Translate this page into:
Hypertensive Disorders in Pregnancy
Lalita Nemani, DM Cardiology Associate Professor Department of Cardiology, Nizam’s Institute of Medical Sciences, Punjagutta 500082 Hyderabad, Telangana India drlalita775@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Hypertension in pregnancy is defined as systolic blood pressure (SBP) ≥ 140 mm Hg or diastolic blood pressure (DBP) ≥ 90 mm Hg or both on two different occasions at least 6 hours apart. Severe hypertension is SBP ≥ 160 mm Hg or DBP ≥ 110 mm Hg. Hypertension is the most common medical problem in pregnancy and one of the major causes of maternal and perinatal mortality and morbidity. Hypertensive disorders in pregnancy (HDP) are classified as (1) chronic hypertension, (2) chronic hypertension with superimposed preeclampsia, (3) preeclampsia-eclampsia, and (4) gestational hypertension. HDP contributes to increased risk of hypertension, stroke, and maternal cardiovascular disease (CVD) in later life. HDP can be considered as a failed cardiovascular stress test identifying women susceptible to CVD in later life. Further research is required to identify the mechanisms in HDP that contribute to CVD in later life so as to initiate appropriate prevention measures.
Keywords
eclampsia
gestational hypertension
hypertension
postpartum
preeclampsia
Introduction
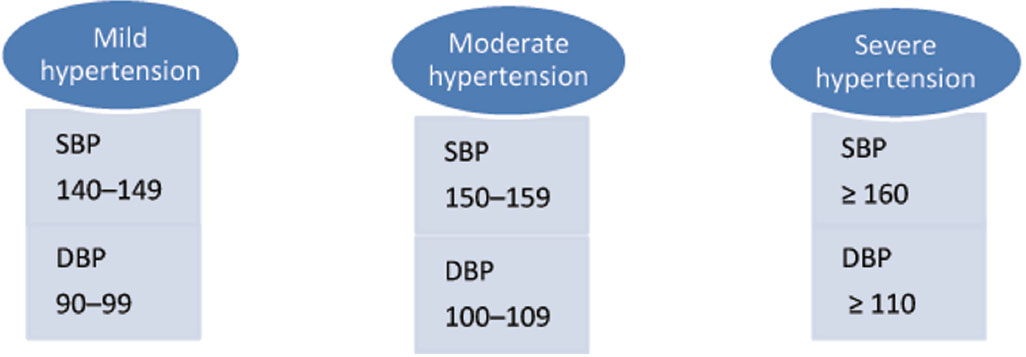
Hypertension in pregnancy is defined as systolic blood pressure (SBP) ≥ 140 mm Hg or diastolic blood pressure (DBP) ≥ 90 mm Hg or both on two different occasions at least 6 hours apart but no more than 1 week apart. An SBP of 140 to 159 and a DBP of 90 to 109 are considered as mild to moderate hypertension. Severe hypertension is SBP ≥ 160 mm Hg or DBP ≥ 110 mm Hg1 (Fig. 1).
-
Fig. 1 Grading of hypertension in pregnancy. DBP, diastolic blood pressure; SBP, systolic blood pressure.
Fig. 1 Grading of hypertension in pregnancy. DBP, diastolic blood pressure; SBP, systolic blood pressure.
Incidence and prevalence
Hypertension is the most common medical problem in pregnancy. Hypertensive disorders in pregnancy (HDP) occur in 10% pregnancies.1 They are one of the major causes of maternal and perinatal mortality and morbidity. Chronic hypertension accounts for 30% of HDP, and pregnancy-induced hypertension (PIH) occurs in 70%.2 Chronic hypertension complicates about 1 to 5% of pregnancies, gestational hypertension complicates around 5 to 6%, and preeclampsia complicates nearly 3 to 6% pregnancies according to population-based data.3 4
Classification
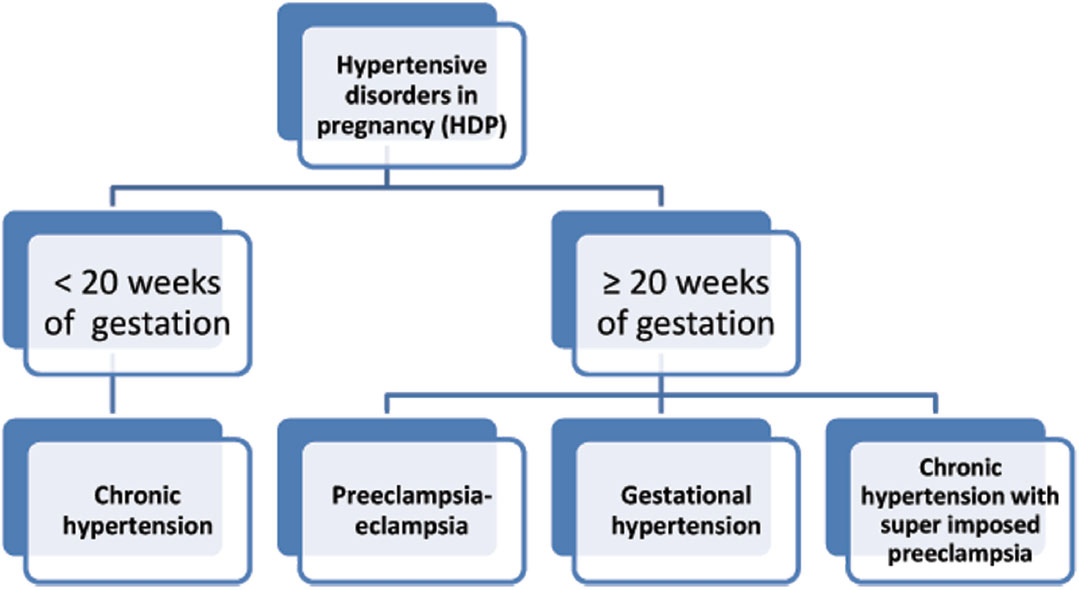
Hypertensive disorders during pregnancy are classified into four categories5 (Fig. 2).
-
Fig. 2 Classification of hypertensive disorders in pregnancy.
Fig. 2 Classification of hypertensive disorders in pregnancy.
Chronic Hypertension
Chronic hypertension is defined as hypertension known prior to conception, is detected before 20 weeks of gestation, and usually persists beyond 12 weeks postpartum. Occasionally blood pressure (BP) may be normal in the first trimester with hypertension detected before 20 weeks. In such cases, gestational hypertension or early preeclampsia must also be considered.
-
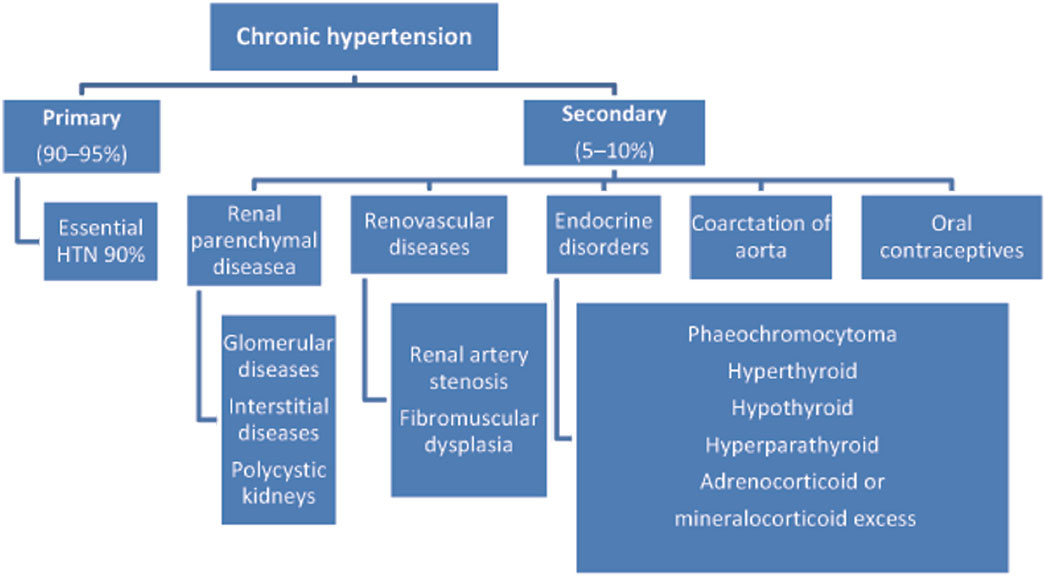
Etiology: Chronic hypertension is a primary hypertension in majority (90–95%) of the cases. However, secondary and potentially treatable causes are seen in a few (5–10%) that need to be evaluated and, if timely treated, could improve outcome in pregnancy (Fig. 3).
-
Incidence: Chronic hypertension is seen in around 22% of women of childbearing age with increasing incidence due to increasing age of the mother at the time of conceiving.
-
Maternal and fetal outcome: Preexisting hypertension is a risk factor for preeclampsia. Uncomplicated chronic hypertension in pregnancy is associated with increased maternal mortality and morbidity though quite less compared with those who develop superimposed preeclampsia (Fig. 4).
-
Fig. 3 Causes of chronic hypertension (HTN) in pregnancy.
Fig. 3 Causes of chronic hypertension (HTN) in pregnancy.

-
Fig. 4 Maternal and fetal outcome in chronic hypertension in pregnancy.
Fig. 4 Maternal and fetal outcome in chronic hypertension in pregnancy.
Adverse maternal outcome is more in uncomplicated chronic hypertensives when compared with normotensives. However, accelerated hypertension and organ damage are less likely without superimposed preeclampsia. Perinatal mortality is higher in uncomplicated chronic hypertension (relative risk [RR] 2.3) over normotensive and still higher in those with superimposed preeclampsia.
-
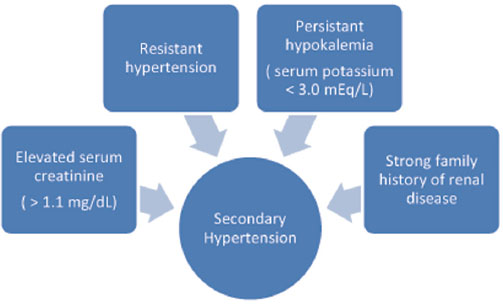
Preconception counseling: All women diagnosed with hypertension before or in early pregnancy should be counseled regarding the risks posed by hypertension in pregnancy. They should be educated about the signs and symptoms of preeclampsia. Whenever secondary hypertension (Fig. 5) is suspected, the patient should be thoroughly evaluated to rule of correctable causes of hypertension.
-
Fig. 5 Clues to evaluate for secondary hypertension.
Fig. 5 Clues to evaluate for secondary hypertension.
Investigations
-
All patients should undergo routine biochemical tests such as:
-
Serum creatinine, uric acid, electrolytes, liver functional test (LFT), thyroid assessment, and urine protein.
-
If proteinuria is detected, 24-hour urine protein or urine protein-to-creatinine ratio spot urine should be done and ultrasonography of the kidneys should be done.
-
Glucose tolerance test should be done in all as these patients are prone for gestational diabetes.
-
A baseline echocardiography for left ventricular hypertrophy and function assessment is ideal.
-
Case-based evaluation to rule out treatable conditions such as pheochromocytoma and renal artery stenosis.
-
Treatment and Management
The goal of treating chronic hypertension in pregnancy is to avoid its acute complications and reduce the fetal risk posed by hypertension itself and the medications used for it. The aim is to ensure a healthy and safe pregnancy if possible till term.
American College of Obstetricians and Gynecologists (ACOG) task force recommendations1 for hypertension management in pregnancy are
-
Home BP monitoring to ensure better control in patients with poorly controlled hypertension.
-
Ambulatory BP monitoring to rule out suspected white coat hypertension to avoid over treating hypertension.
-
Patients with chronic hypertension on medications can be
-
Off their medications and closely monitored as BP normally drops during pregnancy
-
Continue their medications if warranted and safe
-
Shift to alternate group of medications if their antihypertensive medication is not safe in pregnancy.
-
Closely monitored for symptoms of worsening hypertension and/or preeclampsia.
-
Most patients with mild to moderate hypertension can be managed without medications. Antihypertensive drugs are mandatory if SBP exceeds 160 or if DBP exceeds 110 mm Hg. However, lower thresholds (Fig. 6) for initiating antihypertensive drugs are recommended in special circumstances.

-
Fig. 6 Criteria for chronic hypertension with superimposed preeclampsia.
Fig. 6 Criteria for chronic hypertension with superimposed preeclampsia.
Nonpharmacologic Measures
-
The role of aerobic exercise and Dietary Approaches to Stop Hypertension (DASH) diet to reduce BP in pregnant women is not established. Its harmful effects, if any, have also not been studied. Those accustomed to exercise with no obstetric contraindications and well-maintained BP can continue with moderate less of aerobic exercise.
-
Weight loss and extremely low-salt diet (< 100 mEq/d) are not recommended in pregnancy.
Pharmacologic Measures
Patients of chronic hypertension on medication should maintain their SBP between 120 and 160 mm Hg and DBP between 80 and 105 mm Hg.
-
Labetalol, nifedipine, and methyldopa are the preferred agents for initial treatment of chronic hypertension in pregnancy
-
Angiotensin-converting enzyme (ACE) inhibitor, angiotensin receptor blockers (ARBs), and spironolactone agonists should be avoided.
-
Meta-analysis and systemic reviews have suggested a beneficial role for low-dose aspirin when started early in pregnancy (a small but definite reduction in incidence of preeclampsia in high-risk patients).
-
Calcium supplementation positively reduces the incidence of hypertension, prevents preeclampsia in high-risk patients, and is recommended.
Optimal timing for delivery in uncomplicated chronic hypertension in pregnancy is 38 to 39 weeks of gestation. Normal vaginal delivery is recommended, and cesarean section is limited to obstetric indications.
Chronic Hypertension with Superimposed Preeclampsia
When organ damage is present, it is known as superimposed preeclampsia with severe features (Fig. 6).
Superimposed preeclampsia develops in 13 to 40% of patients with chronic hypertension.
Investigations
The magnitude of proteinuria should be assessed and compared with baseline levels. A complete blood picture with hemoglobin, platelet count, and LFT is essential. Lactic acidosis, uric acid, and creatinine assessment are required in severe preeclampsia to assess prognosis. Fetal growth and well-being should be monitored periodically.
Maternal and Fetal Outcome
Adverse maternal outcome in terms of abruptio placenta, postpartum hemorrhage, and accelerated hypertension is more in superimposed preeclampsia, especially with severe feature. Perinatal mortality is also more (RR 3.6) over uncomplicated chronic hypertension.
Treatment and Management
-
Treatment of patients with mild to moderate hypertension has shown to decrease the occurrence of severe hypertension by 50% but does not prevent development of preeclampsia (Cochrane database reviews).6 7 8 β-Blockers and calcium channel blockers (CCBs) appear superior to α-methyldopa in preventing preeclampsia.8 Acute treatment of severe hypertension can be achieved by intravenous (IV) labetalol or oral nifedipine or hydralazine. Oral labetalol, nifedipine, and methyldopa are the initial agents for maintenance of BP after acute control.
-
Antepartum management includes corticosteroid administration for fetal maturity if < 34 weeks of gestation. This is proved to reduce perinatal mortality and morbidity.
-
Eclampsia is seen in 0 to 2.4% cases of superimposed preeclampsia. Role of intrapartum magnesium sulphate for seizure prevention in this subset of superimposed preeclampsia has not been studied. Task force recommendation is to administer prophylactic intrapartum magnesium sulphate for prevention of seizure in superimposed preeclampsia with severe features.
Nearly 34 to 37 weeks of gestation is the ideal time for delivery. However, delivery of the fetus is recommended irrespective of the gestational age after stabilization of the mother when superimposed preeclampsia complicated by uncontrolled BP, eclampsia, pulmonary edema, abruptio placenta, disseminated intravascular coagulation (DIC), or fetus in jeopardy.
Preeclampsia-Eclampsia
Preeclampsia is defined as new onset of hypertension detected after 20th week of gestation association with proteinuria. The revised definition according to the ACOG has defined preeclampsia independent of the presence of proteinuria. In the absence of proteinuria, preeclampsia is defined as new onset of hypertension with any one of the following: thrombocytopenia, renal insufficiency, impaired LFT, pulmonary edema, and cerebral or visual symptoms (Fig. 7).

-
Fig. 7 Diagnostic criteria for preeclampsia with their definitions. DBP, diastolic blood pressure; SBP, systolic blood pressure.
Fig. 7 Diagnostic criteria for preeclampsia with their definitions. DBP, diastolic blood pressure; SBP, systolic blood pressure.
Preeclampsia with severe features is considered when BP is ≥ 160/110 mm Hg and is associated with thrombocytopenia, renal insufficiency, impaired liver function, pulmonary edema, and visual or cerebral symptoms.
Eclampsia refers to new onset of generalized seizure (grand mal epilepsy) in patients with preeclampsia.
HELLP syndrome is considered as a subtype of preeclampsia in which pregnant women present with constellation of finding that are Hemolysis, Elevated Liver enzymes, and Lower Platelet count.
Etiology
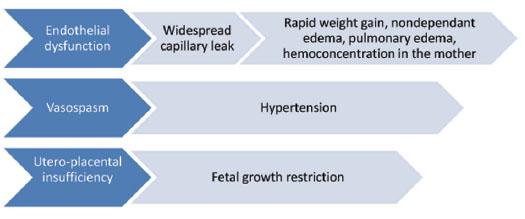
Preeclampsia is a syndrome characterized by widespread endothelial dysfunction and vasospasm (Fig. 8). Altered maternal immune response to fetal/placental tissue also contributes.
-
Fig. 8 Etiopathogenesis of preeclampsia.
Fig. 8 Etiopathogenesis of preeclampsia.
Risk Factors for Preeclampsia
Preeclampsia is common in first pregnancy, extreme age of pregnancy (< 18 years and > 35 years), obese women, family history of preeclampsia (two- to fourfold), and multiple pregnancies. Chronic hypertension, especially secondary, diabetes, obesity, systemic lupus erythematosus (SLE), and migraine all increase the risk for development of preeclampsia. Preeclampsia recurs in subsequent pregnancies, and the history of preeclampsia in previous pregnancy increases the risk for recurrence by sevenfold.
However, preeclampsia is noted most times in healthy nulliparous women with no comorbidity. Prediction of preeclampsia based on clinical risk factors could predict preeclampsia in 37% patients with a false-positive rate of 10%.9 Uterine artery Doppler studies and combination of biomarkers could enhance the clinical accuracy of early detection of preeclampsia.
Investigations
All women should get a baseline complete blood count (CBC), serum creatinine, uric acid, LFTs, and proteinuria assessment. Platelet counts, liver enzymes, and proteinuria should be reassessed weekly in mild preeclampsia. In severe preeclampsia CBC, serum creatinine, and LFTs need to be repeated daily (alternate day if the mother appears stable).
Treatment and Management
Mild Preeclampsia
-
Salt restriction, strict bedrest, and restriction of physical activity are not recommended.
-
Mother should be educated to report symptoms of severe preeclampsia such as severe headache, visual disturbances, epigastric pain, and shortness of breath.
-
Mother should be taught to monitor fetal movements daily.
-
BP measurements should be done twice weekly other than at antenatal visits.
-
Preeclampsia with BP persistently < 160/110 mm Hg, antihypertensives need not be administered.
-
Optimal timing of delivery is 37 weeks. Mild preeclampsia at or beyond 37 weeks, delivery is recommended rather than expectant management.
-
Magnesium sulphate for prevention of seizures is not routinely advised in the absence of maternal symptoms.
Severe Preeclampsia
-
Severe hypertension should be controlled with antihypertensives to prevent the cardiovascular (CV), cerebrovascular and renal complications.
-
Hydralazine, labetalol, and nifedipine remain the initial agents of choice to be used in severe hypertension
-
All patients should receive prophylactic magnesium sulphate for prevention of seizures.
-
Prompt delivery is the safest option for severe preeclampsia with organ involvement. In the few cases in which the mother is stable, optimal timing for delivery is 34 weeks.
-
Corticosteroid for fetal lung maturity should be given if < 34 weeks of gestation.
Eclampsia
-
All patients should receive intrapartum magnesium sulphate. Ideally it should be continued for 24 hours after last seizure.
-
Loading dose of 4 to 6 mg IV followed by maintenance dose of 1 to 2 mg/h for at least 24 hours.
-
Magnesium sulphate should be continued intraoperatively for those undergoing cesarean section. The half-life of MgSO4 is 5 hours; if the medication is discontinued before delivery or CS, the serum levels decrease and the patient is at risk of postpartum seizures.
-
All women should undergo delivery following stabilization.
HELLP Syndrome
-
Prompt delivery is advised.
-
A course of corticosteroids are beneficial in term of improving maternal platelet counts without any effect on maternal and perinatal mortality.
Gestational Hypertension
Gestational hypertension is defined as sustained hypertension detected after 20th week of pregnancy in a previously normotensive woman without the evidence of proteinuria. It usually disappears by 12 weeks postpartum. It is the most common cause of hypertension during pregnancy. Incidence varies from 6 to 17% in nulliparous women to 2 to 4% in multiparous women. Though a transient condition, these patients should be carefully monitored as preeclampsia can develop in one-third of these patients. Gestational hypertension is a risk factor for development of chronic hypertension at later age.
Postpartum Hypertension
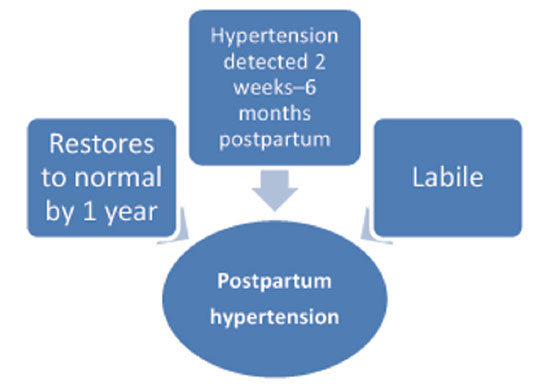
Blood pressure usually dips and remains low for 48 hours after delivery and then starts to rise. Hypertension detected after 72 hours postpartum is known as postpartum hypertension (Fig. 9).
-
Fig. 9 Features of postpartum hypertension.
Fig. 9 Features of postpartum hypertension.
Though transient in nature, it could be a harbinger of chronic hypertension in later life.
Evaluation of Hypertension in Pregnancy
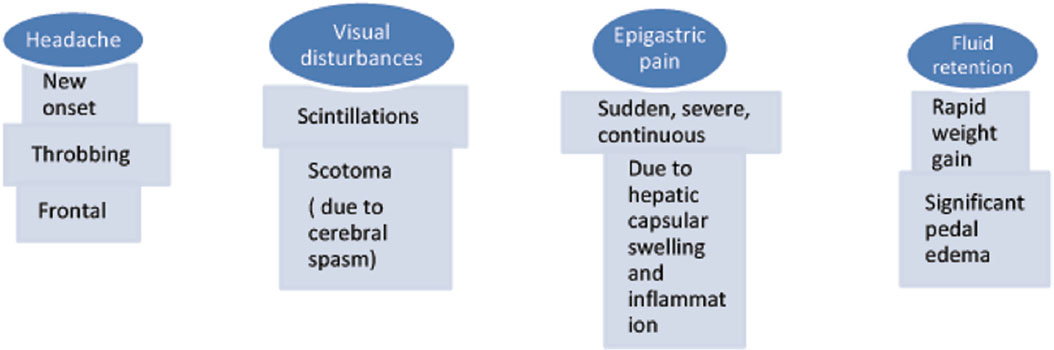
A proper history, clinical examination, and basic investigations are necessary in all cases of hypertension in pregnancy. All women with hypertension in pregnancy should be educated to report symptoms of preeclampsia, which are represented in Fig. 10.
-
Fig. 10 Warning symptoms of preeclampsia.
Fig. 10 Warning symptoms of preeclampsia.
Guidelines for Blood Pressure Measurement in Pregnant Women
-
Blood pressure should be recorded at each antenatal visit. It should be measured after a period of rest in a quiet environment in the sitting position with the arm at the level of the heart using an appropriately sized cuff (i.e., length 1.5 times the circumference of the arm).
-
Manual measurement with a standard mercury sphygmomanometer is the recommended. Automated devices are not recommended in PIH.
-
Supine recording and left lateral position recording could be spuriously low due to inferior vena cava (IVC) compression by the gravid uterus.
-
The arm with higher BP values should be used for further BP monitoring.
-
Repeat BP measurement after a gap of at least 15 minutes when BP is high.
-
Korotkoff’s first and fifth sounds are taken as systolic and diastolic pressure, respectively, in a few patients; fourth sound is considered when the fifth sound approaches zero.
Cardiovascular Findings
-
S4 is abnormal in pregnancy and suggests left ventricular hypertrophy due to chronic hypertension or diastolic dysfunction due to preeclampsia-induced vasospasm.
-
S3 is normally heard in pregnancy; however, S3 gallop is abnormal.
-
Carotid bruit is in favor of atherosclerosis and suggests chronic hypertension.
-
Diminished pulses/unequal pulses suggest coarctation of the aorta.
Other Systems
-
Systolic bruit in the abdomen or flank suggests renal artery stenosis.
-
Retinal spasm/edema and macular detachment—severe preeclampsia.
-
Liver swelling and capsular stretch—pain in the right upper quadrant.
-
Clonus in seen in severe preeclampsia. Seizures are a sign of eclampsia.
Investigations
All patients should have these routine investigations once diagnosed with PIH:
-
Complete blood picture.
-
Blood urea nitrogen (BUN), creatinine and serum electrolytes, calcium, and magnesium.
-
Liver function tests.
-
Urine dips for proteins (urine protein-to-creatinine ratio).
-
Twenty-four hours urine for creatinine clearance and protein excretion.
-
Proteinuria > 300 mg is considered abnormal.
-
Creatinine clearance < 100 mL/min is abnormal and suggestive of renal dysfunction.
-
-
Hemoglobin (HbA1C), thyroid function tests, and serum uric acid are recommended.
-
Uric acid levels > 5 mg are abnormal and suggestive of tubular dysfunction.
-
-
Evaluation of lipid profile, hyperaldosteronism, and hypercortisolism should be deferred till postpartum period.
-
Screening for preeclampsia: Although algorithms based on risk factors, uterine Doppler, and biomarkers have been suggested, no guidelines recommend them other than screening by risk factors.
-
Testing for prothrombin time–international normalized ratio/activated partial thromboplastin time (PT-INR/aPTT) is recommended in the presence of thrombocytopenia and abnormal LFT.
-
Testing for DIC and hemolysis by checking levels of lactate dehydrogenase (LDH), D-dimer, fibrinogen, and haptoglobulin is recommended when coagulation defects are detected.
-
-
Electrocardiogram (ECG) and 2D echocardiography are recommended in all cases of PIH.
-
Chest X-ray, computed tomography (CT) of the brain, magnetic resonance imaging (MRI) of the brain, magnetic resonance angiography (MRA), and magnetic resonance venography can be done safely without fetal risk as the situation demands.
-
Close monitoring of the fetus is essential as placental hypoperfusion resulting in fetal restricted growth and intrauterine death are common. Monthly ultrasound for fetal growth and weekly biophysical profile or twice weekly nonstress tests are suggested.
Treatment and Management
-
Acute severe hypertension: This is a medical emergency and requires immediate attention and treatment. The ACOG10 11 Committee on Obstetric Practice issued updated guidelines (2015 and 2017) regarding the emergency treatment of acute-onset severe hypertension during pregnancy:
-
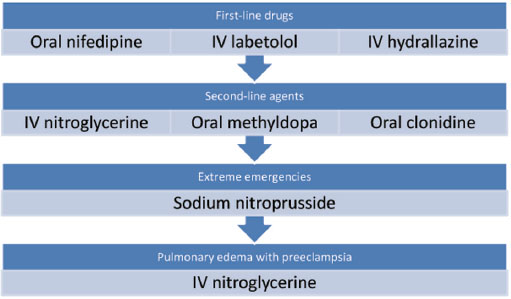
Acute severe hypertension (SBP > 160 and DBP > 110 mm Hg) diagnosed using standard devices and technique that is persistent for 15 minutes is a medical emergency. BP should be reduced to safe levels within 30 minutes to prevent maternal stroke. Pharmacologic algorithm is mentioned in Fig. 11.
-
Oral nifedipine or oral labetalol 200 mg can be given while procuring an IV access with dose repeated in 30 minutes is required.
-
Magnesium sulfate is recommended for seizure prophylaxis in severe preeclampsia and for controlling seizures in eclampsia.
-
Sodium nitroprusside is for extreme emergencies and for the shortest possible time—cyanide and thiocyanate toxicity in the mother and fetus, aggravating cerebral edema in the mother.
-
Individuals and institutions should adopt standard guidelines for managing patients with preeclampsia and be equipped to initiate prompt treatment for hypertensive emergency. Drugs and their dosages are mentioned in Table 1.
-
-
Fig. 11 Pharmacologic treatment for acute severe hypertension in pregnancy.
Fig. 11 Pharmacologic treatment for acute severe hypertension in pregnancy.
|
Drug |
Dose |
Onset of action (min) |
Caution |
|---|---|---|---|
|
Abbreviations: DOC, IV, intravenous. |
|||
|
Labetalol |
Initial dose: 20 mg IV, followed by 20–80 mg IV q30min Or 1–2 mg/min, max 300 mg (then oral) |
5 |
Contraindicated in asthma, heart failure |
|
Nifedipine |
5–10 mg capsule (swallowed/chewed) repeat every 30 min |
5–10 |
Sudden hypotension in mother |
|
Hydralazine |
Initial dose of 5 mg IV, followed by 5–10 mg IV every 30 min Or 0.5–10 mg/h IV, (max of 20 mg IV (or 30 mg IM) |
5 |
Sudden hypotension in mother |
|
Sodium nitroprusside |
0.25–5.0 µg/kg/min IV |
DOC in hypertensive crisis Caution—causes fetal cyanide poisoning |
|
|
Nitroglycerine |
IV infusion of 5 mg/min, and gradually increased every 3–5 min to a maximum dose of 100 mg/min |
DOC in preeclampsia with pulmonary edema |
|
There is no difference between in the efficacy of the three first agent drugs12 in terms of control of hypertension, and preference of one over other is left to the treating physician discretion.10 11 12
-
Mild to moderate hypertension: Nonpharmacologic treatment is recommended. According to the Cochrane database,13 14 15 treatment of mild-to-moderate hypertension during pregnancy with antihypertensive reduces the risk of progression to severe hypertension by 50% but does not prevent preeclampsia. Another large multinational RCT also supports this fact. β-Blockers and CCBs appear superior to α-methyldopa in preventing preeclampsia
-
Bedrest and salt restriction are not recommended.
-
All patients need close monitoring for detection of disease progression.
-
Review of small trials showed no improved outcome with strict BP control to a target < 130/80. However, in women with preexisting end-organ damage due to chronic hypertension, a lower threshold for initiating antihypertensive medication (> 139/89 mm Hg) is recommended. In these patients, the aim is for a lower target BP, that is, < 140/90 mm Hg.
-
All patients at risk for preeclampsia should receive 75 mg of aspirin daily and calcium supplementation.
-
-
Severe hypertension: SBP > 160 mm Hg increases the risk of intracerebral hemorrhage in the mother, whereas DBP > 110 mm Hg is associated with abruptio placenta and fetal growth restriction. Hence antihypertensive medication should be started when SBP is > 160 and/or DBP > 110 mm Hg. Multiple trails have compared the different antihypertensives in pregnancy, and none have proved superior to other in terms of efficacy. However, β-blockers and CCBs appear superior to methyldopa in prevention of preeclampsia.16 The different drugs available for use in severe hypertension are mentioned in Table 2.
|
Drug |
mechanism |
Onset of action |
duration |
Dosage |
Comments |
|---|---|---|---|---|---|
|
Labetalol |
Nonselective β-blocker with A receptor blocking action |
200–2,400 mg/d in 2 or 3 divided doses |
Well tolerated and relatively safe Contraindicated in asthma and congestive heat failure Safe on fetus |
||
|
Nifedipine |
Calcium channel blocker |
30–120 mg/d either as short acting or SR |
Well tolerated and safe Avoid sublingual form—high risk of maternal hypotension Safe on fetus |
||
|
Methyldopa |
Centrally acting α2-adrenergic agonist activity |
0.5–3.0 g/d in 2–3 divided doses |
Safe in pregnancy and fetus Gradual control of blood pressure (BP). Not effective for rapid reduction |
||
|
Thiazide diuretics |
Second-line agents |
May cause intravascular depletion and fetal restricted growth, however, not proven in trials |
|||
|
Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) are not approved for use during pregnancy; they are fetotoxic. Patients with chronic hypertension who are on these agents should be switched to other recommended first class agents. |
|||||
|
Among the agents recommended, no specific agent is first choice because there are no data supporting one over another. |
|||||
According to European Society of Cardiology, recommendations for the management of hypertension in pregnancy are:
A. Under class 1C:
-
Nonpharmacological management for pregnant women with SBP of 140–150 mm Hg or DBP of 90–99 mm Hg.
-
In women with gestational hypertension, or preexisting hypertension superimposed by gestational hypertension, or with hypertension and subclinical organ damage or symptoms at any time during pregnancy, initiation of drug treatment is recommended at a BP of 140/90 mm Hg. In any other circumstances, initiation of drug treatment is recommended if SBP ≥ 150 mm Hg or DBP ≥ 95 mm Hg.
-
SBP ≥ 170 mm Hg or DBP ≥ 110 mm Hg in a pregnant woman is an emergency, and hospitalization is recommended.
-
Induction of delivery is recommended in gestational hypertension with proteinuria with adverse conditions such as visual disturbances, coagulation abnormalities, or fetal distress.
-
In preeclampsia associated with pulmonary edema, nitroglycerin administered as an intravenous infusion is recommended.
-
In severe hypertension, drug treatment with intravenous labetalol or oral methyldopa or nifedipine is recommended.
B. Under class 2A:
Women with preexisting hypertension should be considered to continue their current medication except for ACE inhibitors, ARBs, and direct renin inhibitors under close BP-monitoring.
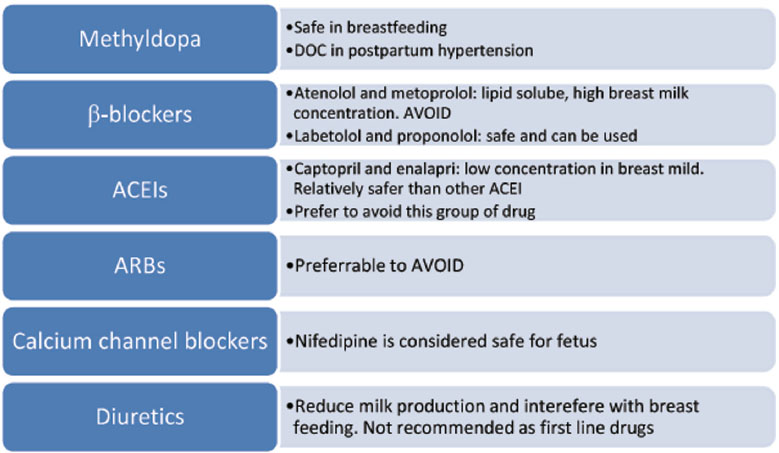
Management of postpartum hypertension: Antihypertensive drugs safe in breast-feeding are recommended (Fig. 12). Drugs that are bound to plasma proteins are less likely to be transmitted in breast milk. Water-soluble drugs are preferred to lipid soluble.
-
Fig. 12 Drug classes for management of postpartum hypertension. ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; DOC,.
Fig. 12 Drug classes for management of postpartum hypertension. ACEI, angiotensin-converting enzyme inhibitor; ARB, angiotensin receptor blocker; DOC,.
Hypertension in Pregnancy and Future Cardiovascular Risk
-
Hypertensive disorders in pregnancy are associated with increased risk (sevenfold) of hypertension, stroke, and maternal cardiovascular disease (CVD) in later life.
-
The risk is higher in those with history of preeclampsia, recurrent preeclampsia, preterm delivery, and fetal restriction. The risk of CVD is compounded by the presence of obesity or overweight.
-
All women with any subtype of HDP face the brunt. Women with gestational hypertension are at greater risk. No difference between patients who have received medication or not for hypertension during pregnancy. Severity of hypertension correlated with hypertension in later life.
-
These women experience chronic hypertension and cardiovascular (CV) risk almost a decade earlier than their normotensive counterparts.
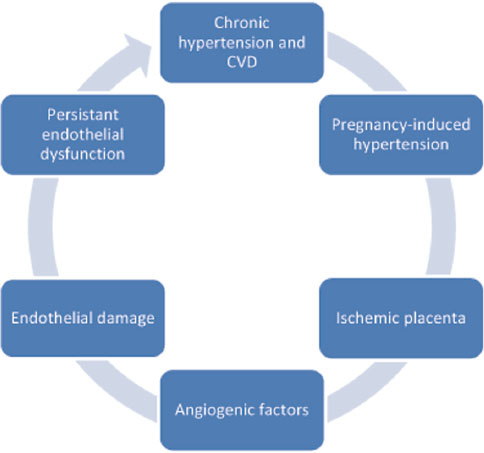
Pathophysiology
There is no uniform consensus on the mechanisms that contribute to increased CV risk in HDP patients. In fact, HDP and CVD share common risk factors such as insulin resistance, inflammation, obesity, and hypertension.17 18 Parity is an independently risk factor for future CVD; they are related in a J-shaped fashion, with the two having the lowest risk.17 19 The two hypotheses for the increased CV risk include endothelial dysfunction and familial propensity to hypertension and CVD.
-
These patients demonstrate an abnormal response to placenta known as ischemic placenta wherein the placenta shows shallow invasion of trophoblasts. The abnormal placenta releases antiangiogenic proteins resulting in endothelial dysfunction. Endothelial dysfunction was initially thought to reverse to prepregnancy state by 12 weeks postpartum. However, studies have demonstrated that this endothelial dysfunction persists and contributes to the risk of CVD in later life (Fig. 13). The risk is equal to that contributed by obesity and/or smoking. HDP women are found to have increased arterial stiffness.
-
○ A familial disposition in these patients to chronic hypertension has been suggested. It was noticed that hypertension and CV manifestation occurred even in normotensives siblings of HDP women.
-
Fig. 13 Pathophysiology of HDP and cardiovascular disease (CVD) in later life.
Fig. 13 Pathophysiology of HDP and cardiovascular disease (CVD) in later life.
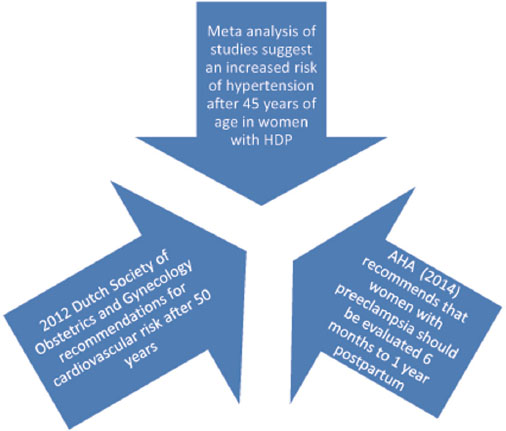
Screening for CVD: The ACOG task force on hypertension in pregnancy emphasizes on early identification of young women at risk for CVD in later life through proper screening and prevention.
Currently, HDP women are routinely discharged from obstetric department without a proper CV advice and follow-up despite established data about the associated increased CVD risk. Unfortunately, there are no standard guidelines on screening and treatment for CV risk factors in women with a history of HDP.20 21 No specific time frame for screening has been studied.
-
The American Heart Association (AHA) (2014) recommends (Fig. 14) that women with preeclampsia should be evaluated 6 months to 1 year postpartum to assess and potentially treat CV risk factors, including hypertension, obesity, smoking, and dyslipidemia.
-
The 2012 Dutch Society of Obstetrics and Gynecology recommendations for CV risk management after HDP (especially preeclampsia) are
-
○ Six weeks postpartum 49 years of age: All women should be educated about the increased CV risk that they would face and encourage lifestyle modification to optimize modifiable CV risk factors.
-
○ A complete CV risk profile assessment at the age of 50 years.
-
Fig. 14 Recommendations for CV risk screening.
Fig. 14 Recommendations for CV risk screening.
All women who had HDP should be closely monitored for CV risk factors such as hypertension, hyperglycemia, and dyslipidemia.
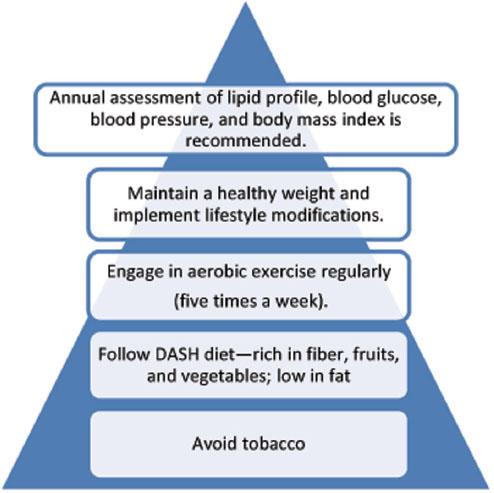
Lifestyle interventions are the cornerstone of prevention strategies after HDP (Fig. 15). They have the potential to decrease CV risk by 4 to 13%.
-
Fig. 15 Recommendations for prevention of CV risk following hypertensive disorders in pregnancy (HDP). DASH, Dietary Approaches to Stop Hypertension.
Fig. 15 Recommendations for prevention of CV risk following hypertensive disorders in pregnancy (HDP). DASH, Dietary Approaches to Stop Hypertension.
Conclusion
Hypertensive disorders of pregnancy are a major issue of concern for the mother and her infant. Pregnancy with its enormous influence on the CV physiology is like a stress test in a woman’s life. Hypertensive disorders in pregnancy can be considered as a failed CV stress test identifying the woman susceptible to CVD in later life. Pregnancy can be considered as a channel to identify women who are at risk for future CVD. As clinicians, we should utilize this channel to implement lifestyle modification in women to reduce their future burden of CVD. Further research is required to identify the mechanisms in pregnancy and HDP that contribute to CVD in later life so as to initiate appropriate preventive measures.
References
- The Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. ACOG; 2013
- Chronic hypertension in pregnancy. ACOG Practice Bulletin No. 29. Obstet Gynecol. 2001;98:177-185.
- [Google Scholar]
- Hypertensive disorders in pregnancy.Textbook of Critical Care. (7th ed.). Philadelphia, PA: Elsevier; 2016. In: eds.
- [Google Scholar]
- Antihypertensive therapy and central hemodynamics in women with hypertensive disorders in pregnancy. Obstet Gynecol. 2009;113(03):646-654.
- [Google Scholar]
- Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Am J Obstet Gynecol. 2000;183(01):S1-S22.
- [Google Scholar]
- Essential and Secondary Hypertension.The Brigham Intensive Review of Internal Medicine. (2nd ed.). Oxford, UK: Oxford University Press; 2014. In: 621–635
- [Google Scholar]
- Presence of baseline prehypertension and risk of incident stroke: a meta-analysis. Neurology. 2011;77(14):1330-1337.
- [Google Scholar]
- Meta-analysis of cohort studies of baseline prehypertension and risk of coronary heart disease. Am J Cardiol. 2013;112(02):266-271.
- [Google Scholar]
- Impact of baseline prehypertension on cardiovascular events and all-cause mortality in the general population: a meta-analysis of prospective cohort studies. Int J Cardiol. 2013;168(05):4857-4860.
- [Google Scholar]
- Diagnosis, evaluation, and management of the hypertensive disorders of pregnancy: executive summary. J Obstet Gynaecol Can. 2014;36(07):575-576.
- [Google Scholar]
- Committee Opinion No. 514: emergent therapy for acute-onset, severe hypertension with preeclampsia or eclampsia. Obstet Gynecol. 2011;118(06):1465-1468.
- [Google Scholar]
- Oral nifedipine versus intravenous labetalol for acute blood pressure control in hypertensive emergencies of pregnancy: a randomised trial. BJOG. 2012;119(01):78-85.
- [Google Scholar]
- Antihypertensive drug therapy for mild to moderate hypertension during pregnancy. Cochrane Database Syst Rev. 2014;2(02):CD002252.
- [Google Scholar]
- Tight control of mild-moderate pre-existing or non-proteinuric gestational hypertension. Cochrane Database Syst Rev (07):CD006907.
- [Google Scholar]
- Less-tight versus tight control of hypertension in pregnancy. N Engl J Med. 2015;372(05):407-417.
- [Google Scholar]
- Drugs for treatment of very high blood pressure during pregnancy. Cochrane Database Syst Rev. 2013;7(07):CD001449.
- [Google Scholar]
- Cardiovascular disease risk in women with pre-eclampsia: systematic review and meta-analysis. Eur J Epidemiol. 2013;28(01):1-19.
- [Google Scholar]
- Pre-eclampsia and risk of cardiovascular disease and cancer in later life: systematic review and meta-analysis. BMJ. 2007;335:974. 7627
- [Google Scholar]
- 2016 European Guidelines on cardiovascular disease prevention in clinical practice: the Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts): Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR) Eur J Prev Cardiol. 2016;23(11):NP1-NP96.
- [Google Scholar]
- Cardiovascular risk management after reproductive and pregnancy-related disorders: a Dutch multidisciplinary evidence-based guideline. Eur J Prev Cardiol. 2016;23(17):1863-1879.
- [Google Scholar]







