Translate this page into:
Mitral Annulus Pre-Systolic Excursion (MAPSE) Versus Modified Simpson’s Method for Ejection Fraction Estimation in Patients with Acute Coronary Syndrome
*Corresponding author: Rajendra Betham, Department of Cardiology, Guntur Medical College, Guntur, Andhra Pradesh, India. dr.b.rajendra@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Baig AA, Betham R, Nathani S. Mitral Annulus Pre-Systolic Excursion (MAPSE) Versus Modified Simpson’s Method for Ejection Fraction Estimation in Patients with Acute Coronary Syndrome. Indian J Cardiovasc Dis Women. 2024;9:74-80. doi: 10.25259/IJCDW_53_2023
Abstract
Objectives:
Evaluating left ventricle (LV) systolic function is pivotal in cardiac assessment, primarily relying on the left ventricular ejection fraction (LVEF) calculated through the modified Simpson’s method. However, challenges arise in accurately determining LVEF, especially in patients with acute coronary syndrome, where difficulty in visualizing the blood tissue interface can lead to inaccuracies. Mitral annular plane systolic excursion (MAPSE), which evaluates longitudinal function of LV has shown promise in detecting subtle myocardial abnormalities, particularly in patients with preserved ejection fraction (EF).
Materials and Methods:
The study included three groups of patients based on EF measurement using modified Simpson’s method: Group A with EF <50%, Group B with EF >50%, and Group C as healthy controls. In each group, MAPSE and EF derived from MAPSE formula were calculated: 4.8 × MAPSE (mm) + 5.8 in males, 4.2 × MAPSE (mm) + 2.0 in females. Statistical analyses were conducted to assess the agreement and potential differences between the two methods within each group.
Results:
The mean age of study population was 55.63 ± 9.21 years in Group A, 54.79 ± 9.82 years in Group B, and 55.10 ± 8.79 years in Group C. In Group A, mean EF measured through modified Simpson’s formula was 37.79 ± 5.38, whereas mean EF measured through MAPSE was 37.95 ± 5.32. There was no statistical difference among EF calculation through Simpson’s method or MAPSE method. (P = 0.8293). In Group B, Mean EF calculated through Simpson method was 56.24 ± 3.12 whereas with MAPSE method was 52.31 ± 4.26. There was found to be a statistical difference in EF calculation by both of this method in patients with EF>50% (P < 0.0001). In Group C, mean EF calculated through Simpson’s method was 64.23 ± 5.21 and through MAPSE was 64.99 ± 4.85, respectively. There was no statistical difference between this two methods in terms of EF calculation (P = 0.2812).
Conclusion:
EF assessment using the traditional modified Simpson’s method and MAPSE demonstrated a strong correlation in patients with EF <50% and controls. However, in patients with EF >50%, MAPSE revealed subendocardial dysfunction undetected by the Simpson method, highlighting MAPSE’s value in identifying subtle myocardial abnormalities.
Keywords
Mitral annular plane systolic excursion
Modified Simpson’s
Ejection fraction
Left ventricle
Acute coronary syndrome
ABSTRACT IMAGE

INTRODUCTION
The evaluation of the left ventricle’s (LVs) systolic function primarily relies on a metric known as left ventricular ejection fraction (LVEF). LVEF quantifies the portion of blood expelled by the LV during each heartbeat, providing a valuable assessment of myocardial function.[1]
A commonly employed method for LVEF assessment is two-dimensional echocardiography (2D-ECHO). This technique allows for the visualization of the LV from multiple angles, offering insights into its structure and operation. In 2D-ECHO, LVEF is typically determined using the modified Simpson’s method, which involves tracing the endocardial borders in different views to calculate enddiastolic volume (EDV) and end systolic volume (ESV). Assessing LVEF through 2D-ECHO is crucial for diagnosing and prognosticating various cardiac conditions. Changes in LVEF can indicate the presence and severity of myocardial dysfunction, guide treatment strategies, and offer insights into a patient’s likely outcomes.[1,2]
Accurately determining the LVEF using echocardiography involves several factors, such as correct positioning of imaging planes and clear definition of the endocardium. However, practical challenges often arise in meeting these requirements. Due to difficulty in visualizing blood tissue interface, it is difficult to measure EF using Simpson’s method in approximately 50% of patients. Similarly, about one-third of elderly individuals encounter technical obstacles that lead to inaccurate EF calculations.[3,4]
Mitral annular plane systolic excursion (MAPSE), also known as left atrioventricular plane displacement, mitral ring displacement, and mitral annulus excursion, serves as an echocardiographic marker derived from M-mode imaging. It assesses the longitudinal function of the LV.[5,6] While there is a connection between MAPSE and EF, they are not entirely interchangeable. MAPSE primarily reflects the performance of longitudinally oriented myocardial fibers in the subendocardial region, whereas modified Simpson’s gauges the function of circumferential fibers in the subepicardial layer concerning LVEF. MAPSE excels at detecting subtle abnormalities in LV function. This is especially relevant in cases where patients experience age-related changes, myocardial hypertrophy, or diastolic dysfunction with preserved EF. In such instances, the long-axis function of the heart is compromised, while radial function may remain unaffected or even improve.[5,7] Consequently, measuring MAPSE becomes a more practical and convenient method for estimating EF. The typical average MAPSE value falls within the 12–15 mm range. A value equal to or >10 mm indicates preserved EF (≥55%), whereas a MAPSE value below 8 mm is associated with reduced LVEF (<50%). Furthermore, a MAPSE measurement below 7 mm signifies an EF below 30%.[2]
The purpose of our study was to evaluate and validate the LVEF derived from MAPSE measurements and compare them with the LVEF obtained from the modified Simpson’s method in 2D-echocardiography.
MATERIALS AND METHODS
Study design
This was an observational, prospective, and case–control study.
Sample size
There are 450 individuals in total, 300 of whom are subjects and 150 of whom are controls. One hundred and fifty patients with EF >50% and 150 patients with EF <50% will make up the subject group. The control group will be made up of 150 relatives in good health free of any heart conditions.
Study area
This study was conducted at the Department of Cardiology.
Study population
Case
Patients with acute coronary syndrome who were admitted in the cardiology department or visited an out-patient clinic.
Controls
Healthy relatives of patients without cardiac diseases.
Sample size
This study was 450 (300 subjects and 150 controls). (Subjects: 150 patients with EF>50%, 150 patients with EF <50% Controls: 150 healthy relatives without cardiac diseases).
Patient eligibility
Inclusion criteria
The following criteria were included in the study: 1. Patients aged 18 years and above 2. Acute coronary syndrome 3. For the control group, inclusion criteria include healthy relatives of patients without any history or current evidence of cardiac diseases.
Exclusion criteria
The following criteria were excluded from the study:
Patients with a history of significant valvular heart disease or congenital heart disease
Patients with significant arrhythmias, or hemodynamic instability
Patients with pacemakers or implanted cardiac defibrillators in situ
Cardiomyopathy patient
Patients with the right ventricular failure
Patients with large pericardial effusion.
Data collection methods
Patients are identified based on clinical histories, ensuring eligibility. Informed consent, approved by the Institutional Review Board, is obtained. Thorough medical history and clinical examinations are conducted. Echocardiography, using the PHILIPS AFFINITY 70 device, is performed in the left lateral decubitus position. Echocardiographic measurements, following American Society of Echocardiography guidelines, including MAPSE [Figure 1] and LVEF, are recorded.

- 2D echocardiography depicting A4CV with M-mode beam crossing across lateral mitral annuli. MAPSE was found to be 1.02 cm in this case. (M: Motion), (MAPSE: Mitral annular plane systolic excursion.)
Statistical analysis
Data Recording: Both continuous and discrete variables were recorded in Microsoft Excel.
Using measurements such as the mean and standard deviation, median and interquartile range, and range and continuous variables were summarized. Frequency and percentage summaries of discrete variables were used.
Shapiro-Wilk test was utilized to determine whether the continuous variables had a normal distribution. This test assists in determining when employing parametric statistical tests are suitable.
Comparison of continuous variables: Depending on the findings of the normality tests, either an unpaired t-test or Mann –Whitney U-test was used to compare continuous variables between two groups. When the data have a normal distribution, the unpaired t-test is performed; when the data have a non-normal distribution, the Mann–Whitney U-test is employed.
The association between the EFs assessed using the Simpson’s method and the EF measured using the MAPSE method was examined using Pearson’s correlation coefficient. The degree and direction of the linear relationship between these variables are determined by this study.
Statistical software: “R Studio version 1.4.1103,” a well-known integrated development environment for the R programming language, was used to carry out the statistical analysis.
A two-tailed P < 0.05 was regarded as statistically significant, suggesting that the observed results were not likely to have been the result of chance alone.
RESULTS
Our study included 450 patients with age ranging from 20 to 75 years. Out of 450, 300 were patients and 150 were controls. Baseline characteristics are depicted in Table 1.
| Parameter | Group A: EF<50% (150 patients) | Group B: EF>50% (150 patients) | Group C: Controls (150 healthy controls) |
|---|---|---|---|
| Age (years) | 55.63±9.21 | 54.79±9.82 | 55.10±8.79 |
| Sex (females) | 65 | 70 | 67 |
| Hypertension | 57 | 51 | 54 |
| Diabetic | 61 | 52 | 54 |
| Presentation | |||
| AWMI | 65 | 18 | Not applicable |
| IWMI | 39 | 48 | |
| LWMI | 14 | 05 | |
| NSTEMI | 32 | 46 | |
| Unstableangina | 0 | 33 | |
| PTCA | 108 | 106 | Not applicable |
| CABG | 22 | 20 | Not applicable |
| Medical management | 20 | 24 | Not applicable |
EF: Ejection fraction, AWMI: Anterior wall myocardial infarction, IWMI: Inferior wall myocardial infarction, LWMI: Lateral wall myocardial infarction, NSTEMI: Non ST elevation myocardial infarction, PTCA: Percutaneous transluminal coronary angioplasty, CABG: Coronary artery bypass grafting
Group A (cases with EF<50%)
In cases with EF <50% group, mean left ventricular end-diastolic volume (LVEDV) and left ventricular end systolic volume (LVESV) were 171.17 mL and 107.38 mL, respectively. The mean MAPSE was 7.43 [Table 2].
Mean EF measured through modified Simpson’s formula was 37.79 ± 5.38, whereas mean EF measured through MAPSE was 37.95 ± 5.32 [Figure 2]. There was no statistical difference among EF calculation through Simpson’s method or MAPSE method (P = 0.8293)
There was no statistical difference when males and females were assessed separately as well Tables 3 and 4.
| Parameter | Group A: EF<50% (150 patients) | Group B: EF>50% (150 patients) | Group C: Controls (150 healthy controls) |
|---|---|---|---|
| LVEDV (mL) | 171.17 | 174.63 | 152.98 |
| LVESV (mL) | 107.38 | 76.39 | 54.59 |
| MAPSE (mean) | 7.43 | 10.628 | 13.38 |
| EF (Simpson) % | 37.79±5.38 | 56.24±3.12 | 64.23±5.21 |
| EF (MAPSE) % | 37.95±5.32 | 52.31±4.26 | 64.99±4.85 |
MAPSE: Mitral annular plane systolic excursion, EF: Ejection fraction, LVEDV: Left ventricular end-diastolic volume, LVESV: Left ventricular end-systolic volume
| Parameter | Group A: EF<50% (150 patients) | Group B: EF>50% (150 patients) | Group C: Controls (150 healthy controls) |
|---|---|---|---|
| LVEDV (mL) | 189 | 185 | 168 |
| LVESV (mL) | 117 | 82 | 61 |
| MAPSE (mean) | 6.35 | 9.47 | 12.2 |
| EF (Simpson) % | 38.1±4.76 | 55.23 | 63.9±4.96 |
| EF (MAPSE) | 36.3±4.32 | 51.3±5.82 | 64.6±5.87 |
MAPSE: Mitral annular plane systolic excursion, LVEDV: Left ventricular end-diastolic volume, LVESV: Left ventricular end-systolic volume, EF: Ejection fraction
| Parameter | Group A: EF<50% (150 patients) | Group B: EF>50% (150 patients) | Group C: Controls (150 healthy controls) |
|---|---|---|---|
| LVEDV (mL) | 153 | 164 | 138 |
| LVESV (mL) | 97 | 70 | 48.8 |
| MAPSE (mean) | 8.95 | 12.2 | 15.1 |
| EF (Simpson) % | 36.6±5.32 | 57.25 | 64.56±5.23 |
| EF (MAPSE) | 39.6±5.46 | 53.32±4.32 | 65.4±5.41 |
MAPSE: Mitral annular plane systolic excursion, LVEDV: Left ventricular end-diastolic volume, LVESV: Left ventricular end-systolic volume, EF: Ejection fraction

- Correlation between ejection fraction (EF) calculation by Simpson method versus mitral annulus pre-systolic excursion method in patients with EF<50%. (MAPSE: Mitral annular plane systolic excursion.)
Group B (cases with EF>50%)
There were 150 patients included with EF>50%. Mean LVEDV and LVESV were 174.63 mL and 76.39 mL, respectively. The mean MAPSE was 10.628, respectively [Table 2].
Mean EF calculated through Simpson method was 56.24 ± 3.12 whereas with MAPSE method was 52.31 ± 4.26 [Figure 3]. There was found to be a statistical difference in EF calculation by both of these methods in patients with EF>50%. (P < 0.0001)
There was statistical difference when males and females were assessed separately as well Tables 3 and 4.
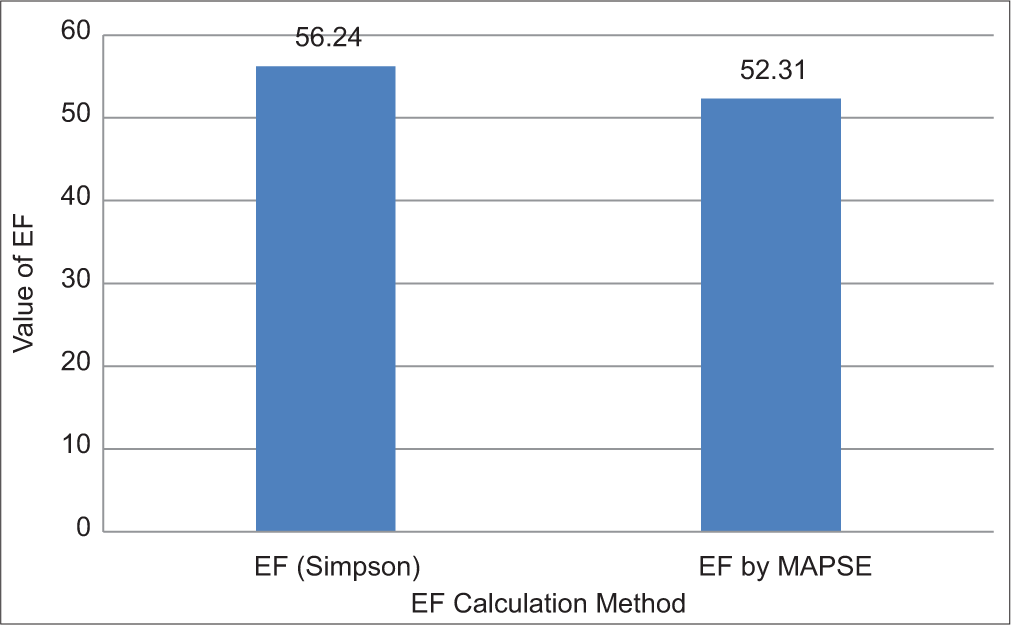
- Correlation between ejection fraction (EF) calculation by Simpson versus mitral annulus pre-systolic excursion (MAPSE) method in patients with EF>50%.
Group C: Controls
There were 150 healthy controls. Mean LVEDV and LVESV were 152.98 mL and 54.59 mL, respectively. The mean MAPSE was 13.38 [Table 2].
Mean EF calculate through Simpson’s method was 64.23 ± 5.21 and through MAPSE was 64.99 ± 4.85, respectively [Figure 4]. There was no statistical difference between these two methods in terms of EF calculation (P = 0.2812).
There was no statistical difference when males and females were assessed separately as well Tables 3 and 4.

- Correlation between ejection fraction (EF) calculation by Simpson’s versus MAPSE method in healthy controls. (MAPSE: Mitral Annulus Pre-Systolic Excursion).
DISCUSSION
This was an observational, prospective, and case–control study conducted in the Department of Cardiology, Government General Hospital, Guntur, Andhra Pradesh from December 2021 to June 2023. There were 450 participants in our study, of whom 300 were cases and 150 were controls. The mean age of the study population was 55.63 ± 9.21 years in Group A, 54.79 ± 9.82 years in Group B and 55.10 ± 8.79 years in Group C. Sixty-five out of 150 in Group A, 70 out of 150 in Group B, and 67 out of 150 in Group C were female. All patients of acute coronary syndromes were included in the study.
Group with EF <50%: Our study found no statistically significant differences between the EF calculations using the conventional method (Modified Simpson’s) and the calculations using MAPSE in the group of instances with EF <50%. This shows that in evaluating EF in this subset of patients, both the approaches were consistent.
This findings were find to be consistent with the study by Adel et al., which included 170 patients with EF<50% and found that EF measured through modified Simpson’s and through MAPSE were consistent with no statistical difference.[4]
Group with EF >50%: The modified Simpson’s technique and MAPSE produced significantly different EF calculations in the group of situations where the EF was larger than 50%.
Control group: There was a correlation between EF evaluated using the conventional approach (Modified Simpson’s) and EF measured using MAPSE in the control group, which included people without acute coronary syndrome. The two techniques in this group did not significantly differ statistically in estimating EF.
Our findings align with those of Matos et al., who suggested that a MAPSE cutoff value of <6 is a suitable threshold for predicting a significantly reduced EF of 30 or lower. The study’s authors, however, acknowledged two significant limitations. First, they relied on comparing MAPSE-derived values to visually estimated EF, rather than using the globally accepted Simpson’s method. Second, they did not investigate specific disease conditions to assess the accuracy of the MAPSE-derived ejection formula.[2] Our study overcame both of these limitations, that is, our study compared MAPSE derived EF with modified Simpson’s derived EF, and also, our study was focused only on acute coronary syndrome patients. Adel et al.[4] established the reliability of the MAPSE-derived ejection formula in cases of dilated cardiomyopathy. However, it is worth noting that their study exclusively included adult male patients. One notable constraint of their research was the inadequate representation of female patients with reduced left ventricular function and a normal mitral valve during the study period. This limitation prevented them from confirming any gender-specific variations in MAPSE measurements. Our study overcame this limitation as we included females equally in all the three groups, approximately 40–45% of the study population.
When males and females were assessed separately, it was seen that MAPSE levels were higher in females when compared to males. This correlates with the study done by Matos et al.,[2] and hence, the formula for calculating EF was different in both males and females.
In the present study, we tried to overcome these limitations and at the same time validated the equation derived by Matos et al.[2] for EF estimation through MAPSE in adult males and females. Furthermore, our study included patients with acute coronary syndrome, whereas Adel et al.[4] included patients with dilated cardiomyopathy. Furthermore, our study was one of the first studies which tried to compare EF estimation in patients with EF >50% and found statistically significant differences in EF values when measured with MAPSE or modified Simpson’s method.
According to the results of our investigation, longitudinal fiber dysfunction may exist even in patients with a normal EF as determined by conventional methods. This was demonstrated with MAPSE derived EF which was found to be low when compared to EF measured using modified Simpson’s method.
Overall, our study advances knowledge of the relationships between EF measurements acquired using various methods and emphasizes the significance of taking MAPSE into account when evaluating cardiac systolic function, especially in patients with coronary artery disease.
Limitations
Our study was limited to the adult population, and the applicability of our findings to the pediatric population remains uncertain.
Our study did not investigate the impact of diastolic dysfunction on MAPSE-derived measurements
Our study only included patients with acute coronary syndrome. Therefore, caution should be exercised when extrapolating these findings to other groups of patients with valvular heart disease or congenital heart disease
Our study did not compare MAPSE-derived EF with more advanced imaging modalities such as strain echocardiography and Cardiac magnetic resonance imaging (MRI) or 3D Trans Thoracic Echocardiography.
These techniques are considered to be the gold standard for quantifying left ventricular function.
CONCLUSION
EF estimates made using the traditional approach (modified Simpson’s) and EF measurements made using MAPSE both displayed a statistically significant correlation in the patients with EF <50% and control group. This shows that in assessing EF in this population, both the methods are consistent and MAPSE derived EF is a validated tool.
In patients with EF >50%, it was noteworthy that MAPSE derived EF did not show an association with the modified Simpson’s method. This discrepancy is explained by the fact that longitudinal function is predominantly represented by MAPSE, which is connected to the subendocardium where longitudinal fibers are found. During a myocardial injury, this area is more vulnerable to hypoperfusion and ischemia, resulting in normal LVEF values with modified Simpson’s but inadequate MAPSE values, which point to subendocardial dysfunction.
These findings demonstrate the complementary nature of MAPSE in assessing myocardial function, particularly in detecting subtle abnormalities that might not be picked up by modified Simpson’s EF measurements alone.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest. Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Audio summary available at
Financial support and sponsorship
Nil.
References
- Echocardiographic Assessment of Systolic Function of Left Ventricle: An Overview of Contemporary Techniques, Including Speckle-Tracking Echocardiography. Mayo Clin Proc. 2019;94:125-38.
- [CrossRef] [PubMed] [Google Scholar]
- Mitral Annular Plane Systolic Excursion as a Surrogate for Left Ventricular Ejection Fraction. J Am Soc Echocardiogr. 2012;25:969-74.
- [CrossRef] [PubMed] [Google Scholar]
- Correlation of Mitral Annular Plane Systolic Excursion [Mapse] with Left Ventricular Ejection Fraction in Tertiary Care Centre. Int J Sci Res. 2023;12:201-4.
- [Google Scholar]
- Mitral Annular Plane Systolic Excursion-Derived Ejection Fraction: A Simple and Valid Tool in Adult Males With Left Ventricular Systolic Dysfunction. Echocardiography. 2015;33:179-84.
- [CrossRef] [PubMed] [Google Scholar]
- Correlation of Mitral Annular Plane Systolic Excursion (MAPSE) and Tissue Doppler Peak Systolic Velocity with Systolic Function of Left Ventricle. J Cardiol Curr Res. 2017;10:349.
- [CrossRef] [Google Scholar]
- Mitral Annular Plane Systolic Excursion (MAPSE) as a Simple Index for Assessing Left Ventricular Function: An Observational Study. J Pharm Res Int. 2021;33:163-70.
- [CrossRef] [Google Scholar]
- Evaluating the Association Between the Three Different Ejection Fraction Measurement Techniques and Left Ventricle Global Strain. Eurasian J Med. 2018;50:173-7.
- [CrossRef] [PubMed] [Google Scholar]







