Translate this page into:
Incidence of Cardiovascular Events and Mortality in COVID-19 Patients Admitted in NIMS Intensive Care Unit during Second Wave
N. Srikanth, DNB, DM Department of Cardiology, Nizam Institute of Medical Sciences Hyderabad, Telangana 500082 India nakka.srikanth268@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Prevalence of pulmonary thromboembolism (PTE) is very high when we compare the coronavirus disease 2019 positive patients with the other patients who are admitted in intensive care unit for other different infection. Thorough evaluation of the different causative factors for PTE should be better evaluated and prevention can be tried accordingly. Incidence of subclinical PTE that can give rise to future cardiac disease needs to be studied and plan of action can be done accordingly. Newer modalities of detecting PTE using non-invasive or simple invasive techniques need to be investigated to cope up in pandemic situation.
Keywords
cardiovascular events
COVID-19
mortality
pulmonary thromboembolism
- Abstract Image
Abstract Image
Introduction
Coronavirus disease 2019 (COVID-19) though initially found as a respiratory system disease. It was recognized to interact and affect the cardiovascular system causing myocardial damage and endothelial dysfunction usually through the angiotensin-converting enzyme 2 receptor.1 2 3 4 In fact, cardiac damage sometimes noted even without having clinical features of respiratory disease. Respiratory symptoms are worse in COVID-19 affected patients with preexisting cardiac ailments. However, new-onset cardiac ailments were also seen commonly.5 6 7 8 Cardiovascular events due to COVID-19 are of wide variety and needs to be studied in detail and mortality can be reduced to a greater extent if detected earlier.
In our study, we had evaluated incidence of pulmonary thromboembolism (PTE), effect of PTE and various cardiovascular diseases on the mortality in COVID-19 patients admitted in intensive care units during May 01,2021 to June 15,2021 in Nizam Institute of Medical Sciences (NIMS) hospital based on their gender preference.
Materials and Methods
We had carried a study in COVID-19 pneumonia patients admitted in NIMS intensive care unit between May 01,2021 and June 15,2021. The study was accepted by the ethics committee of NIMS Hospital. During that period 58 patients got admitted in intensive care. We had included only patients admitted in intensive unit anytime during their hospital stay, who are on invasive or noninvasive ventilation or high-flow nasal cannula. However, we have excluded patients less than 15 years age, who are known case of chronic kidney disease, coronary artery disease, cerebrovascular disease, and collagen vascular disease and also who were at ward stay only. We had enrolled the subjects into the study as per inclusion and exclusion criteria. Our aim is to see the occurrence and prognostication of cardiovascular manifestations in COVID-19 patients. We aimed to see PTE, acute coronary syndrome, and myocarditis as cardiovascular manifestations.
We did all blood investigations including D-dimer levels, ferritin, electrocardiogram (ECG), two-dimensional (2D) echo and high-resolution computed tomography (HRCT) chest, and CT pulmonary angiogram (CT PA) whenever needed or possible to do. CT severity index was given depending on the percentage of involvement of five lobes of lung—score as 0 if no lung involvement, less than 5%;score 1, 5 to 25%; score 2, 26 to 49%; score 3, 50 to 74%; score 4, more than or equal to 75% involvement; and score as 5, with minimum score of 0 and maximum as 25. PTE was diagnosed based on CT PA or in patients who had right atrium (RA) and right ventricle (RV) dilatation on 2D echo with CT severity score less than 14 (so that cause for RA and RV is not due to pulmonary manifestation of the COVID-19). However, 2D echo cannot rule out PTE or rule in PTE completely in patients who did not undergo CT PA, but study being done in pandemic, certain 2D echo features are taken into account to consider PTE. Other cardiac manifestations were detected by ECG and 2D echo finding with biomarkers. Levels of D-dimer estimation were done in every patient and analyzed its prognostic significance on mortality.
Statistical Analysis
For statistical analysis, we used Statistical Package for Social Sciences [SPSS] for Windows version 22.0 (Released 2013. IBM Corp., Armonk, New York, United States). Descriptive analysis of all the explanatory and outcome parameters was done using frequency and proportions for categorical variables and in mean and standard deviation for continuous variables. Mann–Whitney U test was used to compare different diagnostic parameters based on gender and survival status of study patients. Chi-squared test was used to compare study variables in categorical distribution based on gender and survival status of study patients. The level of significance was set at p < 0.05.
Results
A total of 58 patients were enrolled in the study, as per inclusion and exclusion criteria among which 45 (77.6%) were males and 13 (22.4%) were females (Table 1). The average age of enrolled participants was 53.03 years (±15.58 years). It was observed that 17 (29.3%) people aged between 25 and 40 years, 22 people aged (37.9%) between 41 and 60 years, and 19 people (32.8%) aged more than 60 years.
|
Variable |
Category |
n |
% |
|---|---|---|---|
|
Age |
25–40 years |
17 |
29.3% |
|
41–60 years |
22 |
37.9% |
|
|
> 60 years |
19 |
32.8% |
|
|
Mean |
SD |
||
|
Mean |
53.03 |
15.58 |
|
|
Range |
25–82 |
||
|
Median |
54.50 (39–65) |
||
|
Sex |
Males |
45 |
77.6% |
|
Females |
13 |
22.4% |
|
Abbreviation: SD, standard deviation.
We divided the study population, depending on the survival status, into survivors and nonsurvivors and compared the demographic and investigational parameters in these two groups (Table 2).
|
Parameters |
Survived |
Expired |
p-Value |
||
|---|---|---|---|---|---|
|
Median |
IQR |
Median |
IQR |
||
|
Age(y) |
50.5 |
38–61 |
55.5 |
41–70 |
0.19 |
|
Hb |
13.1 |
11.2–13.7 |
11.4 |
9.6–13.95 |
0.41 |
|
TLC |
12300.0 |
9800–17200 |
14400.0 |
9800–25200 |
0.29 |
|
PLT |
202500.0 |
150000–270000 |
150000.0 |
110000–230000 |
0.10 |
|
Urea |
51.5 |
34–78 |
71.0 |
60.5–152 |
0.009a |
|
Creatinine |
0.8 |
0.66–1.4 |
1.4 |
1.25–3.6 |
0.003a |
|
D-dimer |
642.0 |
185–2391 |
2060.0 |
731.5–4045 |
0.02a |
|
Ferritin |
736.5 |
517–1493 |
1600.5 |
664.6–2027 |
0.10 |
|
IL-6 |
21.6 |
8.49–77.2 |
106.9 |
78.94–271.63 |
<0.001a |
|
RBS |
139.0 |
139–257 |
139.0 |
139–167.5 |
0.61 |
|
NT-proBNP |
326.5 |
65–1725 |
1552.5 |
407–3450.5 |
0.01a |
|
HRCT chest CTSI |
14.0 |
10–20 |
22.0 |
19–22 |
<0.001a |
Abbreviations: CTSI, computed tomoraphy severity index; Hb, hemoglobin; HRCT, high-resolution computed tomography; IL-6, interleukin-6; IQR, interquartile range; PLT, platelet; RBS, random blood sugar; TLC, total leukocyte count.
It was noticed that patients who survived had mean creatinine of 0.8 mg/dL (with p-value of 0.03 [significant]) compared with patients who were deceased had mean creatinine of 1.4 mg/dL. Similarly, patients survived had mean blood urea of 51.5 mg/dL (p-value 0.009 [significant]) compared with patients deceased was had mean blood urea of 71 mg/dL (Table 2).
On analysis of data, it is found that in patients studied who were deceased had mean interleukin-6 (IL-6) value of 106.9 compared with patients who were survived had mean IL-6 of 21.6 with p-value of < 0.001; hence, it was observed that patients with low IL-6 values had better outcome. 1) Similarly, CTSI of 14/25 in survivors was observed, and in non survivors was 22/25, which is found to be statistically significant (p < 0.001). (Table 2).
Most important prognostic marker D-dimer showed statistical significance of p-value 0.02, with survivors mean of 642 compared with nonsurvivors mean of 2060 mg/dL (Table 2).
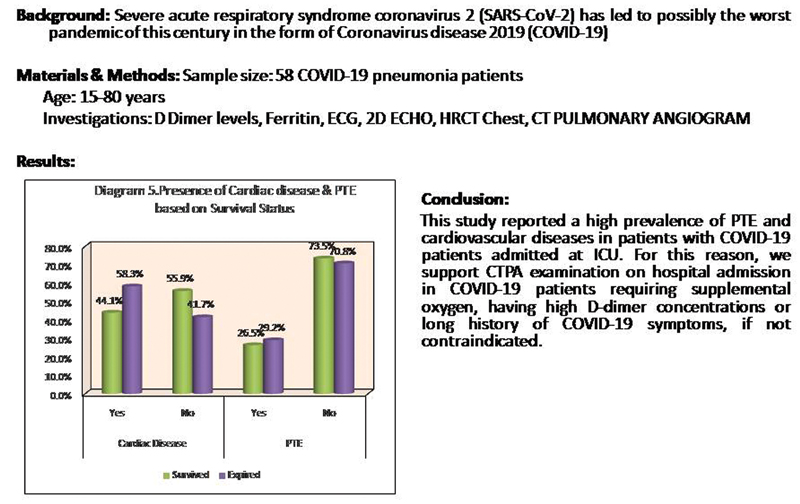
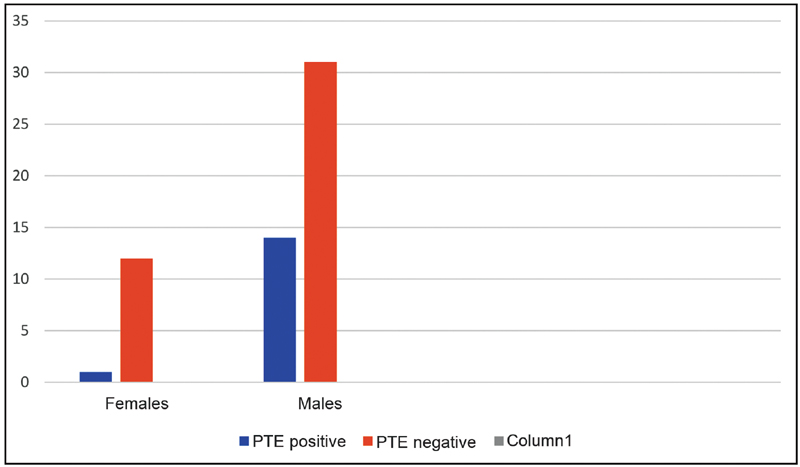
In the study population of 58 patients, one female patient (7.66%) and 14 male patients (31.1%) were found to have PTE with p-value of 0.08 with trend of more PTE in males compared with females, with overall incidence of PTE being 24.13% (15) in NIMS intensive care unit during COVID-19 infection hospitilisation during second wave (Fig. 1).
-
Fig. 1 Gender difference of pulmonary thromboembolism (PTE) in coronavirus disease 2019 patients.
Fig. 1 Gender difference of pulmonary thromboembolism (PTE) in coronavirus disease 2019 patients.
In our study, it was found that 7 (53.84%) out of 13 females were found to have some cardiac illness and 21 (46.66%) out of 45 males were found to have some cardiac illness during hospitalization with overall incidence of 48.27%, with p-value 0.6 being insignificant, observed to have no gender preference (Fig. 2).2

-
Fig. 2 Gender-wise distribution in presence of cardiac disease and pulmonary thromboembolism (PTE).
Fig. 2 Gender-wise distribution in presence of cardiac disease and pulmonary thromboembolism (PTE).
Cardiac disease is found in total of 29 patients (50%) of patients studied with features in favor of right heart failure in 23 patients, myocardial infarction and myocarditis in 6 patients (Table 3). Cardiovascular manifestations when correlated with the survival status found be insignificant (0.56) implying no mortality difference whether patient had cardiac disease or not (Table 4). Similarly, presence of PTE does not show any statistical significance (p value 0.82) on mortality (survivors vs non survivors 26.5% vs 29.2% respectively) (Table 4).
|
Variable |
Category |
Survived |
Expired |
p-Value |
||
|---|---|---|---|---|---|---|
|
n |
% |
n |
% |
|||
|
2D echo |
RA RV dilation |
12 |
35.3% |
11 |
45.8% |
0.56 |
|
Hypokinesia |
3 |
8.8% |
3 |
12.5% |
||
|
Normal |
19 |
55.9% |
10 |
41.7% |
||
Abbreviations: 2D echo, two-dimensional echocardiography; RA, right atrium; RV, right ventricle.
|
Variable |
Category |
Survived |
Expired |
p-Value |
||
|---|---|---|---|---|---|---|
|
n |
% |
n |
% |
|||
|
Cardiac disease |
Yes |
15 |
44.1% |
14 |
58.3% |
0.29 |
|
No |
19 |
55.9% |
10 |
41.7% |
||
|
PTE |
Yes |
9 |
26.5% |
7 |
29.2% |
0.82 |
|
No |
25 |
73.5% |
17 |
70.8% |
||
Abbreviation: PTE, pulmonary thromboembolism.
Discussion
Acute respiratory distress syndrome is the main cause of death in COVID-19 patients. Even though COVID-19 is considered as respiratory disease, it was found that cardiac illness was also one of the main causes of death.9
In one of Chinese study, mortality rate of up to 37% is seen mainly due to COVID-19-related heart diseases.10 Another study in United States states that world mortality due to COVID-19 in ICU ranged from 20 to 62% and especially in mechanically ventilated patients it is 60 to 97%.11 In one New York study, death rate in mechanically ventilated patients is as high as 88.1%.12 Similarly, in our study it was found that mortality due to various cardiac illness is up to 50%, which was seen in 29 people out of 58 people who were admitted in NIMS Hospital ICU, during second wave of COVID-19.
It was observed that major cause of mortality is because of cardiovascular implications in different studies. In one retrospective study in Wuhan in 2020, out of 187 patients, 35% had cardiovascular comorbidities in the form of coronary artery disease, cardiomyopathy, and PTE.9 Another study in Italy, out of 1,591 patients, 21% had cardiovascular disease and 17% had PTE.10 Likewise in New York, out of critically ill 251 patients 19% had cardiovascular disease and 16% had PTE.11 Similarly, in our study various cardiovascular disease is seen in 50% population like myocarditis (3 patients), myocardial infarction (3 patients), and right heart failure with or without PTE (23 patients). Cardiovascular manifestations when correlated with the survival status were found to be insignificant (0.56) implying no mortality difference whether patient had cardiac disease or not. In our study of 58 patients, one female patient (7.66%) and 14 male patients (31.1%) were found to have PTE with p-value of 0.08 with trend of more PTE in males compared with females, with overall incidence of PTE being 24.13% (15) in NIMS intensive care unit during COVID-19 second wave.
D-dimer was one such marker predicting the mortality in high risk COVID-19 cases. D-dimer is a fibrin degradation product and its main utility is in the diagnosis and management of thrombotic disorders. Several studies have been conducted to study the association between initial D-dimer measurements and disease severity and outcome. In one Chinese study, D-dimer value of more than 2 µg/mL on admission was associated with high mortality similar to one Indian study where optimal cutoff was shown for hospitalization requiring intensive care as 1.44 µg/mL and cutoff for mortality as 2.01 µg/mL.13 In our study, D-dimer showed statistical significance of p-value of 0.02, with survivors mean of 642 mg/dL compared with nonsurvivors mean of 2060 mg/dL.
Conclusion
Prevalence of PTE is very high when we compare the COVID-19 positive patients with the other patients who are admitted in intensive care unit for other different infection. Thorough evaluation of the different causative factors for PTE should be better evaluated and prevention can be tried accordingly. Incidence of subclinical PTE that can give rise to future cardiac disease needs to be studied and plan of action can be done accordingly. Newer modalities of detecting PTE using noninvasive or simple invasive techniques need to investigated to cope up in pandemic situation.
Conflict of Interest
None declared.
References
- Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061-1069.
- [Google Scholar]
- Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497-506. (10223):
- [Google Scholar]
- SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(02):271-280.e8.
- [Google Scholar]
- Angiotensin-converting enzyme 2 (ACE2) is a key modulator of the renin angiotensin system in health and disease. Int J Pept. 2012;2012:256294.
- [Google Scholar]
- Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5(07):819-824.
- [Google Scholar]
- Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. Int J Infect Dis. 2016;49:129-133.
- [Google Scholar]
- Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020;109(05):531-538.
- [Google Scholar]
- Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5(07):811-818.
- [Google Scholar]
- Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180(07):934-943. Epub20200314.
- [Google Scholar]
- Covid-19 in critically ill patients in the Seattle region - case series. N Engl J Med. 2020;382(21):2012-2022.
- [Google Scholar]
- Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323(20):2052-2059. Epub20200423.
- [Google Scholar]
- D-dimer level is a useful predictor for mortality in patients with COVID-19: analysis of 483 cases. Diabetes Metab Syndr. 2020;14(06):2245-2249.
- [Google Scholar]







