Translate this page into:
Predicting Coronary Artery Disease with Carotid Intima-media Thickness: Does Gender Matter
*Corresponding author: Anshu Kumar Jha, Department of Cardiology, Maharaja Krushna Chandra Gajapati Medical College and Hospital, Berhampur, Odisha, India akj2410@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Satpathy C, Mishra TK, Jha AK. Predicting Coronary Artery Dise ase with Carotid Intima-media Thickness: Does Gender Matter. Indian J Cardiovasc Dis Women. doi: 10.25259/IJCDW_7_2024
Abstract
Objectives:
Atherosclerosis is the leading cause of coronary artery disease (CAD) worldwide. The gold standard for diagnosing CAD is by doing coronary angiography but this is an invasive procedure. Carotid intima-media thickness (CIMT) is a non-invasive procedure which is suggested to correlate with CAD.
Materials and Methods:
It was a cross-sectional study of 87 subjects who underwent angiography and carotid ultrasound for CIMT. They were divided into male and female groups with or without angiographically proven CAD. Correlations were made between the CIMT and presence of CAD and between CIMT and severity of CAD. The presence of plaque and its association with CAD was also studied.
Results:
Mean value of CIMT was 0.865 mm and plaque was present in 30% of the cases. In males, the severity of CAD has association with CIMT but this was not found in female gender. CIMT does not correlate with the presence or absence of CAD in either gender but the values of CIMT correlate well with the severity of CAD. This means that, higher the CIMT value more the number of vessels affected on angiography and the value with best sensitivity and specificity (from this study) was 0.88 mm. However, this correlation of CIMT with severity of CAD was restricted to male gender as findings were insignificant for females. Furthermore, the presence, morphology, or echogenicity of plaque does not correlate with severity of CAD in either gender.
Conclusion:
Predicting CAD from CIMT value is still inconclusive and requires further studies to look for correlations.
Keywords
Coronary artery disease
Carotid intima-media thickness
Angiography
Gender
ABSTRACT IMAGE

INTRODUCTION
Atherosclerosis is a systemic, chronic inflammatory disorder usually involving multiple vascular territories in the same patient, with carotid and coronary artery plaque known to be closely related.[1] Coronary angiography (CAG) is gold standard for identifying the degree of coronary atherosclerosis. However, this invasive method is related with an uncommon side effect of morbidity, especially for the patients with inconstant hemodynamic variables. Thus, it is useful to explore non-invasive screening methods for diagnosing coronary artery disease (CAD) patients with high accuracy. There are studies which have linked atherosclerotic plaque features to carotid and coronary arteries.[2-4] Many cross-sectional studies have shown correlation between carotid intima-media thickness (CIMT) with the extent as well as severity of coronary atherosclerosis based on angiography.[3,4] The Kuopio ischemic heart disease study showed that there is 11% increase in risk of myocardial infarction with each 0.1 mm increase in CIMT outside its normal range (0.9 mm).[5] When the thickening of intima– media starts, it is commonly recognized as the beginning of development of atherosclerosis.[6,7] It is regarded as a marker for predicting early stages of atherosclerotic process and correlates well with the occurrences of cardiovascular outcomes.[8-10] A study done by Kablak-Ziembicka et al. concluded that CAD patients had high intima-media thickness (IMT) when compared to healthy controls and patients with more advanced CAD had higher IMT.[4] However, the numerical values of this study cannot be applied to both the genders. The previous studies have shown that men have larger CIMT values than women.[11] Thus, gender-adjusted CIMT shall better help to predict the likelihood of CAD (as proved on angiography). Although a significant association between IMT and development of CAD has been observed in many studies, exact role is yet to be established. Main reason is that there was no further prognostic value established by adding CIMT to the well-established risk factor score, such as Framingham Risk Score.[12]
Objectives
Thus keeping the above mentioned literature in mind, this study will be undertaken with following objectives-
To measure the CIMT and correlate it with the angiographic finding in CAD patients
To see the presence and morphology of plaque in the carotid artery, presence or absence of thrombus and correlate with the severity of angiographic findings in CAD patients
To see the difference (if any) in the predictive value of CIMT in men versus women for CAD (as proved on angiography).
MATERIALS AND METHODS
This study was a cross-sectional study done over a period of 2 months and was approved by the Institutional Ethical Committee (Memo no. 1295). The sample size was be calculated using the formula N = Z2 × P(1-P)/d2 where N represents sample size, Z is level of confidence of the study (here taken to be 95%), P represents expected prevalence in the population, and d is the precision (here taken as 5%, i.e., 0.05) with ages ranging from 20 to 80 years. Our sample size came out to be 85. All eligible patients underwent CAG for suspected CAD. Following this, they were divided into two groups – Group I for males and Group II for females. Further, these groups were subdivided into IA representing angiographically confirmed CAD and IB consisting of patients with no significant lesion on angiography. Similar, subdivisions of group II were made as IIA and IIB. Significant lesion was taken as ≥1 lesion with a decrease of >50% in luminal diameter of a coronary artery. Based on CAG, the CAD was divided into five groups and labeled as single-vessel disease, double-vessel disease (DVD), triple-vessel disease (TVD), left main disease (LMD), or normal. B-mode ultrasound measurement of the CIMT was done of patients as a blind study. The radiologist was unaware of the CAG findings. A standardized ultrasound technique was employed, using a GE Logiq E9 ultrasound model. The patient was then kept in supine position with neck slightly extended following which the transducer frequency was set at 11 MHz and depth at 4 mm (was adjusted if required) for all patients. Measurement of the intima-media thickness was carried out at the optimum angle of interrogation (OAI) (as per American Society of Echocardiography guidelines) which allowed visualization of the flow tip divider, the common carotid artery (CCA), external carotid artery (ECA), and internal carotid artery (ICA) from a single selected angle of the carotid arteries at the bifurcation. Doppler study was used to verify the identification of the ECA and ICA. The CIMT was measured when the two echogenic lines, representing the lumenintima interface and the media-adventitia interface, could be seen visualized for a minimum length of 1 cm from carotid bifurcation. Measurements of the CIMT were done manually, using the caliper markers on the ultrasound unit. The CIMT at the OAI was measured bilaterally as the area of maximum thickness at the near and far walls of the CCA (1 cm from the bifurcation), at the bifurcation and ICA within 1 cm from the bifurcation (a total of 12 sites). In cases where calcified plaque obscured the IMT, one wall was measured; the thickest measurement in each segment was imaged and recorded as the final measurement. The mean maximum IMT was recorded as the CIMT. The CIMT was calculated as the average of 12 sites for all subjects, using the Excel program for Windows XP. A mean value for the CIMT of above 0.8 mm was classified as increased thickness.[13] A focal wall thickness distinct from the adjacent boundary measuring ≥1.5 mm was considered as plaque.[14] Its presence, and morphology (focal/diffuse) shall be noted. If the plaque was seen throughout the scanned area then it was regarded as diffuse and if it was localized protuberance, then it was considered as focal. Presence or absence of thrombus shall also be documented. Subjects with overt renal, thyroid, or liver disease were excluded from the study. Subjects who were already on cholesterol lowering therapy for at least 6 months and diabetic patients on pioglitazone therapy for >12 weeks were excluded from the study as these drugs have shown to decrease the CIMT.[15,16] Other exclusions for consideration were related to technical issues which did not allow for measurement of the CIMT, including poor imaging with limited boundary visualization or when there was anatomical constraints, either a high carotid artery bifurcation or a short, thick neck and where more than two segments were not visualized. Data were entered in the table and statistical analysis was done.
Statistical analysis
The distribution of major cardiovascular risk factors was compared between men who had CAD versus who did not have CAD and women who had CAD versus who did not have CAD with Pearson’s Chi-square test. Differences in the mean CIMT value was evaluated by one-way ANOVA (Analysis Of Variance) for the four groups and verified by Tukey’s test for multiple comparisons of means. Receiver operating characteristic (ROC) curve was drawn to see the best cutoff point of CIMT with highest probability of CAD in men and women separately. For the cutoff point established by ROC, sensitivity and specificity was calculated to see the discriminating power of mean CIMT in detection of CAD in men and women separately. The collected data were presented in the form of tables and figures. Obtained data were analyzed using the Statistical Package for the Social Sciences 20.0 version software. P < 0.05 was taken as significant.
Implication
CIMT is a very basic ultrasonographic study which is handy and can be performed even at peripheral health centers. This study shall help us understand the predictive power of CIMT for a patient in whom CAD is suspected. It shall also be helpful in women as they often present with atypical symptoms such as fatigue, anxiety, nausea, indigestion, and upper back pain and have equivocal result from other non-invasive tests. Due to these reasons, the cardiac health in female gender is undermined. We less likely suspect cardiovascular disease in them, due to which they receive fewer emergency treatments than men.[17] Although there are other non-invasive modalities for assessing CAD, they have their own limitations. Exercise Treadmill test has suboptimal sensitivity and there is wide variability of result. Echocardiography is a good modality but until unless there is a wall motion abnormality, suspicion of CAD is less. Cardiac computed tomography has a risk of exposure to radiation. Rest imaging modalities such as nuclear scan, cardiac magnetic resonance imaging, and positron emission test are costly an non available at all centers.
RESULTS
A total of 87 participants were considered for this study of which 77% were male and 23% were female. Age distribution of the subjects is shown in Figure 1 (mean age – 56.77 ± 13.59 years). Total subjects in group IA were 59, in IB were 8, in IIA were 13, and in IIB were 7. Distribution of the subjects on the basis of smoking, alcohol addiction, hypertension, and diabetes mellitus is shown in Figure 2. There was no statistical significant correlation between these studied factor and presence or absence of CAD. The average hemoglobin on the study population was 13.16 (±1.67) g%. The definitive diagnosis along with the total number of patients with that diagnosis is shown in Figure 3. The average CIMT of all the 87 subjects was 0.869 mm. Mean CIMT among male subjects was – 0.865 mm and among female subject was 0.832 mm. Plaque was present in 30 (35%) cases out of which 19 (63%) were focal and 11 (37%) were diffuse. Among all the plaque, 17 (57%) were hyperechoic, 12 (40%) were hypoechoic, and 01 (3%) was isoechoic [Figure 4]. Thrombus was present in only two out of 87 cases (2.2%). The angiographic findings of the studied subject are shown in Figure 5. The mean CIMT values in group IA, IB, IIA, and IIB were – 0.883 mm, 0.848 mm, 0.833 mm, and 0.832 mm, respectively [Figure 6]. On using Kruskal–Wallis test for association of CIMT with the severity of CAD (normal CAG being least severe and LMD being most severe), it was found that in males, the severity of CAD has association with CIMT but this was not found in female gender. The mean value of CIMT across the five groups of CAG is shown in Figure 7.
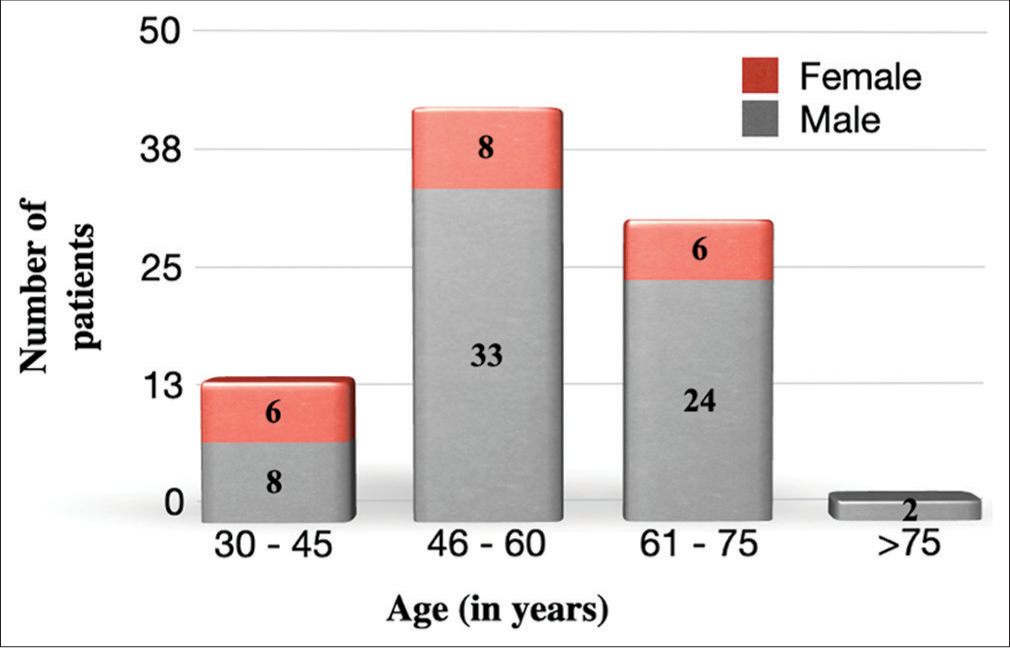
- Age distribution of all subjects gender wise.

- Subject distribution based on various risk factors. IA and IIA: Angiographically confirmed CAD in males and females respectively, IB and IIB: Angiographically confirmed no significant lesion in males and females respectively.

- Diagnosis of patients. (ASMI: Anteroseptal myocardial infarction, AWMI: Anterior wall myocardial infarction, CCS: Chronic coronary syndrome, ILMI: Inferolateral myocardial infarction, IPWMI: Inferoposterior wall myocardial infarction, IWMI: Inferior wall myocardial infarction, LWMI: Lateral wall myocardial infarction, NSTEACS: Non-ST segment elevated acute coronary syndrome, NSTEMI: Non-ST segment elevated myocardial infarction, RVMI: Right ventricular myocardial infarction, UA: Unstable angina, STEMI: ST segment elevated myocardial infarction, ACS: Acute coronary syndrome, CCS: Chronic coronary syndrome, PWMI: Posterior wall myocardial infarction).

- Ultrasonographic image of carotid artery showing an isoechoi c plaque. Bluish white arrow shows an isoechoic plaque.

- Distribution of patients according to angiographic findings. N: Total subject, SVD: Single vessel disease, DVD: Double vessel disease, TVD: Triple vessel disease, LMD: Left main disease.

- Relation between mean carotid intima-media thickness (CIMT) values and various coronary artery disease (CAD) groups. IA and IIA: Angiographically confirmed CAD in males and females respectively, IB and IIB: Angiographically confirmed no significant lesion in males and females respectively.

- Relation between mean carotid intima-media thickness (CIMT) values a nd various groups as per angiography. (SVD: Single vessel disease, DVD: Double vessel disease, TVD: Triple vessel disease, LMD: Left main disease).
It was observed that CIMT was significantly associated with severity of the disease, with highest severity having the lowest CIMT, which was an unexpected finding (Kruskal– Wallis-H = 11.604, df = 4, P = 0.021). The greatest difference of mean CIMT was obtained between LMD and DVD, followed by LMD and TVD. When performed in separate genders, CIMT was observed to be significantly associated with severity of the disease in males with highest severity having the lowest CIMT (Kruskal–Wallis-H = 10.311, df = 4, P = 0.035). In females, the association was not significant. CIMT was not found to be significantly associated with presence or absence of CAD, whether as a whole or when tested gender wise. The severity of disease was not found to be significantly associated with either presence, or morphology or echogenicity of plaque. The ROC curve to see the best cutoff point of CIMT with highest probability of CAD in men and women is shown in Figures 8 and 9. In men, CIMT value of 0.84 mm could predict the presence of CAD with sensitivity of 54% and specificity of 75%. Area under curve (AUC) was 0.537 but from Figure 9, it is clear that there is no cutoff value of mean CIMT which could predict the presence of CAD in women. AUC was 0.489.

- Receiver operating characteristic (ROC) curve for predictability of coronar y artery disease by carotid intima-media thickness in males.

- Receiver operating characteristic (ROC) curve for predictability of coronary arte ry disease by carotid intima-media thickness in females.
DISCUSSION
CAD is a major cause of mortality and morbidity in the developed as well as in developing countries like India. The incidence is rising and atherosclerosis is the major cause of it. Using ultrasonography helps us to determine IMT in a very accurate way with least costing. This method also has a good clinical value in the screening of patients with CAD. However, having said that till date no scoring system has ever incorporated CIMT value in its scoring system pertaining to CAD prediction. This occurs due to various studies showing inconsistent results with respect to CIMT predicting CAD and a very few studies have gone even further and compared the gender differences in this regard.
The mean age in the study group was 56.7 ± 13.59 years, and males constituted 77% and females 23% of this population. The mean age in study conducted by Jadhav and Kadam was 52.8 and males contributed to 65% of their total subjects and rest 35% by females.[18] In the ARIC study, mean age was 56 years whereas, in Rotterdam study, it was 70 years.[19,20] In our study, 50.5% of patients were smokers as compared to 26.5% in Rotterdam study.20] In our study, 43.6% of patients had diabetes which was comparable to study by Jadhav and Kadam where 51.5% of patients had diabetes.[18] This was in contrast to the in the ARIC and Rotterdam study where it was only 9% and 10.5%, respectively.[19,20] This shows the rampant prevalence of diabetes in our country labeling it as the diabetic capital of the world. In our study, 42.5% of patients were hypertensive as compared to 18.2% in ARIC study and 32% in Rotterdam Study.[19,20] This high percentage in our study could be due to biases in selecting the sample which included only those patients in whom CAD was suspected. About 23% of our study population were consuming alcohol and all of them were male. There was no correlation of any of these factors with CIMT. This result was in contrast with respect to study done by Puato et al., Sadeghi et al., and Mitsuhashi et al. where they had shown a positive correlation between CIMT – smoking and CIMT – hypertension and CIMT – diabetes.[21-23] This difference could be due to the small sample size in our study. Unlike the “STRATEGY” study, there was no significant correlation seen between alcohol consumption and CIMT.[24] In our study, CIMT was not found to be significantly associated with the presence or absence of CAD when we compared it either as a whole or gender wise. This was against the finding of study done by Nambi et al.[25] In another study done by Verma et al., it was found that CIMT was not related to the severity of CAD.[26] As there are controversial results with regard to CIMT predicting the presence or absence of CAD, a meta-analysis of 22 articles done by Liu et al. claimed that “Until now, the diagnostic role of IMT for CAD prediction is controversial.”[27] The exact value of CIMT which could predict the presence or absence of CAD was 0.84 mm (only for males). In females, no such cutoff point could be established. The sensitivity and specificity of this value were 54% and 75%, respectively (AUC – 0.53). In the study by Zhang et al., where they had taken cutoff value of IMT was 1 mm, the sensitivity and specificity were 31.91% and 90.52%, respectively.[28] Murphy et al. found sensitivity and specificity of carotid IMT at ≥ 0.9 mm 50% and 96%, respectively.[29] Study by Matsushima et al., where cutoff taken was 0.88 mm of IMT, gave 88% sensitivity and 90% specificity for prediction of CAD[30] whereas meta-analysis by Liu et al. gave a diagnostic sensitivity and specificity of 68% and 70%, respectively. The corresponding AUC was 0.74.[27] Our study showed that there is an association of CIMT with the severity of CAD. This was in concordance with the study done by Kablak-Ziembicka et al.[4] where they found that increased CIMT was positively and linearly related to CAD as subjects with a greater number of vessel involvement showed greater increase in CIMT. The study by Wani et al.[31] also showed that CIMT can be used as a marker for assessing the severity of CAD on CAG. Although these findings are in concordance with our findings, the uniqueness of our study was that the relation was restricted to male gender only. None of the above mentioned studies had done a gender wise analysis to predict this difference.
In our study, the severity of CAD was not found to be associated with either presence, or morphology or echogenicity of plaque. This was against the findings of the Multi-Ethnic Studies of Atherosclerosis done by Gepner et al. and Mitchell et al.[32,33] This difference in finding could be attributed to small sample size of our study.
Limitations
Although this study does not give a very robust evidence of the findings due to small sample size, it helps to generate a hypothesis for other larger multi-centric and multiethnic studies. As it was a single-center study, so this may not be representational to the other CAD population. The time period of the study was not long enough. Furthermore, as it was a cross-sectional study, the follow-up of the patients to see the change in CIMT could not be done which would have better correlated with their disease.
CONCLUSION
Based on the findings of this study, we conclude that CIMT does not correlate with the presence or absence of CAD in either gender but the values of CIMT correlate well with the severity of CAD. This means that, higher the CIMT value more the number of vessels affected on angiography and the value with best sensitivity and specificity (from this study) was 0.88 mm. However, this correlation of CIMT with severity of CAD was restricted to male gender as findings were insignificant for females. Furthermore, the presence, morphology, or echogenicity of plaque does not correlate with severity of CAD in either gender. Due to various limitations stated above, further studies with larger sample population over a longer period are suggested to better understand this correlation.
Ethical approval
The research/study approved by the Institutional Review Board at MKCG Medical College and Hospital, number 1259, dated September 13, 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Audio summary available at
Financial support and sponsorship
Nil.
References
- Acute Coronary Syndromes, Plaque Vulnerability, and Carotid Artery Disease: The Changing Role of Atherosclerosis Imaging. J Am Coll Cardiol. 2003;42:1033-6.
- [CrossRef] [PubMed] [Google Scholar]
- Carotid Artery Plaque and Progression of Coronary Artery Calcium: The Multi-ethnic Study of Atherosclerosis. J Am Soc Echocardiogr. 2013;26:548-55.
- [CrossRef] [PubMed] [Google Scholar]
- Correlation of Coronary Plaque Phenotype and Carotid Atherosclerotic Plaque Composition. Am J Med Sci. 2011;342:480-5.
- [CrossRef] [PubMed] [Google Scholar]
- Association of Increased Carotid Intimamedia Thickness with the Extent of Coronary Artery Disease. Heart. 2004;90:1286-90.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasonographically Assessed Carotid Morphology and the Risk of Coronary Heart Disease. Arterioscler Thromb. 1991;11:1245-9.
- [CrossRef] [PubMed] [Google Scholar]
- The Pathogenesis of Atherosclerosis: A Perspective for the 1990s. Nature. 1993;362:801-9.
- [CrossRef] [PubMed] [Google Scholar]
- Atherosclerosis Imaging as a Benchmark in the Development of Novel Cardiovascular Drugs. Curr Opin Lipidol. 2007;18:613-21.
- [CrossRef] [PubMed] [Google Scholar]
- Carotid Intimalmedial Thickness is Related to Cardiovascular Risk Factors Measured from Childhood Through Middle Age: The Muscatine Study. Circulation. 2001;104:2815-9.
- [CrossRef] [PubMed] [Google Scholar]
- Carotid-Artery Intima and Media Thickness as a Risk Factor for Myocardial Infarction and Stroke in Older Adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med. 1999;340:14-22.
- [CrossRef] [PubMed] [Google Scholar]
- Carotid Wall Thickness and Stroke Risk in Patients with Asymptomatic Internal Carotid Stenosis. Atherosclerosis. 2010;210:452-7.
- [CrossRef] [PubMed] [Google Scholar]
- Carotid Intima-media Thickness: Risk Assessment and Scanning Protocol. Eur Heart J. 2022;23:916-8.
- [CrossRef] [PubMed] [Google Scholar]
- Incremental Predictive Value of Vascular Assessments Combined with the Framingham Risk Score for Prediction of Coronary Events in Subjects of Low-intermediate Risk. Postgrad Med J. 2008;84:153-7.
- [CrossRef] [PubMed] [Google Scholar]
- Intima Media Thickness As a Surrogate Marker for Generalised Atherosclerosis. Cardiovasc Drugs Ther. 2002;16:341-51.
- [CrossRef] [PubMed] [Google Scholar]
- The Predictive Value of Carotid Ultrasonography With Cardiovascular Risk Factors-A “SPIDER” Promoting Atherosclerosis. Front Cardiovasc Med. 2021;8:706490.
- [CrossRef] [PubMed] [Google Scholar]
- Carotid Plaque Regression Following 6-Month Statin Therapy Assessed by 3T Cardiovascular Magnetic Resonance: Comparison with Ultrasound Intima Media Thickness. J Cardiovasc Magn Reson. 2011;13:37.
- [CrossRef] [PubMed] [Google Scholar]
- Pioglitazone Decreases Carotid Intima-media Thickness Independently of Glycemic Control in Patients with Type 2 Diabetes Mellitus: Results from a Controlled Randomised Study. Circulation. 2005;111:2525-31.
- [CrossRef] [PubMed] [Google Scholar]
- Women's Health In: Jameson JL, ed. Harrison's Principles of Internal Medicine (20th ed). United States: McGraw Hill Education; 2018. p. :2823-8.
- [Google Scholar]
- Carotid Intima-media Thickness As an Independent Predictor of Coronary Artery Disease. Indian Heart J. 2001;53:458-62.
- [Google Scholar]
- Arterial Wall Thickness is Associated with Prevalent Cardiovascular Disease in Middle Aged Adults. The Atherosclerosis Risk in Communities (ARIC) Study. Stroke. 1995;26:386-91.
- [CrossRef] [PubMed] [Google Scholar]
- Common Carotid Intima Media Thickness and Risk of Stroke and Myocardial Infarction. Circulation. 1997;96:1432-7.
- [CrossRef] [PubMed] [Google Scholar]
- Increase in Carotid Intima-Media Thickness in Grade I Hypertensive Subjects: White-Coat Versus Sustained Hypertension. Hypertension. 2008;51:1300-5.
- [CrossRef] [PubMed] [Google Scholar]
- Is Common Carotid Intima Media Thickness An Independent Predictor for Coronary Artery Disease? ARYA Atheroscler J. 2005;1:5-8.
- [Google Scholar]
- Coronary Artery Disease and Carotid Artery Intima-media Thickness in Japanese Type 2 Diabetic Patients. Diabetes Care. 2002;25:1308-12.
- [CrossRef] [PubMed] [Google Scholar]
- Association between Alcohol Consumption and Carotid Intima-Media Thickness in a Healthy Population: Data of the STRATEGY Study (Stress, Atherosclerosis and ECG Study) Eur J Clin Nutr. 2010;64:1199-206.
- [CrossRef] [PubMed] [Google Scholar]
- Carotid Intima-media Thickness and Presence or Absence of Plaque Improves Prediction of Coronary Heart Disease Risk: The ARIC (Atherosclerosis Risk in Communities) Study. J Am Coll Cardiol. 2010;55:1600-7.
- [CrossRef] [PubMed] [Google Scholar]
- Carotid Intima-media Thickness Predicted the Presence but not the Severity or Complexity of Coronary Artery Disease in a South Asian Population. Clin Investig Arterioscler. 2022;34:183-92.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic Role of Carotid Intima-Media Thickness for Coronary Artery Disease: A Meta-Analysis. Biomed Res Int. 2020;2020:9879463.
- [CrossRef] [PubMed] [Google Scholar]
- Is Carotid Intima-media Thickness as Predictive as Other Noninvasive Techniques for the Detection of Coronary Artery Disease? Arterioscler Thromb Vasc Biol. 2014;34:1341-5.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic Accuracy of Carotid Intima Media Thickness in Predicting Coronary Plaque Burden on Coronary Computed Tomography Angiography in Patients with Obstructive Sleep Apnoea. J Cardiovasc Comput Tomogr. 2017;11:227-33.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship of Carotid Intima-Media Thickness, Pulse Wave Velocity, and Ankle Brachial Index to the Severity of Coronary Artery Atherosclerosis. Clin Cardiol. 2004;27:629-34.
- [CrossRef] [PubMed] [Google Scholar]
- Carotid Intima-media Thickness as a Marker for Assessing the Severity of Coronary Artery Disease on Coronary Angiography. Int J Res Med Sci. 2018;6:1283-7.
- [CrossRef] [Google Scholar]
- Comparison of Carotid Plaque Score and Coronary Artery Calcium Score for Predicting Cardiovascular Disease Events: The Multiethnic Study of Atherosclerosis. J Am Heart Assoc. 2017;6:e005179.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasound Carotid Plaque Features, Cardiovascular Disease Risk Factors and Events: The Multi-Ethnic Study of Atherosclerosis. Atherosclerosis. 2018;276:195-202.
- [CrossRef] [PubMed] [Google Scholar]







