Translate this page into:
Role of Echocardiographic Aortic Propagation Velocity in Predicting Obstructive Coronary Artery Disease – A Prospective Observational Study
*Corresponding author: Rajendra Betham, Department of Cardiology, Guntur Medical College, Guntur, Andhra Pradesh, India. dr.b.rajendra@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Betham R, Nathani S, Baig AA. Role of Echocardiographic Aortic Propagation Velocity in Predicting Obstructive Coronary Artery Disease – A Prospective Observational Study. Indian J Cardiovasc Dis Women. 2024;9:150-4. doi: 10.25259/IJCDW_63_2023
Abstract
Objectives:
The aim of this study was to assess the relationship between APV and CAD and to compare AS and AD in patients with and without CAD.
Material and Methods:
A total of 100 subjects presenting to Government General Hospital, Guntur, with chest pain and undergoing coronary angiogram were selected for the study. Patients were divided into two groups, the study group comprises patients with >50% stenosis in at least one of the coronary artery on coronary angiogram, and control group comprises patients with normal coronaries on angiography. Two-dimensional echocardiography (Philips Affinity 70) was performed with the recording of data. AS and AD were calculated and APV was determined.
Result:
In the present study, it was observed that there was a statistically significant increased incidence of deranged lipid profile, diabetes, hypertension, alcohol consumption, and a positive family history of CAD in the study group. Mean APV, mean AD, and mean AS was significantly low in the study group as compared to the control group (P < 0.001).
Conclusion:
APV, AS, and AD can be used as surrogate markers to predict the presence of significant CAD and, hence, can be safely recommended as a simple, economical, and non-invasive means to screen CAD.
Keywords
Aortic propagation velocity
Aortic strain
Aortic distensibility
Coronary artery disease
ABSTRACT IMAGE
INTRODUCTION
Atherosclerosis presents a multifaceted pathology characterized by the accumulation of lipids, macrophages, and platelets within arterial walls, culminating in the narrowing of blood vessels. Its ramifications extend throughout the arterial system, impacting various anatomical regions.[1]
Coronary artery disease (CAD), a prominent manifestation of atherosclerosis in the coronary arteries, has been observed to exhibit an inverse association with certain biomechanical attributes of the aorta, such as strain and distensibility.[2]
Aortic distensibility (AD) serves as a pivotal indicator of arterial compliance, reflecting the aorta’s capacity to expand and contract in response to fluctuations in blood pressure. Progressive atherosclerosis is paralleled by a reduction in AD.[2,3]
Likewise, aortic strain (AS), gauging the relative change in the length or diameter of the aorta during each cardiac cycle, correlates with arterial compliance. Elevated AS has been linked to an increased vulnerability to atherosclerosis and CAD.[2,3]
In addition to these conventional parameters, aortic propagation velocity (APV) emerges as an innovative marker of arterial stiffness. APV assesses the velocity of pressure wave propagation along the aorta, complementing conventional methods for evaluating aortic stiffness.
Prior investigations have explored diverse parameters, including AS, AD, augmentation index, and pulse pressure, to evaluate aortic stiffness and its interplay with CAD.[3]
Our study endeavors to probe aortic stiffness using the novel parameter APV and elucidate its correlation with conventional parameters such as AS and AD. By shedding light on these associations, we aim to contribute to a comprehensive understanding of atherosclerosis and its cardiovascular implications.
MATERIAL AND METHODS
This is an observational and prospective study conducted at the Department of Cardiology, Government General Hospital (GGH), Guntur, Andhra Pradesh, India. A total of 100 subjects presenting to GGH-Guntur with chest pain and undergoing coronary angiogram were selected for study during the period of June 2021–November 2022.
Inclusion criteria
Patients who were subjected to coronary angiogram for the purpose of the following issues were included:
Patients with definite angina with/without positive treadmill test
Patients with probable angina and with positive treadmill test
As a part of pre-operative cardiac risk stratification for non-cardiac surgery
As a part of evaluation before electrophysiological study and radiofrequency ablation.
Exclusion criteria
The following criteria were excluded from the study:
Patients with acute coronary syndrome
Patient with moderate or severe valvular stenosis or regurgitation
Patients with any cardiomyopathy
Patients with arrhythmias
Patients with congenital heart disease
Patients with symptomatic heart failure.
Data collection methods
Patients were divided into two groups, the study group comprises patients with >50% stenosis in at least one of the coronary artery on coronary angiogram and the control group comprises of patients with normal coronaries on angiography.
After obtaining informed consent detailed history and medical examination were done, and blood pressure and anthropometric measurements such as height and weight were recorded.
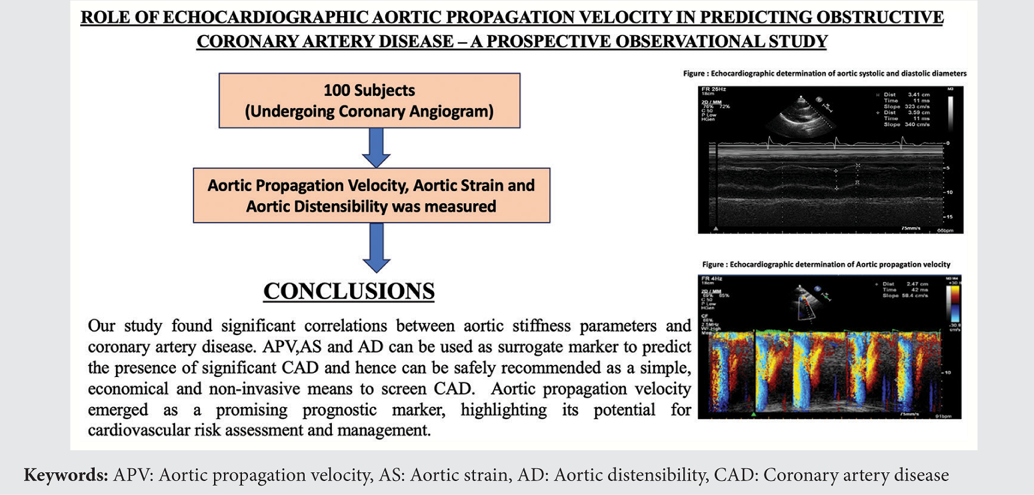
An 8 h fasting sample was drawn and the following parameters were analyzed random blood sugar (RBS), blood urea, creatinine, total cholesterol, low-density lipoprotein (LDL) cholesterol, high-density lipoprotein (HDL) cholesterol, very LDL, and triglycerides. Two-dimensional echocardiography (2D-Echo) (Philips affinity 70) [Figures 1 and 2] and coronary angiogram were performed with recording of data. AS and distensibility were calculated and APV was determined.
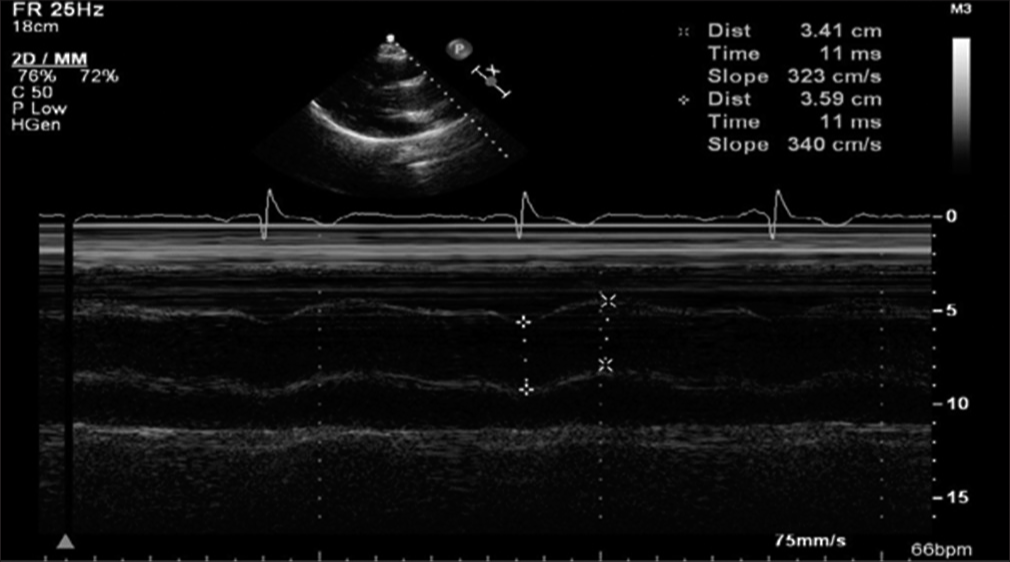
- Echocardiographic determination of aortic systolic and diastolic diameters.
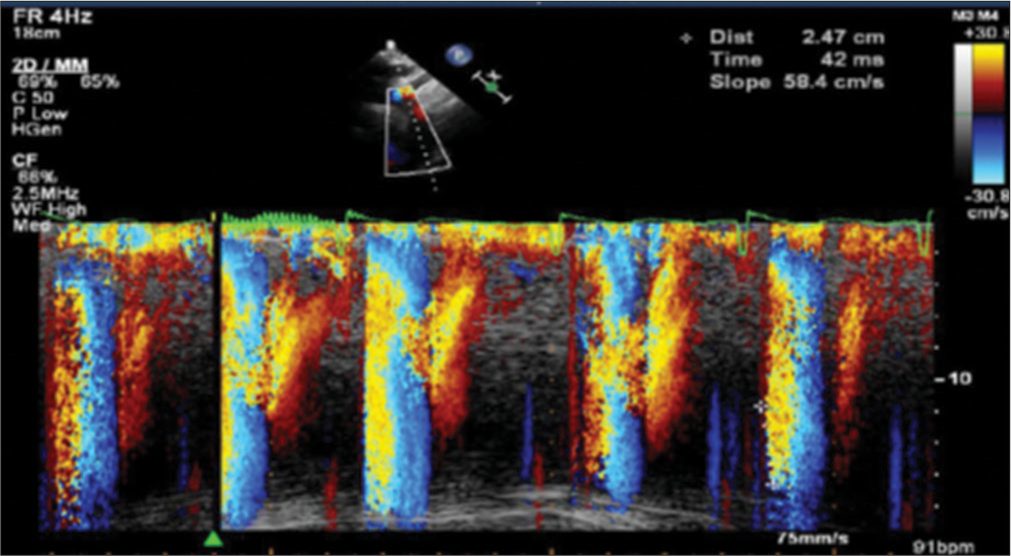
- Echocardiographic determination of aortic propagation velocity.
Statistical analysis
All data were evaluated by the Statistical Package for the Social Sciences (SPSS) (SPSS for Windows, version 15.0, Chicago, IL, USA). Parametric data were expressed as mean standard deviation (SD) and qualitative data as numbers and percentages. Differences between groups were assessed by the Chi-square for normally distributed quantitative variables. The data obtained were analyzed using SPSS version 17.0. Continuous variables were expressed as mean ± SD values. P-value (<0.05) was used to evaluate statistical significance.
Ethical considerations
Electrocardiography (ECG) and 2D-Echo are non-invasive tests. Coronary angiogram is an invasive study. The study protocol was approved by the Ethics Committee. Written informed consent was taken from all the patients after a discussion of the study process with them. After taking proper consent, patients underwent ECG and 2D-Echo and all the patients received appropriate treatment according to the guidelines.
RESULTS
In the present study, it was observed that the mean age in the study group was 56.8 ± 8.21 years compared to a control group where in mean age was 51.08 ± 8.31 years. There was no statistically significant difference in the mean age between the two groups (P = 0.12).
In the present study, it was observed that there was no statistically significant difference in the distribution of patients based on gender in either groups P = 0.38. In the control group, 31 (62%) were male, whereas, in the study group, 36 (72%) were male.
In the present study, it was observed that body mass index, serum creatinine, total cholesterol, LDL cholesterol, and triglycerides were significantly higher in the study group compared to controls P < 0.05. HDL cholesterol levels in the study group were significantly lower when compared to controls P < 0.05 [Table 1]. In the present study, it is observed that there is a statistically significant higher occurrence of diabetes, hypertension, and alcohol consumption in the study group compared to controls (P < 001). In the present study, it was observed that there was a higher occurrence of smoking and family history of CAD in the study group compared to controls but the increase was not statistically significant [Table 2].
| Parameters | Control group | Study group | P-value |
|---|---|---|---|
| Mean±SD | Mean±SD | ||
| BMI | 24.20±1.59 | 24.64±1.18 | 0.026 |
| Sr. Creatinine | 0.93±0.23 | 1.05±0.25 | 0.008 |
| Total cholesterol | 169.72±11.75 | 176.44±13.69 | <0.009 |
| LDL | 87.82±8.1 | 92.08±9.38 | <0.02 |
| HDL | 40.48±2.98 | 39.12±3.17 | <0.01 |
| Triglycerides | 138.5±9.04 | 144.22±8.5 | <0.001 |
BMI: Body mass index, LDL: Low-density lipoprotein, HDL: High-density lipoprotein, SD: Standard deviation, Sr: Serum
| Controls (%) | Study group (%) | P-value | |
|---|---|---|---|
| Diabetes | 8 (16) | 33 (66) | <0.001 |
| Hypertension | 10 (20) | 40 (80) | <0.001 |
| Alcohol | 10 (20) | 22 (44) | <0.005 |
| Smoking | 9 (18) | 13 (26) | 0.33 |
| Family history of CAD | 2 (4) | 5 (10) | 0.24 |
CAD: Coronary artery disease
In the present study, it was observed that there was no statistically significant difference in the mean ejection fraction between the two groups (P = 0.4).
In the present study, it was observed that there is no statistically significant mean difference in aortic diastolic diameter (P = 0.08) and aortic systolic dimension between the two groups P (0.32). However, it was observed that APV, AS, and AD were significantly low in the study group compared to the control group [Table 3].
| Parameters | Control group | Study group | P-value |
|---|---|---|---|
| Mean±SD | Mean±SD | ||
| Aorta diastolic diameter | 2.16±0.15 | 2.22±0.19 | 0.08 |
| Aorta systolic diameter (cm) | 2.70±0.28 | 2.73±0.31 | 0.6 |
| Aorta strain (%) | 32.75±4.67 | 26.5±5.58 | <0.001 |
| Aorta dispensability (cm2/dyn) | 1.49±0.26 | 1.23±0.30 | <0.001 |
| Aorta propagation velocity (cm/s) | 65.68±9.37 | 52.14±13.8 | <0.001 |
SD: Standard deviation
DISCUSSION
Our study demonstrated a noteworthy association between APV and CAD, revealing a statistically significant correlation with both AS and AD. APV exhibited a robust correlation with the extent of CAD, whereas AS and AD displayed stronger associations with risk factors such as aging and hypertension.
We observed a significantly lower mean AS in the study group compared to the control group (P < 0.01). In the control group, AS measured 32.75 ± 4.67%, while in the study group, it was 26.50 ± 5.58%. Similar findings have been reported in the previous studies by Ghaderi et al. and Sen et al. [2,4]
Bakirci et al. did a study in 2022 to find the association between APV and CAD in patients with stable angina pectoris (SAP). Two hundred and fourteen patients were included in this study. They found that decreased APV correlates with the severity of atherosclerotic CAD in SAP patients.[5]
Similarly, mean AD was significantly lower in the study group compared to the control group (P < 0.01). AD measured 1.49 ± 0.26 in the control group and 1.23 ± 0.30 in the study group. Lower AD was observed in patients with hypertension, diabetes, smoking, and alcoholism, suggesting that vascular responsiveness to these risk factors contributes to increased stiffness and reduced distensibility. This is consistent with findings from studies by Ghaderi et al. and Sen et al.[2,4]
Moreover, mean APV was significantly lower in the study group compared to the control group (P < 0.05). APV measured 65.68 ± 9.37 in the control group and 52.14 ± 13.8 in the study group, with P < 0.001. Patients with significantly lower APV were more likely to have double and triple vessel disease. Similar results have been reported in studies by Gunes et al.,[6] Sen et al.,[4] Chetty et al.,[7] and Ghaderi et al.[2]
APV emerges as a straightforward and convenient echocardiographic parameter applicable in routine clinical practice. Its optimal clinical utility lies in non-invasive cardiovascular risk stratification and patient management, aiding in the selection of high-risk individuals. Our study demonstrated a significant reduction in APV among patients with significant CAD compared to those with insignificant disease.
However, several limitations warrant consideration. First, our study involved a relatively small sample size, necessitating further investigation with larger cohorts to validate our findings. In addition, being a single-center study, the generalization of results may be limited.
CONCLUSION
Our study found significant correlations between aortic stiffness parameters and CAD. APV, AS, and AD can be used as surrogate markers to predict the presence of significant CAD and, hence, can be safely recommended as a simple, economical, and non-invasive means to screen CAD. APV emerged as a promising prognostic marker, highlighting its potential for cardiovascular risk assessment and management.
Ethical approval
This study was approved by the Institutional Ethical Committee approval no GMC/IEC/179/2021.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Audio summary available at
Financial support and sponsorship
Nil.
References
- Aortic Propagation Velocity in Predicting Coronary Artery Disease: A Systematic Review and Meta-Analysis. Medicine (Baltimore). 2023;102:e34243.
- [CrossRef] [PubMed] [Google Scholar]
- The Predictive Role of Aortic Propagation Velocity for Coronary Artery Disease. BMC Cardiovasc Disord. 2018;18:121.
- [CrossRef] [PubMed] [Google Scholar]
- The Association of Elasticity Indexes of Ascending Aorta and the Presence and the Severity of Coronary Artery Disease. Coronary Artery Dis. 2008;19:311-7.
- [CrossRef] [PubMed] [Google Scholar]
- A New Echocardiographic Parameter of Aortic Stiffness and Atherosclerosis in Patients with Coronary Artery Disease: Aortic Propagation Velocity. J Cardiol. 2013;62:236-40.
- [CrossRef] [PubMed] [Google Scholar]
- Aortic Propagation Velocity in the Prediction of Coronary Artery Disease Severity. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2022;166:51-6.
- [CrossRef] [PubMed] [Google Scholar]
- The Relation Between the Color M-mode Propagation Velocity of the Descending Aorta and Coronary and Carotid Atherosclerosis and Flow-Mediated Dilatation. Echocardiography. 2010;27:300-5.
- [CrossRef] [PubMed] [Google Scholar]
- Aortic Velocity Propagation: A Novel Echocardiographic Method in Predicting Atherosclerotic Coronary Artery Disease Burden. J Saudi Heart Assoc. 2017;29:176-84.
- [CrossRef] [PubMed] [Google Scholar]







