Translate this page into:
Effect of Dapagliflozin on Left Ventricular Diastolic Function in Diabetics - A Prospective Interventional Study
*Corresponding author: Sri Kiran Jakkula, Department of Cardiology, Nizam’s Institute of Medical Sciences, Hyderabad, Telangana, India. srikiran.jakkula@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Jakkula SK, Maddury J, Nakka S, Kumar A. Effect of dapagliflozin on left ventricular diastolic function in diabetics - A prospective interventional study. Indian J Cardiovasc Dis Women 2022;7:137-42.
Abstract
Objectives:
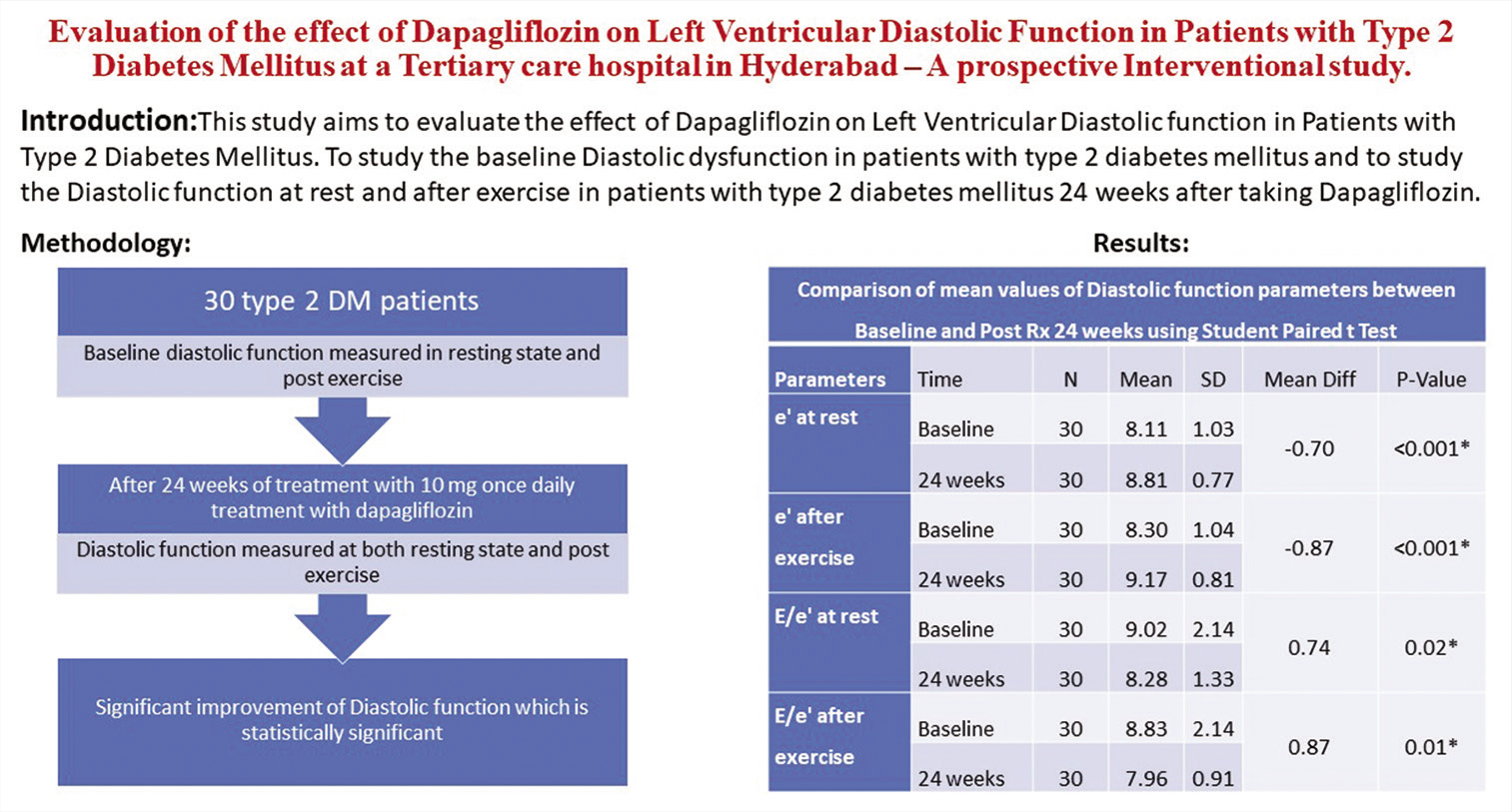
In patients with established heart failure, the SGLT2 inhibitor dapagliflozin found to alleviate the risk of worsening heart failure or cardiovascular mortality regardless of the presence of Diabetes Mellitus. To evaluate the effect of Dapagliflozin on Left Ventricular Diastolic function in Patients with Type 2 Diabetes Mellitus, to study the baseline Diastolic function in patients with type 2 diabetes mellitus and to study the Diastolic function at rest and after exercise in patients with type 2 diabetes mellitus 24 weeks after taking Dapagliflozin.
Materials and Methods:
It is a Prospective interventional Pilot study with study population consisting of T2DM who are 18 years and older with HbA1C between 7.0% to 10% and LV diastolic dysfunction of at least grade 1 on resting echocardiography. Baseline diastolic function was measured. Dapagliflozin 10 mg once daily was given to all patients for 24 weeks and then left ventricular diastolic function was measured by e’, E/A ratio, E/e’ at 24 weeks from baseline as assessed by Stress Echocardiography.
Results:
Diastolic Dysfunction grading between Baseline and post 24 weeks treatment with dapagliflozin, using Marginal Homogeneity Test showed p value <0.001 which is highly significant. Comparision of e’ at rest for baseline and post 24 weeks of treatment with dapagliflozin showed statistical significance. The e’ after exercise for baseline and post 24 weeks of treatment showed p value of <0.01. Comparision of E/e’ at rest and after exercise for baseline and post 24 weeks showed statistical significance.
Conclusion:
The diastolic function has been significantly improved after 24 weeks of using dapagliflozin. The diastolic function parameters between age and sex groups at baseline and post 24 weeks of treatment with dapagliflozin does not correlate.
Keywords
Dapagliflozin
Left ventricular diastolic function
Type 2 diabetes mellitus
ABSTRACT IMAGE
INTRODUCTION
Sodium-glucose cotransporter-2 (SGLT2) inhibitors witness to alleviate adverse cardiovascular outcomes in patients with Type 2 diabetes mellitus (T2DM) and the risk for cardiovascular disease.[1,2] In patients with established heart failure, the SGLT2 inhibitor dapagliflozin found to alleviate the risk of worsening heart failure or cardiovascular mortality regardless of the presence of diabetes mellitus (DM).[3] In patients with DM, the left ventricular (LV) diastolic dysfunction is associated with subsequent heart failure and mortality. This study aims to evaluate the effect of dapagliflozin on the LV diastolic function in patients with T2DM and to study the baseline diastolic dysfunction in patients with T2DM and to study the diastolic function at rest and after exercise in patients with T2DM 24 weeks after taking dapagliflozin.
MATERIALS AND METHODS
The study was done in a tertiary care center from June 2021 to November 2021 for a total duration of six months. It is a prospective interventional pilot study. The study population consists of T2DM patients presenting to the cardiology outpatient department. Patients who are 18 years and older with T2DM and glycated hemoglobin (HbA1c) of 7.0–10% with LV diastolic dysfunction of at least Grade 1 on resting echocardiography were included in the study. Patients with Type 1 DM, with a history of diabetic ketoacidosis, with a history of recurrent urinary tract infection, with renal dysfunction, patients using loop diuretics or with acute coronary syndrome, with a history of stroke within six months or with LV ejection fraction of <50% and with BMI ≥30 kg/m2, and with obstructive sleep apnea syndrome were excluded from the study. Patients satisfying the inclusion and exclusion criteria were enrolled in the study after taking a duly informed consent. Baseline diastolic function was measured in all patients enrolled in the study. Dapagliflozin 10 mg once daily was given to all patients enrolled in the study for 24 weeks and then the LV diastolic function was measured by e’, E/A ratio, and E/e’ at 24 weeks from baseline as assessed by stress echo.[4]
All the patients who qualify the inclusion and exclusion criteria were taken up for the study. Taking into consideration from the previous hospital records, around 50–60 T2DM patients visit outpatient department every day. Thirty patients were eligible for the study and these patients were followed up after 24 weeks for reassessment of diastolic function.
Statistical analysis
The Statistical Package for the Social Sciences for Windows, Version 22.0, was used to perform statistical analyses. Descriptive analysis includes expression of all the explanatory and outcome variables in terms of frequency and proportions for categorical variables, whereas in nine terms of mean and SD for continuous variables. Marginal homogeneity test was used to compare the grading of diastolic dysfunction between baseline and 24 weeks. Student’s paired t-test was used to compare the mean values of diastolic function parameters between baseline and post-treatment with dapagliflozin at 24 weeks. Independent Student’s t-test was used to compare the mean values of diastolic function parameters between age groups and gender at baseline and 24 weeks period. P < 0.05 is considered as statistically significant.
RESULTS
Total study sample consists of 30 out of which 47% are between 51 and 60 years, 33% between 41 and 50 years, and 20% <40 years of age [Figure 1 and Table 1]. Total 70% of the study population are males and 30% are females [Figure 2 and Table 2]. The mean HBA1c value is 8.2 ± 0.7 [Table 3]. [Table 4] shows the comparison of grading of diastolic dysfunction between baseline and post 24 weeks treatment with dapagliflozin, using marginal homogeneity test with P < 0.001 which is highly statistically significant. Paired Student’s t-test was used to compare mean values of diastolic function parameters between baseline and post 24 weeks of treatment with dapagliflozin. The e’ at rest for baseline and post 24 weeks [Figure 3] of treatment with dapagliflozin shows P < 0.001 which is highly significant [Table 5]. The e’ after exercise for baseline and 24 weeks [Figure 4] of treatment with dapagliflozin shows P < 0.01 which is statistically significant [Table 5]. The E/e’ at rest for baseline and post 24 weeks [Figure 5] of treatment with dapagliflozin shows P = 0.02, which is significant [Table 5]. The E/e’ after exercise for baseline and post 24 weeks [Figure 6] of treatment with dapagliflozin shows P = 0.01, which is significant [Table 5]. The mean values of diastolic function parameters between age groups at baseline period using independent Student’s t-test show no statistical significance [Table 6]. The mean values of diastolic function parameters between age groups post 24 weeks of treatment with dapagliflozin using independent Student’s t-tests show no statistical significance [Table 7]. The mean values of diastolic function parameters between genders at baseline period using independent Student’s t-test show no statistical significance [Table 8]. The mean values of diastolic function parameters between genders at post Rx 24 weeks period using independent Student’s t-test show no statistical significance [Table 9].

- Age-wise distribution of study patients.
| Age distribution among study patients | |||
|---|---|---|---|
| Variable | Category | n | % |
| Age | <40 years | 6 | 20.00 |
| 41–50 years | 10 | 33.30 | |
| 51–60 years | 14 | 46.70 | |
| Mean | SD | ||
| Mean | 48.77 | 7.38 | |
| Range | 36–60 years | ||
- Gender distribution of study patients.
| Gender distribution among study patients | |||
|---|---|---|---|
| Variable | Category | n | % |
| Gender | Males | 21 | 70 |
| Females | 9 | 30 | |
| Descriptive for HBA1c values among study patients | |||||
|---|---|---|---|---|---|
| Parameter | n | Mean | SD | Min. | Max. |
| HbA1c | 30 | 8.2 | 0.7 | 7.2 | 9.5 |
HbA1c: Glycated hemoglobin
| Comparison of grading of diastolic dysfunction between baseline and 24 weeks using marginal homogeneity test | |||||
|---|---|---|---|---|---|
| Diastolic dysfunction | Baseline | 24 weeks | P-value | ||
| n | % | N | % | ||
| No diastolic dysfunction | 0 | 0.0 | 8 | 26.7 | <0.001* |
| Grade 1 | 18 | 60.0 | 20 | 66.7 | |
| Grade 2 | 11 | 36.7 | 2 | 6.7 | |
| Grade 3 | 1 | 3.3 | 0 | 0.0 | |
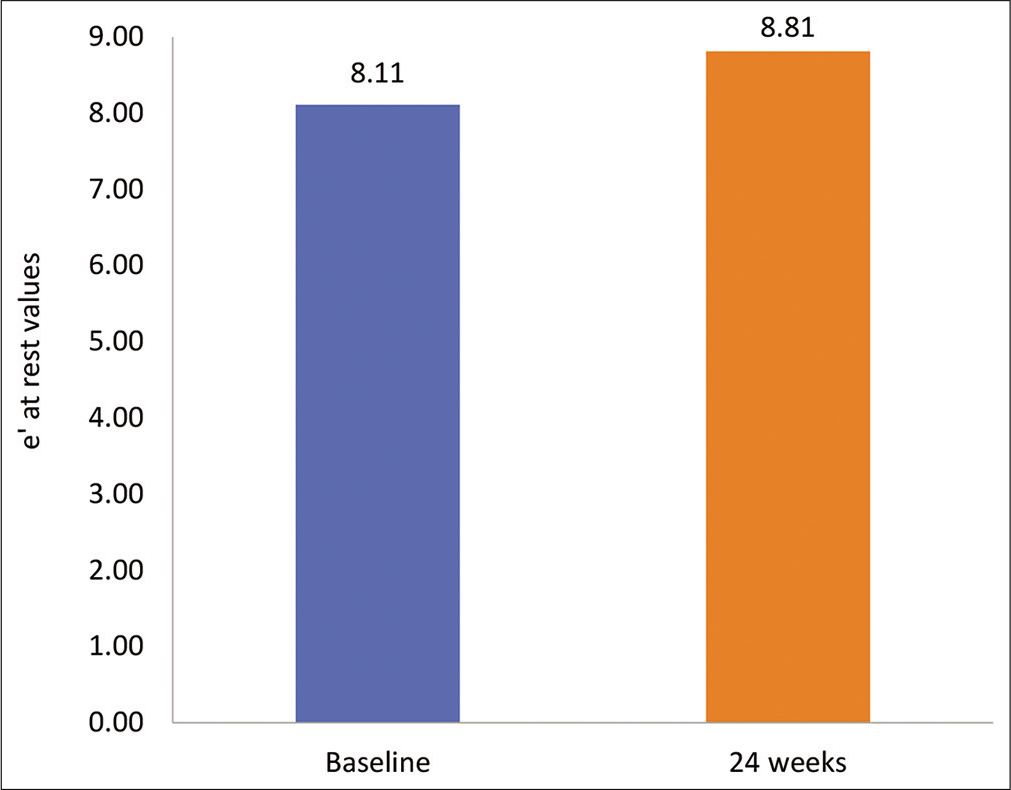
- Mean e’ at rest between baseline and post 24-week treatment with dapagliflozin.
| Comparison of mean values of diastolic function parameters between baseline and post Rx 24 weeks using Student’s paired t-test | ||||||
|---|---|---|---|---|---|---|
| Parameters | Time | N | Mean | SD | Mean diff. | P-value |
| e’ at rest | Baseline | 30 | 8.11 | 1.03 | –0.70 | <0.001* |
| 24 weeks | 30 | 8.81 | 0.77 | |||
| e’ after exercise | Baseline | 30 | 8.30 | 1.04 | –0.87 | <0.001* |
| 24 weeks | 30 | 9.17 | 0.81 | |||
| E/e’ at rest | Baseline | 30 | 9.02 | 2.14 | 0.74 | 0.02* |
| 24 weeks | 30 | 8.28 | 1.33 | |||
| E/e’ after exercise | Baseline | 30 | 8.83 | 2.14 | 0.87 | 0.01* |
| 24 weeks | 30 | 7.96 | 0.91 | |||
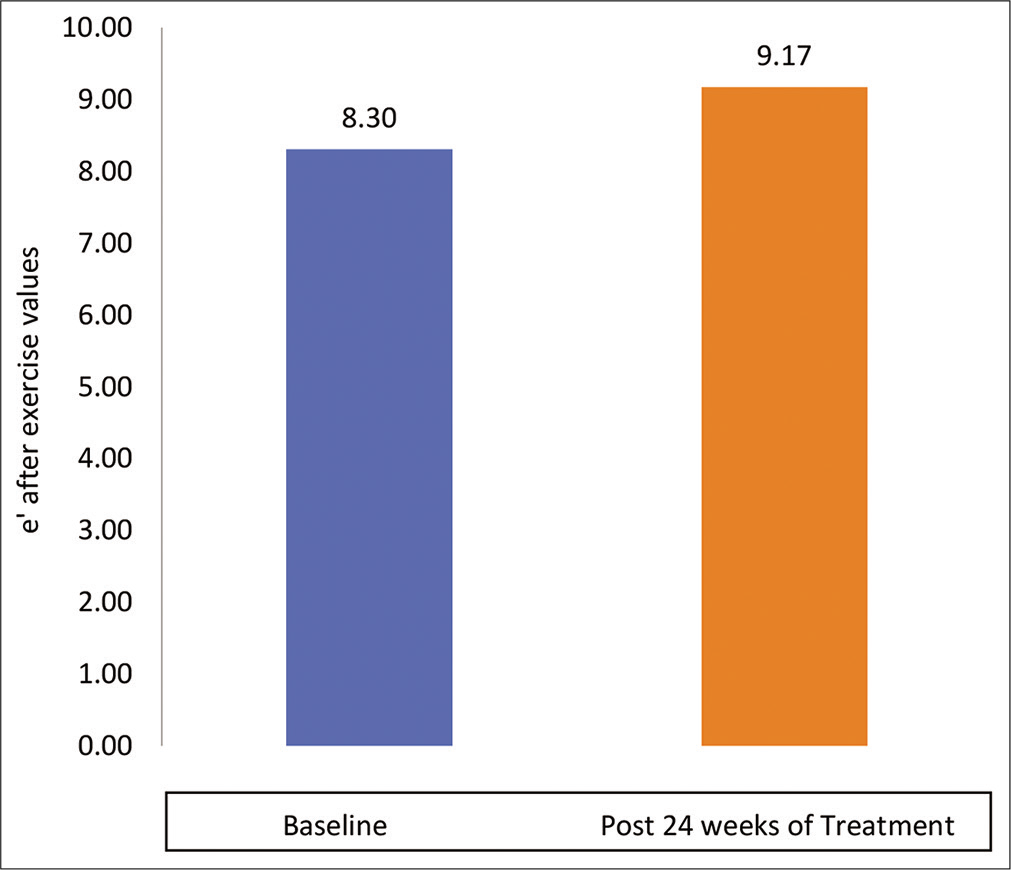
- Mean e’ after exercise between baseline and post 24-week treatment with dapagliflozin.
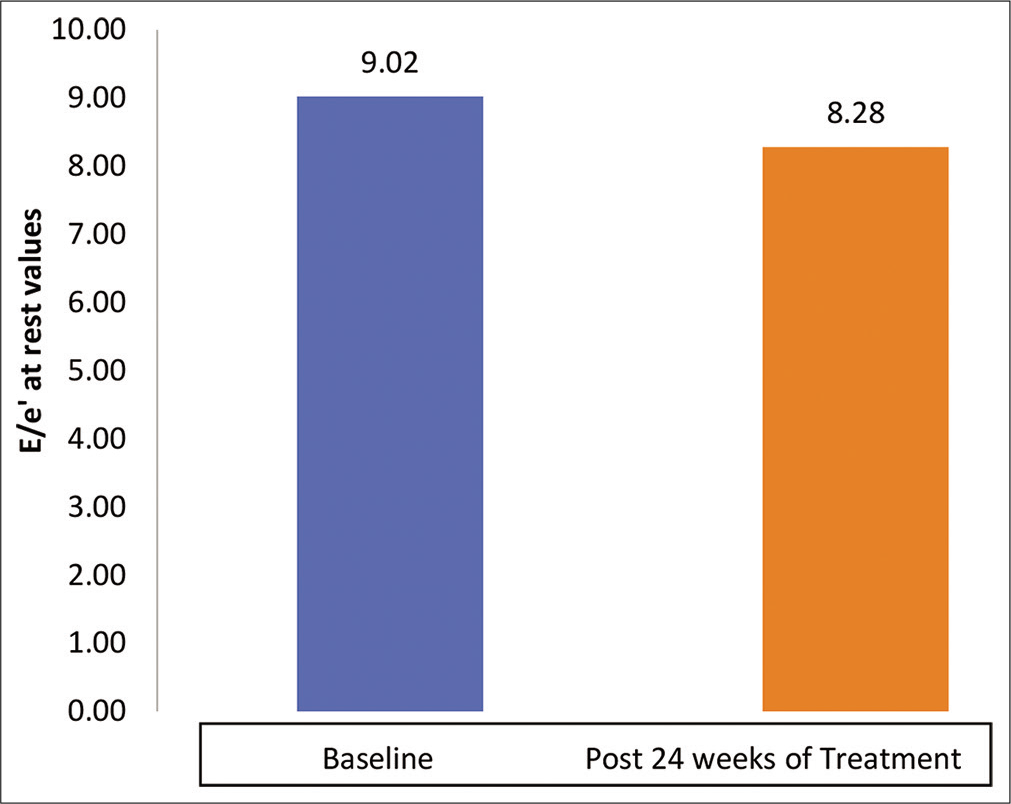
- Mean E/e' at rest between baseline and post 24-week treatment with dapagliflozin.
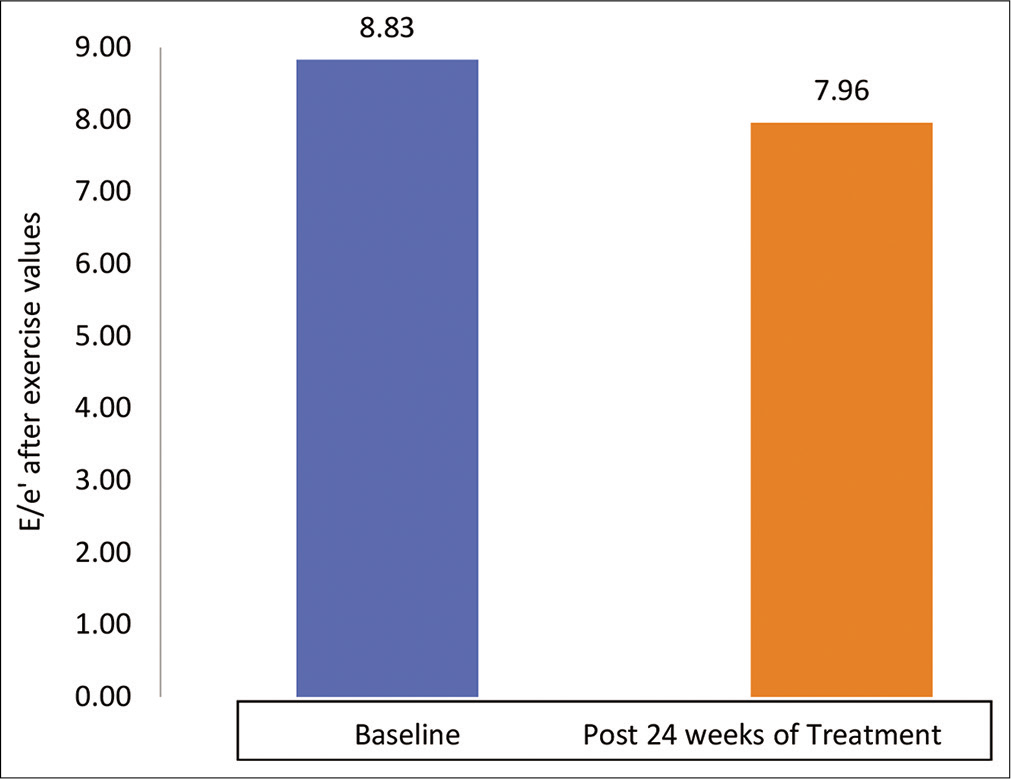
- Mean E/e’ after exercise between baseline and post 24-week treatment with dapagliflozin.
| Comparison of mean values of diastolic function parameters between age groups at baseline period using independent Student’s t-test | ||||||
|---|---|---|---|---|---|---|
| Parameters | Age | N | Mean | SD | Mean diff. | P-value |
| e’ at rest | ≤50 years | 16 | 8.00 | 1.14 | –0.23 | 0.56 |
| >50 years | 14 | 8.23 | 0.92 | |||
| e’ after exercise | ≤50 years | 16 | 8.16 | 1.13 | –0.30 | 0.44 |
| >50 years | 14 | 8.46 | 0.94 | |||
| E/e’ at rest | ≤50 years | 16 | 9.09 | 2.01 | 0.15 | 0.85 |
| >50 years | 14 | 8.94 | 2.36 | |||
| E/e’ after exercise | ≤50 years | 16 | 8.93 | 1.96 | 0.22 | 0.78 |
| >50 years | 14 | 8.71 | 2.41 | |||
| Comparison of mean values of diastolic function parameters between age groups at post Rx 24 weeks period using independent Student’s t-test | ||||||
|---|---|---|---|---|---|---|
| Parameters | Age | N | Mean | SD | Mean diff. | P-value |
| e’ at rest | ≤50 years | 16 | 8.86 | 0.64 | 0.11 | 0.7 |
| >50 years | 14 | 8.75 | 0.91 | |||
| e’ after exercise | ≤50 years | 16 | 9.25 | 0.71 | 0.17 | 0.57 |
| >50 years | 14 | 9.08 | 0.92 | |||
| E/e’ at rest | ≤50 years | 16 | 7.98 | 0.53 | –0.65 | 0.19 |
| >50 years | 14 | 8.63 | 1.84 | |||
| E/e’ after exercise | ≤50 years | 16 | 7.79 | 0.45 | –0.36 | 0.29 |
| >50 years | 14 | 8.15 | 1.25 | |||
| Comparison of mean values of diastolic function parameters between genders at baseline period using independent Student’s t-test | ||||||
|---|---|---|---|---|---|---|
| Parameters | Gender | N | Mean | SD | Mean diff. | P-value |
| e’ at rest | Males | 21 | 8.30 | 1.01 | 0.63 | 0.13 |
| Females | 9 | 7.67 | 1.01 | |||
| e’ after exercise | Males | 21 | 8.51 | 1.01 | 0.69 | 0.1 |
| Females | 9 | 7.82 | 1.01 | |||
| E/e’ at rest | Males | 21 | 8.76 | 2.31 | -0.89 | 0.31 |
| Females | 9 | 9.64 | 1.64 | |||
| E/e’ after exercise | Males | 21 | 8.60 | 2.34 | -0.76 | 0.39 |
| Females | 9 | 9.36 | 1.60 | |||
| Comparison of mean values of diastolic function parameters between genders at post Rx 24 weeks period using independent Student’s t-test | ||||||
|---|---|---|---|---|---|---|
| Parameters | Gender | n | Mean | SD | Mean diff. | P-value |
| e’ at rest | Males | 21 | 8.96 | 0.71 | 0.51 | 0.10 |
| Females | 9 | 8.46 | 0.81 | |||
| e’ after exercise | Males | 21 | 9.34 | 0.75 | 0.56 | 0.08 |
| Females | 9 | 8.78 | 0.84 | |||
| E/e’ at rest | Males | 21 | 8.27 | 1.56 | -0.05 | 0.92 |
| Females | 9 | 8.32 | 0.57 | |||
| E/e’ after exercise | Males | 21 | 7.98 | 1.04 | 0.07 | 0.86 |
| Females | 9 | 7.91 | 0.54 | |||
DISCUSSION
The LV diastolic function as assessed by E/e’ for T2DM patients was significantly improved after six months of dapagliflozin intake. SGLT2 inhibitors are associated with weight loss, blood pressure, and an HbA1c level reduction, making an impact on LV function. Hence, in patients with T2DM, SGLT2 inhibitors may have a potential beneficial effect on LV diastolic function. Recently, it had been reported that SGLT2 inhibitors have a multiple effects on cardiac function including improvement in endothelial dysfunction and aortic stiffness,[5] reduction in accumulation of epicardial fat[4] as well as in visceral adipocyte hypertrophy.[6] These mechanisms may lead to LV diastolic function improvement. Verma et al. observed in 10 patients, the effects of empagliflozin (10 mg/day), an SGLT2 inhibitor, post three months of its usage in patients with cardiovascular disease and T2DM, in relation to objective measurements of cardiac structure and function. This short duration treatment with empagliflozin was associated with a significant LVMI reduction and improvement of LV diastolic function.[7] Matsutani et al. reported the effects of canagliflozin on LV diastolic function in 37 T2DM patients with preserved LVEF in a prospective single-center pilot study.[8] The LV diastolic function post three months after the initiation of canagliflozin has shown significant improvement.[8] Although the exact mechanism of the effects of SGLT2 inhibitors on LV diastolic function is uncertain, the increased diuresis with reduced pre-load may play a major role. In patients with HFrEF, HFmrEF, as well as HFpEF, LV diastolic function plays an important role in the development of cardiovascular events and outcomes. Large outcome trials demonstrated the efficacy of neurohumoral inhibition in HFrEF but not in the case of HFpEF, because the neurohumoral inhibition consistently failed to attain a positive primary outcome.[9-11] This study shows the effectiveness of dapagliflozin on diastolic function in patients with T2DM.
CONCLUSION
The diastolic function of the heart has been significantly improved after 24 weeks of using dapagliflozin. The diastolic function parameters between age and sex groups at baseline and post 24 weeks of treatment with dapagliflozin do not correlate. The diastolic dysfunction is independent of age and sex.
Limitations of the study
Sample size is small and larger sample size is needed to confirm the findings. Lack of control arm in the study is one of the limitations of the study. Comorbidities such as hypertension and obesity and other antidiabetic drugs which were taken along with dapagliflozin such as metformin and glimepiride could act as confounding factors in this study.
Audio summary available at
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Dapagliflozin and cardiovascular outcomes in Type 2 diabetes. N Engl J Med. 2019;380:347-57.
- [CrossRef] [PubMed] [Google Scholar]
- Empagliflozin, cardiovascular outcomes, and mortalityin Type 2 diabetes. N Engl J Med. 2015;373:2117-28.
- [CrossRef] [PubMed] [Google Scholar]
- Dapagliflozin in patientswith heart failure and reduced ejection fraction. N Engl J Med. 2019;381:1995-2008.
- [CrossRef] [PubMed] [Google Scholar]
- The renal tubular damage marker urinary N-acetyl-beta-Dglucosaminidase may be more closely associated with early detection of atherosclerosis than the glomerular damage marker albuminuria in patients with Type 2 diabetes. Cardiovasc Diabetol. 2017;16:16.
- [CrossRef] [PubMed] [Google Scholar]
- Dapagliflozin acutely improves endothelial dysfunction, reduces aortic stiffness and renal resistive index in Type 2 diabetic patients: A pilot study. Cardiovasc Diabetol. 2017;16:138.
- [CrossRef] [PubMed] [Google Scholar]
- Empagliflozin lessened cardiac injury and reduced visceral adipocyte hypertrophy in prediabetic rats with metabolic syndrome. Cardiovasc Diabetol. 2016;15:157.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of empagliflozin on left ventricular mass and diastolic function in individuals with diabetes: An important clue to the EMPA-REG OUTCOME trial? Diabetes Care. 2016;39:e212-3.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of canagliflozin on left ventricular diastolic function in patients with Type 2 diabetes. Cardiovasc Diabetol. 2018;17:73.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of heart failure with normal ejection fraction: An inconvenient truth! J Am Coll Cardiol. 2010;55:526-37.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of treatment on exercise tolerance, cardiac function, and mortality in heart failure with preserved ejection fraction. A meta-analysis. J Am Coll Cardiol. 2011;57:1676-86.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical effectiveness of beta-blockers in heart failure: Findings from the OPTIMIZE-HF (Organized program to initiate lifesaving treatment in hospitalized patients with heart failure) registry. J Am Coll Cardiol. 2009;53:184-92.
- [CrossRef] [PubMed] [Google Scholar]







