Translate this page into:
Impact of the Use of Street Play Mode of Education on the Self-care Capacity of Village Women for Lifestyle Modification for Prevention of Hypertension
*Corresponding author: Amarjeet Singh, Department of Community Medicine, School of Public Health, PGIMER, Chandigarh, India. dramarjeet56@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Arun R, Kumar P, Pradhan KB, Singh A. Impact of the Use of Street Play Mode of Education on the Self-care Capacity of Village Women for Lifestyle Modification for Prevention of Hypertension. Ind ian J Cardiovasc Dis Women. 2024;9:136-42. doi: 10.25259/IJCDW_64_2023
Abstract
Objectives:
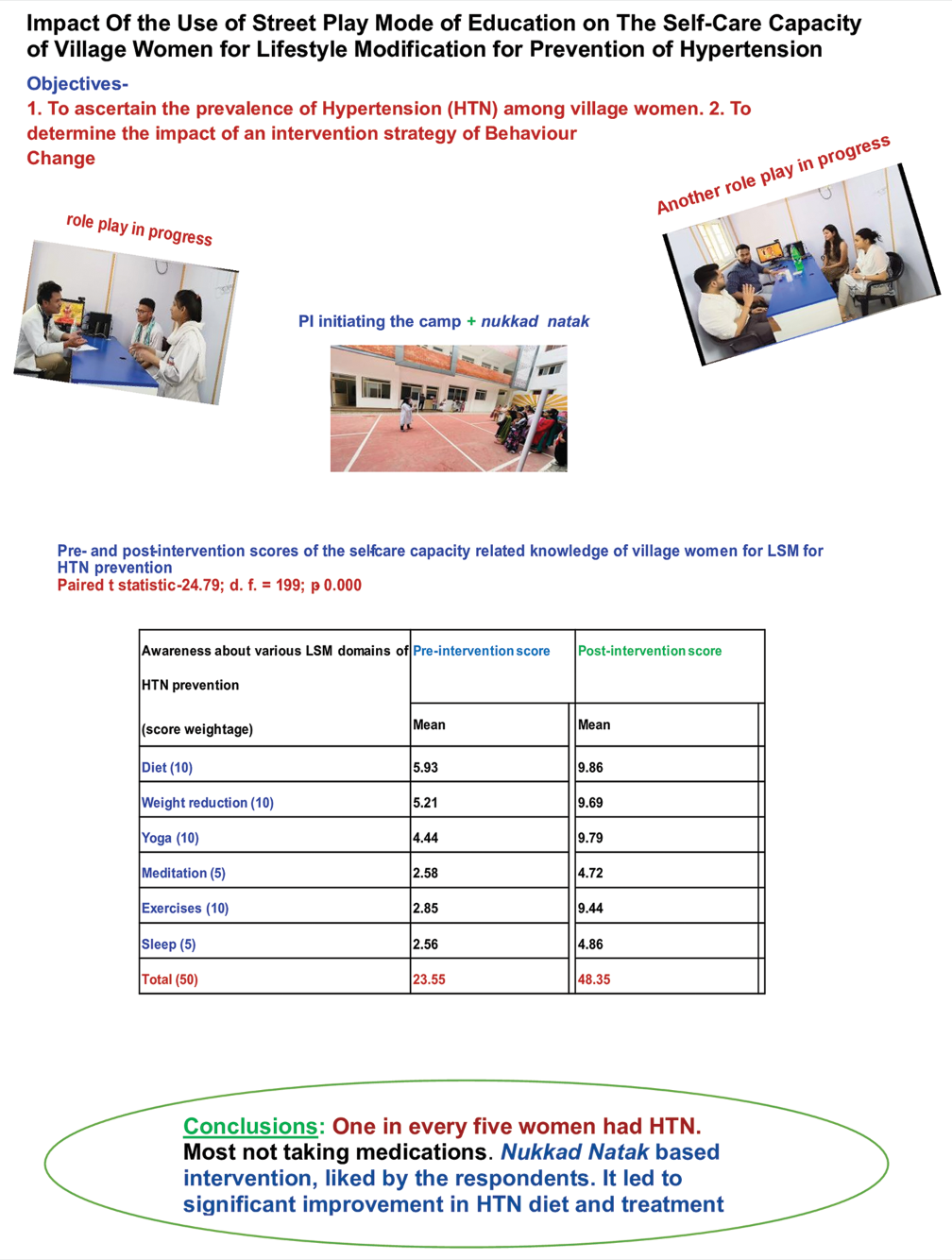
The objectives of this study were as follows: (1) To ascertain the prevalence of hypertension (HTN) among village women. (2) To determine the impact of an intervention strategy of Behavior Change Communication utilizing a camp approach supplemented with nukkad natak on the self-care capacity of village women for lifestyle modification for prevention of HTN.
Materials and Methods:
The study was conducted during June–July 2023 in the field practice area of Community Medicine of a medical college. Sample size was arbitrary (n = 200) out of all willing women attending outpatient departments during the study period. First, a baseline assessment of the study population was done. Street plays were held for the study population on HTN-related healthy lifestyle. Changes in their knowledge were documented. Appropriate statistical analysis was done using Excel sheets.
Results:
Most (79%) of the women in the village had normal blood pressure, with 19% of them having mild and 2% had moderate HTN. Most hypertensive women (72%) were not taking medications. Out of 12 hypertensive women who were taking antihypertensive medications, half of them were regular. There was a significant improvement in the score of self-care capacity, treatment HTN diet-related knowledge of the women after the intervention. Respondents liked the idea of organizing drama to propagate health-related messages.
Conclusion:
One in every five persons in the study population of rural health training centre (RHTC) had HTN. Most hypertensive women (72%) were not taking medications. Those who were taking antihypertensive medications, only half were regular in it. After Nukkad Natak based intervention, there was a significant improvement in the scores of HTN diet and treatment-related knowledge and self-care capacity of the respondents for prevention of HTN. Our respondents liked the idea of organizing drama to propagate health-related messages.
Keywords
Hypertension
Street plays
Behavior Change Communication
Self-care capacity
Lifestyle modification
ABSTRACT IMAGE
INTRODUCTION
In 21st century, the impact of epidemiological transition is clearly visible through the change in disease profile of our society.[1] There is a decline in the incidence of communicable diseases (CDs). Non-communicable diseases (NCDs) such as hypertension (HTN), diabetes, cancer, cardiovascular diseases (CVDs), and stroke are on the rise at an alarming rate in both developed and developing countries with high mortality rates. CVD is the leading cause of death in women accounting for an estimated 17 million people each year. HTN, a major risk factor for CVDs, is fast becoming a major public health problem in India also. Globally, at least 50% HTN cases are remaining hidden and inadequately treated.[2] This issue becomes more serious for women, whose health is often neglected due to their low social status in the society.[3]
Globally, including India, the prevalence of HTN in adults is above 30%.[4-6] HTN control in them can result in a sizable reduction of CVD mortality. Still, there is suboptimal awareness, treatment, and control of HTN in women. Hence, there is a need for more attention to be given to find out and treat the hidden and untreated HTN cases in women.
Health promotion, which focuses on the pre-pathogenesis phase of disease, that is, before the appearance of risk factors, is the best strategy for prevention of NCDs. Adoption of health promoting lifestyle positively contributes to quality of life. For inculcating a healthy lifestyle, a salutogenic approach has been tried by the investigators earlier.[7-12]
Globally, at least 50% of the deaths, each year are related to lifestyle, which has emerged as an extremely useful construct in the health field theory.[13] Hence, more attention is now being given to the role of human behavior in changing the lifestyle as a major strategy for both prevention of CVDs and for promotion of health.[13] Health promotion is not directed against any disease but is intended to strengthen the host through a variety of approaches in the form of lifestyle and behavior change, health education, environmental modifications, and nutritional intervention.[7-12]
At community/grass root level, there is a need to adopt a simple health promotion approach, which a primary healthcare worker can use.[14]
Being a chronic disease, management of HTN requires active involvement of the patients themselves. Medicines are to be taken regularly, along with monitoring of laboratory investigations. This requires their adherence with the prescribed therapies. All this is intimately related to their behavior and habits. Various strategies have been tried in a plethora of health-care projects to bring about changes in health-related behavior of people.[15] However, often they get bored by the traditional sermonizing approaches. It has been advocated that an “infotainment” style of communication may be tried to transmit the message across to the intended audience in a subtle way. It will be worthwhile to study how the use of this approach of lifestyle modification (LSM) will work as an intervention to manage HTN among the village women.
Objectives
The objectives of this study were as follows:
To ascertain the prevalence of HTN (treated and untreated) among village women
To determine the impact of an intervention strategy of Behavior Change Communication utilizing a camp approach supplemented with nukkad natak on the self-care capacity of village women for LSM for prevention of HTN.
MATERIALS AND METHODS
The study was conducted during June–July 2023 in the field practice area of Community Medicine of a medical college. All adult women attending outpatient departments (OPD) of the field clinics were included in this study. Women not willing to participate were excluded.
A pre-tested, pilot tested questionnaire was used for data collection. The participants were examined for medical history and anthropometric measurements (height, weight, and body mass index), blood pressure (BP), treatment details, etc., and relevant history for lifestyle pattern were documented in pre- tested questionnaire.
Spectra Slim+ vital sign monitor was used to digitally measure BP and diagnose HTN. It was regularly calibrated against a mercury sphygmomanometer. To rule out coat HTN the investigators ensured that before measuring the BP, the subjects were sitting relaxed for at least 5 min without talking. They were asked to sit on a chair with their back supported. They were also asked to keep both feet flat on the ground, with their arms at heart level.
Sample size was arbitrary (n = 200) out of all willing women attending OPDs during the study period.
The intervention was carried out at a field practice area under a medical college. Beneficiaries were village women in the study area. A list of interns posted in Community Medicine Department was made. They were groomed for the project by honing their skills through appropriate training for conducting surveys, data collection, and pro forma designing/pretesting and imparting various components of the intervention regime. Then, the script of the nukkad natak on a healthy lifestyle was prepared. Rehearsals were done for the same. Logistics were arranged. The study did not interfere with the existing health-care regimes being used by the concerned users.
First, a baseline assessment of the study population was done. This focused on basic socio-demographic data of the families, their health status, treatment seeking behavior, etc. Their healthy lifestyle-related knowledge was also tested through appropriate tools. A pro forma was developed to record the intervention sessions and impact thereof.
Then, the first intervention session of nukkad natak with camp approach was held for the study population at an appropriate venue (after discussion with them and with the village leaders who were briefed about the project before starting the survey).
Documentation of the post-intervention changes in the healthy lifestyle-related knowledge of the study population was done, immediately after the session. The tool for the same focused only on the issues addressed in the drama.
Appropriate statistical analysis was done using Excel sheets. Percentage, mean, median, mode, standard deviation, Paired t-test, etc., were used. Outcome variables were scores on healthy lifestyle-related knowledge for prevention of HTN.
RESULTS
Table 1 demonstrates that 79% of the women in the village have normal BP, with 19% of them had mild and 2% had moderate HTN. As shown in Table 2, most hypertensive women (72%) were not taking medications. As shown in Table 3, out of 12 hypertensive women who were taking antihypertensive medications, half of them were regular in it. According to Table 4, 54.5% of over 60 years age group women were hypertensive as compared to 36.4% in 40– 60 years age range (Chi-square: 29.23; df: 2; P < 0.001 (Fig. in parentheses are %). Table 5 shows that among the housewives, 23.9% had HTN, as compared to 4.2% in students/skilled workers (Chi-square: 4.855, df: 1, P-value: 0.032; Fisher’s exact test). There was no association between educational/socioeconomic status of women and HTN. Table 6 demonstrates that there was a significant improvement in the score of self-care capacity-related knowledge of the women after the intervention (Paired t-statistic: 24.79, d.f.: 199, P = 0.000). Table 7 shows that there was a significant improvement between pre- and post-intervention score of HTN treatment knowledge of the subjects (Paired t-statistic: 79.82, d.f.: 199, P = 0.000). As shown in Table 8, there was a significant improvement between pre- and post-intervention score of knowledge of women about the HTN diet (Paired t statistic -13.820; d.f. = 199; P = 0.000).
| Category | Systolic or Diastolic (mm Hg) | No. | % |
|---|---|---|---|
| Normal | 130–140 or <90 | 157 | 78.5 |
| Hypertension stage 1 (mild) | 140–159 or 90–99 | 38 | 19 |
| Hypertension stage 2 (moderate) | 160–179 or 100–109 | 4 | 2 |
| Hypertension stage 3 (severe) | >180 or>110 | 1 | 0.5 |
n= Sample size.
| HTN stages | Takes treatment | Total | |
|---|---|---|---|
| Yes | No | ||
| 1 | 12 | 26 | 38 |
| 2 | 0 | 4 | 4 |
| 3 | 0 | 1 | 1 |
| Total | 12 (28%) | 31 (72%) | 43 |
HTN: Hypertension
| Regularity of treatment taken | Regular | Irregular | Total |
|---|---|---|---|
| No. | 6 | 6 | 12 |
| % | 50 | 50 | 100 |
| Age (years) | HTN | Total | |
|---|---|---|---|
| Yes | No | ||
| <40 | 9 (8) | 103 (92) | 112 |
| 40–60 | 28 (36.4) | 49 (63.6) | 77 |
| Above 60 | 6 (54.5) | 5 (45.5) | 11 |
| Total | 43 (21.5) | 157 (78.5) | 200 |
HTN: Hypertension
| Occupation | HTN | Total | |
|---|---|---|---|
| Yes | No | ||
| House wife | 42 | 134 | 176 |
| Students and skilled workers | 1 | 23 | 24 |
| Total | 43 | 157 | 200 |
HTN: Hypertension
| Awareness about various LSM domains of HTN prevention (score weightage) | Pre-intervention score | Post-intervention score | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Diet (10) | 5.93 | 1.22 | 9.86 | 0.46 |
| Weight reduction (10) | 5.21 | 0.86 | 9.69 | 0.74 |
| Yoga (10) | 4.44 | 1.05 | 9.79 | 0.81 |
| Meditation (5) | 2.58 | 1.30 | 4.72 | 0.58 |
| Exercises (10) | 2.85 | 1.28 | 9.44 | 1.16 |
| Sleep (5) | 2.56 | 0.96 | 4.86 | 0.51 |
| Total (50) | 23.55 | 2.68 | 48.35 | 3.20 |
LSM: Lifestyle modification, SD: Standard deviation, HTN: Hypertension
| Aspects of HTN treatment-related knowledge (score weightage) |
Pre-intervention score | Post-intervention score | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Medicinal treatment (15) | 5.81 | 0.69 | 12.65 | 1.40 |
| Lab monitoring (10) | 3.62 | 0.59 | 6.99 | 0.46 |
| Total (25) | 9.43 | 0.999 | 19.64 | 1.480 |
SD: Standard deviation, HTN: Hypertension
| Various domains of diet for HTN prevention (score weightage) |
Pre-intervention score | Post-intervention score | ||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Salt intake/day (10) | 6.91 | 0.53 | 9.94 | 0.24 |
| Sugar intake/day (5) | 3.03 | 0.20 | 4.89 | 0.32 |
| Oil (10) | 6.98 | 0.19 | 9.28 | 0.81 |
| Food to be avoided (10) | 4.89 | 0.32 | 8.47 | 0.56 |
| Outside food intake (10) | 5.06 | 0.29 | 8.11 | 0.42 |
| Total (50) | 26.85 | 0.58 | 40.67 | 1.50 |
HTN: Hypertension, SD: Standard deviation
The impact of using a village-based camp approach organizing street plays (nukkad nataks) on the self-care capacity of women for LSM for prevention of HTN in the study area is illustrated below in the form of subjective responses received from the study population–
Our respondents liked the idea of organizing drama to propagate health-related messages.
This was their first experience of participation (both as an audience as well as amateur actors).
They were glad to see, within their home setting that members from the health care team at RHTC, discussed individually with them about HTN prevention through LSM.
In general, the women liked the health communication technique used by our team through drama.
Use of local dialect in the drama enthused them.
Through demonstration mode during the drama, interested women learned to use the digital sphygmomanometer for HTN monitoring.
Through role play they were told about the crucial role of the family support in HTN management/prevention.
Participant women and their families were also assured about necessary treatment and referral support for HTN as per the need.
The interest of the respondents was evident by the way they asked questions during the open house session.
Majority of them wanted similar events in future. They were eager to attend educational sessions on HTN management.
DISCUSSION
HTN is the most common risk factor for CVDs such as coronary heart disease, stroke, renal disease, and peripheral vascular disease, which are the most common cause of death and disease globally as well as in India.[16-18] Awareness level of their HTN status among the patients was reported to 25–42% in India in various studies. The pooled estimate for awareness of BP in rural and urban India was 25.1% (21.0–29.1) and 41.9% (35.1–48.9), respectively.[4-6] The pooled estimate for the percentage of treated among those diagnosed with HTN in rural and urban areas as reported by researchers was 24.9 (16.7–33.0) and 37.6 (23.9–51.2), respectively.[19-21]
Hidden HTN phenomenon was amply demonstrated in this study, as most hypertensive women (72%), were not taking the prescribed medications. Regarding treatment adherence, only 50% among those who were taking antihypertensive medications were regular in it. This reflects a casual approach of the providers as well as the users regarding HTN management in the study area.
The pooled estimate for percentage of hypertensive patients having their BP under control in rural and urban India was 10.7 (6.4–15.0) and 20.2 (11.6–28.8), respectively. Thus, less than one-fourth of the Indian HT population has their BP under control. This is a serious matter of concern for policy makers. As per the rule of halves also, 50% of the HT people are undiagnosed. In any case, adherence to HTN treatment in known cases is poor everywhere (24.9–37.6% in India).[20-27]
Apparently, the current public health/mass level strategies are not working in this context. This is a serious matter of concern for policy makers. The low awareness and treatment levels among hypertensive patients signify a lower knowledge, attitude, and practice levels among patients. To address this issue, there is a need to foster a conducive communication ambience to convince HT patients to take the treatment prescribed by the concerned physician.
Globally also, adherence to any prescription or advice has been reported to be <50%. Reasons for this may be due to lack of realization of the gravity of the situation.[20,21]
It is a matter of human behavior change. Health belief model is applicable here through its “perceived susceptibility” and “perceived severity” paradigms. People may consider themselves not susceptible to developing HTN. Those who are diagnosed with HTN may not consider it as a severe enough disease which deserves attention/care.[9,10]
It is well known that HTN may have serious cardiovascular and cerebrovascular complications with potentially fatal consequences. In this context, there is a need to put the relevant messages across to the HTN patients and their families in an effective way.
The use of drama can be useful to achieve this, as demonstrated by our study results.[28-39]
The prevalence of HTN in the study population of RHTC (one in every five) was lower than its counterparts in UHTC population, that is, 39%.[40]
Social prescription concept was also implicit in our drama-based intervention as a group of people with similar sociodemographic and morbidity backgrounds were addressed through this strategy.[41] In Indian rural settings, like elsewhere, people do tend to follow the social norm through group dynamics. People do share their experiences and problems with others. They tend to follow advice, if they witness others doing the same thing.
There was significant improvement in the scores of self-care capacity, HTN diet, and treatment-related knowledge of the respondents after the intervention. The modalities of organizing health education sessions through infotainment mode for HTN were appreciated by the respondents. Our respondents liked the idea of organizing drama to propagate health-related messages.
Limitations of the study
This was a small-scale study of 2 months only with a small sample size. It did not include the long-term impacts of the intervention strategy on the self-care capacity of village women for prevention and control of HTN. Since this was a small scale, short-term quasi-experimental, single group, and before-after community-based trial, there is a need to conduct a full scale RCT using the similar intervention, with a control group. The results need to be interpreted in view of potential confounders like social desirability response.
Recommendations
Counseling sessions for motivating the village women for seeking requisite treatment and timely management of HTN need to be arranged. These need to be an engaging experience for the users. An “infotainment” style of communication, as tried in this study may be replicated.
CONCLUSION
One in every five persons in the study population of RHTC had HTN. Most hypertensive women (72%), were not taking medications. Only half of those who were taking antihypertensive medications, were regular in it. After the camp approach supplemented with Nukkad Natak based intervention, there was a significant improvement in the scores of HTN diet and treatment-related knowledge and self-care capacity of the respondents for prevention of HTN. Our respondents liked the idea of organizing drama to propagate health-related messages.
Ethical approval
The research/study was approved by the Institute Ethics Committee, vide its approval number SRMSIMS/ECC/2023/20 dated 02.05.2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Audio summary available at
Financial support and sponsorship
Prajjwalika scheme; WINCARS.
References
- The Global Epidemiologic Transition: Noncommunicable Diseases and Emerging Health Risk of Allergic Disease in Sub-Saharan Africa. Health Educ Behav. 2016;43(1 Suppl):37S-55.
- [CrossRef] [PubMed] [Google Scholar]
- Inadequate Hypertension Control Rates: A Global Concern for Countries of All Income Levels. J Clin Hypertens (Greenwich). 2022;24:362-4.
- [CrossRef] [PubMed] [Google Scholar]
- Gender Differences in Antihypertensive Treatment: Myths or Legends? High Blood Press Cardiovasc Prev. 2016;23:105-13.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic Diseases and Injuries in India. Lancet. 2011;377:413-28.
- [CrossRef] [PubMed] [Google Scholar]
- Diabetes and Hypertension in India: A Nationally Representative Study of 1.3 Million Adults. JAMA Intern Med. 2018;178:363-72.
- [CrossRef] [PubMed] [Google Scholar]
- Hypertension Screening, Awareness, Treatment, and Control in India: A Nationally representative Cross-sectional Study among Individuals Aged 15 to 49 years. PLoS Med. 2019;16:e1002801.
- [CrossRef] [PubMed] [Google Scholar]
- Salutogenic Potential and Health Promoting Behaviors of Indian Students - Sense of Coherence and Health Promoting Lifestyle Score: A Comparative Study of Manipuri and North Indian Students Saarbrucken, Germany: LAP Lambert Academic Publishing; 2012.
- [Google Scholar]
- Mantras for Healthy Lifestyle - A Salutogenic Approach New Delhi: Century Publications; 2012.
- [Google Scholar]
- Health Promotion: Need for Public Health Activism Vol 1. Germany: LAP LAMBERT Academic Publishing; 2013.
- [Google Scholar]
- Health Promotion: Need for Public Health Activism Vol 2. Germany: LAP LAMBERT Academic Publishing; 2013.
- [Google Scholar]
- Study of Sense of Coherence Health Promoting Behaviour in North Indian Students. Indian J Med Res. 2011;134:645-52.
- [CrossRef] [PubMed] [Google Scholar]
- Marc Lalonde, the Health Field Concept and Health Promotion. Case Stud Public Health 2018:523-41. doi: 10.1016/B978-0-12-804571-8.00028-7
- [CrossRef] [Google Scholar]
- Lifestyle Strategies for Risk Factor Reduction, Prevention, and Treatment of Cardiovascular Disease. Am J Lifestyle Med. 2018;13:204-12.
- [CrossRef] [PubMed] [Google Scholar]
- Factors Contributing to Medication Adherence in Patients with a Chronic Condition: A Scoping Review of Qualitative Research. Pharmaceutics. 2021;13:1100.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in Hypertension Epidemiology in India. J Hum Hypertens. 2004;18:73-8.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiovascular Mortality Associated with 5 Leading Risk Factors: National and State Preventable Fractions Estimated from Survey Data. Ann Intern Med. 2015;163:245-53.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence, Awareness, Treatment and Control of Hypertension among the Elderly in Bangladesh and India: A Multicentre Study. Bull World Health Organ. 2001;79:490-500.
- [Google Scholar]
- Treatment Adherence and Blood Pressure Outcome among Hypertensive Out-patients in Two Tertiary Hospitals in Sokoto, Northwestern Nigeria. BMC Cardiovasc Disord. 2020;20:68.
- [CrossRef] [PubMed] [Google Scholar]
- Hypertension Knowledge and Treatment Initiation, Adherence, and Discontinuation among Adults in Chennai, India: A Cross-sectional Study. BMJ Open. 2021;11:e040252.
- [CrossRef] [PubMed] [Google Scholar]
- Hypertension in India: A Systematic Review and Meta-analysis of Prevalence, Awareness, and Control of Hypertension. J Hypertens. 2014;32:1170-7.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and Predictors of Hypertension: Evidence from a Study of Rural India. J Family Med Prim Care. 2022;11:1047-54.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of Knowledge about Hypertension among Hypertensive Patients in Babylon Province. Med J Babylon. 2022;19:31-6.
- [CrossRef] [Google Scholar]
- The Effect of Training on Knowledge, Attitude, and Practice in Patients with Hypertension: The Application of the Expanded Chronic Care Model, A Clinical Trial Study. Iran Red Crescent Med J. 2018;20:e61693.
- [CrossRef] [Google Scholar]
- Impact of Literacy on Hypertension Knowledge and Control of Blood Pressure in a Southern Indian Tertiary Hospital. Cardiovasc Hematol Disord Drug Targets. 2021;21:136-40.
- [CrossRef] [PubMed] [Google Scholar]
- Good Knowledge about Hypertension is Linked to Better Control of Hypertension; A Multicentre Cross-sectional Study in Karachi, Pakistan. BMC Res Notes. 2012;5:579.
- [CrossRef] [PubMed] [Google Scholar]
- Theatre in Health Education In: Jackson T, ed. Learning through Theatre: New Perspectives on Theatre in Education (2nd ed). London: Routledge; 1993. p. :227-38.
- [Google Scholar]
- Effect of Radio Drama Intervention on Knowledge, Attitude, and Practice-Intention of Hypertension Prevention among the Working Class. Am J Health Educ. 2022;54:62-74.
- [CrossRef] [Google Scholar]
- Use of Mass Media Campaigns to Change Health Behavior. Lancet. 2010;376:1261-71.
- [CrossRef] [PubMed] [Google Scholar]
- Cost-effectiveness of Television, Radio, and Print Media Programs for Public Mental Health Education. Psychiatr Serv. 1998;49:808-11.
- [CrossRef] [PubMed] [Google Scholar]
- The Use of Educational Radio in Developing Countries: Lessons from the Past. Int J E-Learn Distance Educ. 1987;2:43-54.
- [Google Scholar]
- A Hands-on-Approach to Popularizing Radio Learning Group Campaigns. Convergence. 1983;16:14-22.
- [Google Scholar]
- Radio Nutrition Education - Using the Advertising Techniques to Reach Rural Families: Philippines and Nicaragua (Final Report) Washington, DC: Manoff International; 1977.
- [Google Scholar]
- Paraguay Using Radio for Formal Education in Rural Areas In: Academy News. Vol 2. Washington, DC: Clearinghouse on Development Communication; 1979. p. :4.
- [Google Scholar]
- Health Messages through Humor In: ICIT Report No. 15. Washington, DC: Clearinghouse on Development Communications; 1976.
- [Google Scholar]
- The Use of Educational Radio in Developing Countries: Lessons from the Past. Int J E-Learn Distance Educ. 1987;2:43-54.
- [Google Scholar]
- Unravelling the Spectrum of Hypertension among Adult Women in an Urban Area of North India Through Level of Prevention-Based Color-Coded Stratification. Indian J Cardiovasc Dis Women Wincars. 2023;9:22-7.
- [CrossRef] [Google Scholar]
- Implementing a Life Cycle Approach through Establishment of a Multipurpose Behavior Therapy Room in PGIMER, Chandigarh for Enhancing the Fitness Level of Women. J Postgrad Med Edu Res. 2017;51:115-22.
- [CrossRef] [Google Scholar]







