Translate this page into:
Pheochromocytoma Masquerading as Acute Coronary Syndrome and Takotsubo Cardiomyopathy: A Diagnostic Dilemma in the Elderly
*Corresponding author: Ajinkya Vijay Mahorkar, Department of Cardiology, Avanti Institute of Cardiology, Dhantoli, Nagpur, India. ajinkyamahorkar1@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mahorkar AV, Mahorkar VU, Vidhale A, Donkalwar A. Pheochromocytoma Masquerading as Acute Coronary Syndrome and Takotsubo Cardiomyopathy: A Diagnostic Dilemma in the Elderly. Indian J Cardiovasc Dis Women. 2025;10:59-62. doi: 10.25259/IJCDW_46_2024
Abstract
This case delineates the intricate diagnostic challenges encountered in a 70-year-old woman presenting with chest tightness and severe shortness of breath, initially suggestive of acute coronary syndrome and Takotsubo cardiomyopathy. Despite inconclusive findings on emergency cardiac catheterization, subsequent evaluation unveiled an underlying pheochromocytoma. The patient’s journey from an initial misdiagnosis to the identification of the adrenal mass, successful medical and surgical management, and stable 2-year follow-up highlights the importance of considering rare etiologies in the elderly population.
Keywords
Pheochromocytoma
Acute coronary syndrome
Takotsubo cardiomyopathy
INTRODUCTION
The atypical presentation of pheochromocytoma, a rare neuroendocrine tumor, as acute coronary syndrome (ACS) and Takotsubo cardiomyopathy (TCMP) poses a formidable diagnostic challenge. This case emphasizes the critical need for heightened clinical suspicion and thorough investigation in elderly patients presenting with cardiovascular symptoms that defy conventional diagnostic paradigms. The patient’s journey, from initial suspicions of ACS and Takotsubo CMP to the ultimate discovery of an adrenal mass, underscores the complexity of differential diagnoses in this demographic.
CASE REPORT
A 70-year-old woman presented to the emergency department with chest tightness and severe shortness of breath. On arrival, her pulse was 80 beats/min, regular, and her blood pressure was 150/92 mmHg. Electrocardiogram revealed sinus tachycardia and T-wave inversions in leads V1 to V6 [Figure 1]. Elevated troponins (Hs Trop I - 3708) and a 2D echocardiogram showing apical hypokinesia with a left ventricular ejection fraction (EF) of 40% raised suspicion for ACS, prompting emergency cardiac catheterization. Unexpectedly, no significant coronary artery stenosis was found, and only coronary ectasia was noted. A detailed 2D echocardiogram was repeated, revealing apical dilatation and hypokinesis with basal hyperkinesia, suggesting TCMP [Video 1] but without an evident stressor. During her stay, the patient had labile hypertension treated with telmisartan and metoprolol and was discharged after 2 days in a stable condition.
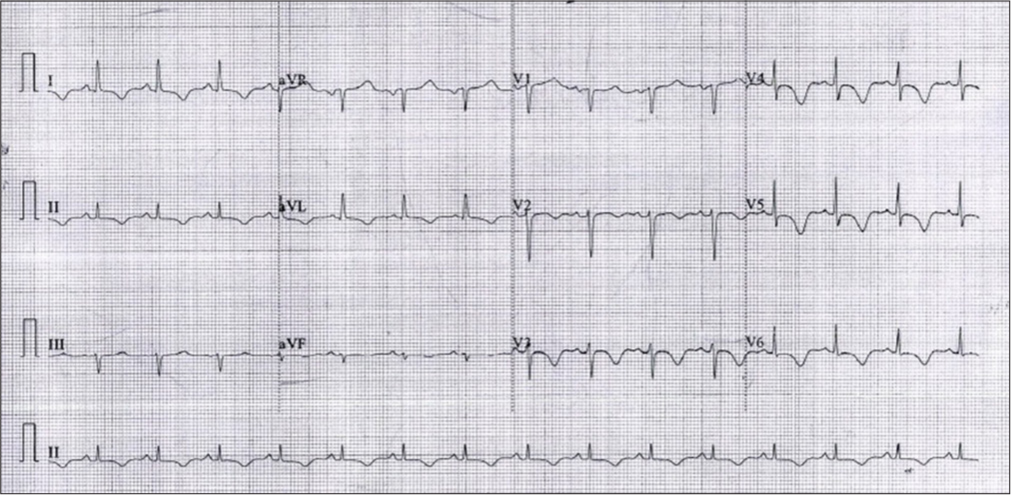
- Electrocardiogram at the first presentation.
Video 1:
Video 1:Echo at showing apical dilatation and left ventricular dysfunction suggestive of Takotsubo cardiomyopathy.A week later, the patient was presented to another hospital with a severe headache, palpitations, and a blood pressure of 180/120 mmHg, and was treated as a hypertensive emergency. Following initial management and stabilization, she was transferred to our hospital for further evaluation. On arrival, her vital signs showed a pulse rate of 110 beats/min and a blood pressure of 154/96 mmHg. A transthoracic echocardiogram showed normalization of her previous LV dysfunction, with an EF of 60% [Video 2]. We exclude other potential causes of reversible cardiomyopathies such as iron overload, sarcoidosis, thyrotoxicosis, alcoholism, and hypocalcemia through a thorough medical history, clinical evaluation, and appropriate laboratory investigations.
Video 2:
Video 2:Echo after 1 week showing normalization of previous echo findings.Further investigations for labile hypertension revealed elevated levels of serum-free metanephrines (1346 pg/mL; normal <65 pg/mL) and serum-free normetanephrines (6207 pg/mL; normal <196 pg/mL), confirming the diagnosis of pheochromocytoma. A computed tomography abdomen scan identified a large, well-defined left supra-adrenal mass [Figure 2]. The patient was started on α-blockers, followed by β-blockers after effective blood pressure management. Tumor resection was performed following blood pressure control [Figure 3]. The patient has remained stable for 2-year post-surgery, with mild hypertension as the only ongoing medical concern. This case underscores the complex interplay of cardiovascular and endocrine disorders, highlighting the need for a comprehensive diagnostic and management approach in elderly patients.

- Computed Tomography of the abdomen showing a large left adrenal mass (indicated by yellow arrow).

- Pheochromocytoma after excision.
DISCUSSION
Pheochromocytoma, a rare neuroendocrine tumor arising from chromaffin cells, poses significant diagnostic challenges due to its highly variable clinical presentation. These tumors secrete excessive catecholamines, leading to diverse cardiovascular manifestations such as hypertension, tachycardia, myocardial infarction, and cardiomyopathies, including TCMP. This discussion synthesizes relevant literature while contextualizing the diagnostic journey of our patient, emphasizing the critical need for heightened clinical suspicion in atypical presentations.
TCMP, often referred to as “stress cardiomyopathy,” is a reversible form of left ventricular dysfunction typically triggered by emotional or physical stress. Merchant et al.’s case series highlights the variability in presentation, encompassing symptoms such as chest pain, dyspnea, and syncope, with a predilection for postmenopausal women (mean age ~63 years) and a female-to-male ratio of approximately 9:1. The hallmark echocardiographic finding is apical ballooning with transient left ventricular dysfunction, typically resolving within weeks. Although commonly associated with emotional stressors, atypical triggers, including catecholamine surges in pheochromocytoma, are increasingly recognized.[1]
Dewi and Saraswati’s case series on pheochromocytoma elucidates the broad spectrum of presentations, ranging from asymptomatic cases to life-threatening hypertensive crises and cardiac complications. Among 15 cases, hypertension was the predominant feature (present in 80% of patients), with episodic symptoms such as palpitations, headache, and sweating. The study also highlighted gender differences, with females comprising a higher proportion of cases (60%) and a median diagnostic age of 45 years. Cardiac manifestations, including arrhythmias, heart failure, and TCMP, were observed in a subset, underscoring the tumor’s cardiovascular impact.[2]
As clear from the above discussion, TCMP and pheochromocytoma demonstrate notable gender predilections. TCMP predominantly affects postmenopausal women, likely due to reduced estrogen’s cardioprotective effects. Conversely, pheochromocytoma, though less common, shows a slight female predominance, with cases frequently diagnosed in middle-aged individuals. Our case, involving an elderly woman, is less typical but highlights the disease’s occurrence across age groups.
A systemic analysis by Batisse-Lignier Marie analyzed 145 cases of pheochromocytoma-induced cardiomyopathies, comprising 49 Takotsubo cardiomyopathies (TCMP) and 96 other catecholamine cardiomyopathies (CC). Both groups shared a severe clinical presentation, including high blood pressure (87.7%) and shock (51.0%), but acute pulmonary edema was more frequent in CC (58.3% vs. 38.8%). TCMP was associated with significantly better left ventricular recovery rates both before (64.9% vs. 40.8%) and after surgical resection (97.7% vs. 73.3%). The findings highlight the need to investigate pheochromocytoma or paraganglioma in cases of unexplained cardiomyopathy or TCMP.[3]
The cardiovascular complications of pheochromocytoma stem from catecholamine-induced mechanisms: Coronary vasospasm, intracellular calcium overload, and myocardial energy metabolism disruption. Behonick et al. elaborate on oxidative stress metabolites’ role in catecholamine cardiotoxicity, contributing to troponin elevation and myocardial dysfunction.[4] Cardiac biomarkers are often raised in pheochromocytoma-induced cardiotoxicity but are often mild compared to ACS,[5] which should raise suspicion in the minds of clinician regarding alternative causes in such scenarios.
Our patient’s initial presentation with ACS, characterized by chest pain, elevated cardiac biomarkers, and diffuse ST-segment abnormalities, mirrors findings commonly reported in pheochromocytoma-associated cardiac complications. Despite a normal coronary angiogram, the absence of a clear emotional stressor and labile hypertension should have raised suspicion for an underlying endocrine disorder. Notably, echocardiography revealed transient apical hypokinesis and left ventricular dysfunction, consistent with TCMP but atypical in the absence of stress triggers.
The delayed diagnosis underscores the challenges in recognizing pheochromocytoma masquerading as ACS and TCMP. As seen in similar cases, catecholamine surges in[6,7] pheochromocytoma can provoke TCMP-like patterns, including inverted variants. Unlike classical TCMP, where symptoms resolve with supportive care, our patient’s hypertensive urgency prompted further evaluation, ultimately revealing the underlying tumor. This highlights the importance of comprehensive diagnostic workups in atypical cases of ACS with labile hypertension.
What distinguishes our case is the convergence of multiple rare phenomena: An elderly woman presenting with ACS-like symptoms, TCMP without an evident stressor, and a delayed diagnosis of pheochromocytoma. This confluence of features underscores the diagnostic dilemma, emphasizing the need for heightened awareness among clinicians. Prompt recognition and management, including alpha-adrenergic blockade and surgical resection, resulted in symptom resolution and favorable outcomes, aligning with findings in the literature.[2,7]
CONCLUSION
This case underscores the deceptive nature of pheochromocytoma, which can masquerade as ACS and TCMP, particularly in the elderly. A detailed review of the literature and our patient’s clinical course highlights the importance of considering pheochromocytoma in patients presenting with ACS-like symptoms, labile hypertension, and atypical TCMP. Comprehensive diagnostic evaluations, including endocrine workups, are paramount to avoid misdiagnosis and ensure timely intervention. Clinicians must remain vigilant for this rare yet treatable entity to improve patient outcomes.
Ethical approval:
Institutional review board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Takotsubo Cardiomyopathy: A Case Series and Review of the Literature. West J Emerg Med. 2008;9:104-11.
- [Google Scholar]
- Pheochromocytoma: A Clinicopathologic Case Series. Indones J Cancer. 2020;14:27.
- [CrossRef] [Google Scholar]
- Acute and Chronic Pheochromocytoma-Induced Cardiomyopathies: A Systematic Analytical Review. Medicine (Baltimore). 2015;94:e2198.
- [CrossRef] [PubMed] [Google Scholar]
- Toxicology Update: The Cardiotoxicity of the Oxidative Stress Metabolites of Catecholamines (Aminochromes) J Appl Toxicol. 2001;21:S15-22.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiovascular Manifestations and Complications of Pheochromocytomas and Paragangliomas. J Clin Med. 2020;9:2435.
- [CrossRef] [PubMed] [Google Scholar]
- Adrenal Pheochromocytoma Presenting with Takotsubo-Pattern Cardiomyopathy and Acute Heart Failure: A Case Report and Literature Review. Medicine (Baltimore). 2016;95:e4846.
- [CrossRef] [PubMed] [Google Scholar]
- Pheochromocytoma: Presenting with Regular Cyclic Blood Pressure and Inverted Takotsubo Cardiomyopathy. J Clin Hypertens. 2009;11:81-6.
- [CrossRef] [PubMed] [Google Scholar]







