Translate this page into:
Mind–Body Connections: Gender differences in Pain Perception, Anxiety Sensitivity, and their Impact on Cardiac Health
*Corresponding author: Gursabeen Kaur, Department of Clinical Psychology, Dayanand Medical College and Hospital, Ludhiana, Punjab, India. gursabeen0381@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Aulakh D, Kaur G, Upadhyay P, Mishra B. Mind–Body Connections: Gender differences in Pain Perception, Anxiety Sensitivity, and their Impact on Cardiac Health. Indian J Cardiovasc Dis Women. doi: 10.25259/IJCDW_97_2024
Abstract
Objectives:
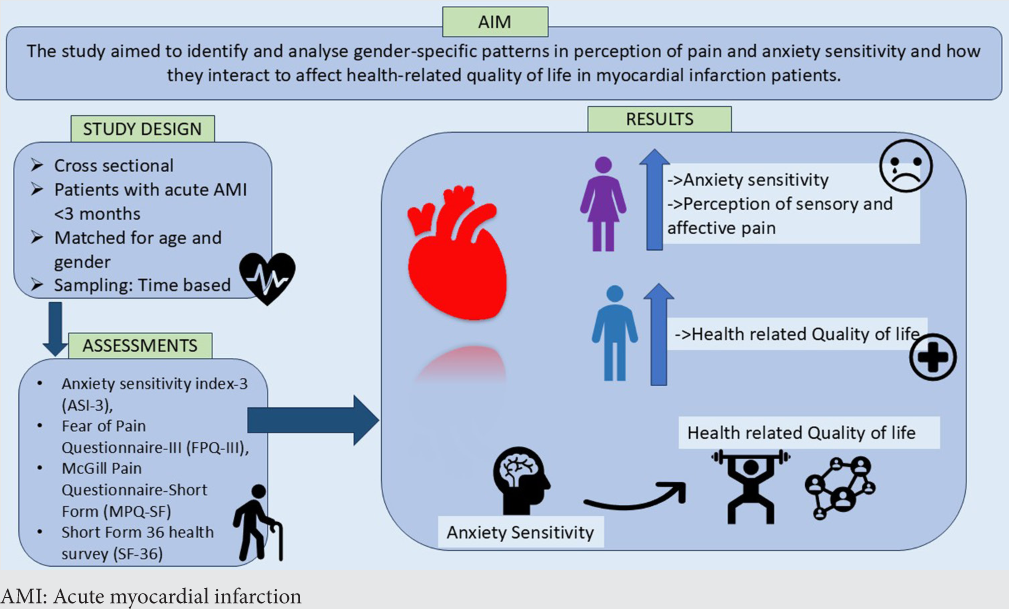
The study aimed to identify and analyze gender-specific patterns in the perception of pain and anxiety sensitivity and how they interact to affect health-related quality of life (HRQoL) in myocardial infarction (MI) patients.
Materials and Methods:
68 acute MI patients presented within 3 months of the cardiac event during the time span from May to September 2024 were included. They were assessed using Anxiety Sensitivity Index-3, Fear of Pain Questionnaire-III, McGill Pain Questionnaire-Short Form, and Short Form-36 Health Survey. Independent samples t-test was used to analyze the gender differences and Cohen’s d as a measure of effect size. Pearson correlation coefficient and linear regression analysis were done to assess the relationship between variables and to ascertain the predicted variance toward HRQoL.
Results:
Anxiety sensitivity and fear of pain were higher in females. Women reported increased perception of sensory and affective pain. HRQoL was found to be higher in males. Anxiety sensitivity played a statistically significant role in the prediction of the HRQoL.
Conclusion:
This study highlights the presence of significant differences in the anxiety sensitivity, pain perception, and fear of pain among male and female acute MI patients. Our findings suggest a significant role of anxiety sensitivity in mediating the quality of life in MI patients post the cardiac event. This may be a result of a unique combination of several biological, psychological, or sociocultural factors which tend to differ by gender and therefore require an individualized approach to assessment and comprehensive management.
Keywords
Acute myocardial infarction
Anxiety sensitivity
Fear of pain
Gender differences
Health-related quality of life
Pain
ABSTRACT IMAGE
INTRODUCTION
Myocardial infarction (MI), a prevalent manifestation of coronary heart disease, remains one of the leading causes of mortality globally.[1] The incidence of MI is projected to rise significantly in developing countries, with an estimated increase of 120% among women and 137% among men.[2] Notably, males exhibit a higher prevalence, accounting for approximately 70% of MI cases.[3] Advances in medical science and technology have significantly improved survival rates among MI patients;[4] however, many survivors experience persistent symptoms, including chronic pain, even years after the event. Pain is the most frequently reported complaint and is often accompanied by sleeplessness and confusion, contributing to increased morbidity and mortality.[5]
Pain perception during and after MI is influenced by nociceptors in ischemic cardiac tissue as well as psychological factors.[6] Anxiety sensitivity, defined as the fear of negative consequences associated with anxiety-related sensations, has been identified as a key psychological factor amplifying pain experiences.[7,8] According to Frazier,[9] approximately 30% of MI patients report no anxiety, while 23%, 25%, and 22% report mild, moderate, and high levels of anxiety, respectively. Anxiety sensitivity not only exacerbates pain perception but also contributes to increased cardiovascular risk through mechanisms such as arterial stiffness and hypertension. Furthermore, MI survivors often experience a reduced health-related quality of life (HRQoL), marked by diminished vocational outcomes, impaired social functioning, and overall reduced well-being.[10,11]
The present study seeks to explore gender differences in pain perception and fear of pain among MI patients, examining their relationship with anxiety sensitivity and its broader impact on HRQoL. Understanding these interrelations may provide valuable insights for improving post-MI care and enhancing long-term outcomes for survivors.
MATERIALS AND METHODS
Study design
This cross-sectional study was conducted on patients diagnosed with acute myocardial infarction (AMI) who visited the outpatient department or were admitted to the inpatient department of a tertiary care hospital in North India. The study was carried out over a 5-month period, from May to September 2024. A purposive sampling method was employed. Since this was a time-bound study, no formal sample size estimation was performed; all eligible participants meeting the inclusion criteria during the study period were recruited. Inclusion criteria included:
Diagnosis of AMI within 3 months of the cardiac event.
Age ≥18 years.
Minimum educational qualification of primary level.
Any gender.
Exclusion criteria included the presence of major psychiatric comorbidities (Major Depressive Disorder, Anxiety, etc.,) or significant physical illnesses, except for hypertension and diabetes. All participants provided informed consent, and confidentiality of identifiable information was strictly maintained throughout the study.
Sociodemographic information was collected using the Kuppuswamy scale. Data collection involved a brief 15– 20 min interview conducted by the interviewer, during which the following standardized tools were administered:
Anxiety Sensitivity Index-3: An 18-item self-report measure assessing fear of potential negative consequences associated with physical, cognitive, and social anxiety-related symptoms. Higher scores indicate greater anxiety sensitivity.[12]
Fear of Pain Questionnaire-III (FPQ-III): A 30-item self-report instrument evaluating fear of pain across three subscales – severe pain, minor pain, and medical pain. The FPQ-III has demonstrated satisfactory reliability and validity.[13]
McGill Pain Questionnaire-Short Form: A multidimensional tool assessing pain perception across sensory-discriminative, motivational-affective, and cognitive-evaluative dimensions. It includes a pain rating index, Visual Analog Scale, and present pain intensity.[14]
Short Form 36 Health Survey: A 36-item questionnaire measuring HRQoL across eight domains: physical functioning, role limitations due to physical problems, bodily pain, general health perceptions, vitality, social functioning, role limitations due to emotional problems, and mental health. Scores range from 0 to 100, with higher scores indicating better health.[15]
Statistics
Descriptive statistics were computed to summarize the characteristics of the study population. To assess gender differences in the variables of interest, independent t-tests were performed. The magnitude of these differences was quantified using Cohen’s d as a measure of effect size. Pearson correlation coefficients were calculated to evaluate the linear relationships between variables. Simple linear regression analyses were conducted to determine the extent to which the independent variables could predict the dependent variable. The normality of the variables was evaluated both graphically and statistically using the Shapiro–Wilk W-test. A significance level of P ≤ 0.05 was adopted to determine statistical significance.
RESULTS
Descriptive statistics are presented in Table 1. The study included a total of 68 participants, who were matched for age, gender, and educational qualification. In terms of diagnosis, the majority of participants (64.06%) had anterior wall MI, followed by inferior wall MI at 30.88% and non-ST-elevation MI at 8.82%.
| Characteristics | Males | Females |
|---|---|---|
| Age | 58 | 58 |
| Socio-economic status (%) | ||
| Upper | 5.8 | 2.9 |
| Upper Middle | 44.11 | 47.05 |
| Lower Middle | 50 | 50 |
| Upper Lower | – | – |
| Lower | – | – |
| Diagnosis (%) | ||
| AWMI | 58.8 | 61.7 |
| IWMI | 29.4 | 32.3 |
| NSTEMI | 11.76 | 5.8 |
| Time since event (%) | ||
| 3 months | 29.41 | 32.35 |
| 2 months | 23.52 | 20.58 |
| 1 month | 11.76 | 20.58 |
| >1 month | 35.29 | 26.47 |
AWMI: Anterior wall myocardial infarction, IWMI: Inferior wall myocardial infarction, NSTEMI: Non-ST-elevation myocardial infarction
Figure 1 represents descriptive age-based analysis which revealed that there is a progressive increase in anxiety sensitivity among females for social and cognitive anxiety, whereas physical anxiety was similar among all age groups. On the fear of pain scale, it was found that both older females and males, that is, 60–65 years had low fear of pain. On the pain perception scale, males among all ages scored almost similar, while women in the 60–65-year age group scored lower indicating lesser perception of pain. On HRQoL, males in the 60–65-year age group scored lower indicating poorer quality of life.
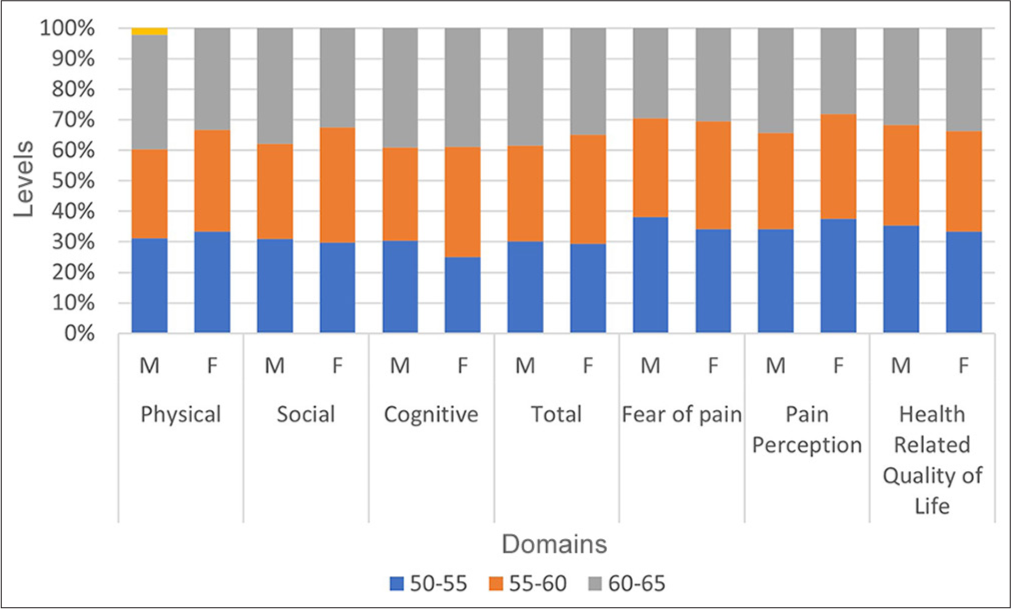
- Age-based comparative analysis of gender differences among anxiety sensitivity, fear of pain, pain perception, and health-related quality of life.
Table 2 presents a comparative analysis of gender differences in anxiety sensitivity, fear of pain, pain perception, and HRQoL. Females reported significantly higher fear of pain across all subscales (severe, minor, and medical) and the total score (P < 0.05). Cohen’s d values indicated medium to large effect sizes, with the cognitive dimension exhibiting the largest effect (d = 1.038). Similarly, females reported significantly greater fear of pain across all subscales (severe, minor, and medical) and the total score (P < 0.05). Cohen’s d values ranged from medium to large, with minor pain exhibiting the largest effect (d = 1.065). For pain perception, females reported significantly higher pain perception in the sensory and affective dimensions. Cohen’s d values indicated small to medium effect sizes d = 0.605. The total pain perception score did not show a significant gender difference (P = 0.561). On the HRQoL, males reported significantly higher scores in physical functioning (t = 7.01, P = 0.001) and role physical (t = 2.67, P = 0.009).
| Anxiety sensitivity | Mean | Standard deviation | t | P | Cohen’s d | ||
|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | ||||
| Physical | 15.382 | 17.735 | 5.009 | 2.620 | −2.426 | 0.017* | 0.500 |
| Social | 9.352 | 12.676 | 5.307 | 3.690 | −2.997 | 0.003** | 0.662 |
| Cognitive | 7.529 | 12.5 | 5.082 | 4.527 | −4.257 | 0.001** | 1.038 |
| Total | 31.970 | 42.911 | 11.008 | 8.229 | −4.68 | 0.001** | 1.131 |
| Fear of pain | |||||||
| Severe | 18.176 | 22.588 | 4.217 | 6.144 | −3.474 | 0.001** | 0.760 |
| Minor | 5.441 | 8.147 | 1.761 | 3.630 | −4.122 | 0.001** | 1.065 |
| Medical | 22.470 | 26.470 | 7.165 | 5.315 | −2.633 | 0.010* | 0.638 |
| Total | 46.088 | 57.205 | 8.897 | 11.257 | −4.601 | 0.001** | 1.083 |
| Pain perception | |||||||
| Sensory | 6.588 | 5.294 | 2.400 | 2.276 | 2.280 | 0.025* | 0.434 |
| Affective | 4.911 | 5.794 | 1.712 | 1.610 | −2.189 | 0.032* | 0.605 |
| Total | 11.470 | 11.088 | 2.809 | 2.586 | 0.583 | 0.561 | 0.148 |
| Short form health survey-36 | |||||||
| Physical functioning | 18.970 | 10.147 | 3.785 | 3.132 | 7.01 | 0.001** | 1.757 |
| Role physical | 5.088 | 4.352 | 1.083 | 1.177 | 2.679 | 0.009** | 0.910 |
| Body pain | 9.111 | 9.047 | 0.887 | 0.766 | 0.258 | 0.796 | 0.101 |
| General health | 9.4 | 11.3 | 2.218 | 14.620 | −0.756 | 0.452 | 0.226 |
| Vitality | 14.441 | 13.235 | 1.192 | 1.634 | 2.552 | 0.130* | 0.519 |
| Social functioning | 5.176 | 5.794 | 1.099 | 0.913 | −2.396 | 0.193* | 0.597 |
| Role emotional | 4.941 | 4.617 | 0.776 | 0.739 | 1.760 | 0.083 | 0.526 |
| Mental health | 18.147 | 20.735 | 4.611 | 3.736 | −2.734 | 0.008** | 0.512 |
| Total | 85.276 | 78.817 | 7.479 | 15.294 | 2.212 | 0.030* | 0.499 |
Table 3 represents the Pearson correlation analysis between anxiety sensitivity, fear of pain, pain perception, and HRQoL. A significant negative correlation was found between anxiety sensitivity and HRQoL (r = −0.405, P = 0.01) whereas fear of pain and anxiety sensitivity had a positive correlation.
| Domains | Anxiety sensitivity | Fear of pain | Pain perception | Health-related quality of life |
|---|---|---|---|---|
| Anxiety sensitivity | ||||
| Pearson correlation | 1 | 0.277* | 0.010 | −0.405** |
| Sig. (2-tailed) | 0.022 | 0.934 | 0.001 | |
| Fear of pain | ||||
| Pearson correlation | 0.277* | 1 | 0.000 | −0.183 |
| Sig. (2-tailed) | 0.022 | 0.999 | 0.135 | |
| Pain perception | ||||
| Pearson correlation | 0.010 | 0.000 | 1 | −0.089 |
| Sig. (2-tailed) | 0.934 | 0.999 | 0.468 | |
| Health-related quality of life | ||||
| Pearson Correlation | −0.405** | −0.183 | −0.089 | 1 |
| Sig. (2-tailed) | 0.001 | 0.135 | 0.468 | |
Figure 2 represents the linear regression analysis, assessing the degree to which the variables can predict changes in HRQoL. Analysis revealed a significant regression for anxiety sensitivity on HRQoL (F[3], [64] = 4.577, P ≤ 0.01). The R2 was 0.177, indicating that anxiety sensitivity explained approximately 17.7% of the variance of HRQoL.
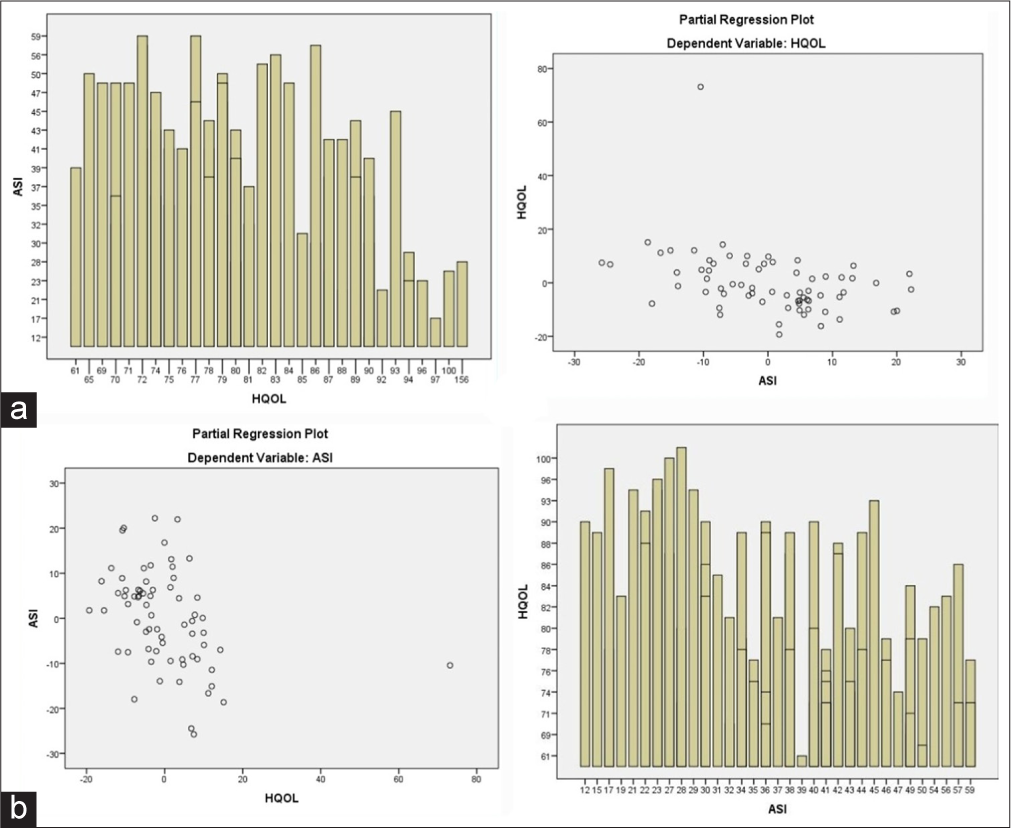
- Linear regression analysis of (a) Anxiety sensitivity with dependent variable as health related quality of life (b) Health related quality of life with dependent variable as Anxiety Sensitivity. (ASI: Anxiety sensitivity index, HQoL: Health Quality of Life.)
Figure 3 represents the time-based analysis and gender differences between anxiety sensitivity, fear of pain, pain perception, and HRQoL. Among all parameters, women had higher mean scores than men, as well as a stable trajectory of mean scores over time.
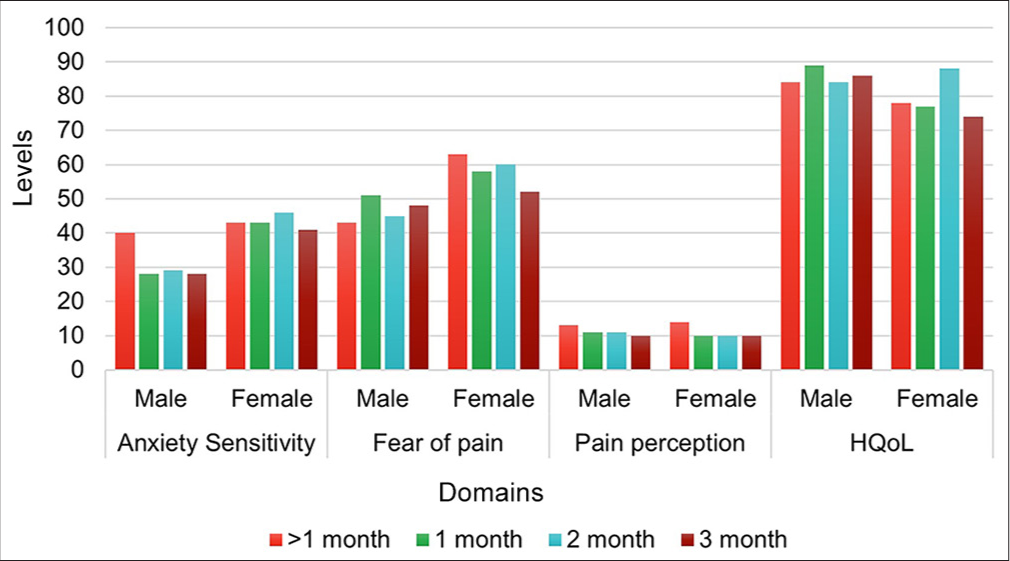
- Temporal analysis of gender differences among anxiety sensitivity, fear of pain, pain perception, and health-related quality of life. (HQoL: Health Quality of Life.)
DISCUSSION
For anxiety sensitivity anxiety sensitivity, results revealed a high prevalence of anxiety sensitivity among females across all three domains of anxiety sensitivity. This aligns with previous research indicating that women often experience a broader spectrum of cardiac symptoms, such as palpitations, light-headedness, and chest pain, which are frequently linked to anxiety. These symptoms may lead to catastrophic misinterpretations of bodily sensations, perpetuating a cycle of heightened anxiety and concern.[16-19] Watt et al.[20] proposed that this gender disparity may stem from societal reinforcement, where women are more likely to receive positive attention for expressing health concerns, while men are socially conditioned to suppress such complaints. Over time, this reinforcement amplifies self-attention and exacerbates anxiety.[21]
Age-wise, the study observed a progressive increase in anxiety sensitivity among both genders, peaking in the 60–65 age group. Older women particularly exhibited a ruminative coping style during stress, characterized by excessive pre-occupation with physiological changes. Educational qualifications appeared to inversely correlate with anxiety sensitivity; individuals with higher education levels demonstrated lower anxiety sensitivity. This finding is consistent with prior studies suggesting that education equips individuals with better-coping mechanisms and access to health-related resources, enhancing their ability to manage anxiety.[21]
Gender differences were also evident in fear of pain, with females reporting higher levels than males. This could be attributed to cultural and social factors that encourage women to express emotions more openly, as well as biological differences in pain perception and prior healthcare experiences. In terms of age, both genders in the 60–65 age group reported reduced fear of pain. Frequent exposure to medical procedures in older adults may normalize pain as part of life, reducing its perceived threat.[22]
Interestingly, educational qualification showed an unexpected trend, wherein individuals with higher education reported greater fear of pain. This contradicts earlier research findings but may be explained in context of the ASI’s physical domain scores.[23] Less-educated individuals exhibited higher scores on this domain of ASI, indicating greater attention to physical sensations despite their educational background mediating cognitive aspects of anxiety. This heightened focus on physical sensations likely leads to increased fear of pain through catastrophizing tendencies. Correlation analysis further supported this relationship by demonstrating a significant positive association between anxiety sensitivity and fear of pain.
For current pain perception, women reported higher sensory and affective pain perception, consistent with findings by Granot et al.[24] Gender differences in pain perception may be attributed to distinct cognitive strategies: Men often employ avoidance strategies, which enhance pain tolerance, while women rely on focused attention strategies, potentially amplifying their pain experience.[25] These findings align with broader evidence suggesting that women reportedly have lower pain thresholds and tolerances compared to men, which may be influenced by both biological mechanisms (e.g., hormonal fluctuations) as well as psychosocial factors.
Age-based analysis revealed that older females reported reduced pain perception. This may be explained by decreased activation of the descending pain modulatory system, particularly in brain regions such as the dorsolateral prefrontal cortex. However, Failla et al. noted that older women exhibit greater adaptation and habituation to high-intensity pain compared to men, potentially mitigating their overall pain experience.[26] These findings highlight the complexity of age-related changes in pain processing.
In terms of HRQoL, males demonstrated better outcomes overall, particularly in physical functioning, role physical, vitality, and general health subscales. Conversely, females scored higher on social functioning and mental health subscales. These gender differences may be mediated by somatosensory amplification and perception.[19] Brink et al.[10] similarly observed that women post-MI had better mental health and social functioning compared to men, who excelled in physical functioning and vitality.
The superior mental health outcomes in women could be attributed to their quicker adaptation to altered health statuses and greater reliance on social support systems, especially in rural settings. Women’s tendency to rely on external cues for symptom interpretation contrasts with men’s approach of comparing current health to past experiences.[27,28] This gendered difference in coping mechanisms likely influences HRQoL outcomes.
A temporal analysis of all the variables revealed that females generally exhibit a stable trend, whereas males experience a more fluctuating course. These findings can be understood within the Indian context, where women typically have a more stable social support system. In contrast, men’s support networks often depend on their functional roles in society.[29] This aligns with Erikson’s concept of “generativity” in older age, where men’s sense of purpose and societal usefulness tends to decrease with age. Following cardiac illnesses like MI, this decline is exacerbated, and a complex interplay of psychosocial factors contributes to a more unstable recovery trajectory in men compared to women.
Our findings on regression analysis reinforce the significant role of anxiety sensitivity in predicting HRQoL among MI patients. This aligns with previous research by Guzelhan et al.,[30] which identified anxiety as an independent predictor of future cardiac complications. Anxiety sensitivity, through its positive correlation with fear of pain, may amplify autonomic perception, leading to symptomatic ischemia and anginal pain.[31] Such heightened pre-occupation with somatic sensations can impair social, physical, and psychological functioning, thereby reducing HRQoL. In the Indian context, the correlation between high pain perception and cognitive apprehension is particularly pronounced among older adults. This often results in frequent medical consultations, a behavior reinforced by collectivistic cultural norms and filial piety traditions. Family members play a critical role in validating and amplifying these health concerns, which may perpetuate anxiety and its associated impacts on HRQoL.
The study provides valuable gender-specific insights into the psychological variables influencing MI recovery. By delineating the time since the MI event, it minimizes potential biases in measuring anxiety and pain perception’s effects on HRQoL. In addition, the inclusion of postmenopausal women eliminates confounding factors related to hormonal or physiological changes, allowing for a clearer understanding of psychological differences between genders.[32,33]
Despite its strengths, the study has limitations. The small sample size restricts the generalizability of results. Furthermore, as a cross-sectional study, it cannot capture longitudinal changes in psychological variables or their evolving impact on HRQoL over time. The study also focuses on a limited range of psychological variables; other factors may contribute significantly to HRQoL but remain unexplored here.
CONCLUSION
This study highlights the complex interplay between chronic pain, anxiety sensitivity, and cardiac health, emphasizing the critical role of gender differences in these interactions. Women reported greater sensory and affective pain perception and higher anxiety sensitivity, which significantly influenced their HRQoL. These findings suggest that gender-specific psychological and physiological patterns must be considered when designing interventions for MI patients. Tailored, integrative approaches that combine psychological therapies, stress management, and cardiovascular care must be employed. Culturally sensitive approaches that account for collectivistic beliefs and familial dynamics may be particularly effective in Indian settings.
Acknowledgment:
We would like to express our gratitude to the Women in Cardiology and Related Sciences (WINCARS) for sponsoring this research as a part of their Prajwalika Scholarship Scheme (PSS). We would also like to thank the faculty and nursing staff of the hospital for their help in making this research possible.
Ethical approval:
The research/study was approved by the Institutional Review Board at Dayanand Medical College and Hospital, Ludhiana, Punjab, number DMCH/IEC/2024/334, dated May 30, 2024.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: This study was financially supported by Prajwalika Scholarship Scheme (PSS).
References
- Predictors of Health-Related Quality of Life among Patients with Myocardial Infarction. West J Nurs Res. 2016;38:43-56.
- [CrossRef] [PubMed] [Google Scholar]
- Anxiety and Quality of Life in Patients with Myocardial Infarction. Nurs Media J Nurs. 2011;1:105-15.
- [Google Scholar]
- Myocardial Infarction Signs and Symptoms: Females VS. Males. Cureus. 2023;15:e37522.
- [CrossRef] [Google Scholar]
- Interventions that Improve Health-Related Quality of Life in Patients with Myocardial Infarction. Qual Life Res. 2016;25:2725-37.
- [CrossRef] [PubMed] [Google Scholar]
- Nurses' Perceptions of Pain Assessment and Pain Management for Patients with Myocardial Infarction in a Coronary Care Unit. Middle East J Nurs. 2013;7:9-22.
- [CrossRef] [Google Scholar]
- Extracardiac Contributions to Chest Pain Perception in Patients 6 Months after Acute Myocardial Infarction. Am Heart J. 1999;137:528-34.
- [CrossRef] [PubMed] [Google Scholar]
- The Role of Anxiety-Relevant Transdiagnostic Factors in Comorbid Chronic Pain and Tobacco Cigarette Smoking. Cogn Ther Res. 2019;43:102-13.
- [CrossRef] [Google Scholar]
- Anxiety Sensitivity and Physical Inactivity in a National Sample of Adults with a History of Myocardial Infarction. Int J Behav Med. 2020;27:520-6.
- [CrossRef] [PubMed] [Google Scholar]
- Management of Anxiety after Acute Myocardial Infarction. Heart Lung. 2002;31:411-20.
- [CrossRef] [PubMed] [Google Scholar]
- Health-Related Quality of Life in Women and Men One Year after Acute Myocardial Infarction. Qual Life Res. 2005;14:749-57.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluating the Impact of Depression, Anxiety and Autonomic Function on Health Related Quality of Life, Vocational Functioning and Health Care Utilisation in Acute Coronary Syndrome Patients: The Advent Study Protocol. BMC Cardiovasc Disord. 2013;13:103.
- [CrossRef] [PubMed] [Google Scholar]
- Anxiety Sensitivity Index Consolidated User Manual: ASI, ASI-3, and CASI Worthington, OH: IDS Publishing; 2008.
- [Google Scholar]
- Development of the Fear of Pain Questionnaire--III. J Behav Med. 1998;21:389-410.
- [CrossRef] [PubMed] [Google Scholar]
- The McGill Pain Questionnaire: Major Properties and Scoring Methods. Pain. 1975;1:277-99.
- [CrossRef] [PubMed] [Google Scholar]
- Short Form 36 (SF36) Health Survey Questionnaire: Normative Data for Adults of Working Age. BMJ. 1993;306:1437-40.
- [CrossRef] [PubMed] [Google Scholar]
- Women and Non-Cardiac Chest Pain: Gender Differences in Symptom Presentation. Arch Womens Ment Health. 2008;11:287-93.
- [CrossRef] [PubMed] [Google Scholar]
- Biobehavioral Responses to Stress in Females: Tend-and-Befriend, not Fight-or-Flight. Psychol Rev. 2000;107:411-29.
- [CrossRef] [PubMed] [Google Scholar]
- Brave Men and Timid Women? A Review of the Gender Differences in Fear and Anxiety. Clin Psychol Rev. 2009;29:496-505.
- [CrossRef] [PubMed] [Google Scholar]
- Gender Disparities in Anxiety and Quality of Life in Patients with an Implantable Cardioverter-Defibrillator. Europace. 2011;13:1723-30.
- [CrossRef] [PubMed] [Google Scholar]
- A Retrospective Study of the Learning History Origins of Anxiety Sensitivity. Behav Res Ther. 1998;36:505-25.
- [CrossRef] [PubMed] [Google Scholar]
- Somatic Symptoms and Panic Attacks: A Retrospective Study of Learning Experiences. Behav Res Ther. 1993;31:269-78.
- [CrossRef] [PubMed] [Google Scholar]
- Fear of Pain Across the Adult Life Span. Pain Med. 2021;22:567-76.
- [CrossRef] [PubMed] [Google Scholar]
- Educational Attainment, Family Background and the Emergence of Pain Gradients in Adulthood. Soc Sci Med. 2024;346:116692.
- [CrossRef] [PubMed] [Google Scholar]
- Gender Differences in the Perception of Chest Pain. J Pain Symptom Manag. 2004;27:149-55.
- [CrossRef] [PubMed] [Google Scholar]
- Avoidance Versus Focused Attention and the Perception of Pain: Differential Effects for Men and Women. Pain. 2000;85:225-30.
- [CrossRef] [PubMed] [Google Scholar]
- Gender Differences in Pain Threshold, Unpleasantness, and Descending Pain Modulatory Activation Across the Adult Life Span: A Cross Sectional Study. J Pain. 2024;25:1059-69.
- [CrossRef] [PubMed] [Google Scholar]
- Psychological factors influencing the reporting of physical symptoms In: The Science of Self-Report. United Kingdom: Psychology Press; 1999. p. :311-28.
- [CrossRef] [Google Scholar]
- The Body, Identity, and Self: Adapting to Impairment. Sociol Q. 1995;36:657-80.
- [CrossRef] [Google Scholar]
- The Influence of Providing and Receiving Social Support on Older Adults' Well-Being. Clin Pract Epidemiol Ment Health. 2022;18
- [CrossRef] [PubMed] [Google Scholar]
- Anxiety and Health-Related Quality of Life after Cardiac Surgery. Arch Med Sci Atheroscler Dis. 2020;5:e27-35.
- [CrossRef] [PubMed] [Google Scholar]
- The Relation between Anxiety and Quality of Life in Heart Patients. ARYA Atheroscler J. 2009;5:19-24.
- [Google Scholar]
- Symptoms in the Menopausal Transition: Hormone and Behavioral Correlates. Obstet Gynecol. 2008;111:127-36.
- [CrossRef] [PubMed] [Google Scholar]
- Why is Depression More Common among Women than Among Men? Lancet Psychiatry. 2017;4:146-58.
- [CrossRef] [PubMed] [Google Scholar]








