Translate this page into:
Retrograde Percutaneous Intervention of Chronic Total Occlusion Step by Step
V. Suryaprakasa Rao, MD, DM Department of Cardiology, Care Hospitals Banjara Hills, Hyderabad, Telangana India sp.vithala@yahoo.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Retrograde approach for chronic total occlusion percutaneous intervention is the ultimate technique for success in cases of high Japan-CTO (JCTO) score, ostial locations, long calcific lesions with calcium, and in retry cases. There are various methods of collateral cross, reverse controlled antegrade and retrograde tracking, and externalization, which are practiced by various experts. Intravascular ultrasound-guided procedures will minimize complications and increase chances of stent optimization for better outcomes.
Keywords
chronic total occlusion
retrograde
percutaneous intervention
Introduction
Percutaneous intervention (PCI) of chronic total occlusion (CTO) is the last frontier of coronary interventions and has substantial evidence that it improves the quality of life, relieves angina, and improves left ventricular function, particularly in left anterior descending (LAD) artery territory.1 2 3 CTO PCI reduces arrhythmias and improves outcomes in acute coronary syndrome4 5 in other vessels. The retrograde approach in complex CTO PCI is based on the principle that a softer distal cap can be penetrated with more ease. An intercoronary collateral either septal or epicardial or a bypass graft is important for a retrograde approach.
Historical Prospective and Indications
This approach was first attempted by Dr. Kahn and Dr. Hartzler using saphenous vein graft (SVG) for accessing a LAD CTO in 1990.6 In 1996, Silvestri et al performed left main stenting through the retrograde approach via the SVG.7 As the Japanese operators took lead in innovations, Dr. Saito and his colleagues from Japan published their experience in several retrograde PCI registries with encouraging results approaching 90% success. Having originated in Japan, retrograde PCI was adopted in Europe and the United States. Although a failed antegrade approach8 9 10 11 12 is the most important indication, other anatomical subsets needing primary retrograde approach include ostial location of occlusion, ambiguous proximal cap, major bifurcation near distal cap, and long occlusions with calcification. Almost 20 to 50% of CTO PCIs are performed through the retrograde approach. The success rate of CTO PCI increased from 70 to 90% with use of retrograde approach.11 12 13 14 15 16 17 18 19
Procedural Details
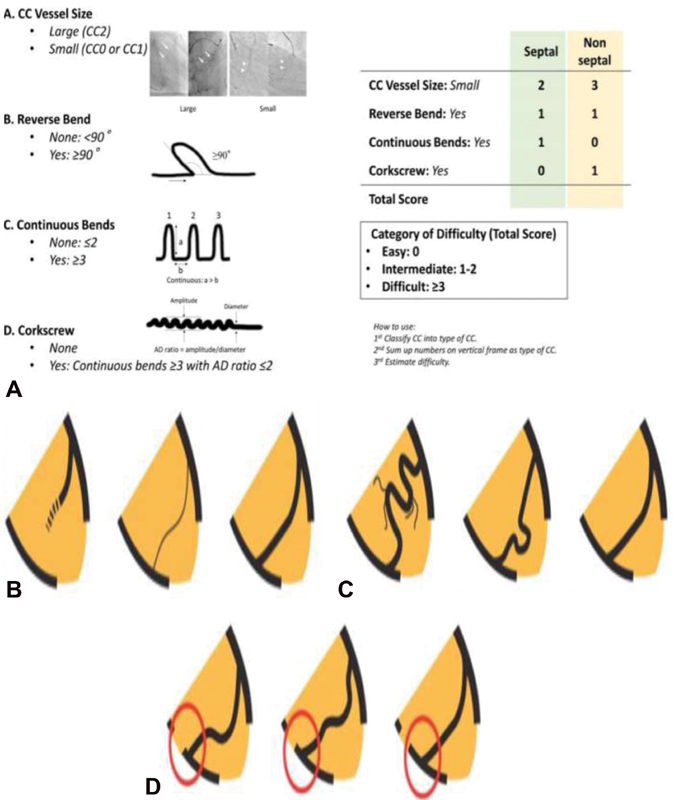
A dual injection in low magnification with donor artery injection first and without panning provides a detailed analysis of proximal cap, distal cap, length of lesion, calcium, tortuosity, and collaterals from the donor artery (Fig. 1A–C). Visualization of collaterals is the most important step in retrograde PCI intervention. Collaterals are basically divided into epicardial and septal pathways. Based on the diameter of collateral connection (CC) size, Werner classification grades it into three categories: CC0, no angiographic connection; CC1, thread-like connection (<0.4 mm); and CC2, side branch-like connection (>0.4 mm). A CC1, CC2 septal collateral (Werner classification) is a prerequisite for a successful wire cross. Very rarely CC0 collateral can be crossed by what is called surfing and a no contrast injection approach.20

-
Fig. 1 (A) Algorithm of chronic total occlusion crossing. (B) Dual injection. (C) Dual injection.
Fig. 1 (A) Algorithm of chronic total occlusion crossing. (B) Dual injection. (C) Dual injection.
Toolbox of Retrograde Approach
Appropriate hardware, operator's skill, suitable anatomy with good-sized donor artery, and regular activated clotting time (ACT) monitoring (300–350 seconds) are required for successful retrograde approach. Septal collaterals are safest and are preferred as initial choice. A less tortuous, less branching (CC1, CC2) without much angulation at entry and exit are key for successful cross. Early arising S1, S2 collaterals are better as navigating microcatheters will be difficult with distally arising collaterals.21 22 Navigating a LAD to posterior descending artery (PDA) septal collateral is easier than navigating a PDA to LAD septal collateral. The preferred guiding catheters are extra back-up (EBU) 3.0, 3.5 for left coronary artery and amplatzer 1 (AL1), AL2 0.75/1 with side holes (SH) for right coronary artery in most of the cases. Side holes AL in right coronary artery (RCA) CTO is useful to protect from ischemia of conus artery and avoid pressure dampening, but contrast usage will be more. Also, 7F bifemoral sheaths are preferable in a difficult CTO PCI by most operators though European operators use biradial approach not uncommonly. A 7F slender radial sheath (Terumo) and a 7F femoral approach is another option. Long 45 cm 7F or 8F braided sheaths in case of tortuous iliac arteries give good backup support. Furthermore, 90 cm short guiding catheters are required in case of SVG graft or left internal mammary artery (LIMA) as donor artery or for navigating long epicardial collateral or for distal septal collateral. Microcatheters play a key role in navigating collateral after wire crossing and support the CTO crossing with dedicated wires and even externalization of wires. The Corsair 150 (Asahi Intec), Caravel 150 (Asahi Intec), Finecross 150 (Terumo), and Turnpike 150 (Vascular Solutions)18 are important in support catheter category. Most operators prefer a Corsair 150 (2.6 F) or Caravel 150 (1.9 F) in septal collateral crossing, and Caravel 150 in an epicardial collateral crossing. The Corsair needs minimum 10 rotations clockwise and counterclockwise with gentle push while Caravel does not need any rotations but a gentle push. The radio-opaque tip of Caravel is less visible on fluoroscopy and is slippery.
Toolbox
-
7F and 8F systems
-
Intravascular ultrasound (IVUS) + Support catheters + Balloon – 8F
-
Support catheters: Corsair 135 cm, 150 cm; Caravel Pro, Finecross
-
Dual lumen catheters: Crusade
-
Guide extensions: Guideliner, Guidezilla
-
Guidewires: Sion series, Suoh 03, Fielder XTR series, Gaia series, Ultimate series, Miracle series, Conquest Pro, RG3
-
Low-profile balloons
-
2 cc Leuer lock syringes
-
Push-pull Y connector
-
Trapping balloons
-
Long drug eluting stents (DES)
-
Coils and snares
-
ACT monitoring
-
IVUS
Collateral Wire Navigation
Multiple orthogonal views are required to study collaterals with selective, super selective injection with 2 mL Leuer lock syringe (0.5 mL contrast) (Fig. 2A–D). This will ensure evaluating any acute angulation or tortuosity, and defining exit points up to distal cap. An aspiration through a microcatheter is absolutely necessary before any selective injection. Epicardial collateral with tortuosity is crossed by rotation of wire than gentle push and preferably in diastole. The septal collateral is crossed with Sion or Runthrough wires with tiny bend at tip and exchanged to a Sion blue, Suoh 03, or Sion black. The workhorse wire is closely followed by a microcatheter. The Suoh 03 is a hydrophilic, preshaped, and atraumatic wire with low penetrating power. It is the wire of choice for a difficult septal collateral cross. Sion black polymer jacket with slip coat and rope coil structured tip is good for distal tortuosity. Fielder XTR is another polymer jacketed wire with low penetration power that is useful for septal surfing of invisible collateral.
-
Fig. 2 (A) J channel score. (B) Collateral connection size. (C) Collateral tortuosity. (D) Collateral to recipient artery.
Fig. 2 (A) J channel score. (B) Collateral connection size. (C) Collateral tortuosity. (D) Collateral to recipient artery.
Wire Crossed into Distal Cap but Microcatheter Does Not Cross
In this situation, visualization in left anterior oblique (LAO) view (especially RCA CTO) uncovers an acute bend that Corsair may not be able to negotiate. The options include deep throating the donor guiding catheter, anchor balloon for guiding support, Guidezilla or Guideliner support, and finally changing the microcatheter from Caravel to Corsair Pro or to Finecross. Sometimes change of collateral channel will be helpful.
Puncture of Distal Cap
Distal cap penetration needs wires with more penetration power with good torque. Gaia 2, which is preshaped with 1:1 torque transmission, Miracle 3, and Ultimate Bros are good wires for distal cap puncture. Sometimes wires with more penetrating power like Gaia 3, Pilot 200, Conquest Pro 12, or Hornet (Boston Scientific) are needed.6 23
Antegrade–Retrograde Channel Connection
Antegrade bed preparation by microcatheter and antegrade wire (Fielder XTR, Gaia, etc.) is necessary before retrograde device tracking (Fig. 3A–N). About 30% of cases can be completed by a simple retrograde wire cross to the antegrade microcatheter. Retrograde microcatheter can be a landmark, like kissing wire, for antegrade wire.24 In most cases, a reverse controlled antegrade and retrograde tracking (CART) is performed to create connection in subintimal space in CTO segment. In this technique, after the antegrade–retrograde wire overlap, a 2 mm/2.5 mm NC balloon is inflated on antegrade wire with retrograde catheter close to the shoulder of the balloon. The retrograde wire is then navigated to the subintimal space and then into the proximal true lumen once the balloon is deflated. In assisted reverse CART, a 5F IVUS (Eagle Eye, Philips, HD 60, and Boston Scientific) assists in assessing the wire position and selecting the balloon site for reverse CART.25 A Guidezilla 5.5F or 6F on antegrade wire is also helpful for assisted reverse CART. The retrograde wire26 in intima and antegrade wire in subintima are most difficult subset for reverse CART. In contemporary reverse CART, a low profile (2 mm NC balloon) is dilated on antegrade wire in subintima in the distal part of CTO and Gaia 2 wire is manipulated to make connection with antegrade wire. In extended reverse CART, the connection is made with higher-sized balloon beyond the CTO segment proximally. Finally, in case of difficulty in navigating the retrograde wire, knuckle wire technique can be used to enter subintimal space and into the true lumen. A Fielder XTR, Sion black, Pilot 200, and Gladius are good for this technique. An IVUS check of wire positions is always safe before the entry of retrograde wire into antegrade guiding to avoid serious problems of subintimal stenting at ostial RCA or left main coronary artery (LMCA), respectively.27 28 29 30 31 32 33
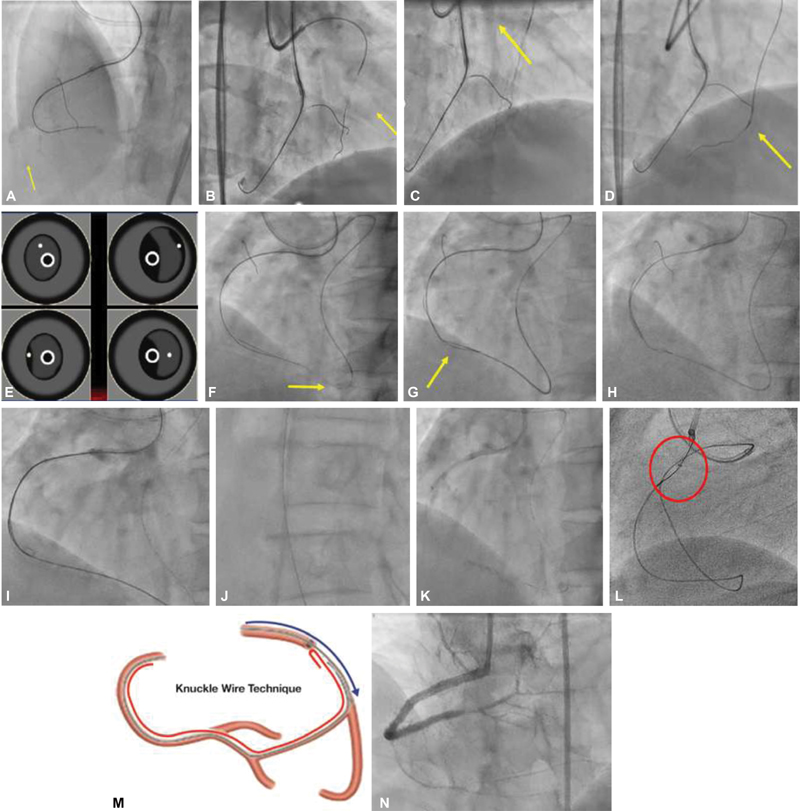
-
Fig. 3 (A) Antegrade bed preparation with Corsair 135 with Gaia 2 in false lumen. (B) Sion Blue in septal S1 collateral. (C) Selective channel injection. (D) Suoh 3 in tortuosity. (E) Wire position in intravascular ultrasound: (1) both wires in intima, (2) both wires in subintima, (3) antegrade wire in intima, retrograde wire in subintima, and (4) antegrade wire in subintima, retrograde wire in intima. (F) Corsair nonnegotiable at the bend, exchanged to Corsair Pro by balloon trap technique. (G) Suoh 03 exchanged to Gaia 2. (H) Reverse controlled antegrade and retrograde tracking at the chronic total occlusion site with 2.0 × 10 NC balloon. (I) Retrograde Gaia 2 into antegrade Guidezilla. (J) Externalization with RG3. (K) Angioplasty with 2.0 and 2.25 NC on the RG3 wire. (L) Antegrade Sion to retrograde Corsair (Rendezvous technique). (M) Knuckle wire technique. (N) Overlapping long drug eluting stent.
Fig. 3 (A) Antegrade bed preparation with Corsair 135 with Gaia 2 in false lumen. (B) Sion Blue in septal S1 collateral. (C) Selective channel injection. (D) Suoh 3 in tortuosity. (E) Wire position in intravascular ultrasound: (1) both wires in intima, (2) both wires in subintima, (3) antegrade wire in intima, retrograde wire in subintima, and (4) antegrade wire in subintima, retrograde wire in intima. (F) Corsair nonnegotiable at the bend, exchanged to Corsair Pro by balloon trap technique. (G) Suoh 03 exchanged to Gaia 2. (H) Reverse controlled antegrade and retrograde tracking at the chronic total occlusion site with 2.0 × 10 NC balloon. (I) Retrograde Gaia 2 into antegrade Guidezilla. (J) Externalization with RG3. (K) Angioplasty with 2.0 and 2.25 NC on the RG3 wire. (L) Antegrade Sion to retrograde Corsair (Rendezvous technique). (M) Knuckle wire technique. (N) Overlapping long drug eluting stent.
Externalization and DES Deployment
The retrograde wire is guided into the antegrade guiding catheter and trapped in the guiding catheter (2.5 mm NC balloon suitable for a 7F guide). This facilitates the microcatheter track along the wire into antegrade guide. Usage of Guidezilla or Guideliner is encouraged to externalize the wire so that subintimal positions of wire at ostioproximal locations (RCA or LMCA) can be avoided. It also fastens the externalization process. Once the microcatheter is in antegrade guide catheter, the wire is exchanged to RG3 (330cm) or Fielder FC 300 cm wire, which are long hydrophilic wires and very soft. RG3 is the preferred choice of most of CTO operators. Sometimes snaring by Ensnare (18 × 30 mm, 6F) or goose neck snare is used to navigate retrograde wire into antegrade guiding catheter. Snaring is done just proximal to the radio-opaque part of wire. The externalized RG3 wire is followed on fluoroscopy along the common iliac region and the Y connector is unlocked and detached from the guiding catheter hub. The retrograde wire is drawn carefully into copilot and the Y connector is reattached to guiding catheter hub. Flushing of the guide should be strictly avoided at this step and 20–30 cm of wire is externalized beyond the Y connector. The author uses rendezvous technique either in the coronary artery or in the antegrade guiding catheter where retrograde or antegrade wire can be carefully negotiated from one microcatheter to another making the externalization much easy.32 Balloon angioplasty and DES deployment are done by IVUS guidance over the RG3 wire after the retrograde microcatheter is withdrawn into the collaterals. A donor artery injection is given to check the collateral injury and donor artery dissection. Microcatheter can be threaded on to the RG3 wire in antegrade guide catheter and RG3 can be pulled back gently along with retrograde microcatheter to avoid collateral injury. In this process, both guiding catheters should be kept away from ostial locations to avoid guide-induced trauma. A workhorse wire in antegrade microcatheter and a check injection after the withdrawal of microcatheter complete the procedure.34 35 36 37 38
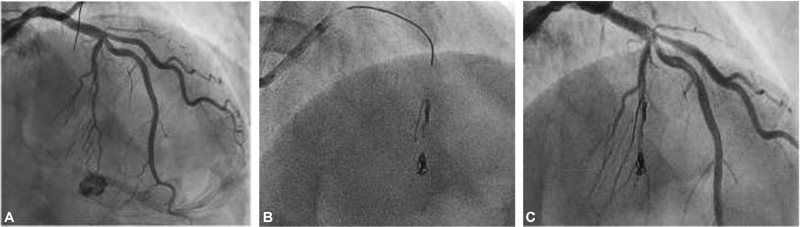
Complications
Donor artery dissection and thrombosis are dreadful complications of retrograde PCI that can be prevented by allowing back bleed during the procedure, monitoring pressure curve of the guiding catheter, and taking care during retrograde wire and microcatheter withdrawal (Fig. 4A–C). Dissection should be immediately addressed by prompt stenting. ACT should be monitored and maintained between 300 and 350 seconds to avoid donor artery thrombosis. Collateral injury can occur during wire navigation, microcatheter negotiation in bends, microcatheter withdrawal, and selective channel injection without allowing back bleed. Collateral channel perforation can occur into a cardiac chamber diagnosed by free wire movement and contrast disappearing fast or can be increasing septal hematoma.39 40 41 42 Usually septal hematomas are benign but need monitoring and, if large, need closure with the help of coils (Cook Hilal 2 mm, 3 mm coils). Coils can be delivered through Cook 4F delivery catheter or Finecross 130, 2.6F.43 44 45 Epicardial injury is catastrophic. It produces cardiac tamponade and can be avoided by checking position of wire before microcatheter advancement, ensuring back bleed before any selective injection. Epicardial injury is dealt by coil closure from both sides to seal perforation.
-
Fig. 4 (A) Channel injury. (B) Hilal coil deployment. (C) Septal leak sealed.
Fig. 4 (A) Channel injury. (B) Hilal coil deployment. (C) Septal leak sealed.
Conclusion
Retrograde PCI technique improves the overall success rate of CTO PCI to 90%. Improvements in wires, microcatheters, and imaging have contributed to the improvement in success rate. Retrograde PCI comes with its own unique challenges and complications and should be handled by experienced operators.
Conflict of Interest
None declared.
References
- Percutaneous transluminal coronary angioplasty of chronic total occlusions. Primary success, restenosis, and long-term clinical follow-up. Circulation. 1992;85(01):106-115.
- [Google Scholar]
- Procedural outcomes and long-term survival among patients undergoing percutaneous coronary intervention of a chronic total occlusion in native coronary arteries: a 20-year experience. J Am Coll Cardiol. 2001;38(02):409-414.
- [Google Scholar]
- Coronary angioplasty for chronic total occlusion reduces the need for subsequent coronary bypass surgery. Am Heart J. 1990;120(02):270-274.
- [Google Scholar]
- Ventricular arrhythmias among implantable cardioverter-defibrillator recipients for primary prevention: impact of chronic total coronary occlusion (VACTO Primary Study) Circ Arrhythm Electrophysiol. 2012;5(01):147-154.
- [Google Scholar]
- Percutaneous coronary intervention for chronic total occlusions: the Thoraxcenter experience 1992-2002. Eur Heart J. 2005;26(24):2630-2636.
- [Google Scholar]
- Retrograde coronary angioplasty of isolated arterial segments through saphenous vein bypass grafts. Cathet Cardiovasc Diagn. 1990;20(02):88-93.
- [Google Scholar]
- Angioplasty for chronic total occlusion by using tapered-tip guidewires. Catheter Cardiovasc Interv. 2003;59(03):305-311.
- [Google Scholar]
- Results of coronary angioplasty of chronic total occlusions (the National Heart, Lung, and Blood Institute 1985-1986 Percutaneous Transluminal Angioplasty Registry) Am J Cardiol. 1992;69(01):69-76.
- [Google Scholar]
- Angiographic assessment of collateral connections in comparison with invasively determined collateral function in chronic coronary occlusions. Circulation. 2003;107(15):1972-1977.
- [Google Scholar]
- The retrograde coronary approach for chronic total occlusions: mid-term results and technical tips & tricks. J Interv Cardiol. 2007;20(06):466-473.
- [Google Scholar]
- Different strategies of retrograde approach in coronary angioplasty for chronic total occlusion. Catheter Cardiovasc Interv. 2008;71(01):8-19.
- [Google Scholar]
- In-hospital outcomes of percutaneous coronary intervention in patients with chronic total occlusion: insights from the ERCTO (European Registry of Chronic Total Occlusion) registry. EuroIntervention. 2011;7(04):472-479.
- [Google Scholar]
- Hybrid approach improves success of chronic total occlusion angioplasty. Heart. 2016;102(18):1486-1493.
- [Google Scholar]
- Retrograde percutaneous recanalization of chronic total occlusion of the coronary arteries: procedural outcomes and predictors of success in contemporary practice. Circ Cardiovasc Interv. 2009;2(02):124-132.
- [Google Scholar]
- Retrograde coronary chronic total occlusion intervention. Curr Cardiol Rev. 2015;11(04):291-298.
- [Google Scholar]
- Guidewire crossing techniques in coronary chronic total occlusion intervention: A to Z. Indian Heart J. 2016;68(03):410-420.
- [Google Scholar]
- Retrograde coronary chronic total occlusion intervention using a novel reverse controlled antegrade and retrograde subintimal tracking. J Interv Cardiol. 2016;29(01):70-74.
- [Google Scholar]
- Deja vu of retrograde recanalization of coronary chronic total occlusion: a tale of a journey from Japan to India. Indian Heart J. 2016;68(04):584-585.
- [Google Scholar]
- Coronary septal collaterals as an access for the retrograde approach in the percutaneous treatment of coronary chronic total occlusions. Catheter Cardiovasc Interv. 2007;69(06):826-832.
- [Google Scholar]
- The retrograde technique for recanalization of chronic total occlusions: a step-by-step approach. JACC Cardiovasc Interv. 2012;5(01):1-11.
- [Google Scholar]
- Retrograde chronic total occlusion intervention: tips and tricks. Catheter Cardiovasc Interv. 2008;72(06):806-814.
- [Google Scholar]
- Current status of percutaneous coronary intervention of chronic total occlusion. J Zhejiang Univ Sci B. 2012;13(08):589-602.
- [Google Scholar]
- A complex case of right coronary artery chronic total occlusion treated by a successful multi-step Japanese approach. J Invasive Cardiol. 2006;18(08):E230-E233.
- [Google Scholar]
- New concept for CTO recanalization using controlled antegrade and retrograde subintimal tracking: the CART technique. J Invasive Cardiol. 2006;18(07):334-338.
- [Google Scholar]
- The first clinical experience with a novel catheter for collateral channel tracking in retrograde approach for chronic coronary total occlusions. JACC Cardiovasc Interv. 2010;3(02):165-171.
- [Google Scholar]
- Intravascular ultrasound guided percutaneous coronary intervention for chronic total occlusion. Curr Cardiol Rev. 2015;11(04):323-317.
- [Google Scholar]
- A novel modification of the retrograde approach for the recanalization of chronic total occlusion of the coronary arteries intravascular ultrasound-guided reverse controlled antegrade and retrograde tracking. JACC Cardiovasc Interv. 2010;3(02):155-164.
- [Google Scholar]
- The utility of a guideliner™ catheter in retrograde percutaneous coronary intervention of a chronic total occlusion with reverse cart-the “capture” technique. Catheter Cardiovasc Interv. 2014;83(06):929-932.
- [Google Scholar]
- The confluent balloon technique–two cases illustrating a novel method to achieve rapid wire crossing of chronic total occlusion during retrograde approach percutaneous coronary intervention. J Invasive Cardiol. 2009;21(10):539-542.
- [Google Scholar]
- Antegrade balloon transit of retrograde wire to bail out dissected left main during retrograde chronic total occlusion intervention–a variant of the reverse CART technique. J Invasive Cardiol. 2009;21(06):e113-e118.
- [Google Scholar]
- Use of the kissing microcatheter technique to exchange a retrograde wire for an antegrade wire in the retrograde approach to intervention in chronic total occlusion. J Invasive Cardiol. 2010;22(05):E74-E77.
- [Google Scholar]
- A new retrograde wiring technique for chronic total occlusion. Catheter Cardiovasc Interv. 2010;75(01):117-119.
- [Google Scholar]
- Percutaneous coronary intervention for a right coronary artery stent occlusion using retrograde delivery of a sirolimus-eluting stent via a septal perforator. Catheter Cardiovasc Interv. 2009;73(04):475-480.
- [Google Scholar]
- The final steps of the retrograde technique: wire externalization, stenting, and wire removal. Interv Cardiol Clin. 2012;1(03):345-348.
- [Google Scholar]
- A percutaneous treatment algorithm for crossing coronary chronic total occlusions. JACC Cardiovasc Interv. 2012;5(04):367-379.
- [Google Scholar]
- “Putting it all together”: a global approach to chronic total occlusion revascularization. J Indian Coll Cardiol. 2016;6:152-157. (3–4):
- [Google Scholar]
- Septum hematoma: a complication of retrograde wiring in chronic total occlusion. Int J Cardiol. 2006;113(02):e64-e66.
- [Google Scholar]
- Images in cardiovascular medicine. Interventricular septal hematoma and ventricular septal defect after retrograde intervention for a chronic total occlusion of a left anterior descending coronary artery. Circulation. 2010;122(20):e518-e521.
- [Google Scholar]
- Complications encountered in coronary chronic total occlusion intervention: prevention and bailout. Indian Heart J. 2016;68(05):737-746.
- [Google Scholar]
- Problems encountered in retrograde recanalization of coronary chronic total occlusion: should we lock the backdoor in 2018? Indian Heart J. 2018;70(01):132-134.
- [Google Scholar]
- Distal coronary perforation in patients with prior coronary artery bypass graft surgery: the importance of early treatment. Cardiovasc Revasc Med. 2016;17(06):412-417.
- [Google Scholar]
- Complications of chronic total occlusion angioplasty. Interv Cardiol Clin. 2012;1(03):373-389.
- [Google Scholar]
- Outcomes with the use of the retrograde approach for coronary chronic total occlusion interventions in a contemporary multicenter US registry. Circ Cardiovasc Interv. 2016;9(06):e003434.
- [Google Scholar]
- “Rendezvous in coronary” technique with the retrograde approach for chronic total occlusion. J Invasive Cardiol. 2010;22(09):E179-E182.
- [Google Scholar]







