Translate this page into:
Gender Specific Coronary Artery Diameters in CT Coronary Angiogram: A Comparative Study in Female and Male Population
*Corresponding author: Bairy Thejasree, Department of Radiology and Imageology, Nizams Institute of Medical Sciences, Hyderabad, Telangana, India. thejasreebairy10@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Thejasree B, Patnaik S, Maddury J. Gender specific coronary artery diameters in CT coronary angiogram: A comparative study in female and male population. Indian J Cardiovasc Dis Women 2022;7:121-9.
Abstract
Objectives:
Women show significant in-hospital morbidity and mortality with greater extent of symptoms, poorer post-revascularization outcome with increased restenosis and repeat revascularization after angioplasty, than men. Smaller sized coronary arteries in females can be attributable for this differential outcome, which is also similar in case of Indians, compared to Caucasians. Our aim is to assess the gender-specific difference in coronary arteries using noninvasive Multidetector Computed-Tomography Coronary-Angiogram(CT-CAG) and comparing the same with other racial database.
Materials and Methods:
With Ethics committee approval, present retrospective comparative study conducted in 128CT-CAG scans in 18-45years aged 100 women and 89 men with no atherosclerotic burden excluding pathological coronaries and high calcium score>100. Diameter measurements of proximal (≤10mm) segments of right coronary artery(RCA), left main coronary artery(LMCA), left anterior descending(LAD) and circumflex(LCx) arteries were taken, averaged and compared using 2-sample z-test. Considering the obtained mean diameters of total sample as South-Indian dataset which is then compared with Caucasians dataset taken from previous study.
Results:
Women showed smaller coronary artery diameters compared to men in all the arteries, with greater gender-specific age-adjusted difference in LMCA, followed by LAD, RCA and least in LCX. South-Indians showed statistically significant smaller diameters of all the coronary arteries compared to Caucasians.
Conclusion:
Gender-specific difference among the coronary arteries does exist, with females having smaller dimensions; South-Indians also show smaller diameters. This warrants a clinician for gender-specific approaches during the interventions because of technical difficulties.
Keywords
Coronary artery diameters
CT-CAG
Gender difference
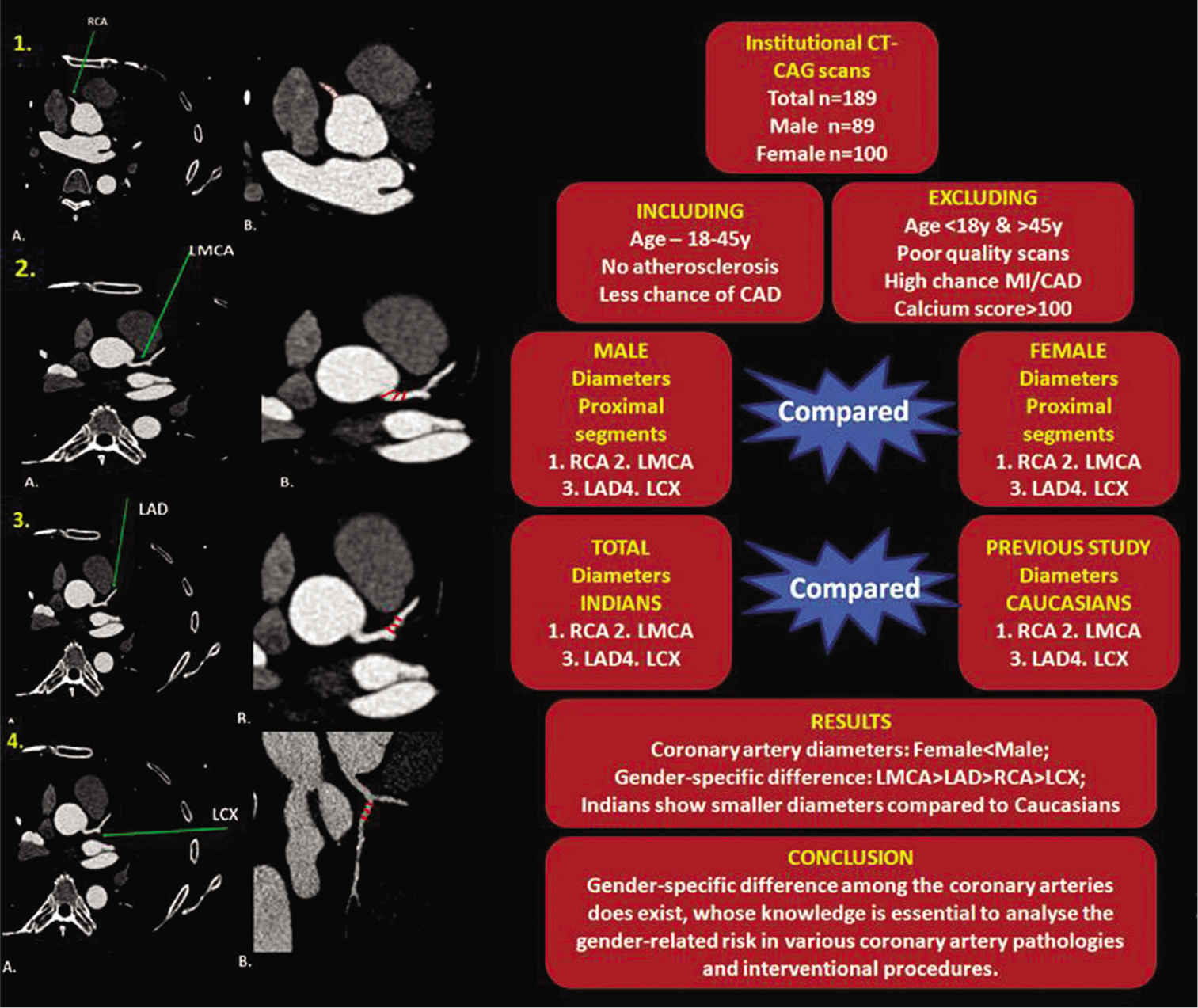
ABSTRACT IMAGE
INTRODUCTION
Despite significant breakthrough in the early diagnosis and optimal treatment in the medical field, cardiovascular disease is the foremost leading cause of morbidity and mortality among women and men worldwide with incidence of 4.1 for women and 6.4 for men per 1000 person-years.[1] Women show a greater extent of symptoms, poorer post-revascularization outcome, and more coronary vascular complications, than men. Smaller size of coronary arteries may be attributed for this gender specific outcome, although limited data exist to support this assumption.
It has been postulated that women are at high risk of restenosis and repeated revascularization after coronary angioplasty and also in-hospital morbidity and mortality with Coronary Artery Bypass Grafting (CABG) and Percutaneous Coronary Intervention (PCI) procedures.[2-4] The presentation may include higher bleeding rates, lower graft patency, more thrombotic events, and higher readmission rates. This gender-specific differential outcome is worse in case of females, which may be attributed for having smaller coronary arteries with more comorbidities at presentation and requiring more emergency surgeries.[5-10]
Quicker detection of at-risk patients is essential for earlier prophylaxis of coronary artery disease (CAD). The atherosclerotic plaques in the coronary arteries which are formed due to systemic vascular wall inflammation, endothelial dysfunction, and remodeling can result in partial or complete blood flow obstruction and thereby myocardial ischemia. Interestingly, these vessel wall changes are related to a reduced lumen of the coronary arteries, and the diameters of the targeted coronary arteries may be important to predict the CAD risk.[11-13] As a foremost diagnostic tool for low-risk suspected CAD cases, the prime strength of CCTA over functional tests is to effectively determine the anatomic atherosclerotic burden.[14]
It is assumed that coronary artery diameter is probably related to body habitus.[15,16] There is a proposal that Asians suffer excess mortality from CAD compared to Caucasians; this can be attributed to the smaller dimensions of coronaries in the former group. There are also added therapeutic complications regarding coronary intervention to the already known excess mortality risk from CAD itself.[17] According to some studies, the smaller size of coronary arteries is noted in most of the segments when compared to Caucasians (right coronary artery [RCA], left main coronary artery [LMCA], left anterior descending [LAD], and left circumflex [LCX]). Due to smaller body habitus, Indians show smaller dimensions of the coronary arteries. This is previously thought to be due to ethnic origin per se, but it has been cleared that the reason is body size alone. It may lead to therapeutic implication of technical difficulties during procedures such as bypass graft, stenting, atherectomy, and Percutaneous Transluminal Coronary Angioplasty.[18]
Hereby, one usual reason for added female gender related risk is that women have smaller coronary arteries than men. The aim of our study is to evaluate the coronary artery diameters in multidetector computed tomography coronary angiogram (CT-CAG), in both women and men, on an appropriate sample showing no atherosclerotic burden and without or less probable of CAD and hence considering them to be normal vessels. Moreover, as very little literature is available presently and that too especially in the female population, we extend our research in this field to evaluate and compare the same. In addition, we are also interested to see whether or not this proposed difference is comparable with that of the other existing racial database.
Aims and objectives
The objectives of the study are as follows:
To evaluate the gender-specific coronary artery diameters among women and men of 18–45 years age group in multidetector CT-CAG
To evaluate the gender difference in our study population and compare the same with that of the existing other ethnic and racial database.
MATERIALS AND METHODS
Study population
Ours was a retrospective comparative study conducted from June 2018 to June 2021 in the Department of Radiology and Imageology following approval of institutional scientific and ethical committee. All the CT-CAG datasets selected were within the age group of 18–45 years with coronary arteries showing no atheromatous changes (like calcified or non-calcified plaques), referred for screening computed tomography (CT) without or with low probability of CAD and diagnostic CT with calcium score below 100, likely to eliminate potential coronary arterial remodeling. After excluding the subjects with high probability of CAD or myocardial infarction and poor-quality imaging due to motion artifacts, a total of 189 cases (100 female and 89 male) were selected.
Imaging protocol of CT coronary angiogram
All the CT-CAG scans were done in supine position with breath holding at maximum inspiration from the level of carina to the hemidiaphragm using 128-slice MDCT (SOMATOM Definition AS+/SEIMENS) with scanning parameters of 120 kV and 560 mA, section thickness − 0.6 mm, rotation time – 300 ms, and prospective craniocaudal ECG gating. Care was taken for achieving a pre-scan heart rate of not >65 beats/minute with orally administered β-blocker 1 h before every scan. Intravenous Iohexol (Omnipaque™) usually administered depending on the patient’s body weight and total scanning time (approximately 350 mgI/ml at the rate of 5.5 mL/s), then followed by 45 ml saline flush using a dual-barrel power injector (MEDRAD SALIENT). All the images were subsequently reconstructed with slice thickness 0.6 mm, using medium soft-tissue convolution kernel (B26F), and 512 × 512 sized reconstruction matrix. Axial, cross-sectional, multiplanar reformation, curved reformation, 3D-maximum intensity projection, and 3D-volume rendered technique images were generated during the best diastolic phase (66% of the ECG cycle) that gives best image quality with least artifacts.
Data acquisition
Coronary artery diameters were calculated manually using axial cross-sectional data with thin-slab reconstruction and the window-level 300–400HU and window-width 800–1000HU. Bifurcating points of the coronary arteries were taken as landmarks. Measurements were taken at three arbitrary points in each of the main arteries – LMCA at the proximal-half portion before its bifurcation (into LAD and LCX) or trifurcation (into LAD, LCX, and ramus intermedius) preferably within proximal-most 10 mm (in cases of LMCA length >1 cm); LAD and LCX at three arbitrary points in the proximal-most 10 mm before giving off the first marginal or septal perforator branch – whichever the earlier in LAD; RCA at three arbitrary points in the proximal portion before first LV branch preferably within proximal 10 mm. All the three arbitrary measurements taken at equidistant points are shown in [Figures 1 and 2] were averaged and tabulated accordingly. Few of the confronted anatomical variants of coronary arterial system are shown in [Figure 3].
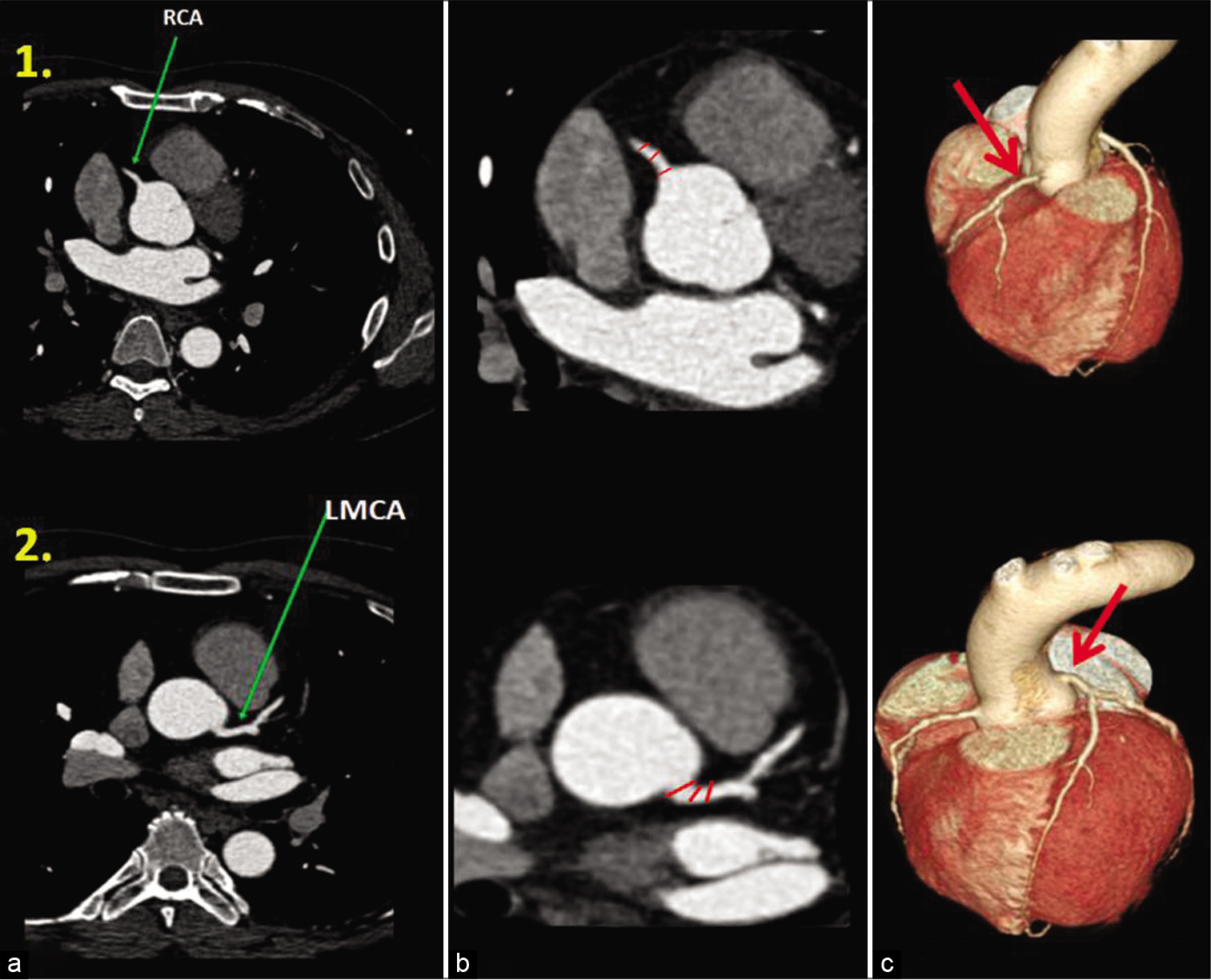
- Coronary artery diameter measurements. Axial CT-CAG (1a, 1b and 2a, 2b) and 3D volume rendered images (1c and 2c) show normal anatomy (green and red arrows) of the right coronary artery-RCA (panel 1) and left main artery-LMCA (panel 2). The coronary artery diameter measurements (red color marks in equidistant manner) were taken in the RCA (1b) within the 10 mm proximal segment and the LMCA (2b) 10 mm before bifurcation as shown in zoomed image (b). The three arbitrary measurements taken for each artery are then averaged for the final diameter of that particular coronary artery.
![Coronary artery diameter measurements (continued with [Figure 1]). Axial CT-CAG (3a, 3b and 4a), curved planar reformatted (4b) and (3d), and volume rendered images (3c and 4c) shows normal anatomy (green and red arrows) of the left anterior descending artery-LAD (panel 3) and left circumflex artery-LCX (panel 4). The coronary artery diameter measurements were taken in a similar way (i.e., within the proximal 10 mm segment after bifurcation from the LMCA) with equidistant points (red color lines) in the LAD as shown in (3b)-zoomed axial image, and the LCX as shown in curved planar reformatted image-4B. The three arbitrary measurements taken for each artery are then averaged for the final diameter of that particular coronary artery.](/content/148/2022/7/3/img/IJCDW-7-121-g002.png)
- Coronary artery diameter measurements (continued with [Figure 1]). Axial CT-CAG (3a, 3b and 4a), curved planar reformatted (4b) and (3d), and volume rendered images (3c and 4c) shows normal anatomy (green and red arrows) of the left anterior descending artery-LAD (panel 3) and left circumflex artery-LCX (panel 4). The coronary artery diameter measurements were taken in a similar way (i.e., within the proximal 10 mm segment after bifurcation from the LMCA) with equidistant points (red color lines) in the LAD as shown in (3b)-zoomed axial image, and the LCX as shown in curved planar reformatted image-4B. The three arbitrary measurements taken for each artery are then averaged for the final diameter of that particular coronary artery.
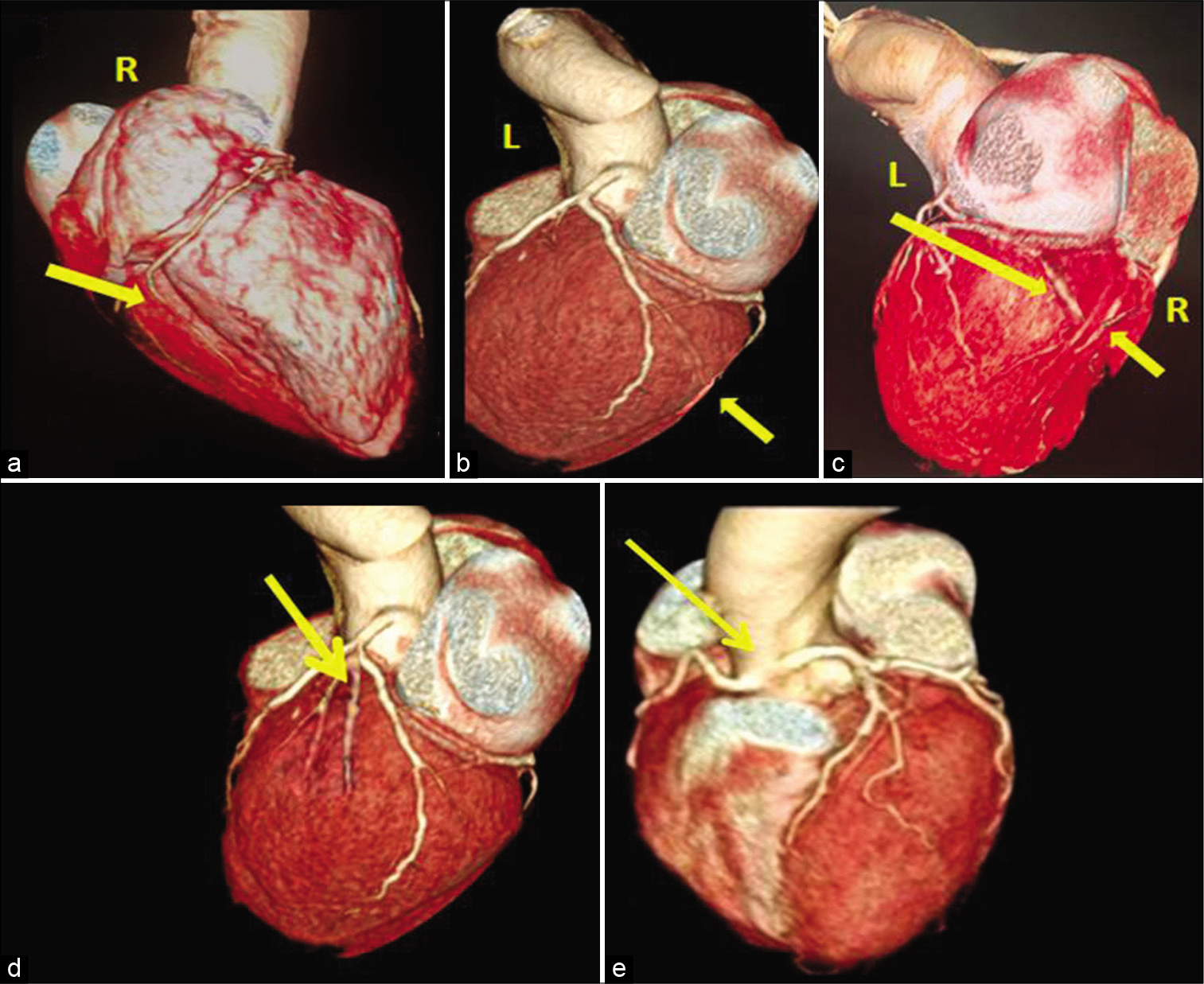
- Coronary artery dominance and variants. The artery that contributes to posterior and inferior supply is the dominant artery. 3D volume rendered images show RCA (a), LCX (b) giving off the posterior descending artery – PDA branch (yellow arrows), hence right and left dominant arteries. (c) Shows that PDA branch is contributed by both RCA and LCX (yellow arrows); hence, it is codominant circulation. 3D volume rendered images (d) shows trifurcation of LMCA into LAD, LCX, and ramus intermedius (yellow arrow), and image (e) shows anomalous common origin of LMCA from right coronary sinus (yellow arrow).
Statistical analysis
The results of continuous variables were noted down as mean±standard deviation. Gender difference of coronary arterial diameters was evaluated on MDCT by comparing them using 2-sample Z-test for 2-means. Calculations of subsequent P-value were performed for the comparison between the genders and also with the existed other ethnic and racial database.
OBSERVATION AND RESULTS
Clinical characteristics
We have done study in a cohort of 189 patients out of which 89 were males and 100 were females with mean age of 40.25 ± 5 years in females and 40 ± 5.7 years in males. Age range was 22–45 years in males and 18–45 years in females. Mean age of women with normal coronary arteries was almost similar to the men in this group as shown in [Figure 4].
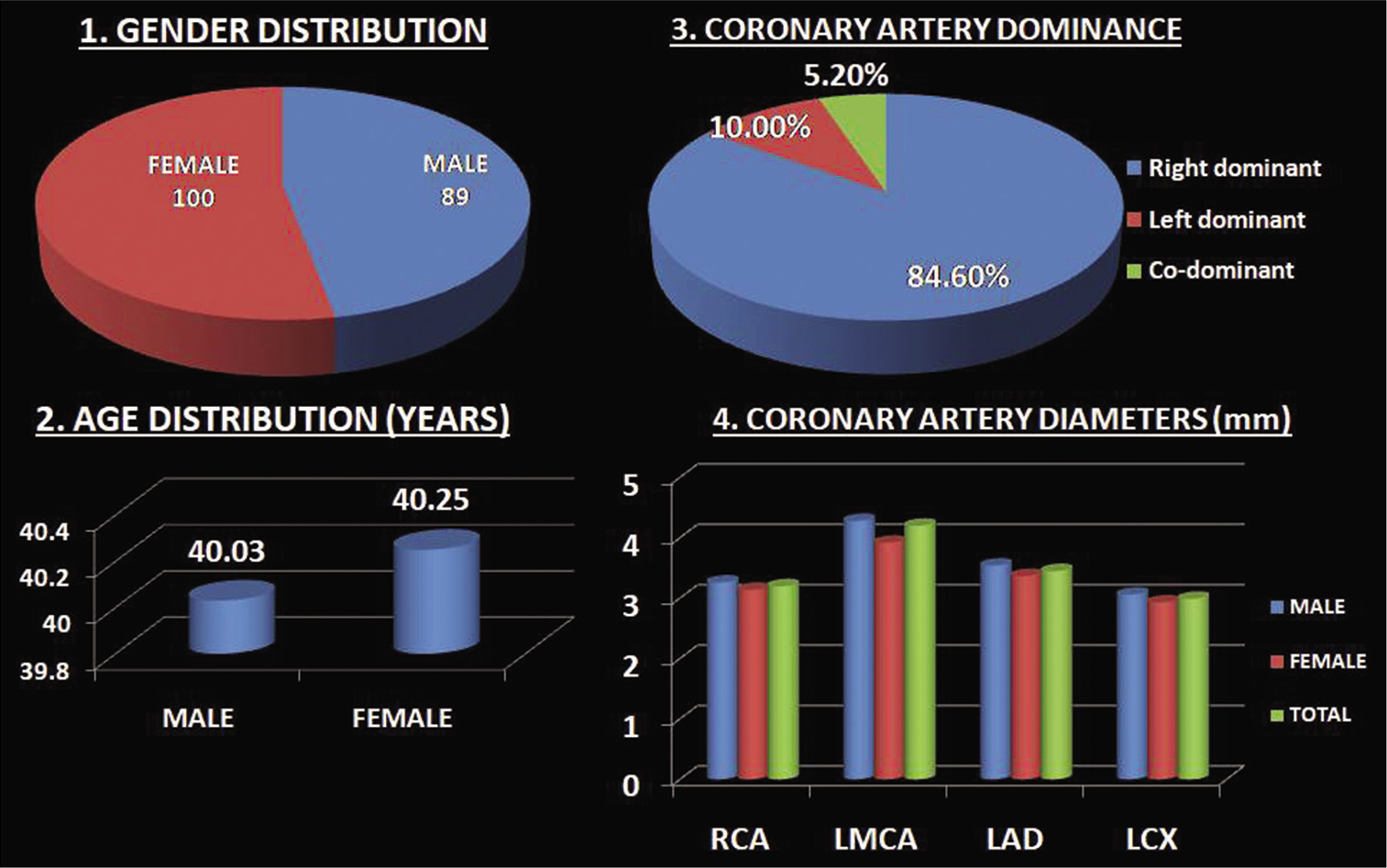
- Conglomerate of charts showing baseline characteristics of the study population. Pie-charts showing gender distribution (image 1) with females (n = 100) and males (n = 89) and coronary artery dominance (image 3) with the right dominance more than left and codominances. Bar-charts of age distribution(image 2) showing mean age of female population is almost similar to that of the males and coronary artery diameters of the study population (image 4) showing coronary artery diameters of males were higher than that of females, difference is higher in LMCA and least in LCX.
Coronary artery dominance
Dominance of the coronary circulation was assessed depending on the arteries that contribute to posterior descending artery (PDA) branch. The RCA gave PDA in 80.4% of the cases, hence, was dominant, left dominance seen in 12.6% and codominance in 6.8% [Figure 4]. Concurrently, a few coronary artery variants noted – common origin of RCA and LMCA, trifurcation of LMCA into LAD, LCX, and ramus intermedius, and anomalous course of LAD between aorta and pulmonary artery [Figure 3].
Coronary artery diameters
We first calculated calcium score by Agatson method to exclude all those datasets with score>100. Coronary artery diameters for the proximal segments of LMCA, LAD, RCA, and LCX are presented in [Table 1 and Figure 4]. The proximal segments of coronary arteries were larger in size in males compared to females. In our study, gender-specific difference among all the proximal coronary artery segments was higher in LMCA, followed by LAD, RCA and LCX in a descending order. When the diameters of these vessels in males and females were taken collectively, that is, averaged for the entire sample (n = 189), the LMCA was greatest in size followed by proximal LAD, proximal RCA, and proximal LCX, respectively, (4.2 ± 0.71 mm, 3.45 ± 0.57 mm, 3.20 ± 0.58 mm, and 2.99 ± 0.57 mm). Good statistical significance is seen in the comparison of the male and female population in our study.
| Proximal portion of coronary artery | Male n=89 | Female n=100 | P-value from Z-test | Statistical significance | TOTAL n=189 (Average of male and female) |
|---|---|---|---|---|---|
| RCA | 3.26±0.65 | 3.14±0.52 | <0.05 | ✓ | 3.2±0.58 |
| LMCA | 4.28±0.86 | 3.92±0.57 | <0.05 | ✓ | 4.2±0.71 |
| LAD | 3.54±0.57 | 3.37±0.55 | <0.05 | ✓ | 3.45±0.57 |
| LCX | 3.05±0.55 | 2.94±0.58 | <0.05 | ✓ | 2.99±0.57 |
The computed mean of the respective arterial diameters was shown as mean±standard deviation. Women have smaller diameters compared to men, which were statistically significant. In our study, the gender-specific difference among all the proximal segments of coronary arteries was greater in LMCA, followed by LAD, RCA, and LCX in a descending order. For total 189 cases, the mean diameters were averaged and tabulated in the last column. RCA: Right coronary artery, LMCA: Left main coronary artery, LAD: Left anterior descending artery, LCX: Left circumflex artery
The proximal vessel size in the present study was computed as an average for the diameters of male and female study population as shown in [Table 2]. This was taken as South Indian database, subsequently compared to other ethnic racial database which was done in the previous studies to find if there exists a significant difference between South Indians and Caucasians. We have taken the racial database from Lip et al.[17] study with 77 Caucasian study population and compared with our study as shown in [Table 2]. In our study which is compared to Caucasians, statistically significant difference existed between their proximal coronary diameters, unadjusted for body surface area (BSA), with Caucasian arteries being larger (P < 0.05).
| Proximal portion of Coronary artery | Present study (South-Indian) n=189 | Lip et al. study[16] (Caucasian) n = 77 | P-value from Z test | Statistical significance |
|---|---|---|---|---|
| RCA | 3.2±0.58 | 3.35±0.69 | <0.05 | ✓ |
| LMCA | 4.2±0.71 | 4.44±0.91 | <0.05 | ✓ |
| LAD | 3.45±0.57 | 5.53±0.69 | <0.05 | ✓ |
| LCX | 2.99±0.57 | 3.17±0.63 | <0.05 | ✓ |
The computed mean of the respective arterial diameters was shown as mean±standard deviation. Total 189 samples taken as South-Indian racial database have been compared with Lip et.al.[16] study on Caucasian database. Their comparison showed that there was statistical significance between the diameters of South-Indian and Caucasian population with South Indians showing smaller dimensions. RCA: Right coronary artery, LMCA: Left main coronary artery, LAD: Left anterior descending artery, LCX: Left circumflex artery
DISCUSSION
Out of 100 female and 89 male population, mean age of women with normal coronary arteries was almost similar to that of the men in this group with slightly higher range in females [Figure 4]. Assessment of coronary artery dominance was dependent on those arteries that supply the posterior and inferior wall of the left ventricle frequently by PDA or posterolateral artery. In our study, the RCA gave PDA branch in 80.4% of the cases, hence, was dominant, left dominance seen in 12.6% and codominance in 6.8%. This is in correlation with the previous study by Ramteke et al.[19] where right dominance seen in 78.5% (55/70), left dominance in 20% (14/70), and codominance in 1.4% (1/70). Few coronary artery variants noted were – (1) common origin of RCA and LMCA, (2) trifurcation of LMCA into LAD, LCX, and ramus intermedius, and (3) anomalous course of LAD between ascending aorta and main pulmonary artery [Figure 3]. Coronary dominance and anatomical variants have a necessary role to be known before planning cardiac surgeries like bypass graft placement.
In our study of comparing the coronary artery diameters on CTCAG between male and female population, we have noted that males had significant greater diameters than females statistically, unadjusted for individual BSA (P < 0.05). The present study is in line with the previous studies by O’Connor et al.[3] (who had done a prospective study on 1325 patients for CABG concluding that females having smaller coronary arteries and were related to more peri-operative mortality) and by Dhall et al.[20] on histomorphic analysis of human coronaries in 20– 40 years aged 25 male and 25 female autopsied heart specimens concluding the lesser coronary diameters of females.
In our study of gender influencing the coronary artery dimensions that included proximal segmental analysis, we noted that the female gender predispose to smaller coronary arteries in the proximal RCA, LMCA, LAD, and LCX. However, the difference is more in the dimension of proximal LMCA followed by LAD and RCA, and less effectively in LCX. This variability in the LCX could be partially ellucidated depending on the variability in coronary arterial dominance.[18] Giving an explanation of retrospective nature of our study, we have not included the patient demographic details such as height, weight, and BSA all the measurements were not adjusted to BSA, which may be a limitation.
Various associations such as lower rate of successful procedural outcome and increased rate of in-hospital major events with PCI and CABG were seen with smaller coronaries, proved in various previous studies.[2-4] Not only with the above procedures, women with smaller sized coronaries are at higher risk for CAD, at least after menopause.[11-13] Observing that women generally start with smaller coronary diameters and undergo greater changes in the lumen for the equal degree of atherosclerosis occurring in the male peers, with notable sex differences in the magnitude of the adverse effects and receiving inferior treatments for CAD, we strongly suggest more aggressive primary preventive strategies in females.[21,22]
To the best of our knowledge, only very few studies are available till date establishing normative sizes of coronary arteries without using intravascular catheters – Hiteshi et al.[22] and Mahadevappa et al.[23] Besides, the gender-related difference in proximal coronary segments may show a sequential influence on microvascular physiology. Using the noninvasive more readily available volumetric imaging, like CT-CAG, we, hence, aim to provide our work for the convenient ease of in vivo quantification of proximal coronary dimensions without intracoronary catheter manipulations or intracoronary drug usage like vasodilators (e.g., nitroglycerin). Moreover, with ECG-gated synchronized dual-source dual-energy cardiac CT scanners having multiple detectors that yield very nice morphological characteristics (like temporal resolution, contrast resolution), the virtual measurement of coronary arteries complying with heart-rate associated with a great (submillimetric) precision helps in follow up of the temporal evolution of various pathologies.[24]
Indians’ coronary artery dimensions were being described to be significantly smaller than that of the Western population. This can be attributed to the smaller body habitus, built, and BSA.[17,25] Lip et al.[17] conducted studies between Caucasians and Asians by means of angiography, and finally concluded that the unadjusted mean coronary arterial diameters in the Caucasians were more than those of the Asians, but, not much difference noted when the same values were calculated per unit BSA. Hence, the smaller coronary artery sizes in the Asians may be accredited to their smaller BSA is their final conclusion. Similar conclusion had been drawn by Dhawan and Bray[25] who compared the cross-sectional areas of coronary arteries.
In our present study, the proximal coronary artery diameters of our South Indian study population and unadjusted for individual BSA when compared to those of Caucasians[16] showed that Caucasians have greater coronary dimensions than South Indians. Lip et al.[17] studied the same angiographically on 77 Caucasians and 39 Indians (mean age > 50 years) and found that Indo-Asians had smaller coronary artery sizes showing a significant difference in the mean diameters of the LMCA, LAD, and RCA statistically, and if adjusted to BSA, no such difference noted. Raut et al.,[18] studied over 229 patients with coronary angiography and found that Indians showed lesser diameters than Caucasians, which is not seen when adjusted to BSA. Our study was in concordance with the previous studies with Indians showing lesser diameters, though the comparison was not done with BSA adjusted measurements, which may be a limitation [Figure 5].
Limitations
As per the inclusion criteria, though our study cohort consisted of younger aged patients with no demonstrable CAD with zero calcium score, it is always possible to have early stage or subclinical CAD, as it may be missed in few cases unknowingly.
Comorbidities such as diabetes and hypertension may lead to subclinical or earlier setting of atherosclerosis causing vessel wall remodeling; which might have altered our study.
Furthermore, we did not taken into account some of the clinical details, because of retrospective study pattern, like BSA, usage of vasodilator medication, which might have modified the distribution and variability of coronary artery sizes.
The contrast agent itself may cause vasodilatation;[26] however, it is minimized with the use of nonionic monomeric contrast agent (Iohexol) and we expect that both the genders were equally affected, and this should not modify the study outcome.
CONCLUSION
Gender-specific difference among the coronary arteries does exist, for LMCA, LAD, RCA, and LCX in the descending order with females having smaller dimensions, whose knowledge is essential for a clinician to analyze the gender-related risk in various coronary artery pathologies and may encourage gender-specific approaches for interventions.
Audio summary available at
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Heart disease and stroke statistics-2016 update: A report from the American heart association. Circulation. 2016;133:447-54.
- [CrossRef] [PubMed] [Google Scholar]
- Gender-related differences in coronary artery dimensions: A volumetric analysis. Clin Cardiol. 2010;33:E44-9.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of coronary artery diameter in patients undergoing coronary bypass surgery: Northern New England cardiovascular disease study group. Circulation. 1996;93:652-5.
- [CrossRef] [PubMed] [Google Scholar]
- Implications of small reference vessel diameter in patients undergoing percutaneous coronary revascularization. J Am Coll Cardiol. 1999;34:40-8.
- [CrossRef] [Google Scholar]
- The influence of gender in patients undergoing coronary artery bypass graft surgery: An eight-year prospective hospitalized cohort study. J Am Coll Surg. 2003;196:428-34.
- [CrossRef] [Google Scholar]
- Sex differences in hospital mortality after coronary artery bypass surgery: Evidence for a higher mortality in younger women. Circulation. 2002;105:1176-81.
- [CrossRef] [PubMed] [Google Scholar]
- Gender differences in coronary heart disease. Neth Heart J. 2010;18:598-603.
- [CrossRef] [PubMed] [Google Scholar]
- Role of target vessel size and body surface area on outcomes after percutaneous coronary interventions in women. Am Heart J. 2002;144:297-302.
- [CrossRef] [PubMed] [Google Scholar]
- Gender differences in outcomes after hospital discharge from coronary artery bypass grafting. Circulation. 2006;113:507-16.
- [CrossRef] [PubMed] [Google Scholar]
- Gender and restenosis after coronary artery stenting. Eur Heart J. 2003;24:1523-30.
- [CrossRef] [Google Scholar]
- Endothelial function predicts progression of carotid intima-media thickness. Circulation. 2009;119:1005-12.
- [CrossRef] [PubMed] [Google Scholar]
- Endothelial dysfunction and coronary artery disease: A state of the art review. Cardiol Rev. 2015;23:119-29.
- [CrossRef] [PubMed] [Google Scholar]
- Large-artery stiffness, hypertension and cardiovascular risk in older patients. Nat Clin Pract Cardiovasc Med. 2005;2:450-5.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac CT angiography in current practice: An American society for preventive cardiology clinical practice statement. Am J Prev Cardiol. 2022;9:100318.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of gender on vessel size in patients with angiographically normal coronary arteries. J Interv Cardiol. 2006;19:340-4.
- [CrossRef] [PubMed] [Google Scholar]
- Gender differences in coronary artery size per 100 g of left ventricular mass in a population without cardiac disease. Swiss Med Wkly. 2001;131:610-5.
- [Google Scholar]
- Do Indo-Asians have smaller coronary arteries? Postgrad Med J. 1999;75:463-6.
- [CrossRef] [PubMed] [Google Scholar]
- Coronary artery dimensions in normal Indians. Indian Heart J. 2017;69:512-4.
- [CrossRef] [PubMed] [Google Scholar]
- A study of coronary dominance pattern in central India population. Indian J Clin Anat Physiol. 2017;4:529-31.
- [Google Scholar]
- Histomorphometric analysis of coronary arteries: Sexual dimorphism. J Anat Soc India. 2003;52:144-6.
- [Google Scholar]
- Sex and gender matter in cardiovascular disease and beyond. Heart. 2022;108:994-5.
- [CrossRef] [PubMed] [Google Scholar]
- Gender differences in coronary artery diameter are not related to body habitus or left ventricular mass: Gender differences in coronary diameter. Clin Cardiol. 2014;37:605-9.
- [CrossRef] [PubMed] [Google Scholar]
- Normal proximal coronary artery diameters in adults from India as assessed by computed tomography angiography. J Clin Diagn Res. 2016;10:TC10-3.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac CT angiography: normal and pathological anatomical features-a narrative review. Cardiovasc Diagn Ther. 2020;10:1918-45.
- [CrossRef] [PubMed] [Google Scholar]
- Are Asian coronary arteries smaller than Caucasian? A study on angiographic coronary artery size estimation during life. Int J Cardiol. 1995;49:267-9.
- [CrossRef] [Google Scholar]
- Vasomotor effects of iodinated contrast media: Just side effects? Curr Vasc Pharmacol. 2003;1:321-8.
- [CrossRef] [PubMed] [Google Scholar]







