Translate this page into:
Gender-based Differences in Young Indian Patients with Acute Coronary Syndrome: A Comprehensive Analysis
*Corresponding author: Ajinkya Vijay Mahorkar, Department of Cardiology, Avanti Institute of Cardiology, Nagpur, Maharashtra, India. ajinkyamahorkar1@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mahorkar V, Mahorkar U, Vidhale A, Mahorkar AV, Sarwale SJ, Dhundele T, et al. Gender-based Differences in Young Indian Patients with Acute Coronary Syndrome: A Comprehensive Analysis. Indian J Cardiovasc Dis Women. doi: 10.25259/IJCDW_43_2024
Abstract
Objectives:
The steep rise in acute coronary syndrome (ACS) cases among young adults, particularly those ≤ 45 years old, poses a significant concern, especially in India. This study delved into the baseline characteristics, risk factors, and echocardiographic and angiographic profiles of ACS patients under 45 years of age, with a focus on discerning gender-based differences.
Materials and Methods:
A retrospective, observational cohort study was conducted, including young adults aged 18–≤45 years diagnosed with ACS who underwent coronary angiography. Demographic, clinical, and angiographic data were meticulously analyzed.
Results:
Our study of 550 young ACS patients (mean age: 40.2 ± 4.7 years) from January 2018 to July 2023 found that females, forming nearly 10% of the cohort, had a higher obesity prevalence (38.7% vs. 56.9%, P = 0.012). Multivessel disease was less common in females (P < 0.0001). Left anterior descending (67.3%) and right coronary (41.3%) arteries predominantly affected, seen in significantly higher proportion of males (P = 0.003 and P = 0.011, respectively). Left ventricular ejection fraction ≤40% was notably lower in males (P = 0.029). Percutaneous coronary intervention (PCI) was the primary treatment modality (59.3%), with significantly lower rates among females (43.1% vs. 60.9%, P = 0.040).
Conclusion:
Despite the increasing prevalence, research on gender differences in young adults with ACS is limited, especially in the Indian population. We observed higher obesity rates in females compared to males, along with lower rates of multivessel disease in females. Males had lower ejection fractions and underwent PCI more often than females. These findings highlight the need for gender-specific approaches and tailored interventions in ACS management.
Keywords
Acute coronary syndrome
Young
Gender
India
ABSTRACT IMAGE
INTRODUCTION
Acute coronary syndrome (ACS), a pressing global health issue, has seen a notable uptick in prevalence, especially among young adults in South Asian countries like India. In fact, a significant portion of coronary artery disease cases in India occurs in individuals under 45 years of age, with nearly a quarter of anterior myocardial infarction cases happening in those under 40.[1] Despite this surge, there is a glaring lack of gender-based disparity studies within this demographic. Global studies and registries report a 7–10.3% prevalence of ST-elevation myocardial infarction in young adults, depending on age cut-offs, and highlight gender-based differences in outcomes.[2] While research elsewhere has shed light on gender differences in ACS, such investigations are notably absent in India, where unique sociocultural, genetic, and environmental factors may influence cardiovascular health differently. A recent study in the US population revealed gender disparities in ACS patients, underlining the urgency of investigating such phenomena in specific populations.[3] Addressing this gap, our study aims to thoroughly analyze clinico-demographic factors and coronary angiography (CAG) profiles among young ACS patients (<45 years) in India, with a keen focus on potential gender differences. By uncovering nuanced differences in ACS presentation and outcomes among males and females, this research endeavors to inform tailored interventions aimed at mitigating the burden of cardiovascular disease in the Indian population.
MATERIALS AND METHODS
This single-center retrospective study was conducted at a tertiary care cardiology center in Central India. The data collection was started after approval from the local institutional ethics committee, i.e., Criticare hospital and research institute – EC/CHRI/24/65 on July 22, 2024. The study was conducted following ethical principles of the Declaration of Helsinki, good clinical practice guidelines, and applicable local regulations.
CAG and 2D-echocardiography (2D-ECHO) were performed by trained cardiologists following hospital protocols. Angiographic measurements were made by visual estimation by two cardiologists. A diameter stenosis of 50% in coronary segment was considered significant.
We reviewed medical records of 550 young adults (18–≤45 years) diagnosed with ACS between January 2018 and July 2023. Information on demographics, comorbidities, addiction history, laboratory parameters, 2D-ECHO, and CAG findings was recorded in Microsoft Excel.
Clinical follow-up data were collected through clinic visits or telephonic interviews. No routine angiographic follow-up was conducted. ACS was defined by typical clinical symptoms, relevant electrocardiographic changes, and/or elevated troponin T or troponin I. All deaths were considered cardiac in origin unless a clear non-cardiac cause could be established. All patients had at least a 1-year follow-up unless they died within that year. For deceased patients, next of kin were interviewed and death certificates reviewed.
Analysis was performed using Microsoft Excel. We reported frequencies, proportions, and measures of central tendency for categorical and continuous variables, respectively. We used the Chi-square test for categorical data and either a student t-test or Mann–Whitney U-test for continuous data based on the data distribution. Significance for all comparisons was set at 5% (i.e., P < 0.05).
RESULTS
Baseline characteristics
The study population’s baseline characteristics are summarized in Table 1. The mean age was 40.2 ± 4.7 years, with 59.3% aged above 40 years. Around 10% of females developed ACS. Obesity, hypertension, and diabetes were prevalent in 40.4%, 38.7%, and 30.4% of patients, respectively. Gender-wise analysis showed no age distribution difference (P = 0.202). Obesity was significantly higher in females (38.7% vs. 56.9%, P = 0.012). Serum triglycerides showed non-significantly higher median values in males (P = 0.252), while serum creatinine was significantly higher (P < 0.001) in males. On 2D-ECHO, males had significantly lower mean left ventricular ejection fraction (LVEF) than females (48.4 ± 11.1% vs. 52.0 ± 10.3%, P = 0.029). While LVEF categories did not significantly differ between genders (P = 0.076), more males had LVEF ≤40% (30.3% vs. 15.7%). Males also showed significantly higher regional wall motion abnormality (RWMA) rates (P = 0.026).
| Baseline characteristics | Total (n=550) | Male (n=499) | Female (n=51) | P |
|---|---|---|---|---|
| Age (years) | 40.2±4.7 | 40.1±4.8 | 41.3±3.2 | 0.080 |
| 18–30 | 25 (4.5) | 25 (5.0) | 0 | 0.202 |
| 31–40 | 199 (36.2) | 182 (36.5) | 17 (33.3) | |
| 41–45 | 326 (59.3) | 292 (58.5) | 34 (66.7) | |
| Co-morbidities | ||||
| Obesity | 222 (40.4) | 193 (38.7) | 29 (56.9) | 0.012 |
| Hypertension | 213 (38.7) | 190 (38.1) | 23 (45.1) | 0.327 |
| Diabetes mellitus | 167 (30.4) | 150 (30.1) | 17 (33.3) | 0.628 |
| Stressful work | 14 (2.5) | 13 (2.6) | 1 (2.0) | 0.781 |
| Addictions | ||||
| Tobacco Only | 12 (2.2) | 12 (2.4) | 0 | 0.250 |
| Smoking and Tobacco both | 59 (10.7) | 56 (11.2) | 3 (5.9) | |
| Alcohol | 59 (10.7) | 55 (11.0) | 4 (7.8) | 0.485 |
| Laboratory parameters | ||||
| Total cholesterol (n=221) (mg/dL) | 164.0 (138–194.5) | 165 (138–195) | 156 (126.5–199.0) | 0.717 |
| LDL-C (n=212) (mg/dL) | 98 (72.5–122.2) | 98.6 (71.8–122.4) | 89.6 (74.4–121.8) | 0.764 |
| Serum Triglyceride (n=195) (mg/dL) | 134 (95–197) | 134 (96–197) | 101 (58–157) | 0.252 |
| Serum Creatinine (n=477) (mg/dL) | 1.0 (0.86–1.15) | 1.02 (0.89–1.16) | 0.78 (0.68–0.89) | <0.001 |
| Left ventricular ejection fraction | 48.7±11.1 | 48.4±11.1 | 52.0±10.3 | 0.029 |
| ≤40% | 159 (28.9) | 151 (30.3) | 8 (15.7) | 0.076 |
| 41–50% | 161 (29.3) | 145 (29.1) | 16 (31.4) | |
| >50% | 230 (41.8) | 203 (40.7) | 27 (52.9) | |
| Regional wall motion abnormality | ||||
| Absent | 221 (40.2) | 192 (38.5) | 29 (56.9) | 0.026 |
| Anterior | 169 (30.7) | 159 (31.9) | 10 (19.6) | |
| Inferior | 117 (21.3) | 110 (22.0) | 7 (13.7) | |
| Anterior+inferior | 23 (4.2) | 22 (4.4) | 1 (2.0) | |
| Other | 20 (3.6) | 16 (3.2) | 4 (7.8) |
LDL-C: Low-density lipoprotein cholesterol
Coronary angiographic findings and treatment
Table 2 illustrates coronary angiographic findings and treatments. Single vessel disease (SVD) was most common, followed by double vessel disease (DVD) and triple vessel disease (TVD). Males had higher rates of DVD (26.7% vs. 17.6%) and TVD (18.2% vs. 7.8%) (P < 0.0001). Left anterior descending artery involvement was significantly higher in males (69.3% vs. 47.1%, P = 0.011). Medical management was more common in females, while males predominantly underwent PCI (P = 0.040).
| Parameters | Total (n=550) (%) | Male (n=499) | Female (n=51) | P |
|---|---|---|---|---|
| No. of vessels involved | ||||
| Single vessel disease | 271 (49.1) | 248 (49.7) | 23 (45.1) | <0.0001 |
| Double vessel disease | 142 (25.7) | 133 (26.7) | 9 (17.6) | |
| Triple vessel disease | 95 (17.2) | 91 (18.2) | 9 (7.8) | |
| Normal coronaries | 42 (7.6) | 27 (5.4) | 15 (29.4) | |
| Major vessels involved | ||||
| Left anterior descending artery | 370 (67.3) | 346 (69.3) | 24 (47.1) | 0.011 |
| Right coronary artery | 227 (41.3) | 216 (43.3) | 11 (21.6) | 0.003 |
| Left circumflex artery | 169 (30.7) | 157 (31.5) | 12 (23.5) | 0.242 |
| Obtuse marginal artery | 99 (18.0) | 95 (19.0) | 4 (7.8) | 0.047 |
| Diagonal artery | 86 (15.6) | 78 (15.6) | 8 (15.7) | 0.992 |
| Left main artery | 79 (14.4) | 71 (14.2) | 8 (15.7) | 0.777 |
| Ramus artery | 75 (13.6) | 71 (14.2) | 4 (7.8) | 0.206 |
| Treatments | ||||
| Medical management | 213 (38.7) | 186 (37.3) | 27 (52.9) | 0.040 |
| PCI | 326 (59.3) | 304 (60.9) | 22 (43.1) | |
| CABG | 11 (2.0) | 9 (1.8) | 2 (3.9) |
PCI: Percutaneous coronary intervention, CABG: Coronary artery bypass grafting
Distribution of vessel involvement by age
Figure 1a provides the distribution of vessel involvement identified on CAG by the patient’s age. In age group 18– 30 years, SVD and DVD were present in 96% and 4% of patients, respectively. In 31–40-year age group, SVD (53.8%) was most common followed by DVD (22.2%), and TVD (13.6%) while 10.6% had normal coronaries. In age 41–45 years, SVD, DVD, and TVD were seen in 42.9%, 29.8%, and 20.9% of patients, respectively. Figure 1b demonstrated vessel involvement by age in males. As seen from the distribution of proportions, it was statistically significant (P < 0.0001) with DVD and TVD occurring at a greater frequency in above 30-year age groups. Among males, SVD (96%) was most common in 18–30-year age. In males above 40 years, 31.5% had DVD and 22.3% had TVD. Figure 1c shows the same in females. None of the female below 30 years of age had ACS. In 31–40-year age females, SVD, DVD, and TVD were seen in 29.4%, 23.5%, and 5.9%, respectively. Similarly, in 41–45 years of females, these were seen in 52.9%, 14.7%, and 8.8%, respectively, with no statistically significant differences (P = 0.359).
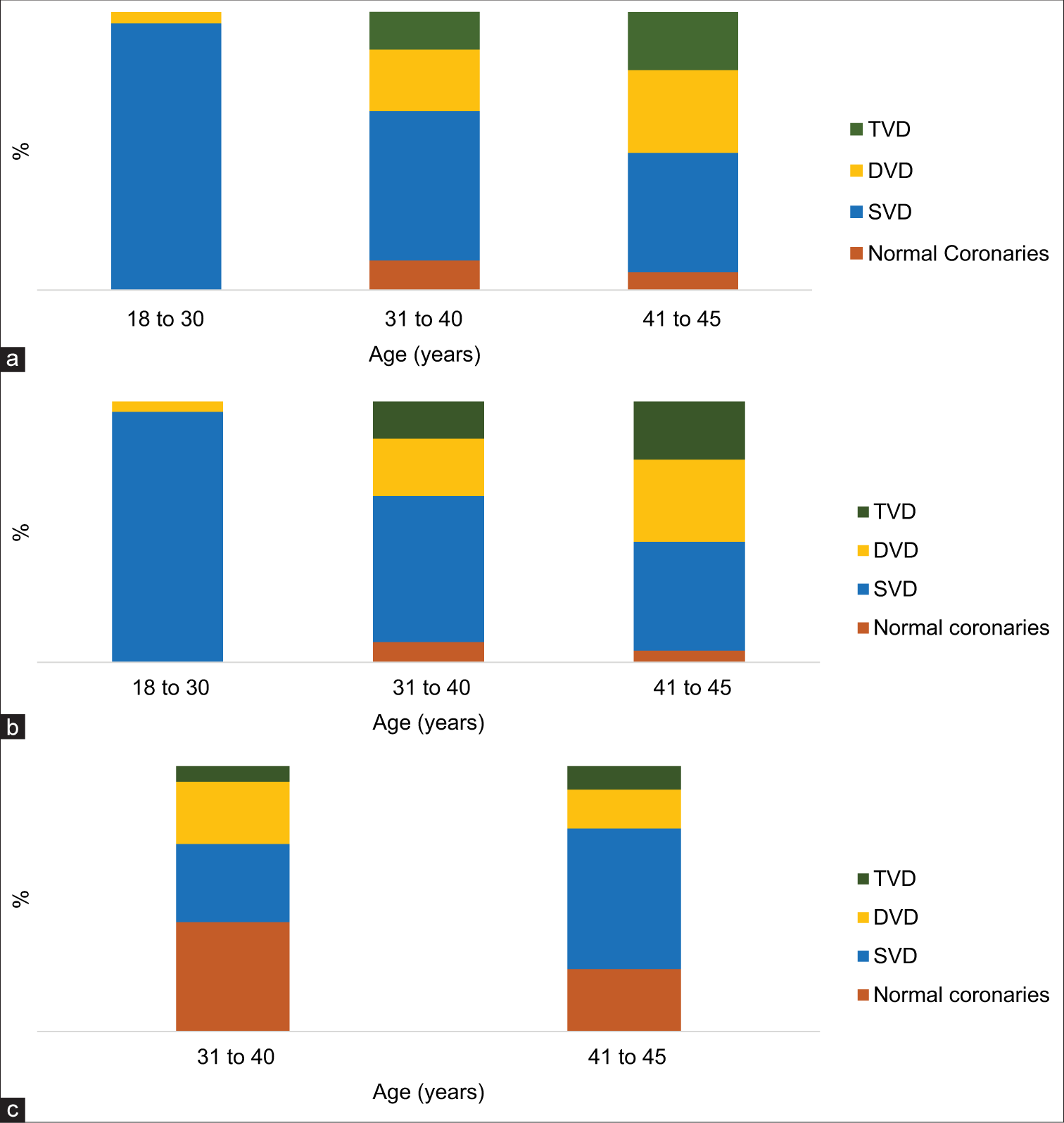
- Distribution of vessel involvement by patient age. (a) Total sample, (b) Males, (c) Females. (a) The Y-axis represents the percentage (%) of the total sample size (males + females combined). (b) The Y-axis represents the percentage (%) of the total number of males in the study. (c) The Y-axis represents the percentage (%) of the total number of females in the study.
Major cardiovascular outcomes
With a telephonic follow-up, 497 patients responded. Each of the patient was inquired for the major cardiovascular events (MACE), hospitalizations, revascularization, and mortality. Within 1 year of ACS diagnosis, mortality occurred in six (1.2%) patients. Among the six cases [Table 3], five were males, above the age of 40 years, and three were diabetic. On CAG, SVD, DVD, and TVD were noted in 3, 2, and 1 patient, respectively. Two cases had undergone PCI.
| Parameters | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 |
|---|---|---|---|---|---|---|
| Age | 45 | 45 | 34 | 41 | 45 | 45 |
| Gender | F | M | M | M | M | M |
| Diabetes | Yes | No | No | Yes | Yes | No |
| LVEF | 50 | 45 | 55 | 60 | 60 | 40 |
| CAG Profile | DVD | DVD | SVD | TVD | SVD | SVD |
| PCI | No | Yes | No | No | Yes | No |
LVEF: Left ventricular ejection fraction, CAG: Coronary angiography, PCI: Percutaneous coronary intervention, SVD: Single vessel disease, TVD: Triple vessel disease, DVD: Double vessel disease
DISCUSSION
ACS poses a significant global health challenge with varied impacts across demographics. Our discussion compares our study’s findings with existing literature, focusing on gender differences in young Indian ACS patients. We explored patients up to 45 years old, with a mean age of 40.2 years. Traditional risk factors such as obesity, hypertension, and diabetes mellitus were prevalent, aligning with earlier Indian studies.[4] However, our study showed higher diabetes mellitus prevalence compared to some Western populations.[5] Notably, obesity was significantly more prevalent among females, emphasizing the need for gender-specific risk assessment and management strategies.[6] Metabolic factors, such as obesity, diabetes, and hypertension, play a significant role in cardiovascular disease, as highlighted by the coronary artery disease in the young registry from India.[7] Higher obesity rates in Indian females may stem from cultural norms that restrict physical activity for women, especially in urban areas, combined with diets high in carbohydrates and low in balanced nutrients. In addition, the higher prevalence of polycystic ovary syndrome (PCOS) among young Indian females, a condition linked to obesity and insulin resistance, contributes to this trend. In our study, approximately 10% of young women were diagnosed with ACS, consistent with rates in Indian studies 9.86–12.9%,[8,9] but lower than in the West 15.8–26%,[10,11] likely due to differing lifestyle factors. Single-vessel disease prevailed in nearly 50% of young adults with ACS, similar across genders as in other Indian studies,[12,13] also aligning with findings in older adults. We also observed exclusively SVD in individuals aged 18–30, with a progressive increase in multivessel disease prevalence beyond the age of 30 in both genders. Notably, a higher proportion of females exhibited normal coronary arteries, indicating potential non-atheromatous ACS. Males had a lower mean LVEF than females, with 30.3% having LVEF ≤40% compared to 15.7% of females. Indian males tend to have lower LVEF due to higher rates of smoking, hypertension, and diabetes, along with genetic factors such as insulin resistance and central obesity, which accelerate atherosclerosis. These factors contribute to early vascular aging, leading to reduced LVEF at younger ages compared to males in Western populations. Western men with ACS often show better LVEF due to proactive hypertension management and lifestyle differences. In addition, 40.2% of patients showed no RWMA on ECHO, with females notably more absent of RWMA than males, highlighting potential gender-related differences.
In ACS treatment, options include medical management or procedures like percutaneous coronary intervention (PCI) or coronary artery bypass grafting. Our study found around 60% opting for PCI, influenced by factors like financial constraints, especially in India. Studies from Kuwait and Spain reported PCI rates from 32% to 52%.[14,15] indicating regional treatment differences. While our findings align with some Western studies on gender disparities in ACS, differences exist, with Western populations having higher lifestyle-related risk factors.[16] Indian patients may have a distinct risk profile, influenced by metabolic syndrome and cultural factors affecting healthcare-seeking behavior.[17,18]
Although young adults with ACS comparatively have lower rates of MACE than older adults,[11,19] the risk persists for the worse outcomes. Readmission and recurrent cardiovascular events are reported in young ACS as well. Smoking, diabetes, hypertension, no use of stents, and lower LVEF are identified as important predictors of such events.[14,20] Mortality rate is lower as seen in our study. Studies from Kenya (1.5%) and Saudi Arabia (0.9%)[21] reported similar mortality rates. Over nearly 9-year follow-up, a study in Israeli young ACS patients observed mortality rate of 9.1%.[20,22] Thus, identification of possible factors that contribute to MACE outcomes is essential in young ACS patients.
The observed gender differences in young ACS patients may stem from complex interactions among hormonal, genetic, and lifestyle factors. Higher ACS prevalence in young Indian males is influenced by genetic predispositions for early-onset atherosclerosis and a greater frequency of lifestyle risk factors such as smoking and alcohol use and pro-inflammatory state which accelerate cardiovascular aging. In contrast, the protective effects of estrogen in females delay atherosclerosis onset, offering relative protection against early cardiovascular events compared to males. Highlighting these gender-specific findings could lead to tailored ACS management strategies in India, with a focus on targeted prevention for young males, i.e., smoking cessation programs and early screening for hypertension and on the other hand, metabolic health interventions such as PCOS and obesity for females, ultimately enhancing outcomes in resource-limited settings.
Our study has limitations, primarily due to its retrospective nature, which inherently entails design constraints. Other limitations include a smaller sample size compared to Western studies, the potential influence of confounding variables, and possible bias in follow-up. Long-term prospective follow-up to document major cardiovascular outcomes like heart failure or recurrent ACS, finding gender specific risk factors including emotional behaviors which could offer valuable clinical insights into young ACS.
CONCLUSION
In summary, our study highlights significant gender differences in young Indian ACS patients, mirroring but also differing from Western populations. In our study of ACS in young Indians, most patients were over 40 years old. Notably, females showed higher rates of obesity and received PCI less often, with no female patients presenting with ACS below 30 years of age. Males, on the other hand, showed a significantly higher prevalence of multivessel disease and lower LVEF. These findings highlight important gender-based disparities in the presentation and management of young ACS patients, underscoring the need for tailored strategies in clinical practice.
Ethical approval
The data collection was started after approval from the local institutional ethics committee, i.e., Criticare hospital and research institute – EC/CHRI/24/65 on July 22, 2024.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Audio summary available at:
Financial support and sponsorship
Nil.
References
- Premature Coronary Artery Disease in Indians and Its Associated Risk Factors. Vasc Health Risk Manag. 2005;1:217-25.
- [Google Scholar]
- Age and Gender Differences in Quality of Care and Outcomes for Patients with ST-segment Elevation Myocardial Infarction. Am J Med. 2012;125:1000-9.
- [CrossRef] [PubMed] [Google Scholar]
- Sex Disparities in Management and Outcomes Among Patients with Acute Coronary Syndrome. JAMA Netw Open. 2023;6:e2338707.
- [CrossRef] [PubMed] [Google Scholar]
- Risk Factors and Angiographic Profile in Young Individuals with Acute ST-Elevation Myocardial Infarction (STEMI) Indian J Clin Cardiol. 2023;4:242-7.
- [CrossRef] [Google Scholar]
- Traditional Risk Factors and Premature Acute Coronary Syndromes in South Eastern Europe: A Multinational Cohort Study. Lancet Reg Health Eur. 2024;38:100824.
- [CrossRef] [PubMed] [Google Scholar]
- Premature Coronary Artery Disease in India: Coronary Artery Disease in the Young (CADY) Registry. Indian Heart J. 2017;69:211-6.
- [CrossRef] [PubMed] [Google Scholar]
- Study of Lipid Profile in Young Patients (age 40 Years or Below) with Acute Coronary Syndrome. J Family Med Prim Care. 2022;11:3034-9.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical Characteristics and Cardiovascular Outcomes among Young Patients with Acute Myocardial Infarction in Kerala, India: A Secondary Analysis of ACS QUIK Trial. Atheroscler Plus. 2022;50:25-31.
- [CrossRef] [PubMed] [Google Scholar]
- Acute Coronary Syndrome: The Risk to Young Women. J Am Heart Assoc. 2017;6:e007519.
- [CrossRef] [PubMed] [Google Scholar]
- Acute Coronary Syndromes in Young Patients: Phenotypes, Causes and Clinical Outcomes Following Percutaneous Coronary Interventions. Int J Cardiol. 2022;350:1-8.
- [CrossRef] [PubMed] [Google Scholar]
- Myocardial Infarction in Young Adults-risk Factors and Pattern of Coronary Artery Involvement. Niger Med J. 2014;55:44-7.
- [CrossRef] [PubMed] [Google Scholar]
- Demographic and Angiographic Profile in Premature Cases of Acute Coronary Syndrome: Analysis of 820 Young Patients from South India. Cardiovasc Diagn Ther. 2016;6:193-8.
- [CrossRef] [PubMed] [Google Scholar]
- Acute Coronary Syndrome in the Young: Clinical Characteristics, Risk Factors and Prognosis. Open Cardiovasc Med J. 2014;8:61-7.
- [CrossRef] [PubMed] [Google Scholar]
- Coronary Artery Disease in Patients Aged 35 or less-A Different Beast? Heart Views. 2011;12:7-11.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of Potentially Modifiable Risk Factors Associated with Myocardial Infarction in 52 Countries (the INTERHEART Study): Case-control Study. Lancet. 2004;364:937-52.
- [CrossRef] [PubMed] [Google Scholar]
- Metabolic Risk Factors in First Acute Coronary Syndrome (MERIFACS) Study. Indian Heart J. 2022;74:275-81.
- [CrossRef] [PubMed] [Google Scholar]
- Race and Ethnicity Considerations in Patients with Coronary Artery Disease and Stroke: JACC Focus Seminar 3/9. J Am Coll Cardiol. 2021;78:2483-92.
- [CrossRef] [PubMed] [Google Scholar]
- Acute Coronary Syndromes in Young Patients: Presentation, Treatment and Outcome. Int J Cardiol. 2011;148:300-4.
- [CrossRef] [PubMed] [Google Scholar]
- Long-Term Prognosis in Young Patients with Acute Coronary Syndrome Treated with Percutaneous Coronary Intervention. Vasc Health Risk Manag. 2021;17:153-9.
- [CrossRef] [PubMed] [Google Scholar]
- Acute Coronary Syndrome Patterns in the Young: Risk Factor Profile and In-hospital Outcomes in a Tertiary Referral Hospital in Kenya. BMC Cardiovasc Disord. 2024;24:192.
- [CrossRef] [PubMed] [Google Scholar]
- Differences in Clinical Nature and Outcome among Young Patients Suffering from an Acute Coronary Syndrome. J Blood Med. 2021;12:1011-7.
- [CrossRef] [PubMed] [Google Scholar]







