Translate this page into:
Dynamic Enigma: Exercise Induced Left Bundle Branch Block
*Corresponding author: C. N. Abhishek Samdesi, Department of Cardiology, Sapthagiri Institute of Medical Sciences and Research Center, Bengaluru, Karnataka, India. samdesi.abhishek@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Samdesi CN, Latha BA, Chinnaswamy Narayanaswamy N. Dynamic Enigma: Exercise Induced Left Bundle Branch Block. Indian J Cardiovasc Dis Women. 2025;10:63-6. doi: 10.25259/IJCDW_79_2024
Abstract
EI-LBBB represents a rare phenomenon observed during electrocardiographic evaluation in response to exercise. We present an asymptomatic patient referred for cardiac fitness before tympanoplasty surgery. During the treadmill exercise test, the patient developed a left bundle branch block, which reverted spontaneously in the recovery phase. A coronary angiogram revealed double vessel disease involving the left anterior descending and left circumflex arteries. The occurrence of EI-LBBB during stress tests like the treadmill test (TMT) can be a direct marker of underlying ischemia and underlying coronary artery disease as seen in our case.
Keywords
Bundle branch block
Exercise-induced Left bundle branch block
Rate dependent Left bundle branch block
Transient bundle branch block
Treadmill test
INTRODUCTION
EI-LBBB refers to a conduction abnormality in which a transient or newly developed left bundle branch block manifests during exercise (e.g., exercise stress test-Treadmill test [TMT]) and resolves when the individual rests or the heart rate (HR) returns to baseline. It is a rare phenomenon, occurring in approximately 0.5–1.1% of patients undergoing TMT.[1] This condition occurs approximately six times more frequently in women.[2] The proposed mechanisms for transient bundle branch block (BBB) are as follows:[3]
Phase 3 block occurs when the initial aberrant complex results from an impulse encroaching on the refractory period (Phase 3 of the action potential). Tachycardia-associated LBBB is considered to occur because of an abnormality in Phase 3 conduction (repolarization), leading to delayed or blocked impulses at elevated heart rates when they fall within the refractory period of the action potential.
Phase 4 or bradycardia-dependent block is due to loss of resting membrane potential owing to disease and/or phase 4 depolarization. At slower heart rates, spontaneous diastolic (Phase 4) depolarization of the left bundle branch renders it refractory to the next incoming impulse.[4,5]
Rate dependent conduction block: At higher HRs, the electrical impulse travels faster reducing the refractory period. If one bundle branch cannot conduct impulse fast enough, a temporary block occurs at a certain HR (rate dependent block) and resolves when the HR slows
An acceleration-dependent block resulting from pathology within the His-Purkinje system
Retrograde concealment: It refers to the process by which, at faster heart rates, retrograde penetration of a bundle branch leaves it refractory, inhibiting the forward conduction of subsequent impulses through the normal pathways.
Ischemia-related conduction block: Ischemia due to coronary artery disease (CAD) can impair conduction systems ability to transmit electrical impulses and is often seen during episodes of stress or exertion
During episodes of increased vagal tone or autonomic imbalance (e.g., fainting and bradycardia), a transient bundle branch block (BBB) can occur
Infection or inflammation such as myocarditis may cause transient BBB due to inflammation affecting the conducting system.
EI-LBBB serves as an independent predictor of significant cardiovascular morbidity and mortality.[4] Coronary artery disease (CAD) is present in 70% of patients with EI-LBBB, whereas exercise-induced right bundle branch block (EIRBBB) has been associated with CAD in all reported cases.[4] LBBB can lead to mechanical dyssynchrony, deterioration of left ventricular function, and heart failure. Transient exercise-induced left bundle branch block (EI-LBBB) can result in reversible left ventricular dyssynchrony. The existing understanding of this phenomenon primarily stems from case reports and case series, and its management remains a subject of ongoing discussion. Here, we present a case of EILBBB attributed to coronary artery disease (CAD).
CASE REPORT
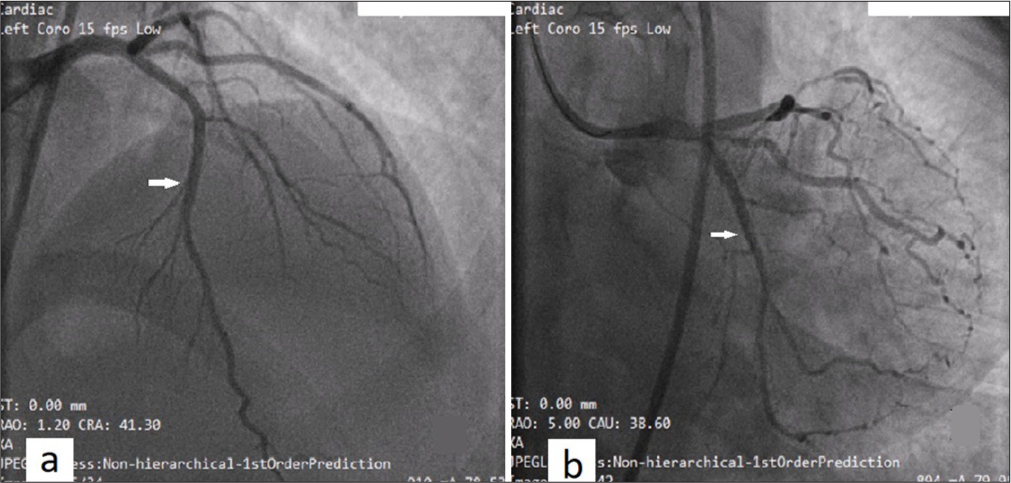
A 50-year-old female with the right-sided otitis media, on cefixime oral antibiotic, planned for tympanoplasty was referred for surgical fitness. She had no cardiorespiratory complaints and had been newly diagnosed with hypothyroidism (Thyroid stimulating hormone [TSH]: 104.4 mIU/L, T3: 2.35 pg/mL, Free T4: 0.42 ng/dL). The electrocardiogram (ECG) had a normal sinus rhythm, with HR of 80 bpm (beats/min), poor R wave progression, inverted T waves were observed in leads I, aVL, II, aVF, and V3-6 [Figure 1]. Echocardiography done was normal with no regional wall motion abnormalities, no diastolic dysfunction, and a normal left ventricular ejection fraction (LVEF) of 60%. An exercise stress test, TMT was conducted using the Bruce protocol, during which LBBB developed in stage 2 at a HR of 145 bpm, 85% of Target HR (THR) at 6:00 min of exercise [Figure 2]. Exercise was terminated in view of chest pain at 6:53 min. The LBBB reverted to sinus rhythm at a HR of 85 bpm after 3 min into the recovery phase, but ST depression and inverted T waves were observed in inferior leads [Figure 3], validating the need for coronary angiogram. During the TMT, the patient attained a normal HR response, blood pressure response, good exercise capacity (8 metabolic equivalent [METS]), and was diagnosed to have EI-LBBB. A coronary angiogram was advised to rule out ischemic heart disease and it revealed double-vessel disease, involving left anterior descending (LAD) showing proximal-to-mid long lesion maximum 90% [Figure 4a] and left circumflex arteries (LCXs) non-dominant vessel with ostial 20–30% lesion, proximal to distal long segment 90% lesion [Figure 4b], and right coronary artery was dominant and normal. The patient was advised for percutaneous transluminal coronary angioplasty (PTCA) stenting of the LAD and LCX. During the course of admission, endocrinologist opinion was taken for Hypothyroidism and was started on 100 mcg of Thyroxine tablet. The patient was taken up for elective PTCA stenting and successful PTCA stenting was done to LAD and LCX [Figure 5a and b]. At 1-month follow-up, her repeat TSH was 0.66 mIU/L and thyroxine tablet dose tapered accordingly. She remains symptomatically and hemodynamically stable on subsequent follow-up.
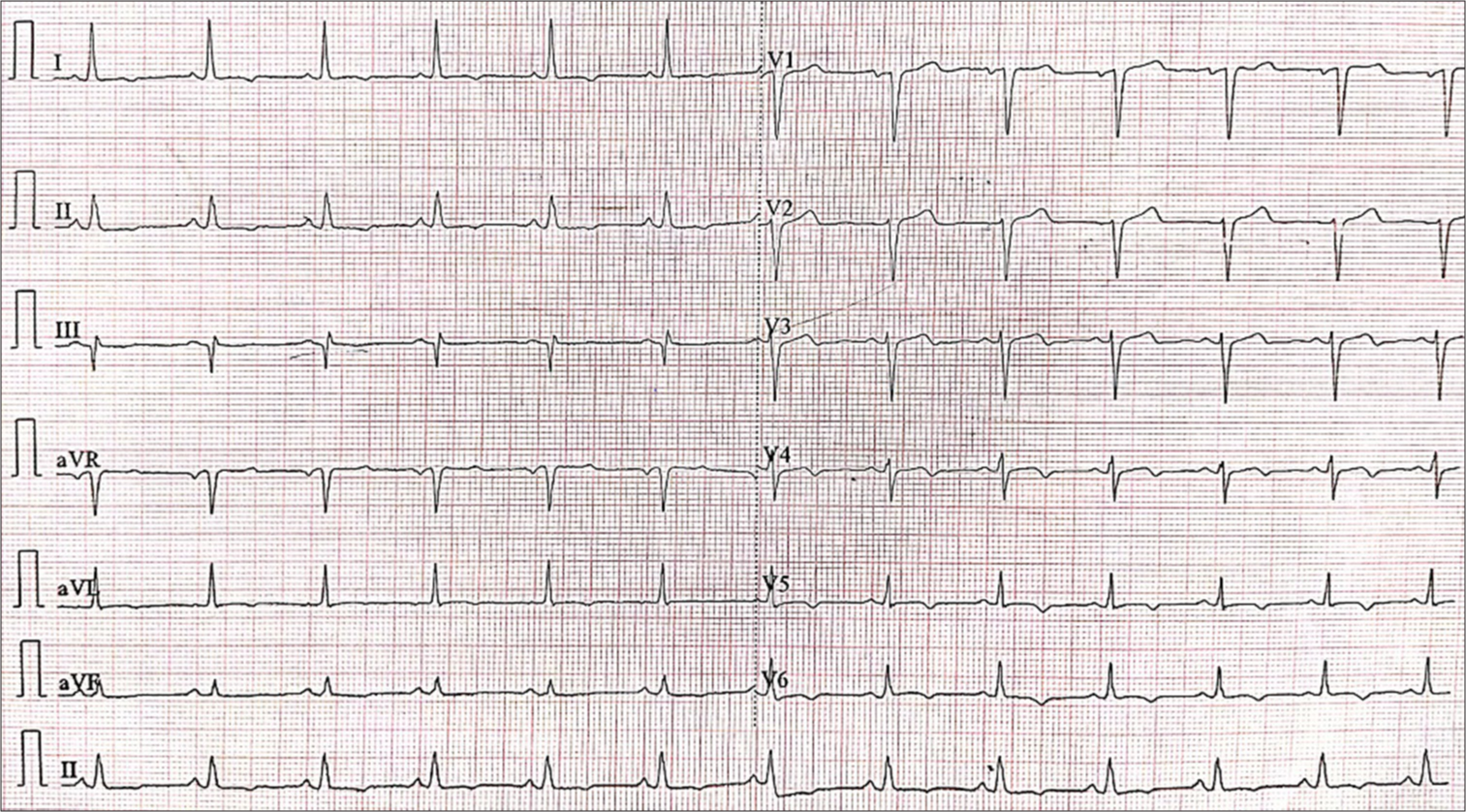
- Baseline electrocardiogram. Normal sinus rhythm, heart rate of 75 bpm, poor R wave progression, and inverted T waves were observed in leads I, aVL, II, aVF, and V3-6.
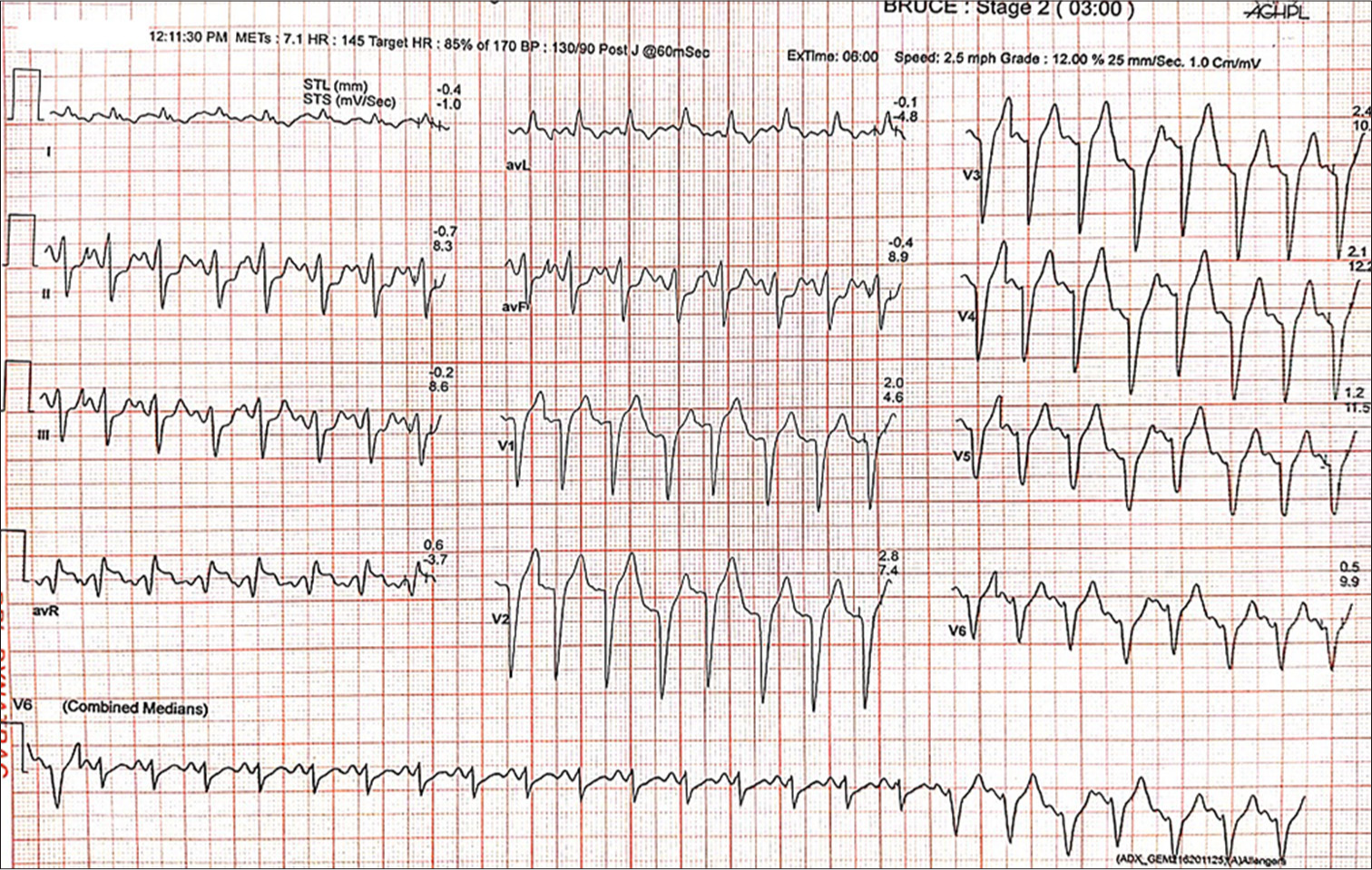
- Stage 2 of Bruce protocol. A transition from sinus rhythm to left bundle branch block pattern observed at heart rate of 145 bpm.
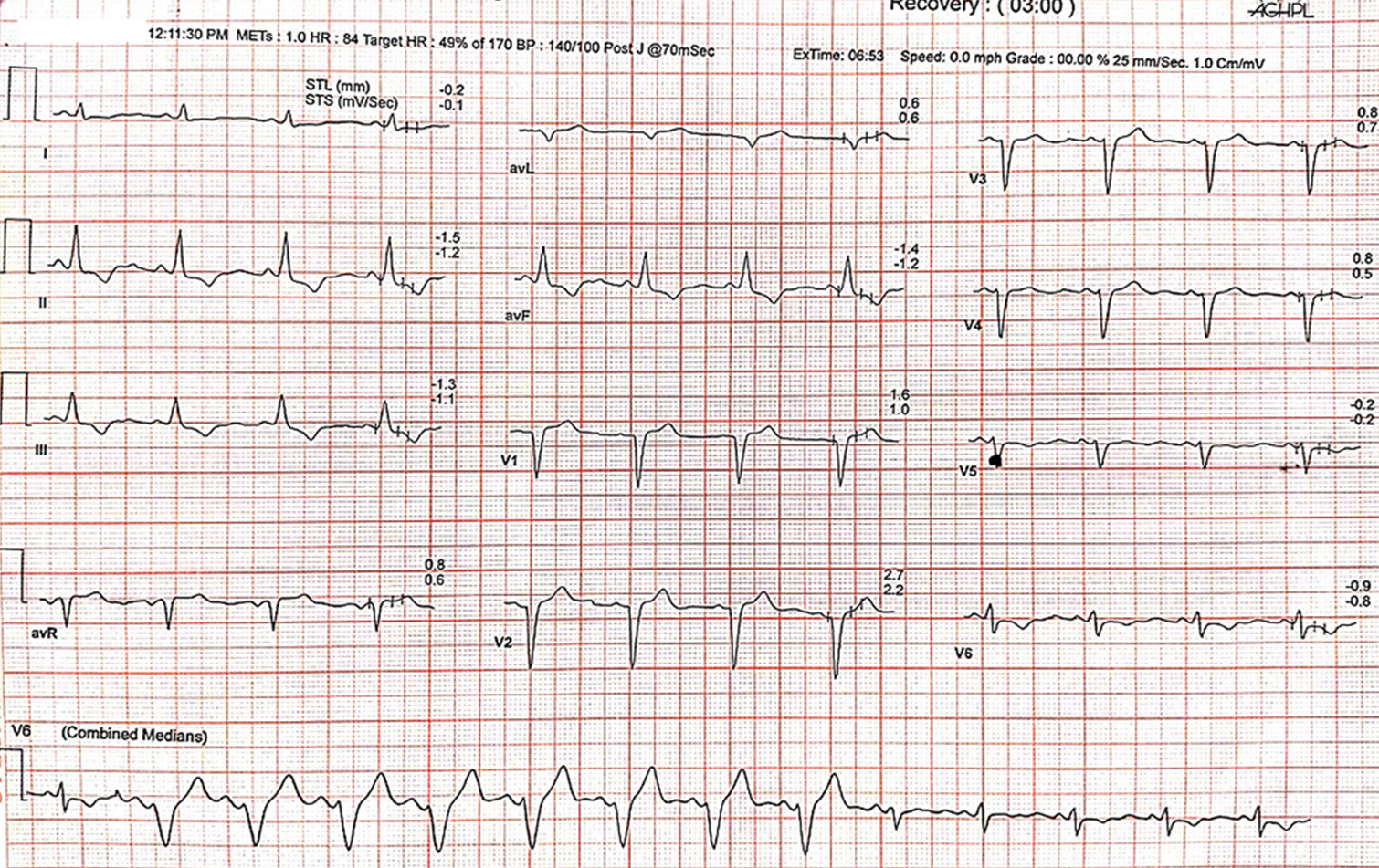
- Recovery phase of exercise stress test. Transition from the left bundle branch block to sinus rhythm can be observed at a heart rate of 85 bpm at 3 min into recovery phase. ST depression with inverted T waves are noted in inferior leads.
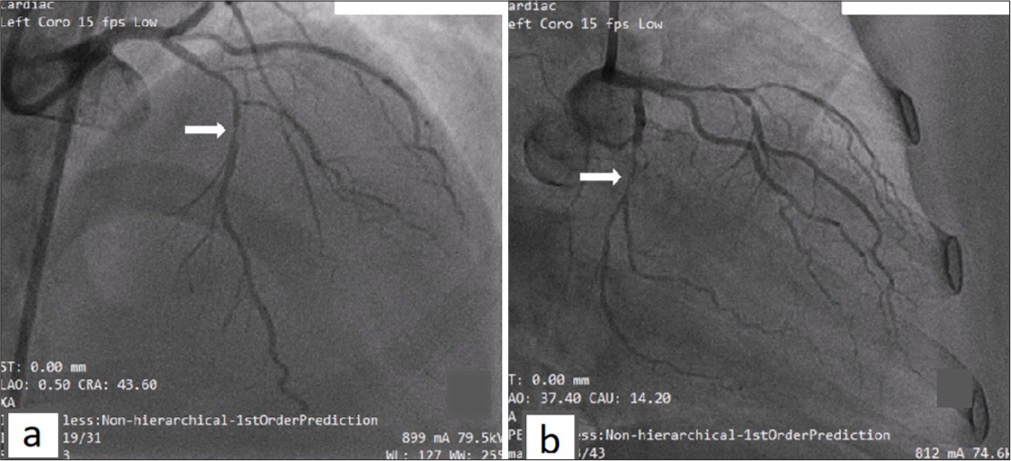
- Coronary angiogram. (a) Left anterior descending shows proximal to mid long lesion maximum 90%. (b) Left circumflex arteries shows ostial 20–30% disease and proximal 9 0% lesion (white arrows indicating the narrowest part of stenosis).
- Post PTCA stenting with drug-eluting stents (DES). (a) Proximal to mid left anterior descending stented with 2.25 × 28 mm DES, post dilated with 2.75 × 10 mm non-compliant Balloon. (b) Proximal left circumflex arteries stented with 2.25 × 10 mm DES (white arrows indicating site of stent placement).
DISCUSSION
EI-LBBB was initially described in 1946 in a young man with a history of smoking, presenting with exertional palpitations and dizziness.[5] EI-LBBB is an uncommon electrocardiographic finding, observed in approximately 0.4% to 0.5% of exercise tests[1] and independently predicts significant cardiovascular morbidity in 19% of cases and mortality in 29%.[1]
Hypothyroidism can lead to various electrocardiographic changes including bradycardia (7–15%), BBBs such as RBBB (5.2%), LBBB (5.1%), low voltage QRS complexes, and arrhythmias due to QT prolongation. The relationship between hypothyroidism and EILBBB is not well-established in medical literature.[6]
Although EI-RBBB is less frequently observed than EI-LBBB, it demonstrates a 100% association with CAD, commonly involving obstructive lesions in the left anterior descending artery.[7,8]
The clinical prognosis of individuals with EI-LBBB is determined by the degree of coronary artery disease involvement, patient age and presence of heart failure. Patients with EI-LBBB are usually considered benign when EI-LBBB occurs at a HR of ≥120–125 bpm. These subset of patients were found to have normal epicardial coronaries and a better prognosis.[9-11] EI-LBBB occurring at heart rates of <120–125 bpm is associated with occlusive coronary artery disease (CAD) in approximately 70% of cases.[7]
However, in our case, the patient developed EI-LBBB at a heart rate of 145 bpm at 6-minutes, with the onset of chest pain occurring at 6 minutes and 53 seconds, prompting termination of the TMT. On further evaluation with coronary angiogram, the patient had underlying multi-vessel CAD.
In a patient with EI-LBBB, especially when they develop symptoms or ECG changes on recovery phase during exercise testing, it is always better to do further cardiac evaluation such as coronary angiogram to rule out underlying CAD.
CONCLUSION
Patients with EI-LBBB are typically considered as having a benign condition; However, its occurrence is associated with an increased risk of all-cause mortality. The appearance of EI-LBBB during treadmill test (TMT) may indicate underlying ischemia, warranting test termination, especially if accompanied by chest pain or other concerning symptoms. Thus, patients developing EI-LBBB on exercise stress tests should be evaluated for any underlying CAD.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Prognostic Significance of Exercise Induced Left Bundle-Branch Block. JAMA. 1998;279:153-6.
- [CrossRef] [PubMed] [Google Scholar]
- Exercise-Induced Left Bundle Branch Block: Prevalence and Prognosis. Arq Bras Cardiol. 2011;97:26-32.
- [CrossRef] [PubMed] [Google Scholar]
- The Concept of Masquerading Bundle-Branch Block; An ElectrocardiographicPathologic Correlation. Circulation. 1958;17:397-409.
- [CrossRef] [PubMed] [Google Scholar]
- Intraventricular Conduction Disturbances In: Clinical Cardiac Electrophysiology (3rd ed). Philadelphia, PA: Lippincott Williams and Wilkins; 2004. p. :110-39.
- [Google Scholar]
- Left Bundle Branch Block: Current and Future Perspectives. Circ Arrhythm Electrophysiol. 2020;13:e008239.
- [CrossRef] [PubMed] [Google Scholar]
- Thyroid Dysfunction in Patients Admitted in Cardiac Care Unit: Prevalence, Characteristic and Hospitalization Outcomes. Int J Gen Med. 2021;14:505-14.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical Significance of Exercise-Induced Bundle Branch Block. Am J Cardiol. 1988;61:346-8.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and Prognostic Significance of Exercise-Induced Right Bundle Branch Block. Am J Cardiol. 2010;105:677-80.
- [CrossRef] [PubMed] [Google Scholar]
- Chest Pain and Exercise Induced Left Bundle Branch Block-A Clinical Dilemma. J Family Med Prim Care. 2019;8:3434-6.
- [CrossRef] [PubMed] [Google Scholar]
- Complete Bundle Branch Block During Exercise Test. Clinical and Coronary Angiographic Data. Arch Mal Coeur Vaiss. 1991;84:167-71.
- [Google Scholar]
- Exercise Dependent Complete Left Bundle Branch Block. Eur Heart J. 1992;13:1447-51.
- [CrossRef] [PubMed] [Google Scholar]








