfunction was 96 ± 61.59 and those with diastolic dysfunction was 84.1 ± 44.722 (Table 2). The distribution of NT-ProBNP among all patients has been depicted as a histogram with the median range of distribution at 75.50 pg/mL in Fig. 2. These parameters had non-significant distribution between both the groups (p > 0.05), suggestive of a similar distribution of patients with age, level of diabetes, and levels of NT–ProBNP between both groups and allowing us to draw conclusions as the data were matched.

-
Fig. 2 Histogram showing the mean range of distribution of NT-ProBNP in the study.
Fig. 2 Histogram showing the mean range of distribution of NT-ProBNP in the study.
|
Parameter |
Group |
N |
Mean |
Std. Deviation |
p-Value |
|---|---|---|---|---|---|
|
NT-ProBNP |
DD |
20 |
96.00 |
61.593 |
0.592 |
|
NO DD |
10 |
84.10 |
44.722 |
The mean value of LVEDP in patients with no diastolic dysfunction at resting was 4.40 ± 3.169 and after exercise was 8.40 ± 4.169 (Table 3). The mean value of LVEDP in patients with established diastolic dysfunction at resting was 5.30 ± 3.948 and after exercise was 8.75 ± 4.506. (Table 3). Paired t-test to compare the LVEDP at rest and post exercise in patients with no diastolic dysfunction was found to be significant (p = 0.01). Similarly, p-value was significant (p = 0.01) in patients with diastolic dysfunction as well (Table 3). On subgroup analysis, for both genders, the elevation of LVEDP was found to be 3.64 ± 2.060 in males, irrespective of the group they belonged to. The elevation of LVEDP was found to be 3.63 ± 1.847 in females. The elevation of LVEDP across both groups was not significantly affected by the gender, evident by insignificant p-value (0.989; Table 4).
|
Group |
Resting LVEDP |
Post exercise LVEDP |
p-Value (paired t-test) |
|---|---|---|---|
|
No diastolic dysfunction |
4.40 ± 3.169 |
8.40 ± 4.169 |
0.001 |
|
Diastolic dysfunction |
5.30 ± 3.948 |
8.75 ± 4.50 |
0.001 |
|
Sex |
N |
Mean |
Std. deviation |
p-Value |
|
|---|---|---|---|---|---|
|
Difference |
Males |
22 |
3.64 |
2.060 |
0.989 |
|
Females |
8 |
3.63 |
1.847 |
|
Group Statistics |
||||
|---|---|---|---|---|
|
Group |
N |
Mean |
Std. deviation |
p-Value |
|
No diastolic dysfunction |
9 |
4.222 |
2.5386 |
0.431 |
|
Diastolic dysfunction |
18 |
3.556 |
1.7564 |
|
Paired t-test among two individual groups revealed a significant p-value of 0.001 after exercise among both groups, suggesting a significant increase in LVEDP in patients with exercise. Unpaired t-test comparing both groups revealed that the elevation of LVEDP in no diastolic dysfunction group was comparable with patients with diastolic dysfunction (p = 0.432) (Table 5).
Discussion
Patients with normal systolic function and systemic hypertension have symptoms of dyspnea on exertion as a result of diastolic dysfunction. In these patients, in the baseline state, diastolic filling can be compensated without symptoms; however, during exercise, they fail to increase cardiac output without an increase in the left atrial pressure because a stiff left ventricle is unable to enhance its diastolic filling. Studies on left heart catheterization demonstrated a higher PCWP in patients with a history of heart failure with normal systolic function, providing objective evidence of exercise-induced diastolic dysfunction.1 6 7
Obakata et al5 in their study on simultaneous invasive-echocardiographic assessment of heart failure with preserved ejection fraction questioned the current approaches of making and excluding a diagnosis of HFpEF on the basis of resting data and firmly supported employing invasive or noninvasive hemodynamic assessments along with exercise to definitely confirm or refute the diagnosis of HFpEF.
In our study, we measured level of LVEDP rise in both groups from resting state to post exercise state. Paired t-test among two individual groups revealed a significant p-value of 0.001 after exercise among both groups, suggesting a significant increase in LVEDP in patients with exercise. Unpaired t-test comparing both groups revealed that the elevation of LVEDP in no diastolic dysfunction group was comparable with that in patients with diastolic dysfunction (p = 0.432).
In our study, we used the handgrip exercise by motion adjustable hand gripper exercise tool for 3 minutes as exercise protocol to maintain uniformity. Many of the previous studies were done using bicycle ergometer, which is a difficult exercise for many patients to perform during invasive catheterization, especially older patients. The advantage of handgrip exercise over bicycle ergometry is less respiratory and movement artifacts.
In our study, we found no significant distribution in parameters such as age, gender, and risk factors (hypertension, diabetes mellites, dyslipidemia, smoking, and alcohol), which could be individually be responsible for causing diastolic dysfunction. However, to the non-significant distribution of the above-said parameters across both the groups eliminates the possible selection bias and reduces the confounding effect on diastolic dysfunction.
The mean value of NT-ProBNP in our study in patients with diastolic dysfunction was 96 and in patients without diastolic dysfunction was 84; the difference between the two groups was statistically insignificant (p = 0.59). Indeed, it is a better known fact that elevation of NT-ProBNP was relatively less in patients with HFpEF than that in patients with heart failure with reduced ejection fraction (HFrEF). The probable explanation is believed to be due to lower wall stress, owing to thicker ventricular walls and a smaller cavity size and a wider association of obesity in these patients, where NT-ProBNP levels are usually lower. Thus, normal natriuretic peptide levels do not exclude the diagnosis of HFpEF, particularly among patients with early-stage HFpEF, which includes the majority of subjects participating in our study.
The results of our study add to the existing literature on invasive evaluation of LV filling pressures during exercise. The normal physiologic response to exercise is the occurrence of a rapid myocardial relaxation rate causing an enhanced suction effect of the LV. This suction effect causes a shift in the LV pressure–volume curve downward during early diastolic phase, allowing for complete emptying of the left atrium. In patients who were referred with symptoms of breathlessness and a limited exercise tolerance, it was postulated that ventricular filling was impaired as a result of the lack of this suction effect. Thus, to meet the increased demands of the body during exercise, an elevated left atrial pressure is a necessity, and symptoms of dyspnea occur at the expense of increased cardiac output.7 8
In our study, we found a significant rise in LVEDP with exercise in both groups, and level of rise in LVEDP in patients with no diastolic dysfunction was comparable to that in patients with established diastolic dysfunction.
There were certain limitations to our study. Our small study population was highly selected and did represent those patients who posed the greatest diagnostic dilemma to the clinician. The number of patients was too small to provide definitive predictive value of certain parameters. Further studies involving a much larger number of patients will be required to establish whether this methodology can be applied to larger groups of patients; and patients with different disease entities and determine clinically relevant cut off values that can be applied in clinical practice.
Conclusion
The increase in LVEDP with exercise is a well-established fact in patients with diastolic dysfunction. Our study adds to the fact that patients with unexplained shortness of breath can have raised LVEDP after exercise, thereby unmasking the underlying diastolic dysfunction. Our study stresses the importance of inclusion of exercise as a provocative test for the assessment of diastolic function, either invasively or non-invasively, in patients presenting with exertional dyspnea.
Conflict of Interest
None declared.
References
- Abnormalities of diastolic function as a potential cause of exercise intolerance in chronic heart failure. Circulation. 1990;81:78-86. (2, Suppl)III78–III86,
- [Google Scholar]
- Diastolic pressure-volume relations in the diseased heart. Fed Proc. 1980;39(02):148-155.
- [Google Scholar]
- Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016;29(04):277-314.
- [Google Scholar]
- Estimation of left ventricular filling pressure with exercise by Doppler echocardiography in patients with normal systolic function: a simultaneous echocardiographic-cardiac catheterization study. J Am Soc Echocardiogr. 2007;20(05):477-479.
- [Google Scholar]
- Role of diastolic stress testing in the evaluation for heart failure with preserved ejection fraction: a simultaneous invasive-echocardiographic study. Circulation. 2017;135(09):825-838.
- [Google Scholar]
- Prevalence, clinical features and prognosis of diastolic heart failure: an epidemiologic perspective. J Am Coll Cardiol. 1995;26(07):1565-1574.
- [Google Scholar]
- Assessment of diastolic function of the heart: background and current applications of Doppler echocardiography. Part I. Physiologic and pathophysiologic features. Mayo Clin Proc. 1989;64(01):71-81.
- [Google Scholar]
- Dynamic change in left ventricular apical back rotation: a marker of diastolic suction with exercise. Eur Heart J Cardiovasc Imaging. 2018;19(01):12-19.
- [Google Scholar]








