Translate this page into:
Obesity Paradox—Does It Exist in the Contemporary South Indian Post-Percutaneous Coronary Intervention Population?
Aramalla Sunitha, DM Student Department of Cardiology, Nizam's Institute of Medical Sciences Punjagutta, Hyderabad, Telangana 500082 India Sunitha.aramalla@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background Obesity is a predisposing factor for atherosclerotic coronary arterial disease. Many studies have shown a protective effect of obesity for major adverse cardiovascular events after percutaneous coronary intervention (PCI).
Aim The main purpose of this article is to assess the clinical characteristics, invasive angiographic features, and in-hospital cardiovascular events in obese patients compared with normal and underweight patients. We wanted to know the relationship between body mass index (BMI) and outcomes after PCI.
Methods We conducted a prospective study among patients undergoing PCI. Between 2017 and 2019, we included 1,669 participants. Multiple logistic regression was performed to determine the effect of BMI on in-hospital adverse events.
Results The patients were classified into four groups: obese (BMI ≥30 kg/m2), overweight (BMI 25 to <29.9 kg/m2), normal BMI (BMI 18.51 to <24.9 kg/m2), and underweight (BMI <18.5 kg/m2). Of 1,669 enrolled patients, 1,233 were men, and 436 were women. Among the women, 19 (35.8%) were underweight, 214(25.4%) were normal having normal BMI, 137 (23.5%) were overweight, and 66 (34%) were obese. Among the men, 34 (2.7%) were underweight, 626 (51%) has normal BMI, 445(36%) were overweight, and 128 (10.3%) were obese. Among 840 patients with normal BMI, 797 (95.4%) had no in-hospital events, 39 (4.6%) had in-hospital events. Among 582 patients who were overweight, 30 (5%) had in-hospital events, and 551 (95%) had no in-hospital events. Among 194 patients who were obese, 9 (4.6%) had in-hospital events and 181 (95.4%) had no in-hospital events.
There were no in-hospital events in the underweight group. When in-hospital events were compared with different subgroups depending on the weight, it was not statistically significant (for obesity, p = 0.72, and underweight, p = 0.162). When the events in patients with higher than normal BMI (overweight and obese) were compared with events in underweight, it was statistically significant (p = 0.03). It means that a higher BMI was associated with a higher in-hospital event rate.
Conclusion A paradox regarding the association of higher BMI with decreased in-hospital events after PCI is not seen in contemporary south Indian post PCI patients.
Keywords
body mass index
percutaneous coronary intervention
obesity paradox
Introduction
Studies globally reported that more than 2 billion people are overweight, and 650 million are obese. Nearly 2.8 million deaths have been reported as a result of having a higher body mass index (BMI). In India, nearly around 135 million individuals are affected by obesity.1 Obesity is neglected problems that lead to metabolic syndrome and thus cardiovascular disease.2 Obesity is an independent risk factor of mortality and morbidity due to cardiovascular disease.3 It is known that obesity was associated with adverse cardiovascular events after the percutaneous coronary intervention (PCI).4 5 6 However, many studies have shown a paradoxical U-shaped relationship between obesity and cardiovascular events such as heart failure and myocardial infarction, thus suggesting that patients with higher BMI had less short- and long-term mortality rates that have been termed the “obesity paradox” or “reverse epidemiology.”7 8 9 10 11 12 13 14 15 The precise mechanism of this phenomenon is unclear.16 17 18 There are few data regarding the obesity paradox, especially in south Indian populations, because few studies have been conducted. The objective of our study is to evaluate for the presence of obesity paradox among the contemporary South Indian population.
Materials and Methods
After informed consent, we prospectively enrolled 1,669 patients from our unit PCI registry. We noted the demographic data (age, sex, socioeconomic status), risk factors (diabetic mellitus, hypertension, smoking), clinical presentation, electrocardiogram, echocardiography, complete blood picture, renal function tests, liver function tests, serum electrolytes, and angiographic findings in all the patients. BMI was calculated in all the patients who underwent PCI, and the population was stratified according to the World Health Organization classification into four groups as underweight, normal, overweight, and obese. The in-hospital events were noticed in all the patients for 3 days post-PCI, and the results were analyzed using binary logistic regression.
Results
Baseline Clinical Characteristics
A total of 1,669 patient population were studied over 2 years. The baseline clinical characteristics of the study patients, according to BMI, are shown in Table 1.
|
n = 1,669 |
BMI <18.5 kg/m2 (n = 53) |
BMI 18.5–24.9 kg/m2 (n = 840) |
BMI 25–30 kg/m2 (n = 582) |
BMI >30 kg/m2 (n = 194) |
|---|---|---|---|---|
|
Abbreviations: ACS, acute coronary syndrome; BMI, body mass index; CABG, coronary artery bypass grafting; CSA, chronic stable angina; PCI, percutaneous coronary intervention; LV, left ventricle. |
||||
|
Age (y) |
60.64 ± 10.7 |
57.43±10.6 |
57.54±10.15 |
56.98±9.9 |
|
Female (n = 436) |
19 (35.8%) |
214 (25.4%) |
137 (23.5%) |
66 (34%) |
|
Male (n = 1233) |
34(64.2%) |
626 (74.6%) |
445 (76.4%) |
128 (66%) |
|
Diabetes |
||||
|
Yes |
36 (73.5%) |
640 (76.2%) |
446 (76.6%) |
151 (77.8%) |
|
No |
16 (26.4%) |
200 (23.8%) |
136 (23.4%) |
44 (22.2%) |
|
Smoker |
||||
|
Yes |
10 (18.9%) |
165 (19.6%) |
141 (24.2%) |
41 (21.1%) |
|
No |
43 (81.1%) |
675 (80.3%) |
441 (75.7%) |
153 (78.8%) |
|
Hypertension |
||||
|
Yes |
44 (83%) |
708 (84.3%) |
508 (87.2%) |
173 (89.1%) |
|
No |
8 (17%) |
132 (15.7%) |
74 (12.7%) |
21 (10.8%) |
|
Presentation |
||||
|
ACS |
29 (54.7%) |
351 (41.7%) |
231 (39.7%) |
79 (40.7%) |
|
CSA |
24 (45.4%) |
489 (58.2%) |
351 (60.3%) |
115 (59.2%) |
|
LV ejection fraction |
||||
|
Good |
27 |
519 |
389 |
148 |
|
Mild |
11 |
126 |
83 |
26 |
|
Moderate |
6 |
107 |
61 |
9 |
|
Severe |
9 |
88 |
49 |
11 |
|
Previous PCI |
||||
|
Yes |
10 (18.9%) |
153 (18.2%) |
112 (19.2%) |
36 (18.5%) |
|
No |
43 (81.1%) |
687 (81.8%) |
470 (80.8%) |
158 (81.5%) |
|
Previous CABG |
||||
|
Yes |
1 (1.8%) |
59 (7%) |
38 (6.5%) |
20 (10%) |
|
No |
52 (98.2%) |
781 (93%) |
544 (93.5%) |
174 (90%) |
|
In-hospital events |
||||
|
Yes |
0 (0%) |
39 (4.6%) |
30 (5%) |
9 (4.6%) |
|
No |
53 (100%) |
797 (95.4%) |
551 (95%) |
181 (95.4%) |
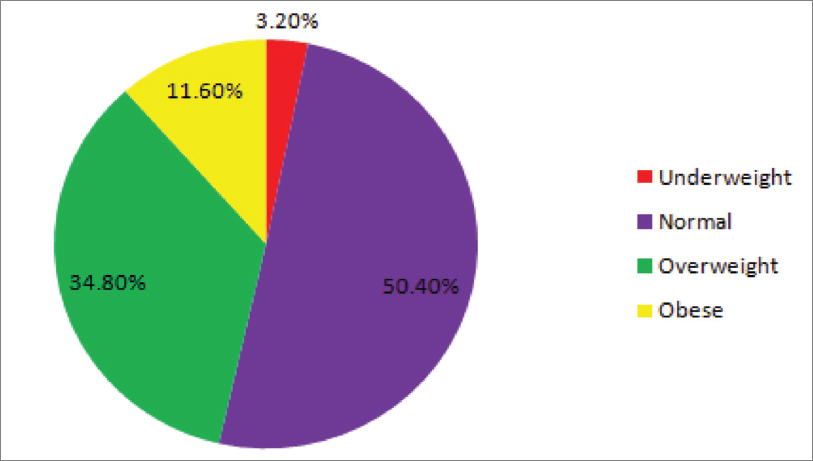
The distribution of BMI for the 1669 study population is shown in Fig. 1. The distribution average BMI in the total population is 25.25.
-
Fig. 1 Distribution of body mass index.
Fig. 1 Distribution of body mass index.
Of 1,669 patients, 3.2% (n = 53) were underweight, 50.3% (n = 840) were normal weight, 34.9% (n = 582) were overweight, and 11.6% (n = 194) were obese. There is no difference in mean age in patients with obesity when compared with those without obesity 56.2 versus 57.5 years. Patients with a high BMI did not have a higher incidence of coronary risk factors such as hypertension (p = 0.08) and diabetes mellitus (p 0.34), current smoking habit (p 0.46 rate of previous PCI (p 0.49) than those with a low BMI. On the other hand, patients with a low BMI also did not show any less occurrence of risk factors when compared with the other population who were older and had risk factors like hypertension (p = 0.38), and diabetes mellitus (p = 0.11), current smoking habit (0.33) rate of previous PCI (p = 0.46). Patients with a lower BMI were more likely to present with the acute coronary syndrome (p < 0.03) when compared with those with a higher BMI. The fact that obese people had more incidence of heart failure with preserved ejection fraction was examined, which showed a statistically significant difference in the occurrence of good left ventricle function when compared with the underweight group.
Angiographic and Procedural Data
Angiographic and procedural data are shown in Table 2. The performance of transradial access and transfemoral access was equal among both obese and underweight groups with no statistically significant difference, which is 0.44. Procedural success was high in the underweight group when compared with the obese group. However, the result is not statistically significant, with a p-value of 0.39.
|
n = 1,669 |
BMI <18.5 kg/m2 (n = 53) |
BMI 18.5–24.9 kg/m2 (n = 840) |
BMI 25–30 kg/m2 (n = 582) |
BMI >30 kg/m2 (n = 194) |
|---|---|---|---|---|
|
Type of CAD |
||||
|
Abbreviations: BMI, body mass index; CAD, coronary artery disease; MVD, multivessel disease; SVD, single-vessel disease. |
||||
|
SVD |
30 (56.6%) |
496 (59%) |
338 (58%) |
116 (59.7%) |
|
MVD |
23 (55.6%) |
344 (41%) |
244 (42%) |
78 (40.2%) |
|
Access |
||||
|
Radial |
40 (75.5%) |
673 (80%) |
453 (77.8%) |
148 (76.2%) |
|
Femoral |
13 (74.5%) |
167 (20%) |
129 (22.2%) |
46 (23.8%) |
|
Procedural success |
||||
|
Yes |
53 (100%) |
766 (95.3%) |
37 (6%) |
0 (0%) |
|
No |
0 (0%) |
7 (4.7%) |
545 (94%) |
0 (0%) |
Complications
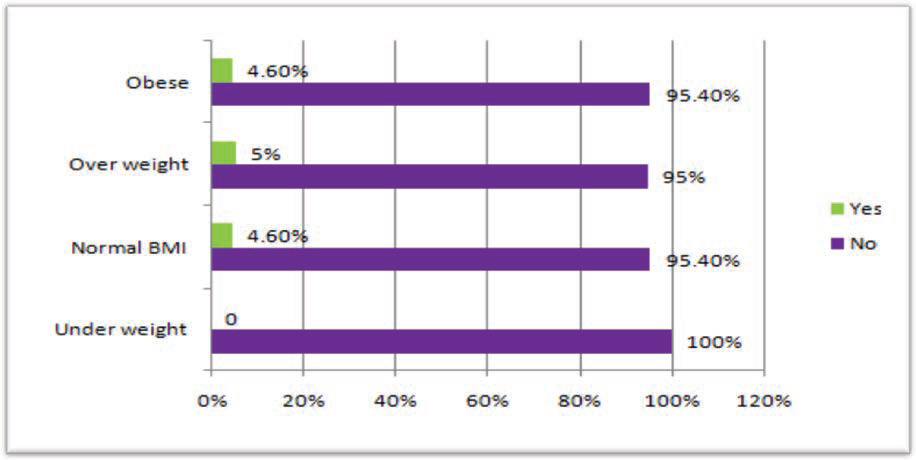
In-hospital events are shown in Fig. 2 Table 3. The underweight group had no in-hospital events. Importantly, patients in the normal BMI group (39 events; 4.6%), overweight (30 events; 5.1%) and obese groups (9 events; 4.6%), had the worst in-hospital outcomes, when compared with the underweight group.
-
Fig. 2 In-hospital events distributed among different subgroups. BMI, body mass index.
Fig. 2 In-hospital events distributed among different subgroups. BMI, body mass index.
|
n = 1,669 |
BMI <18.5 kg/2 (n = 53) |
BMI 18.5–24.9 kg/2 (n = 840) |
BMI 25–30 kg/m2 (n = 582) |
BMI >30 kg/m2 (n = 194) |
Total |
|---|---|---|---|---|---|
|
In-hospital events |
|||||
|
Type of event |
|||||
|
Abbreviations: ADHF, acute decompensated heart failure; BMI, body mass index; CIN, contrast-induced nephropathy; CVA, cerebrovascular accident; Hb, hemoglobin. |
|||||
|
1. CIN |
0 |
39 |
30 |
9 |
78 (100%) |
|
2. Fall of Hb without cause |
0 |
13 |
9 |
2 |
24 (32%) |
|
3. Access hematoma |
0 |
6 |
2 |
1 |
9 (7%) |
|
a. Femoral |
0 |
2 |
1 |
1 |
4 (3.1%) |
|
b. Radial |
0 |
1 |
0 |
1 |
2 (1.6%) |
|
4. Periprocedural MI |
0 |
7 |
4 |
2 |
13 (10.1%) |
|
5. Bleeding PR |
0 |
1 |
0 |
0 |
1 (0.78%) |
|
6. Death |
0 |
3 |
7 |
0 |
10 (7.8%) |
|
7. Pseudoaneurysm |
0 |
1 |
2 |
0 |
3 (2.34%) |
|
8. ADHF |
0 |
5 |
1 |
1 |
7 (5.5%) |
|
9. CVA |
0 |
0 |
1 |
1 |
2 (1.6%) |
|
10. Cardiogenic shock |
0 |
0 |
3 |
0 |
3 (2.34%) |
Binary logistic regression done on the relation of occurrence of in-hospital events across various variables showed no statistically significant relation with any variable except for the parameter of procedural success, which was related to the more malignant course of the hospital with a statistically significant difference of p = 0.00. The previous history of coronary artery bypass grafting and the presence of multivessel disease were also observed to tend the occurrence of higher in-hospital events with a p-value of 0.52 and 0.62 respectively. This is shown in Table 4.
|
Chi-square |
p-Value |
|
|---|---|---|
|
Abbreviations: DM, diabetes mellitus; HTN, hypertension; PCI, percutaneous coronary intervention; SM, smoking. |
||
|
Age |
0.09 |
0.766 |
|
Sex |
0.05 |
0.830 |
|
HTN |
0.75 |
0.385 |
|
DM |
0.15 |
0.694 |
|
SM |
0.22 |
0.641 |
|
Alcoholic |
0.26 |
0.613 |
|
Multivessel disease |
2.82 |
0.093 |
|
Previous PCI |
0.55 |
0.458 |
|
Procedural unsuccessful |
134.13 |
0.000 |
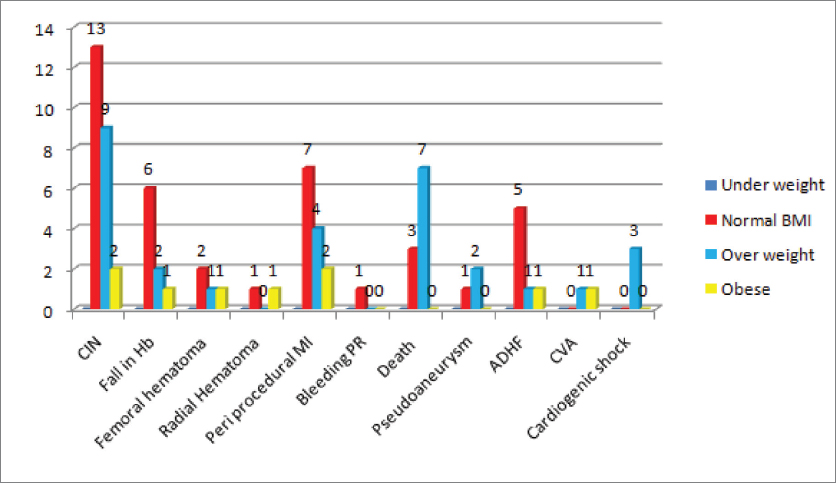
The distribution of various in-hospital events across all the four groups is demonstrated in Fig. 3. Contrast-induced nephropathy (CIN) (32% of cases) was the most frequently observed complication, followed by cerebrovascular accident (10.1%). When higher than normal BMI (overweight and obese) was considered as a risk factor for the occurrence of when compared with the underweight population, the result was not statistically significant with a p-value of 0.36.
-
Fig. 3 Distribution of types of in-hospital events across different subgroups of BMI. ADHF, acute decompensated heart failure; BMI, body mass index; CIN, contrast-induced nephropathy; CVA, cerebrovascular accident; Hb, hemoglobin.
Fig. 3 Distribution of types of in-hospital events across different subgroups of BMI. ADHF, acute decompensated heart failure; BMI, body mass index; CIN, contrast-induced nephropathy; CVA, cerebrovascular accident; Hb, hemoglobin.
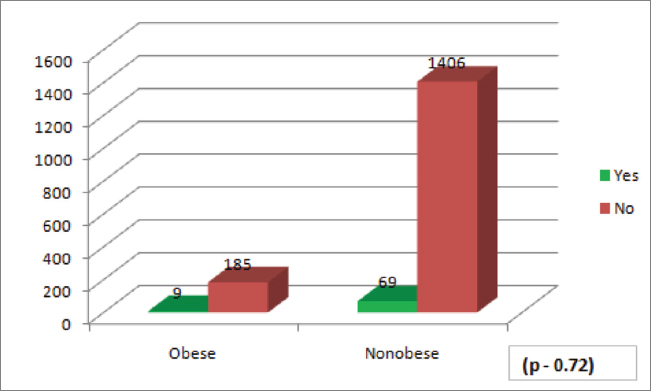
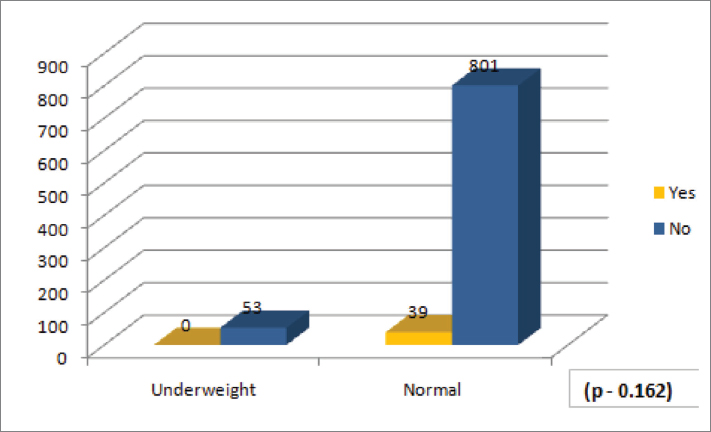
Binary logistic regression is done, and the occurrence of in-hospital events was compared with normal BMI versus obese group across various parameters, which showed no statistically significant difference in the occurrence of the events except for the procedural success, which was associated with poor in-hospital course (p = 0.000). When obesity is considered a risk factor for the occurrence of in-hospital events, the result was not significant, with a p-value of 0.720. When underweight is considered as a risk factor for the occurrence of in-hospital events, the result was not statistically significant, with a p-value of 0.162 (Figs. 4 5).
-
Fig. 4 In-hospital events in obese versus nonobese patients.
Fig. 4 In-hospital events in obese versus nonobese patients.
-
Fig. 5 In-hospital events in underweight versus normal patients.
Fig. 5 In-hospital events in underweight versus normal patients.
When the events in patients with higher than normal BMI (overweight and obese) were compared with events in the underweight group, a p-value of 0.03 was observed, which suggests that a higher BMI was associated with higher in-hospital event rate (Fig. 6).

-
Fig. 6 In-hospital events in underweight versus overweight and obese patients. BMI, body mass index.
Fig. 6 In-hospital events in underweight versus overweight and obese patients. BMI, body mass index.
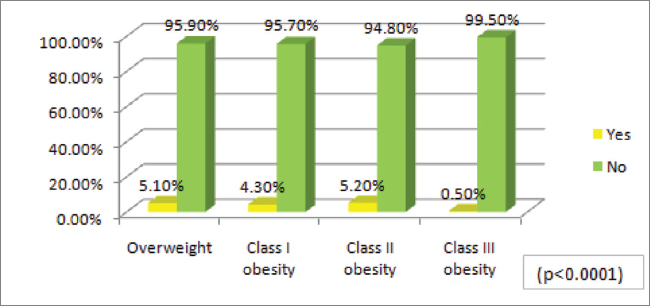
To know the correlation of higher class of obesity with in-hospital events, we have compared the events among overweight and class 1 obesity with those of obesity class 2 and 3. The result was statistically significant with a p-value of < 0.00001 (Table 5 Fig. 7).
|
In-hospital events |
Overweight (n = 582) |
Class I obesity (n = 137) |
Class II obesity (n = 38) |
Class III obesity (n = 19) |
|---|---|---|---|---|
|
Yes |
30 (5.1%) |
6 (4.3%) |
2 (5.2%) |
1 (0.5%) |
|
No |
552 (95.9%) |
131 (95.7%) |
36 (94.8%) |
18 (99.5%) |
-
Fig. 7 In-hospital events in class II and III obesity versus class I obesity and overweight.
Fig. 7 In-hospital events in class II and III obesity versus class I obesity and overweight.
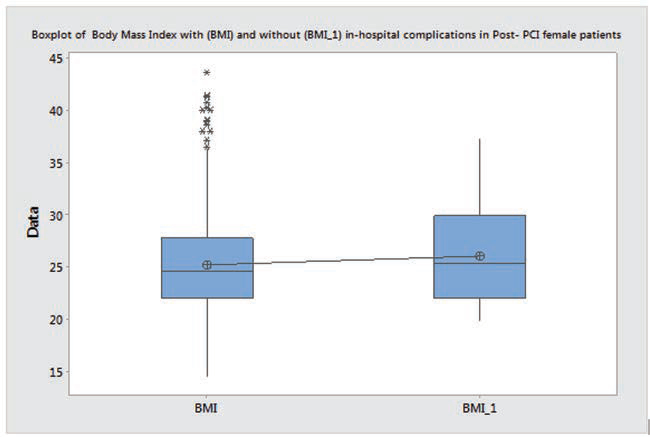
As females have more bleeding complications, we did subanalysis in female patients. In this subgroup of females also, BMI was not the determinant for in-hospital events, but the results were not statistically significant, with a p-value of 0.522 (Figs. 8 9).

-
Fig. 8 Distribution of BMI among females. BMI, body mass index; PCI, percutaneous coronary intervention.
Fig. 8 Distribution of BMI among females. BMI, body mass index; PCI, percutaneous coronary intervention.
-
Fig. 9 Box plot of BMI and without BMI in-hospital complications in post-PCI females. BMI, body mass index; PCI, percutaneous coronary intervention.
Fig. 9 Box plot of BMI and without BMI in-hospital complications in post-PCI females. BMI, body mass index; PCI, percutaneous coronary intervention.
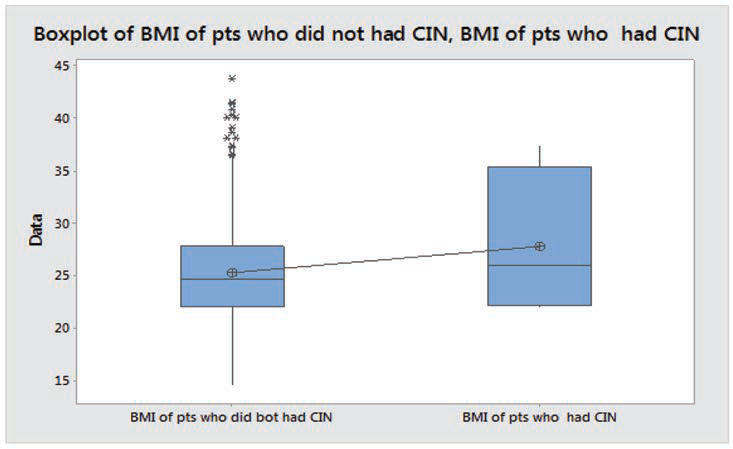
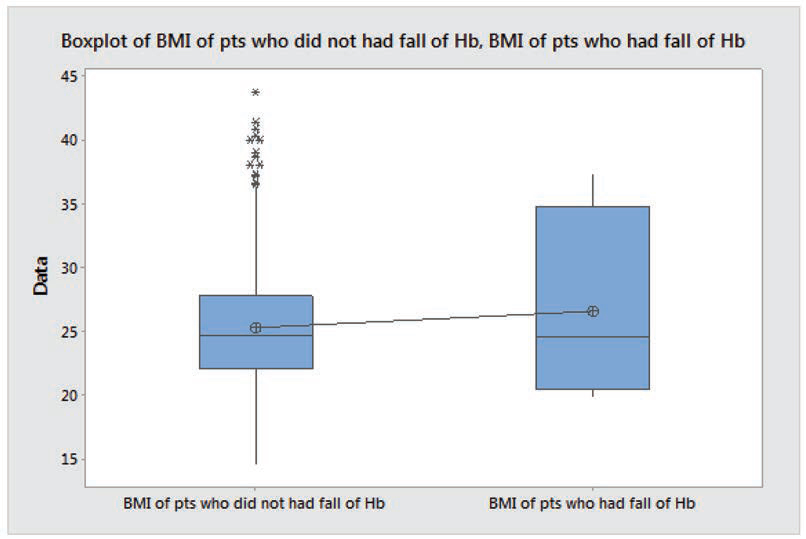
Even when subgroup analysis of in-hospital events was done for CIN and fall of hemoglobin (Hb), the BMI was not connected with both the complications. Patients with CIN had more BMI (27.8± 7.15) than the patients without CIN (25.3 ± 4.92), but the difference was not statistically significant (p = 0.53). Similarly, patients who had fallen of Hb had more BMI (26.59± 7.75) than the patients who did not have a fall of Hb (25.31 ± 4.92), but the difference was not statistically significant (p = 0.76) (Figs. 10 11).
-
Fig. 10 Box plot of patients who did not have CIN and who had CIN. BMI, body mass index; CIN, contrast-induced nephropathy.
Fig. 10 Box plot of patients who did not have CIN and who had CIN. BMI, body mass index; CIN, contrast-induced nephropathy.
-
Fig. 11 Box plot of BMI of patients who did not have a fall in Hb versus BMI of patients who had fallen in Hb. BMI, body mass index; Hb, hemoglobin.
Fig. 11 Box plot of BMI of patients who did not have a fall in Hb versus BMI of patients who had fallen in Hb. BMI, body mass index; Hb, hemoglobin.
Discussion
Individuals with higher BMI undergoing coronary angiogram tend to differ in clinical presentation and coronary anatomy when compared with individuals with normal and below normal BMI. Obese individuals have a lower incidence of high-risk coronary anatomy in the form of less prevalence of thin cap fibro atheroma compared with nonobese patients. This association was studied by Rubinshtein et al (p = 0.0002).19 These results were attributed to the younger age. The obese individuals were likely to be referred for coronary angiogram, which could be a potential explanation for the obesity paradox.
Obese patients who are on lipid-lowering therapy tend to have a significant reduction in the rate of plaque progression. These findings emphasize the potential antiatherosclerotic advantages of lipid-lowering drugs in obese patients, which may contribute to the obesity paradox.20
Kovacic et al studied individuals undergoing PCI, analyzing coronary artery calcium, and found BMI to be a negative predictor of coronary artery lesion calcification (p < 0.0001). Obese patients had lower levels of coronary artery calcium and speculated that it could be a potential mechanism leading to the obesity paradox. BMI plays a role in the level of bone mineral density, and it is proposed that the physiological strain of a higher BMI translates to denser bones.21
Gupta et al in Dallas Heart Study wanted to determine the relationship between BMI with C-reactive protein (CRP) and coronary atherosclerosis. Their study demonstrated that the association between CRP and various markers of atherosclerosis like coronary artery calcium, aortic wall thickness, and aortic plaque burden was weak in obese patients when compared with nonobese individuals (p < 0.05). This mechanism could explain the obesity paradox.22
Biasucci et al demonstrated that obese individuals have also been shown to have good endothelial function when compared with nonobese individuals. Assessing vascular function by vascular health growth factors like CD34+KDR+/CD133+ in endothelial progenitor cells that are considered as markers of vascular health/protection in 71 healthy participants, in 45 it was demonstrated that flow-mediated dilation was higher in obese individuals (p = 0.019).23
Pingitore et al used cardiac magnetic resonance imaging to measure infarct size among patients with the first episode of myocardial infarction and found that smaller infarct size was noted among the obese than in those with normal body weight (p = 0.03).24
Das et al investigated patients with morbid obesity (BMI >40 mg/m2) with ST-elevation myocardial infarction and found that these patients present at a younger age (median age 55 years for class III obese versus 66 years for normal weight) and have less severe coronary artery disease and good left ventricular function. However, class III obesity was independently associated with high major adverse cardiovascular events. So, U-shaped bimodal distribution was noticed with morbid obesity, demonstrating poor outcomes. The mechanism of this association was not known.25
In the recent decade, the number of younger females presenting with coronary artery disease has been increasing. The prevalence of class III obesity in women is also increasing. Since a long-time estrogen is known to have a protective effect on coronary artery disease, it adds further to the complexity in the process of atherogenesis that could explain the phenomenon of obesity paradox.26
Poston et al studied a total of 1,631 PCI patients and the effect of BMI on the outcomes and concluded that BMI was not a significant predictor of cardiac events. The results of his study imply that physicians should not significantly alter management for patients based on obesity status.27
Ghoorah and Campbell in his review on obesity and cardiovascular outcomes concluded that class II or III obesity had increased mortality, when compared with class I obesity category who had a lower rate of mortality.28
Our study is in line with Ghoorah and Campbell study showing that extreme obesity was associated with higher complications; however, underweight individuals did not experience any complications.
More robust studies are mandatory to analyze the concept of reverse epidemiology as the exact mechanism for this is not known.
Conclusions
Elevated BMI is not associated with lower in-hospital events after PCI, which contradicts the concept of obesity paradox. Hence, other parameters that reflect the distribution of body fat other than BMI, which is a nonspecific marker of obesity, should be considered while evaluating the risk for in-hospital events in post PCI patients.
Limitations
Following are the limitations of this study:
-
Selection bias.
-
Single-center study.
Conflict of Interest
None.
References
- Prevalence of obesity in India: a systematic review. Diabetes Metab Syndr. 2019;13(01):318-321.
- [Google Scholar]
- Global status report on noncommunicable diseases 2014. Geneva, Switzerland: WHO; Available from: http://www.who.int/nmh/publications/ncd-status-report-2014. Accessed March 1, 2020
- Impact of obesity on cardiovascular disease risk factor. Asian J Med Sci. 2019;10(01):1-12.
- [Google Scholar]
- The impact of body mass index on the one year outcomes of patients treated by percutaneous coronary intervention with Biolimus- and Sirolimus-eluting stents (from the LEADERS Trial) Am J Cardiol. 2010;105(04):475-479.
- [Google Scholar]
- Impact of body mass index on the five-year outcome of patients having percutaneous coronary interventions with drug-eluting stents. Am J Cardiol. 2011;108(02):195-201.
- [Google Scholar]
- Obesity and cardiovascular thrombotic events in patients undergoing percutaneous coronary intervention with drug-eluting stents. Heart. 2009;95(19):1587-1592.
- [Google Scholar]
- Evidence for obesity paradox in patients with acute coronary syndromes: a report from the Swedish Coronary Angiography and Angioplasty Registry. Eur Heart J. 2013;34(05):345-353.
- [Google Scholar]
- MIG (Melbourne Interventional Group) Registry. Is there an obesity paradox after percutaneous coronary intervention in the contemporary era? An analysis from a multicenter Australian registry. JACC Cardiovasc Interv. 2010;3(06):660-668.
- [Google Scholar]
- Body mass index and bleeding complications after percutaneous coronary intervention: does bivalirudin make a difference? Am Heart J. 2010;159(06):1139-1146.
- [Google Scholar]
- Relation of body mass index to mortality among men with coronary heart disease. Am J Cardiol. 2010;106(03):297-304.
- [Google Scholar]
- Effect of obesity on short- and long-term mortality postcoronary revascularization: a meta-analysis. Obesity (Silver Spring). 2008;16(02):442-450.
- [Google Scholar]
- The impact of obesity on the short-term and long-term outcomes after percutaneous coronary intervention: the obesity paradox? J Am Coll Cardiol. 2002;39(04):578-584.
- [Google Scholar]
- The influence of body mass index on mortality and bleeding among patients with or at high-risk of atherothrombotic disease. Eur Heart J. 2009;30(07):857-865.
- [Google Scholar]
- Body mass index, periprocedural bleeding, and outcome following percutaneous coronary intervention (from the British Columbia Cardiac Registry) Am J Cardiol. 2009;103(04):507-511.
- [Google Scholar]
- Relation of body mass index to bleeding during percutaneous coronary interventions. Am J Cardiol. 2015;115(04):434-440.
- [Google Scholar]
- Absence of obesity paradox in Saudi patients admitted with acute coronary syndromes: insights from SPACE registry. Ann Saudi Med. 2014;34(01):38-45.
- [Google Scholar]
- Body mass index and acute and long-term outcomes after acute myocardial infarction (from the Harmonizing Outcomes With Revascularization and Stents in Acute Myocardial Infarction Trial) Am J Cardiol. 2014;114(01):9-16.
- [Google Scholar]
- Impact of body mass index on mortality in Swiss hospital patients with ST-elevation myocardial infarction: does an obesity paradox exist? Swiss Med Wkly. 2014;144:w13986.
- [Google Scholar]
- Relation between obesity and severity of coronary artery disease in patients undergoing coronary angiography. Am J Cardiol. 2006;97(09):1277-1280.
- [Google Scholar]
- Effects of obesity on lipid-lowering, anti-inflammatory, and antiatherosclerotic benefits of atorvastatin or pravastatin in patients with coronary artery disease (from the REVERSAL Study) Am J Cardiol. 2006;97(11):1553-1557.
- [Google Scholar]
- Inverse relationship between body mass index and coronary artery calcification in patients with clinically significant coronary lesions. Atherosclerosis. 2012;221(01):176-182.
- [Google Scholar]
- The relationship between C-reactive protein and atherosclerosis differs on the basis of body mass index: the Dallas Heart Study. J Am Coll Cardiol. 2012;60(13):1148-1155.
- [Google Scholar]
- Paradoxical preservation of vascular function in severe obesity. Am J Med. 2010;123(08):727-734.
- [Google Scholar]
- The obesity paradox and myocardial infarct size. J Cardiovasc Med (Hagerstown). 2007;8(09):713-717.
- [Google Scholar]
- Impact of body weight and extreme obesity on the presentation, treatment, and in-hospital outcomes of 50,149 patients with ST-Segment elevation myocardial infarction results from the NCDR (National Cardiovascular Data Registry) J Am Coll Cardiol. 2011;58(25):2642-2650.
- [Google Scholar]
- Gender-specific characteristics of atherosclerosis in menopausal women: risk factors, clinical course and strategies for prevention. Climacteric. 2007;10:16-20. (Suppl 2)
- [Google Scholar]
- Impact of obesity on disease-specific health status after percutaneous coronary intervention in coronary disease patients. Int J Obes Relat Metab Disord. 2004;28(08):1011-1017.
- [Google Scholar]
- Alexandra Kent Obesity and cardiovascular outcomes: a review. Eur Heart J Acute Cardiovasc Care. ;5(01):77-85.
- [Google Scholar]







