Translate this page into:
Correlation of Global Longitudinal Strain with Functional Status of Patients with Left Ventricular Systolic Dysfunction: Does Gender Difference Exist?
*Corresponding author: Biraja Prasad Beura, Department of Cardiology, Maharaja Krushna Chandra Gajapati Medical College and Hospital, Berhampur, Odisha, India. subhashreebarik91@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Beura BP, Singh S. Correlation of Global Longitudinal Strain with Functional Status of Patients with Left Ventricular Systolic Dysfunction: Does Gender Difference Exist? Indian J Cardiovasc Dis Women. 2024;9:213-20. doi: 10.25259/IJCDW_66_2023
Abstract
Objectives:
Two-dimensional (2D) echocardiographic (echo) assessment of the left ventricular ejection fraction (LVEF) by Simpson’s biplane method is routinely used in clinical practice for patient management. The measurement of global longitudinal strain (GLS) using speckle tracking echocardiography is a new method for assessing left ventricular (LV) systolic function with several advantages. There are very few observations regarding the correlation of 2D GLS with the functional status of patients with the LV systolic dysfunction (LVSD). Therefore, we aimed to evaluate the superiority of GLS over Simpson’s method of LVEF in predicting the functional status of the patients with moderate-to-severe LVSD (ejection fraction <40%) and to find out if any difference exists between male and female patients.
Materials and Methods:
Fifty patients aged 18–80 years satisfying the inclusion and exclusion criteria were studied over a period of 2 months. Simpson’s method was used to calculate 2D LVEF. 2D GLS was assessed using an automated function imaging technique. The Minnesota living with heart failure questionnaire was used to assess the functional status of patients.
Results:
Correlation of functional status of patients was better with 2D GLS than 2D LVEF, although both were found to be statistically significant and no statistically significant difference was found in observations between both genders.
Conclusion:
The correlation of functional status of patients with moderate-to-severe LVSD was better with 2D GLS than 2D LVEF. Further studies are needed to identify the gender differences in 2D GLS correlation with the functional status of patients with LVSD.
Keywords
Global longitudinal strain
2D left ventricular ejection fraction
Minnesota living with heart failure questionnaire
Functional status
ABSTRACT IMAGE
INTRODUCTION
Two-dimensional (2D) echocardiographic (echo) assessment of the left ventricular ejection fraction (LVEF) is commonly used in clinical practice for patient management. It is also an independent predictor of mortality. However, 2D LVEF by Simpson’s biplane method has several limitations such as it is dependent on the imaging plane, and observer experience, requires manual endocardial tracking of end-diastolic and end-systolic frames from 2D imaging is time-consuming, is restricted by a high-level of measurement variability, has limitations of reproducibility and inability to detect small changes in contractility. Its accuracy varies with image quality.[1]
Doppler tissue imaging (DTI) emerged as a useful echo tool for the quantitative assessment of the left ventricular (LV) systolic and diastolic function. Myocardial mitral annular or basal segmental systolic (S’) and early diastolic (Ea or E’) velocities were shown to predict mortality or cardiovascular events in cardiac diseases. Patients with reduced S’ or E’ values, in particular, have a very poor prognosis.[2] However, for a predefined value of the ejection fraction (EF) in patients with intermediate-stage heart failure (HF), a large range of DTI values may be observed, highlighting the discrepancy between the two parameters.
Recent advances in three-dimensional echocardiography are likely to improve the accuracy of LV volumes, but these techniques are not yet feasible in clinical routine.[3]
Other emerging techniques have been developed and provide new hope by directly targeting myocardial contraction or deformation rather than its consequences (i.e., DTI velocities). The first approaches are based on velocity imaging data sets, with encouraging experimental and clinical results.[4,5] However, these techniques are not yet feasible in routine clinical practice.
More recently, deformation analyses were switched from color-derived DTI to pure grayscale imaging, applying the speckle-tracking method.[6] This method was validated in experimental studies[7] and implemented in conventional echo systems for direct clinical applications.[8,9]
The measurement of global longitudinal strain (GLS) using speckle tracking echocardiography (STE) has emerged as a new modality for assessing LV systolic function, proven to be effective in the early detection of contraction abnormalities in cardiac diseases such as hypertrophic cardiomyopathy HF with preserved EF (HFpEF).[10] 2D GLS is relatively operator-independent, better reproducible, and can detect minor changes in myocardial function. Studies have shown that 2D GLS can predict mortality more accurately than 2D LVEF.[11] There are limited observations regarding the functional status of patients with LV systolic dysfunction (LVSD) in different genders.
Based on these reflections, our hypothesis is that the stratification of patients with abnormal LV function would be better predicted using GLS than conventional echo parameters and to find out if any gender difference exists.
Review of literature
HF is a complex clinical syndrome. HF is defined as a clinical syndrome with symptoms and/or signs caused by a structural and/or functional cardiac abnormality and corroborated by elevated natriuretic peptide levels and/or objective evidence of pulmonary or systemic congestion.[12] Based on LVEF, HF is classified into three EF categories, namely, HF with reduced (HFrEF), mildly reduced, and HFpEF, according to the EF ranges ≤40%, 41–49%, and ≥50%, respectively.
Echocardiography is the principal cardiac imaging tool used when assessing LV systolic function in patients with HF. Quantifying LV systolic function is vital in predicting adverse outcomes in patients with HF.[13] Two-dimensional echocardiography can be used for evaluating LV systolic function by obtaining LVEF.[14] This parameter is widely used in clinical practice[15] and has been established as a predictor of mortality in HF patients.[16] However, the measurement of EF presents a number of challenges related to image quality, assumptions of LV geometry, and expertise.
The regional wall motion is usually assessed by the operator by visualizing (eyeballing) the LV endocardial motion as well as wall thickening. The left ventricle is divided into 17 segments – six basal segments, six mid-cavity segments, and five apical segments. These 17 segments can be arranged as a polar (bull’s-eye) plot with the apex in the center, the four apical segments as the first ring, the six mid-cavity segments as the second ring, and the six basal segments as the outer ring. The terminologies advocated by the American Society of Echocardiography for wall motion are normal, hypokinetic, akinetic, dyskinetic, aneurysmal, or hyperkinetic. Visual assessment of wall motion requires individual expertise and is purely subjective.[17] The wall motion could be labeled as one of the six types as termed above. As the left ventricle contracts in systole, it shortens in the longitudinal and circumferential direction (negative strain) and thickens in the radial direction (positive strain).[18] The change in length or thickness is measured and expressed as a percentage of its diastolic length or thickness. This change in length or thickness is called the strain or deformation.[19,20]
The systolic shortening of a segment of the myocardium is strain or deformation and is expressed as a percentage of the diastolic length. This mimics the EF, where it is expressed as a percentage of the diastolic volume ejected out in systole.
Conventionally, strain curves were recorded by tissue Doppler echocardiography from various segments of the myocardium.[21] For precise evaluation, the incident ultrasound beam should be parallel to the myocardium interrogated. This problem is avoided by Speckle tracking,[22] Speckle tracking is angle-independent and, hence, has less interobserver and intraobserver variability.[23] The strain measurements are done by different software from various vendors. In our study, the automated function imaging (AFI) protocol by the general electric echo machines is used.
The Copenhagen City Heart Study (2017) by Biering-Sørensen et al.[24] conducted a study on GLS by Echocardiography Predicting Long-Term Risk of Cardiovascular Morbidity and Mortality in a Low-Risk General Population. They opined that GLS provides independent and incremental prognostic information regarding the long-term risk of cardiovascular morbidity and mortality. GLS seemed to be a stronger prognosticator in men than in women.
Romano et al. (2018)[25] found that cardiac magnetic resonance (CMR) feature-tracking derived GLS was a powerful independent predictor of mortality in a multi-center population of patients with ischemic or non-ischemic dilated cardiomyopathy, incremental to common clinical and CMR risk-factors, including EF and late-gadolinium-enhancement.
A study on ventricular longitudinal shortening as an independent predictor of death in HF patients with reduced EF by Berg et al. (2021)[26] found that measures of ventricular longitudinal shortening were important predictors of cardiovascular and all-cause death in patients with HFrEF and remained independently prognostic even after adjusting for well-known clinical risk factors.
Aims and objectives
The objectives of this study were as follows:
To assess whether 2D GLS is better correlated with the functional status of the patients when compared to 2D LVEF in patients with moderate to severe LVSD
Compare the above findings in male and female patients.
MATERIALS AND METHODS
Study area
The study was conducted at MKCG Medical College and Hospital, Berhampur, Odisha.
Study population
Fifty patients of either gender presenting to the cardiology department of our hospital with moderate-to-severe LVSD (2D LVEF <40%), satisfying inclusion and exclusion criteria were included in the study.
Study period
The study period was 2 months (September 13, 2023– November 13, 2023).
Sample size
Fifty consecutive, eligible, consenting patients, satisfying inclusion and exclusion criteria were included in the study.
Study design
This was a prospective hospital-based single-center observational study.
Ethical clearance and confidentiality
The ethical clearance for the study was taken by the Institutional Review Board for Ethical Clearance of M.K.C.G. Medical College and Hospital, Berhampur. All subjects/attendants were explained about the procedure and purpose of the study. All consenting patients/attendants were asked to sign a written informed consent form (in the language best understood by them). The information regarding each patient was kept confidential and was not revealed at any point of time.
Inclusion criteria
Age of 18–80 years of either gender presenting with moderate-to-severe LVSD (2D LVEF <40%) was included in the study.
Exclusion criteria
Patients in New York Heart Association (NYHA) IV patients of rheumatic heart disease or valvular heart disease poor echo window critically ill patients were excluded from the study.
Parameters studied
2D LVEF by Simpson’s biplane method
2D GLS using automated function imaging (AFI) technique.
After a detailed clinical history, an examination of all these patients was performed. Basic routine blood tests were done for all participants. Written informed consent for participation in this study was obtained.
Echo study was done with GE Healthcare, Vivid Ultrasound E95 echocardiography machine according to the American Society of Echocardiography guidelines.[27] Data acquisition was performed using a 5S transducer. 2D LVEF was assessed by Simpson’s biplane method of disks and noted. 2D GLS was calculated using the Automated Function Imaging technique using a-PLAX view, apical 4-chamber view, and apical 2-chamber view. The endocardial border was manually traced at an end-systolic frame and then the software automatically tracked these markers. A mean global strain value for the entire LV was automatically displayed on the bulls-eye map of LV strain. The Minnesota Living with HF questionnaire (MLHFQ) was used to assess the functional status of the patients with moderate-to-severe LVSD [Figure 1].[28] Patients were asked to grade their symptoms. Since many patients felt difficulty in scoring as per their symptoms, I modified the MLHFQ scoring system – if affected by the symptoms very little then a score of 1, if affected very much then a score of 3, intermediate grade symptoms then a score of 2 given. If the question was not applicable then a score of 0 was given, then the cumulative score was calculated.
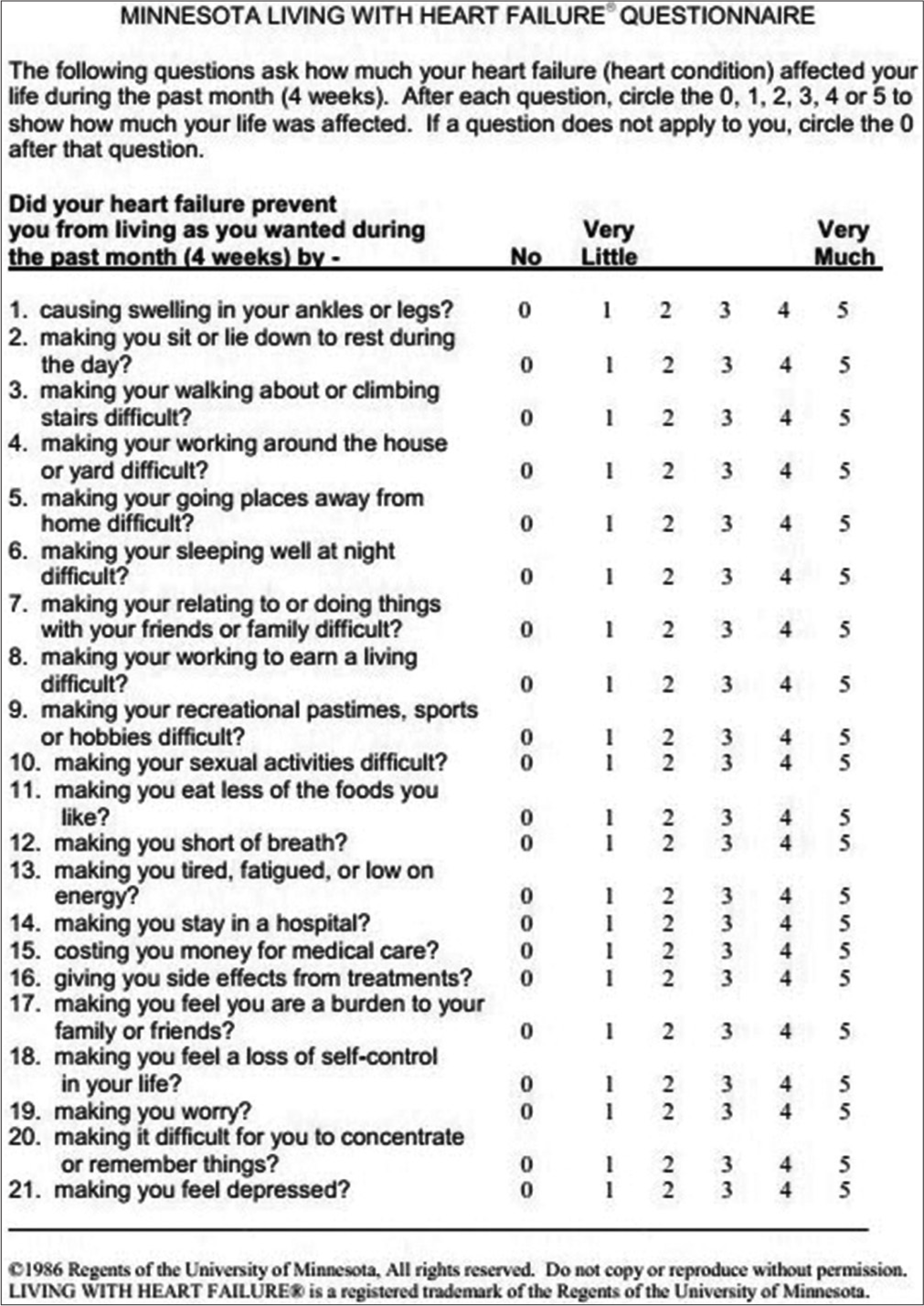
- Minnesota living with heart failure questionnaire.
Collected data were analyzed with appropriate statistical tests using the International Business Machines Statistical Package for the Social Sciences statistics for Windows, version 21.0. For uniformity reasons, categorical variables were presented as frequencies and percentages and were compared. The correlation coefficient (r) was used to calculate the association between GLS and functional status.
RESULTS
A total of 50 patients were included in this study.
The majority of the study population was of age ≥50 years (70%). The patient population consisted of 58% males and 42% females. Among the risk factors, 58% were hypertensive and 56% were diabetics. The majority of patients were of NYHA Class II functional class (58%) and the rest 42% patients were of NYHA Class III. About 26% of patients were taking angiotensin receptor neprilysin inhibitor (ARNI). The affordability of ARNI was found to be one of the important causes of the low percentage of the study population taking this class of drug. The majority of the patients coming to our hospital were referred from peripheral health institutions and they were attended by general practitioners – this accounts for most of the patients (92%) taking diuretics to relieve symptoms. About 76% of patients were on beta-blocker treatment, 64% of patients were taking angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, 64% were on dapagliflozin, and 54% of the patients were taking aspirin [Table 1].
| Variable | n(%) |
|---|---|
| Total number of patients | 50 |
| Age (years) | |
| <50 | 15 (30) |
| ≥50 | 35 (70) |
| Males | 29 (58) |
| Females | 21 (42) |
| Diabetes | 29 (58) |
| Hypertension | 28 (56) |
| NYHA class | |
| II | 29 (58) |
| III | 21 (42) |
| Treatment | |
| ARNI | 13 (26) |
| ACEI/ARB | 32 (64) |
| Beta-blocker | 38 (76) |
| Diuretics | 46 (92) |
| Dapagliflozin | 32 (64) |
| Aspirin | 27 (54) |
ARNI: Angiotensin receptor neprilysin inhibitor, ACEI/ARB: Angiotensin-converting enzyme inhibitors/angiotensin receptor blockers, NYHA: New York Heart Association
The mean 2D LVEF was found to be 32 ± 5.18. The mean 2D GLS was calculated to be −14.65 ± 3.82 and the mean MLHFQ score was 27.30 ± 9.64. The mean 2D LVEF in males was 31.28 ± 5.08 and, in females, it was 33.0 ± 5.27. The mean 2D GLS was found to be −13.98 ± 2.83 and −15.59 ± 4.79 in males and females, respectively. The mean MLHFQ score was 27.59 ± 7.99 in males and 26.90 ± 11.75 in females [Table 2].
| Parameters | 2D LVEF (Mean±SD) | 2D GLS (Mean±SD) | Functional status (MLHFQ score) (Mean±SD) |
|---|---|---|---|
| Overall | 32±5.18 | −14.65±3.82 | 27.30±9.64 |
| Male | 31.28±5.08 | −13.98±2.83 | 27.59±7.99 |
| Female | 33.0±5.27 | −15.59±4.79 | 26.90±11.75 |
2D: Two-dimensional, LVEF: Left ventricular ejection fraction, MLHFQ: Minnesota living with heart failure questionnaire, SD: Standard deviation, GLS: Global longitudinal strain
With the decrease in GLS, there was an increase in MLHFQ Score. Similarly, with the decrease in 2D LVEF, there was an increase in MLHFQ score [Figure 2a and b].
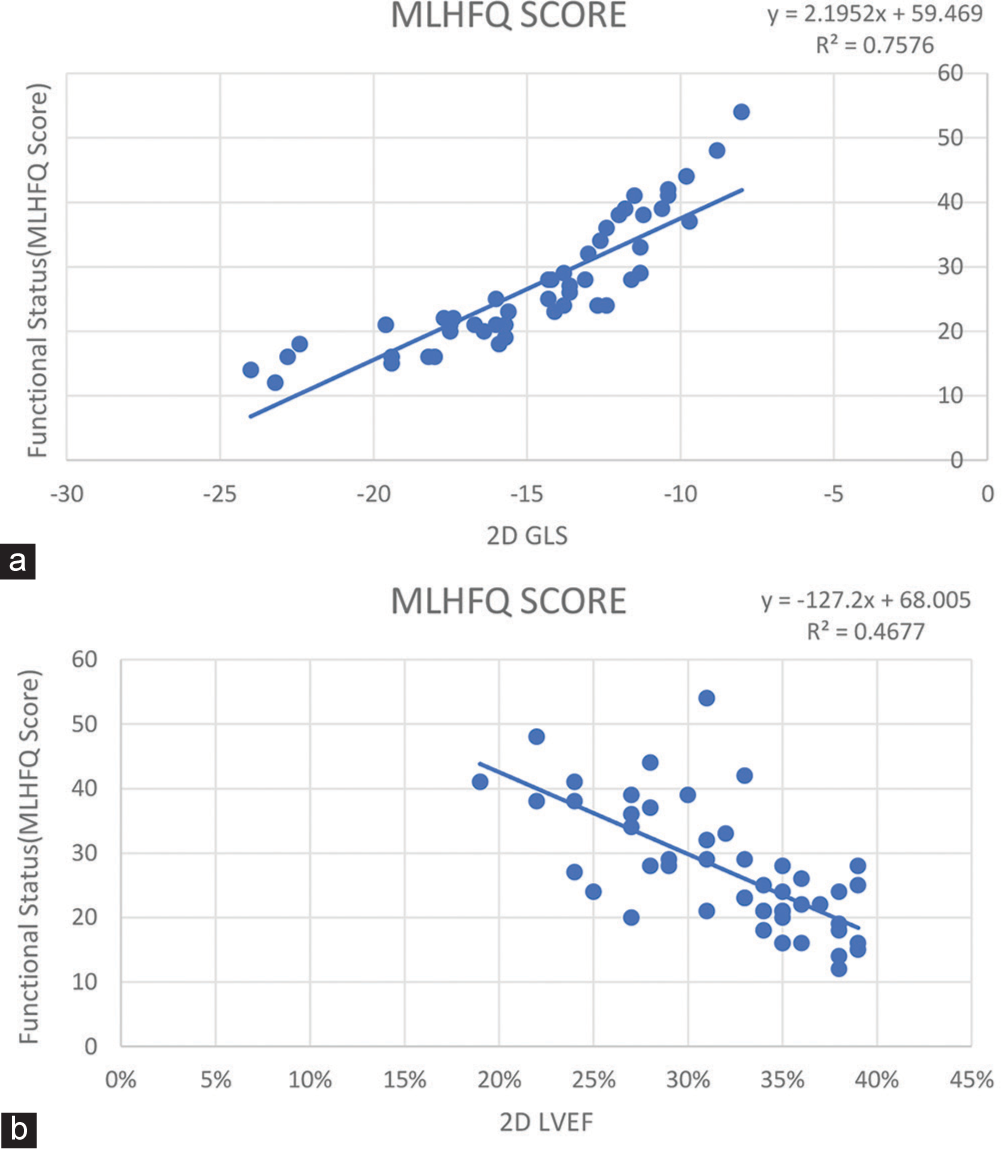
- (a) Correlation of 2D GLS with MLHFQ Score. (b) Correlation of 2D LVEF with MLHFQ Scor. (MLHFQ: Minnesota Living with Heart Failure Questionnaire, 2D GLS: 2 Dimensional Global Longitudinal Strain, 2D LVEF: 2 Dimensional Left Ventricular Ejection Fraction.)
The correlation coefficient between 2D LVEF and mean 2D GLS was 0.621 and the P-value for two-tailed tests of significance was <0.005. Hence, we conclude that there is a strong positive correlation between 2D LVEF and 2D GLS and the correlation is significant at the significance level of 0.01.
There was a strong negative correlation between 2D LVEF and MLHFQ score (functional status). The correlation coefficient between them was −0.684 and the P-value for two-tailed tests of significance was <0.005.
Similarly, the correlation coefficient between the MLHFQ score and mean 2D GLS was −0.870 and the P-value for two-tailed tests of significance was <0.005. There was a strong negative correlation between MLHFQ score and 2D GLS and the correlation was significant at the significance level of 0.01 [Table 3].
| Sex | 2D LVEF | Mean 2D GLS | MLHFQ Score | |
|---|---|---|---|---|
| Sex | 1 | |||
| 2D LVEF | 1 | 0.621** | -0.684** | |
| Mean 2D GLS | 0.621** | 1 | -0.870** | |
| MLHFQ Score | -0.684** | -0.870** | 1 |
2D LVEF: 2-Dimensional Left Ventricular Ejection Fraction,
2D GLS:2-Dimensional Global Longitudinal Strain,
MLHFQ: Minnesota Living with Heart Failure Questionnaire
It was observed that 2D GLS is better correlated with the functional status of the patients than 2D LVEF, although both were found to be statistically significant [Figure 3 and Table 4].
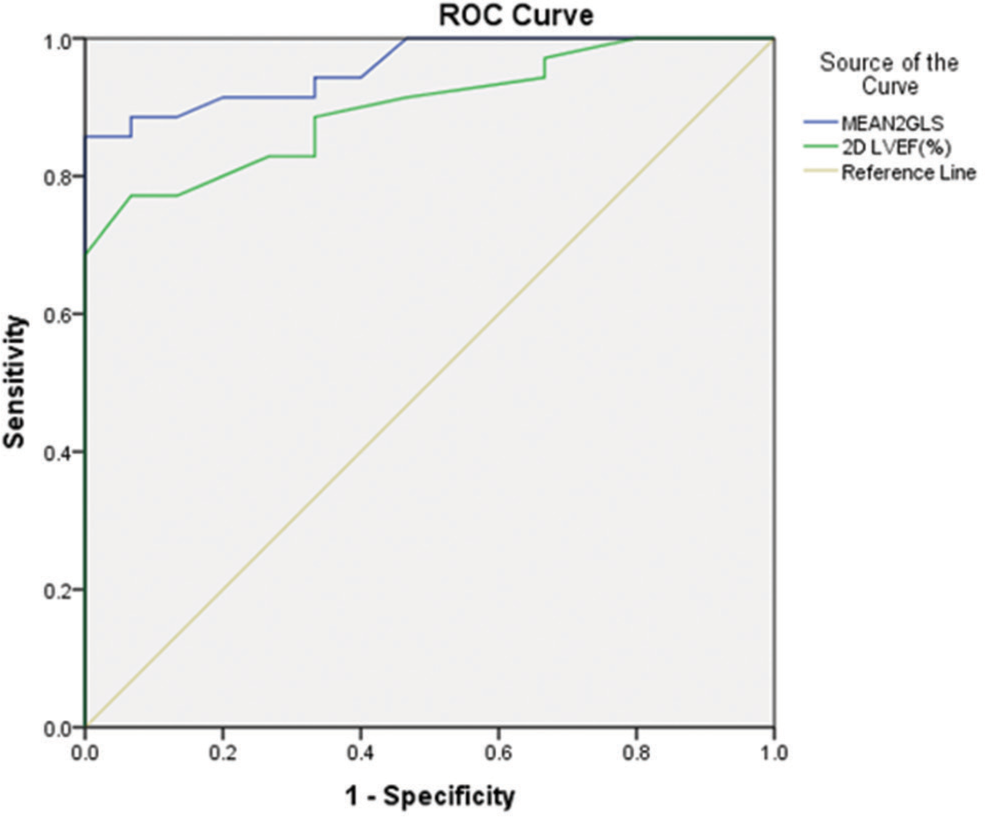
- Comparison between correlation of 2D GLS-MLHFQ score and 2D LVEF-MLHFQ score using ROC curve. (MLHFQ: Minnesota living with heart failure questionnaire, 2D LVEF: 2 Dimensional left ventricular ejection fraction, 2D GLS: 2 Dimensional global longitudinal strain, ROC: Receiver operating characteristic. MEAN 2GLS: Mean 2 dimensional Global Longitudinal Strain.)
| Test result variables | AUC | Std. error |
|---|---|---|
| Mean 2D GLS | 0.959 | 0.024 |
| Mean 2D LVEF | 0.899 | 0.042 |
LVEF: Left ventricular ejection fraction, AUC: Area under the curve, 2D GLS: 2 Dimensional global longitudinal strain, ROC: Receiver operating characteristics
In the study, no statistically significant difference was observed between both genders.
DISCUSSION
Although 2D LVEF is the most commonly used parameter to assess LV function, in the past decade, GLS has emerged as a new modality for LV function assessment which is more sensitive and reproducible. STE is used as a novel technique to allow the assessment of 2D GLS and there is a paucity of studies that correlated the functional status of the patients with 2D GLS, so this study compared both parameters (2D LVEF and 2D GLS) with the functional status of patients and the results showed that 2D GLS had a better correlation.
Stanton et al. conducted a study on 546 patients to compare GLS with standard measures such as EF and wall motion score index. They found that 2D GLS assessed with 2D STE had an incremental value over LVEF in the prediction of outcome. This study also showed that 2D GLS assessment was more reproducible as compared with 2D LVEF assessment.[29]
Bertini et al. took 1060 patients with chronic ischemic cardiomyopathy and evaluated the prognostic value of GLS as a new index of LV systolic function to predict long-term outcomes. During follow-up, compared with survivors, patients who died had greater impairment of LV GLS (P < 0.001). They concluded that the assessment of LV GLS with speckle-tracking echocardiography is significantly related to long-term outcomes in patients with chronic ischemic cardiomyopathy.[30]
Radwan and Hussein included 80 patients with stable angina and evaluated the diagnostic accuracy of LV GLS obtained by 2D STE in the prediction of the severity of coronary artery disease (CAD). The study showed that there was an incremental significant decrease in GLS with an increasing number of coronary vessels involved. They concluded that the measurement of GLS using 2D STE is a sensitive and accurate tool in the prediction of severe CAD.[31]
Sengeløv et al. conducted a study on 1065 HFrEF patients to investigate the prognostic value of GLS to all-cause mortality. They found that GLS was an independent predictor of all-cause mortality in HFrEF patients, especially in male patients without AF. Furthermore, GLS was a superior prognosticator compared with all other echo parameters. They found that GLS did not predict mortality in women. They concluded that these findings may indicate an intrinsic difference in the cardiac architecture, physiology, and LV systolic performance between men and women, and further studies are needed to clarify the exact underlying mechanism of the cardiac differences between sexes.[32]
In the present study, the mean 2D LVEF was found to be 32 ± 5.18. The mean 2D GLS was calculated to be −14.65 ± 3.82 and the mean MLHFQ score was 27.30 ± 9.64. The mean 2D LVEF in males was 31.28 ± 5.08 and, in females, it was 33.0 ± 5.27. The mean 2D GLS was found to be −13.98 ± 2.83 and −15.59 ± 4.79 in males and females, respectively. The mean MLHFQ score was 27.59 ± 7.99 in males and 26.90 ± 11.75 in females.
There was a strong negative correlation between 2D LVEF and MLHFQ score (functional status). The correlation coefficient between them was −0.684 and the P-value for two-tailed tests of significance was <0.005.
There was a strong negative correlation between 2D GLS and MLHFQ score and the correlation was significant at the significance level of 0.01. The correlation coefficient was −0.870 and the P-value for two-tailed tests of significance was <0.005.
The area under the curve for 2D GLS was found to be more than that of 2D LVEF (0.959 vs. 0.899).
In this study, 2D GLS is better correlated with the functional status of the patients than 2D LVEF, although both were found to be statistically significant.
The correlation coefficient between gender and 2D GLS was 0.210 (P = 0.144), gender and 2D LVEF was −0.166 (P = 0.250), and between gender and MLHFQ score was 0.035 (P = 0.808). In the present study, we did not find any statistically significant difference between both genders.
Limitations
The number of patients in the study was small
This was a single-center study of short duration (2 months)
Long-term follow-up was not done
Radial and circumferential strains were not explored
Assessment of LV filling pressure and PAH was not done in the present study.
CONCLUSION
2D GLS with STE is significantly related to the functional status of the patients with moderate-to-severe LVSD. The stratification of patients with abnormal LV function would be better predicted using GLS than conventional echo parameters such as 2D LVEF measured by Simpson’s method. Hence, along with 2D LVEF, 2D GLS should also be measured in daily clinical practice for better management of the patients. In the present study, no significant difference was observed between male and female patients. Further studies are needed to identify the gender differences in 2D GLS correlation with the functional status of patients with LVSD.
Acknowledgments
I would like to thank my professor and HOD for their guidance and the staff of the Cardiology department of my hospital for their support, as well as all the patients who participated in the study.
Ethical approval
The research/study was approved by the Institutional Review Board at MKCG Medical College, Berhampur, number 1260, dated 13 September 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Audio summary available at
Financial support and sponsorship
Nil.
References
- 2D and 3D Echocardiography-Derived Indices of Left Ventricular Function and Shape: Relationship With Mortality. JACC Cardiovasc Imaging. 2018;11:1569-79.
- [CrossRef] [PubMed] [Google Scholar]
- Tissue Doppler Imaging a New Prognosticator for Cardiovascular Diseases. J Am Coll Cardiol. 2007;49:1903-14.
- [CrossRef] [PubMed] [Google Scholar]
- Reconstructed Versus Real-time 3-Dimensional Echocardiography: Comparison with Magnetic Resonance Imaging. J Am Soc Echocardiogr. 2007;20:862-8.
- [CrossRef] [PubMed] [Google Scholar]
- Quantification of the Spectrum of Changes in Regional Myocardial Function during Acute Ischemia in Closed Chest Pigs: An Ultrasonic Strain Rate and Strain Study. J Am Soc Echocardiogr. 2001;14:874-84.
- [CrossRef] [PubMed] [Google Scholar]
- Muscle Afferent Inputs from the Hand Activate Human Cerebellum Sequentially through Parallel and Climbing Fiber Systems. Clin Neurophysiol. 2003;114:2107-17.
- [CrossRef] [PubMed] [Google Scholar]
- Noninvasive Myocardial Strain Measurement by Speckle Tracking Echocardiography: Validation against Sonomicrometry and Tagged Magnetic Resonance Imaging. J Am Coll Cardiol. 2006;47:789-93.
- [CrossRef] [PubMed] [Google Scholar]
- Experimental Validation of Circumferential, Longitudinal, and Radial 2-dimensional Strain during Dobutamine Stress Echocardiography in Ischemic Conditions. J Am Coll Cardiol. 2008;51:149-57.
- [CrossRef] [PubMed] [Google Scholar]
- Automated Function Imaging: A New Operator-independent Strain Method for Assessing Left Ventricular Function. Arch Cardiovasc Dis. 2008;101:163-9.
- [CrossRef] [PubMed] [Google Scholar]
- An Ultrasound Speckle Tracking (Two-Dimensional Strain) Analysis of Myocardial Deformation in Professional Soccer Players Compared with Healthy Subjects and Hypertrophic Cardiomyopathy. Am J Cardiol. 2007;100:128-32.
- [CrossRef] [PubMed] [Google Scholar]
- Global and Regional Myocardial Function Quantification by Two-dimensional Strain: Application in Hypertrophic Cardiomyopathy. J Am Coll Cardiol. 2006;47:1175-81.
- [CrossRef] [PubMed] [Google Scholar]
- Global Longitudinal Strain: A Useful Everyday Measurement? Echo Res Pract. 2016;3:85-93.
- [CrossRef] [PubMed] [Google Scholar]
- Universal Definition and Classification of Heart Failure: A Report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure: Endorsed by the Canadian Heart Failure Society, Heart Failure Association of India, Cardiac Society of Australia and New Zealand, and Chinese Heart Failure Association. Eur J Heart Fail. 2021;23:352-80.
- [CrossRef] [PubMed] [Google Scholar]
- 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;62:e147-239.
- [Google Scholar]
- Assessment of Left Ventricular Ejection Fraction and Volumes by Real-time, Two-dimensional Echocardiography. A Comparison of Cineangiographic and Radionuclide Techniques. Circulation. 1979;60:760-6.
- [CrossRef] [PubMed] [Google Scholar]
- Recommendations for Chamber Quantification: A Report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, Developed in Conjunction with the European Association of Echocardiography, a Branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440-63.
- [CrossRef] [PubMed] [Google Scholar]
- The Association of Left Ventricular Ejection Fraction, Mortality, and cause of Death in Stable Outpatients with Heart Failure. J Am Coll Cardiol. 2003;42:736-42.
- [CrossRef] [PubMed] [Google Scholar]
- Echocardiographic Assessment of Left Ventricular Systolic Function: From Ejection Fraction to Torsion. Heart Fail Rev. 2016;21:77-94.
- [CrossRef] [PubMed] [Google Scholar]
- Myocardial Strain Imaging: How Useful is it in Clinical Decision Making? Eur Heart J. 2016;37:1196-207.
- [CrossRef] [PubMed] [Google Scholar]
- Introduction of Tissue Doppler Imaging Echocardiography-Based on Pulsed-Wave Mode. J Med Ultrasound. 2008;16:202-9.
- [CrossRef] [Google Scholar]
- Tissue Tracking Technology for Assessing Cardiac Mechanics: Principles, Normal Values, and Clinical Applications. JACC Cardiovasc Imaging. 2015;8:1444-60.
- [CrossRef] [PubMed] [Google Scholar]
- Imaging Techniques for Cardiac Strain and Deformation: Comparison of Echocardiography, Cardiac Magnetic Resonance and Cardiac Computed Tomography. Expert Rev Cardiovasc Ther. 2013;11:221-31.
- [CrossRef] [PubMed] [Google Scholar]
- Studying Diastology with Speckle Tracking Echocardiography: The Essentials. Ann Card Anaesth. 2017;20:S57-60.
- [CrossRef] [PubMed] [Google Scholar]
- Strain and Strain Rate Imaging by Echocardiography-Basic Concepts and Clinical Applicability. Curr Cardiol Rev. 2009;5:133-48.
- [CrossRef] [PubMed] [Google Scholar]
- Global Longitudinal Strain by Echocardiography Predicts Long-term Risk of Cardiovascular Morbidity and Mortality in a Low-risk General Population: The Copenhagen City Heart Study. Circ Cardiovasc Imaging. 2017;10:e005521.
- [CrossRef] [PubMed] [Google Scholar]
- Feature-Tracking Global Longitudinal Strain Predicts Death in a Multicenter Population of Patients With Ischemic and Nonischemic Dilated Cardiomyopathy Incremental to Ejection Fraction and Late Gadolinium Enhancement. JACC Cardiovasc Imaging. 2018;11:1419-29.
- [CrossRef] [PubMed] [Google Scholar]
- Ventricular Longitudinal Shortening is an Independent Predictor of Death in Heart Failure Patients with Reduced Ejection Fraction. Sci Rep. 2021;11:20280.
- [CrossRef] [PubMed] [Google Scholar]
- Recommendations for Cardiac Chamber Quantification by Echocardiography in Adults: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1-39.e14.
- [CrossRef] [PubMed] [Google Scholar]
- Activity Questionnaires; a Useful Tool in Accessing Heart Failure Patients. Int J Cardiol. 2005;105:294-9.
- [CrossRef] [PubMed] [Google Scholar]
- Prediction of all-cause Mortality from Global Longitudinal Speckle Strain: Comparison with Ejection Fraction and Wall Motion Scoring. Circ Cardiovasc Imaging. 2009;2:356-64.
- [CrossRef] [PubMed] [Google Scholar]
- Global Longitudinal Strain Predicts Long-term Survival in Patients with Chronic Ischemic Cardiomyopathy. Circ Cardiovasc Imaging. 2012;5:383-91.
- [CrossRef] [PubMed] [Google Scholar]
- Value of Global Longitudinal Strain by Two Dimensional Speckle Tracking Echocardiography in Predicting Coronary Artery Disease Severity. Egypt Heart J. 2017;69:95-101.
- [CrossRef] [PubMed] [Google Scholar]
- Global Longitudinal Strain is a Superior Predictor of All-Cause Mortality in Heart Failure With Reduced Ejection Fraction. JACC Cardiovasc Imaging. 2015;8:1351-9.
- [CrossRef] [PubMed] [Google Scholar]







