Translate this page into:
Right Ventricular Infarction in Inferior Wall Myocardial Infarction
Velam Vanajakshamma, MD, DM Department of Cardiology, SVIMS Tirupati 517507, Andhra Pradesh India vvanaja1966@yahoo.in
This article was originally published by Women in Cardiology and Related Sciences and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background Right ventricular infarction (RVI) is common in patients with inferior wall myocardial infarction (IWMI). Right ventricular involvement increases mortality and morbidity in IWMI patients. Clinical presentation of RVI differs, and accordingly treatment and management of patients also differs.
Aim To find out the frequency of RVI among patients with acute IWMI and to determine the utility of clinical examination, electrocardiography (ECG), and echocardiography (ECHO) in the diagnosis of RVI and its severity. Also o study the frequency and complications with reference to sex.
Material and Methods One hundred patients with acute IWMI were recruited. Clinical examination, ECG with right precordial leads, and 2D ECHO (right ventricular end-systolic volume [RVESV] and right ventricular end-diastolic volume [RVEDV], right ventricular stroke volume [RVSV], RVESV index [RVESVI], RVEDV index [RVEDVI], RVSV index [RVSVI], and right ventricular ejection fraction [RVEF]) were done to diagnose RVI and its severity. RVI patients were divided into two groups basing on RVEF as severe RVI (EF < 35%) and mild RVI (EF > 35%).
Results Forty-three (43%) patients had RVI. Thirty-one (72%) patients had mild RVI (EF > 35%) and 12 (28%) had severe RVI (EF < 35%). Clinical examination had less sensitivity (35%) and high specificity (93%) in the diagnosis of RVI whereas it was highly sensitive (100%) and specific (90%) in detecting severe RVI. Total ST elevation of ≥ 3 mm was highly sensitive (92%), and ≥ 5 mm was highly specific (94%) in detecting severe RVI. RVEF (p < 0.01), RVESVI (p < 0.01), RVEDVI (p < 0.01), RVSVI (p < 0.05), and total ST elevation (p < 0.01) were equally effective in detecting severe RVI. Case fatality rate in RVI was 7%. Proportional mortality rate in females was 67%, with higher mortality in females compared with males (p ≤ 0.05).
Conclusion Right-sided leads should be taken in all cases of acute IWMI. Careful clinical examination, total ST elevation in V1, V2, V3R, V4R, ECHO RVESV, RVEDV, RVSV, RVEF, RVESVI, RVEDVI, and RVSVI are useful in detecting severe RVI. Complications were significantly associated with the severity of RVI. Mortality is high in females compared with males.
Keywords
right ventricular infarction
inferior wall myocardial infarction
electrocardiography
echocardiography
Introduction
Myocardial infarction (MI) was generally regarded as an ischemic injury to the left ventricle. Right ventricle as the site of major damage from acute MI has been recognized clinically only recently.
Right ventricular infarction (RVI) was first described more than 70 years ago in autopsy studies. Between 1949 and 1959 several authors correlated electrocardiographic (ECG) and clinicopathologic findings in patients with MI and concluded that there were no definite ECG signs referable to right ventricular involvement, producing skepticism about the utility of ECG for diagnosis of RVI.1 2 3
In 1974 Cohn et al4 described the syndrome of predominant right ventricular dysfunction during acute inferior wall myocardial infarction (IWMI) and reported that hemodynamics deteriorate markedly and atrioventricular block tends to occur in patients with RVI, with a resulting increase in the hospital death rate. Since then the right ventricle that was the forgotten chamber has drawn much attention, and research was focused on RVI. This landmark study was followed by a renewed interest in the diagnosis of RVI by the use of noninvasive modalities such as ECG, echocardiography (ECHO), nuclear imaging studies, and invasive modalities like right-sided heart catheterization. Among these investigations, earlier investigators focused on the ECG diagnosis of RVI, because the right precordial leads provide the simplest and most objective data in the acute stage of infarction.
The diagnosis of RVI is important because the management of RVI differs from left ventricular infarction. The profound hemodynamic sequelae of RVI may be prevented by the administration of an appropriate intravenous volume load. If RVI is neglected or treated as left-sided heart failure with diuretics, cardiogenic shock may supervene. Nitrates are contraindicated in RVI,5 as RV function is preload dependant.
Depending on the various criteria used, approximately 50% of patients with IWMI have some involvement of the right ventricle,5 because both posterior wall of the right ventricle and the inferior wall of the left ventricle share a common blood supply, that is, usually the right coronary artery.6 7 8 RVI is rare because of lower oxygen demands of the right ventricle, rich intercoronary collateral system, thin right ventricle driving some nutrition from the blood with in right ventricular cavity itself,9 10 11 and systolic compressive forces of the left ventricle producing throttling effect on the left coronaries that drive blood from the left to right coronaries during systole.
Isolated RVI is seen in 3 to 5% of cases with preexisting right ventricular hypertrophy in which oxygen needs of the right ventricle are increased.9 10
Right-sided heart catheterization in every patient presenting with acute IWMI is an impracticable, noninvasive diagnosis. ECG to detect or to raise the suspicion of associated RVI at an early stage would be helpful. In search of reliable noninvasive diagnostic method to assess the severity of RVI, we prospectively evaluated 100 patients with acute IWMI by clinical symptoms/signs, ECG, and ECHO.
Material and Methods
This cross-sectional descriptive study was conducted in the coronary care unit of our hospital. One hundred patients with acute IWMI (ST elevation ≥ 1 mm in LII, LIII, and aVF) were taken into the study. Patients with history of previous MI and history of chronic obstructive pulmonary disease (COPD) were excluded from the study. Coronary risk factors were assessed. Clinical examination was done.
Clinically RVI was diagnosed if hypotension, elevated jugular venous pressure (JVP), pulsus paradoxus, and RV S3/S4 were present within 48 hours of admission.
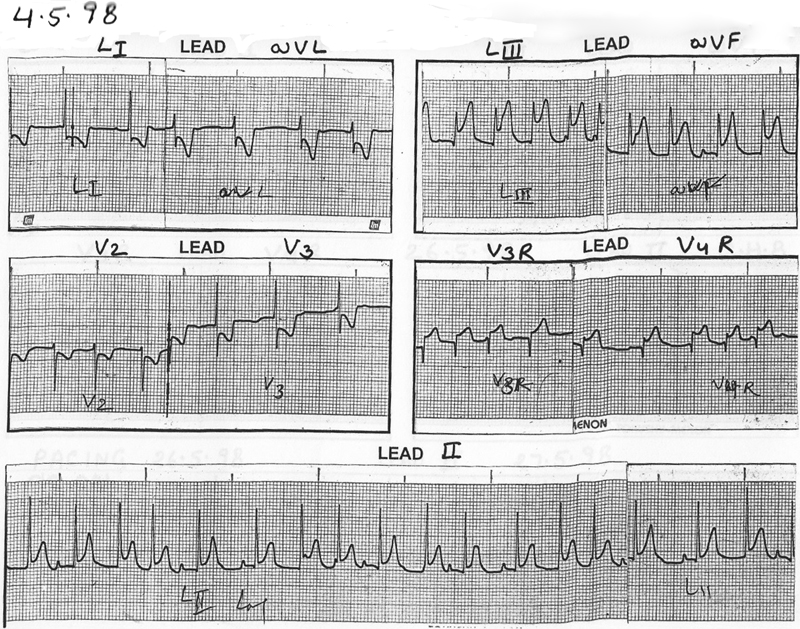
ECGs with right precordial leads were taken on admission, and total scoring of ST elevation in right precordial leads (V1, V2, V3R, and V4R) was done (Figs. 1, 2).

-
Fig. 1 Electrocardiography with right precordial leads on admission.
Fig. 1 Electrocardiography with right precordial leads on admission.
-
Fig. 2 Electrocardiography with right precordial leads on admission.
Fig. 2 Electrocardiography with right precordial leads on admission.
ECHO was done by using H.P. Sonos 2000 color-coded Doppler. Right ventricular end-systolic volume (RVESV) and right ventricular end-diastolic volume (RVEDV) were measured. RVESV index (RVESVI), RVEDV index (RVEDVI), right ventricular stroke volume (RVSV), RVSV index (RVSVI), and right ventricular ejection fraction (RVEF) were calculated. RVI patients were divided into two groups basing on RVEF as severe RVI (ejection fraction [EF] < 35%) and mild RVI (EF > 35%) (Figs. 3, 4).

-
Fig. 3 Short-axis view showing dilated right ventricle.
Fig. 3 Short-axis view showing dilated right ventricle.

-
Fig. 4 Apical four-chamber views showing dilated right ventricle.
Fig. 4 Apical four-chamber views showing dilated right ventricle.
An attempt to correlate coronary risk factors, clinical symptoms/signs, ECG, and ECHO evidence of right ventricular dysfunction (RVD) was made. Treatment was given according to RVI protocol. Frequency and complications with reference to sex were analyzed.
Statistical Analysis
The data were analyzed by calculating percentage in categories, chi-square test for significance of association, odds ratio (95% confidence interval [CI]) for strength of association, and Student's t-test for comparing mean values of ECG and ECHO.
Results
Among 100 patients of IWMI, 43 (43%) patients had RVI. Mean age of RVI patients was 53.3 ± 10 years (range: 30–77 years), male-to-female ratio was 6:1. We found RVS3/S4 in 12 (28%) patients, pulsus paradoxus in 7 (16%), elevated JVP in 7 (16%), and bradycardia in 5 (12%) patients. Thirty-nine (91%) patients, 3 (7%), and 1 (2%) patient were in Killip class I, II, and III and IV, respectively. Smoking was the major modifiable risk factor and seen in 65% patients. Hypertension, dyslipidemia, and diabetes were found in 47%, 47%, and 21%, respectively. Thirty-one (72%) patients had mild RVI (EF > 35%) and 12 patients (28%) had severe RVI (EF < 35%) (Table 1).
|
RVI severity grading |
No. |
% |
|---|---|---|
|
Mild RVI |
||
|
(EF > 35%) |
31 |
72 |
|
Severe RVI |
||
|
(EF < 35%) |
12 |
28 |
Abbreviations: EF, ejection fraction; RVEF, right ventricular ejection fraction; RVI, right ventricular infarction.
Severe RVI was more common in females, which was statistically significant (p < 0.01) (Table 2), whereas other risk factors did not have significant association with severe RVI (p > 0.05).
|
Sex |
No. of cases of severe RVI |
No. of cases of mild RVI |
Total |
Chi-square test, df, P |
OR (95% CI) |
|---|---|---|---|---|---|
|
Male |
7 |
29 |
36 |
7.83 |
1.00 |
|
Female |
5 |
2 |
7 |
1 |
10.35 |
|
Total |
12 |
31 |
43 |
< 0.01 |
(1.65–62.8) |
Abbreviations: CI, confidence interval; df, degrees of freedom; OR, odds ratio; P, p value; RVI, right ventricular infarction.
Clinical examination had less sensitivity (35%) and high specificity (93%) in the diagnosis of RVI whereas it was highly sensitive (100%) and specific (90%) in detecting severe RVI (Table 3).
|
Clinical examination |
Sensitivity (TP) (%) |
Specificity (TN) (%) |
PPV (%) |
NPV (%) |
Accuracy (%) |
|
|---|---|---|---|---|---|---|
|
a. |
Any one of 4 clinical signs |
100 |
90.3 |
80 |
100 |
93 |
|
b. |
Hypotension |
8.3 |
93.5 |
33 |
73 |
70 |
|
c. |
Pulsus paradoxus |
58.3 |
100 |
100 |
86 |
88.4 |
|
d. |
Elevated JVP |
58.3 |
100 |
100 |
86 |
88.4 |
|
e. |
RV S3/S4 |
91.7 |
96.8 |
92 |
97 |
95.3 |
Abbreviations: JVP, jugular venous pressure; NPV, negative predictive value; PPV, positive predictive value; RV, right ventricle; RVI, right ventricular infarction; TN, true negative; TP, true positive.
Total ST elevation of ≥ 3 mm was highly sensitive (92%), and ≥ 5 mm was highly specific (94%) in detecting severe RVI. ST elevation ≥β2 mm in V3R, V4R were less sensitive (67% and 71% respectively) and less specificity (77% and 84% respectively) in detecting severe RVI (Table 4).
|
ECG |
Sensitivity (TP) (%) |
Specificity (TN) (%) |
PPV (%) |
NPV (%) |
Accuracy (%) |
|
|---|---|---|---|---|---|---|
|
Total ST elevation in V1,V2, V3R, V4R |
||||||
|
a. |
1.≥ 3 mm |
91.7 |
54.8 |
44 |
94 |
65 |
|
2. ≥4 mm |
75 |
77.4 |
56 |
89 |
76.7 |
|
|
3. ≥5 mm |
58.3 |
93.5 |
78 |
85 |
83.7 |
|
|
b. |
ST elevation in V3R (≥2 mm) |
71.4 |
77.4 |
42 |
77 |
67.4 |
|
c. |
ST elevation in V4R (≥2 mm) |
66.7 |
83.9 |
62 |
87 |
70 |
Abbreviations: ECG, electrocardiogram; NPV, negative predictive value; PPV, positive predictive value; RVI, right ventricular infarction; TN, true negative; TP, true positive.
RVEF (p < 0.01), RVESVI (p < 0.01), RVEDVI (p < 0.01), RVSVI (p < 0.05), and total ST elevation (p < 0.01) were equally effective in detecting severe RVI (Table 5).
|
ECHO findings |
Severe RVI (12) |
Mild RVI (31) |
p Value |
|
|---|---|---|---|---|
|
a. |
RVESVI |
|||
|
Mean |
29.02 |
9.86 |
< 0.01 |
|
|
SD |
11.25 |
3.97 |
||
|
b. |
RVEDVI |
|||
|
Mean |
36.5 |
19.94 |
< 0.01 |
|
|
SD |
12.18 |
6.20 |
||
|
c. |
RVSVI |
|||
|
Mean |
7.3 |
10.8 |
< 0.05 |
|
|
SD |
4.37 |
4.68 |
||
|
B. |
ECG finding (total ST elevation V1,V2, V3R, V4R in mm) |
|||
|
Mean |
5.38 |
2.82 |
< 0.01 |
|
|
SD |
2.62 |
1.57 |
||
Abbreviations: ECHO, echocardiography; ECG, electrocardiogram; RVI, right ventricular infarction; RVESVI, right ventricular end-systolic velocity index; RVEDVI, right ventricular end-diastolic volume index; RVSVI, right ventricular stroke volume index; SD, standard deviation.
Correlation between total ST elevation and RVEF was computed and correlation coefficient r was −0.52. There was statistically significant negative linear correlation between total ST elevation and RVEF (p < 0.01, t = 2.84, degrees of freedom [df] = 41). Case fatality rate in RVI was 7%. Proportional mortality rate in females was 67%, with higher mortality in females compared with males (p ≤ 0.05) (Table 6).
|
Dead |
Alive |
Total |
Chi-square, df, P |
OR (95% CI) |
|
|---|---|---|---|---|---|
|
Male |
1 |
35 |
36 |
5.91, |
1.00 |
|
Female |
2 |
5 |
7 |
1, |
14 |
|
Total |
3 |
40 |
43 |
< 0.05 |
(1.06–184.9) |
Abbreviations: df, degrees of freedom; OR, odds ratio; P, p value; RVI, right ventricular infarction.
Discussion
The frequency of RVI in IWMI was 43%, which is in accordance with other studies (50%).5
There was no specific symptom pertaining to RVI as compared with IWMI. Smoking was the major risk factor that ranks next to age and sex. When differences in the frequency of IWMI and RVI in relation to coronary risk factors were considered, there was no statistically significant difference. The clinical signs had less sensitivity (35%) and less specificity (68%) in detecting RVI, which is in accordance with other studies12 and in contrast to the study of Shantaram et al according to which clinical signs were present in 80% of cases.13
According to the study conducted by Braat et al,14 sensitivity and specificity of V3R is 69% and 97%, of V4R is 93% and 95%, which were high. Based on this and so many other studies,14 15 16 17 V3R and V4R were taken for diagnosing RVI. In our study, RVI patients were divided into two groups as severe and mild based on ECHO RVEF < 0.35 and > 0.35, respectively. Twelve patients had severe RVI (28%) and 31 had mild RVI (72%).
In the present study, clinical examination showed 100% sensitivity, 90% specificity, and 93% accuracy in detecting severe RVI.
RVI patients were divided into two groups based on the number of risk factors ≥ 5, < 5, and were found to have no relationship to the number of risk factors and severity of RVI (p > 0.05).
In the present study, a cutoff valve was given to total ST elevation in V1, V2, V3R, V4R, and found that total ST elevation of ≥ 3 mm had 92% sensitivity, 55% specificity with 65% accuracy; ≥ 4 mm had 75% sensitivity, 77% specificity with 77% accuracy; and ≥ 5 mm had 58% sensitivity, 94% specificity with 84% accuracy in detecting severe RVI. ST elevation of ≥ 2 mm in V3R had 71% sensitivity, 77% specificity with 67% accuracy, and V4R had 67% sensitivity, 84% specificity, and 70% accuracy in detecting severe RVI. Total ST elevation had high sensitivity and specificity when compared with V3R or V4R alone in detecting severity. Total ST elevation compared with RVEF by using Student's t-test found statistical significant association (p < 0.01), and there was statistically significant negative linear correlation between these two variables (r = − 0.52, p < 0.01), similar to Hasche et al18 who studied the severity of anterior wall infarction in relation to total ST elevation.
In RVI patients, other ECHO variables such as RVESVI, RVEDVI, and RVSVI were compared for association with RVEF by using Student's t-test, and a statistically significant association among these variables was found (p < 0.01, < 0.01, and < 0.05, respectively). This is in accordance with other studies.15 19 20 21
In the present study, severe RVI was associated with high mortality that is comparable to the study conducted by Mavrić et al.22 In the present study, severe RVI was 10 times more common, and mortality was 14 times higher in females, which is similar to the study conducted by Pell et al.23
Conclusion
Careful clinical examination, total ST elevation in V1, V2, V3R, V4R, ECHO end-systolic, end-diastolic, stroke volumes, and EF of the right ventricle are useful in detecting severe RVI. Complications were significantly associated with the severity of RVI. Mortality is high in females compared with males.
Funding
None.
Conflict of Interest
None.
References
- Correlation of electrocardiographic and pathologic findings in infarction of the interventricular septum and right ventricle. Am Heart J. 1949;37(05):720-770.
- [Google Scholar]
- Difficulties in the electrocardiographic diagnosis of myocardial infarction. Am Heart J. 1950;39(02):243-262.
- [Google Scholar]
- The pathogenesis of infarction of the right ventricle. Br Heart J. 1959;21(04):545-554.
- [Google Scholar]
- Right ventricular infarction. Clinical and hemodynamic features. Am J Cardiol. 1974;33(02):209-214. ; Clinical and Hemodynamic Features.
- [Google Scholar]
- Anatomy of the coronary arteries in health and disease. Circulation. 1965;32(06):1020-1033.
- [Google Scholar]
- Angiology Gray's Anatomy. 38th ed. London: Churchill Livingstone; 1992. p. :727-731. . In: , ed.
- [Google Scholar]
- Coronary Arteriography. Braunwald Heart Disease. 5th ed, Volume 1. Philadelphia, PA: W.B. Saunders; 1997. p. :247-252. Eugene Braunwald MD. FRCP ed.
- [Google Scholar]
- Infarction of the heart II. Clinical course and morphological findings. Ann Intern Med. 1938;12:71-94.
- [Google Scholar]
- Physical examination for exclusion of hemodynamically important right ventricular infarction. Ann Intern Med. 1983;99(05):608-611.
- [Google Scholar]
- Right ventricular infarction. Clinical, ECG and echocardiographic profile. Indian Heart J. 1987;18(01):27-30.
- [Google Scholar]
- Value of electrocardiogram in diagnosing right ventricular involvement in patients with an acute inferior wall myocardial infarction. Br Heart J. 1983;49(04):368-372.
- [Google Scholar]
- ST-segment elevation in right precordial leads implies depressed right ventricular function after acute inferior myocardial infarction. Am Heart J. 1998;135(04):689-695.
- [Google Scholar]
- Electrocardiographic diagnosis of right ventricular infarction. Am J Med. 1981;70(06):1175-1180.
- [Google Scholar]
- The early recognition of right ventricular infarction: diagnostic accuracy of the electrocardiographic V4R lead. Circulation. 1983;67(03):558-565.
- [Google Scholar]
- Relation between ischemia time, infarct size, and left ventricular function in humans. Circulation. 1995;92(04):710-719.
- [Google Scholar]
- The noninvasive diagnosis of right ventricular infarction. Circulation. 1978;57(03):483-490.
- [Google Scholar]
- Relations between Doppler tracings of pulmonary regurgitation and invasive hemodynamics in acute right ventricular infarction complicating inferior wall left ventricular infarction. Am J Cardiol. 1995;75(07):425-430.
- [Google Scholar]
- Right ventricular dysfunction in acute inferoposterior myocardial infarction. An echocardiographic and isotopic study. Chest. 1985;87(03):307-314.
- [Google Scholar]
- Prognostic significance of complete atrioventricular block in patients with acute inferior myocardial infarction with and without right ventricular involvement. Am Heart J. 1990;119(04):823-828.
- [Google Scholar]
- Trends in the incidence of myocardial infarction and in associated mortality and morbidity in a large employed population, 1957–1983. N Engl J Med. 1985;312(16):1005-1011.
- [Google Scholar]







