Translate this page into:
ECG—An Axis Dilemma with Tachycardia
Seema Kale, MD Apollo Clinic, Rajouri Garden New Delhi 110027 India drseemakale@hotmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Cardiac arrhythmias are common in acute myocardial infarction (MI), especially in ST elevation MI. Almost 90% of patients develop some form of cardiac arrhythmia in acute MI. Mostly they are benign and transient. Incidence of atrial tachycardia is fairly uncommon in such setting. Most of the arrhythmias disappear after reperfusion. Interpretation of electrocardiograms (ECGs) in emergency becomes even more difficult if there is unusual QRS axis and possibility of arm lead reversal.
Keywords
atrial tachycardia
STEMI
right axis
sinus
Author: Dr Seema Kale
A 50-year-old man presented with chest pain with sweats; no other risk factors were present.
Opinion 1
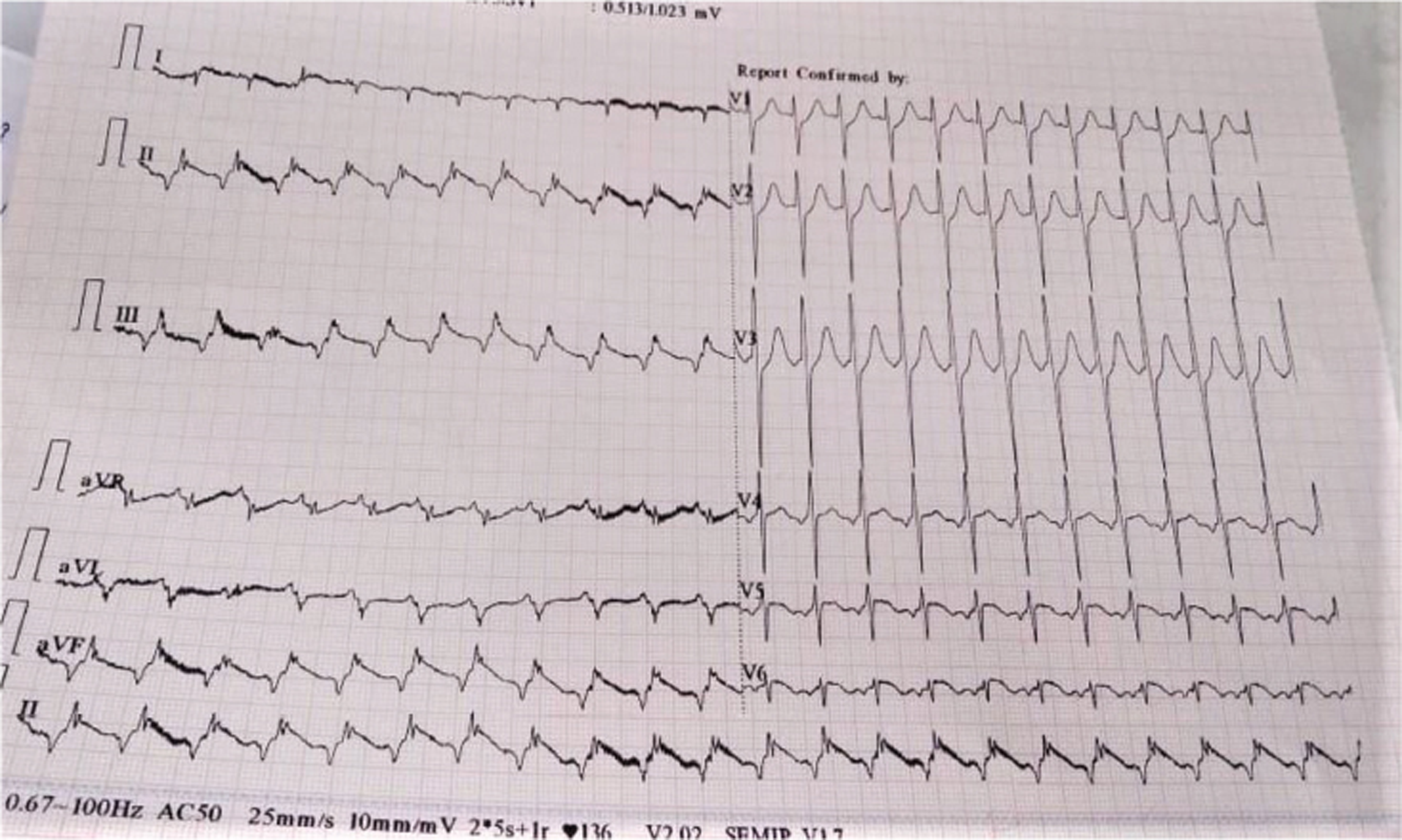
Fig. 1 shows a long RP tachycardia with1:1 AV conduction at heart rate of approximately 138 bpm with inferolateral ST elevation myocardial infarction (MI). The P-QRS-T morphology are negative in I. V6 shows biphasic P and RS complex.
-
Fig. 1 ECG at presentation.
Fig. 1 ECG at presentation.
II, III, AVF show “inverted P.” There is poor transition of QRS (rS) from V1–6.
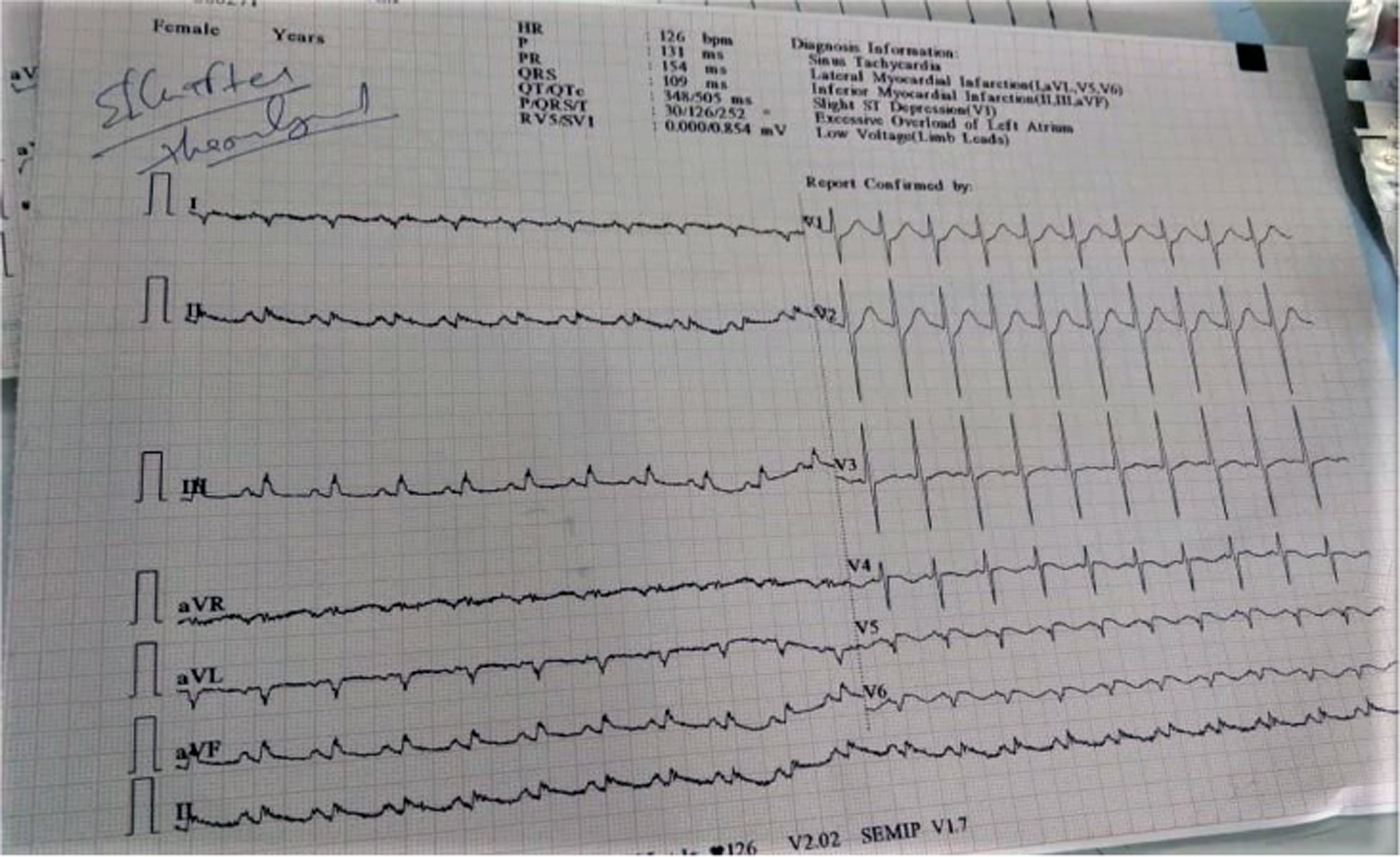
Post thrombolysis, we find sinus tachycardia at nearly the same rate, same PR interval, with change in P which is positive in I, II, III, AVF (Fig. 2). The ST has settled down.
-
Fig. 2 Post thrombolysis.
Fig. 2 Post thrombolysis.
The doctor in the emergency room (ER) is faced with critical electrocardiogram (ECG) diagnosis. Normally (s)he looks for normalcy, normal variants, ischemia, and arrhythmia. But the ER ECG can also be subject to lead misconnection, misplacement, and artifacts.
Fig. 1 suggests MI with dextrocardia, atrial tachycardia, and congenital heart disease, but this is due to lead misconnection, which is rectified in Fig. 2.
Right and left arm lead reversal causes P-QRS-T reversal in I, and negative P in II, III, and AVF. Normally, I and V6 show similar polarity. Discordance suggests lead reversal.
Despite change in morphology the PR remains same in both ECGs, again suggesting lead reversal.
Atrial arrhythmias are known in acute MI, but are unusual.
Opinion 2
In Fig. 1, the ECG shows ectopic atrial tachycardia from a low atrial focus, and in Fig. 2 the ECG shows sinus rhythm with acute lateral wall injury.
Opinion 3
In Fig. 1, the ECG reveals atrial tachycardia; QRS axis is 100 approximately. QRS is narrow, PR interval is normal; Q waves are seen in leads I, aVL, V5, and V6. R/S in V1 is equal, with upright T in V1. ST elevation is seen in V5 and V6, but in I and aVL ST elevation is not evident due to technical issue.
All suggest evolved lateral wall MI. RT QRS axis at first look gives impression of lead reversal but it is not there.
Author’s Opinion
In Fig. 1 the ECG revealed a narrow complex tachycardia. Heart rate (HR) was ~138/min; each QRS was preceded by P wave, but the P waves were inverted in inferior leads and upright in aVR.
Inverted P waves were also seen in V4, V5, and biphasic in V6 before each QRS and upright P in V1 and aVL; all this suggested that P waves were not sinus in origin.
So, it was most likely focal atrial tachycardia (long RP). Since P waves were negative in inferior leads, the origin of P waves could be low RA, low LA, proximal CS, or low atrial septum.
But it was difficult to assess whether it was from RA or LA, as the P wave was upright in aVL (which indicates RA origin), but upright in V1 too, which indicates LA origin!
Another differential was nonparoxysmal junctional tachycardia (NPJT). In NPJT, retrograde P waves are similar but would be close to QRS, so PR interval in NPJT is <120 milliseconds, which was not the case here.
There was ST elevation in inferior leads and lead I, V5, and V6; this was suggestive of inferolateral STEMI. Voltage was low in limb leads.
The QRS axis was right, which appeared initially as due to arm lead reversal, but on closer inspection the right axis appeared to be due to QS complex in lead I due to lateral MI.
Low precordial voltage in V5, V6 was also due to lateral MI.
Final impression: acute inferolateral STEMI with focal atrial tachycardia.
Fig. 2 is post thrombolysis; ST segment elevation has reduced especially in inferior leads; and some ST elevation is still persisting in V5, V6, with development of Q in V5 and V6. Heart rate is approximately the same ~132/min but now it is sinus tachycardia, P waves are upright in inferior leads and inverted in avR.
QRS axis is still right due to Q waves in lead I.
Atrial tachycardia in this case was transient and with reperfusion it disappeared; it did not require treatment.
The hemodynamic consequences of this rhythm are usually minimal as the rhythm is supraventricular with narrow QRS and heart rate is also only modestly elevated!
Expert’s Opinion
In the setting of inferolateral STEMI, there is atrial tachycardia, probably arising from lower crista or coronary sinus (CS).
Tachycardia arising from CS OS is a possibility as it is close to inferior septum and tachycardia P waves are narrower than sinus P waves.
There is no lead reversal as postconversion and preconversion QRS axis is same.
Discussion
Right Axis Deviation, Common Causes
The most common causes of right axis deviation are as follows:
-
Arm lead reversal.
-
Dextrocardia.
-
Pulmonary embolism.
-
COAD.
-
Hyperkalemia.
-
RAD is uncommon in MI except lateral MI, wherein RAD is due to Q waves in lead I and development of left posterior fascicular block.
Dilemma of Right Axis
In this case due to negative QRS in lead I, the first thought that comes is of either lead reversal or dextrocardia.
-
Why not is it lead reversal?1
Following lead reversal will cause negative QRS in lead I.
-
RA/LA (right arm/left arm) lead reversal.
-
RA/ LL (right arm/ left leg) lead reversal.
-
RA/RL or N (right arm/right leg or neutral limb) lead reversal.
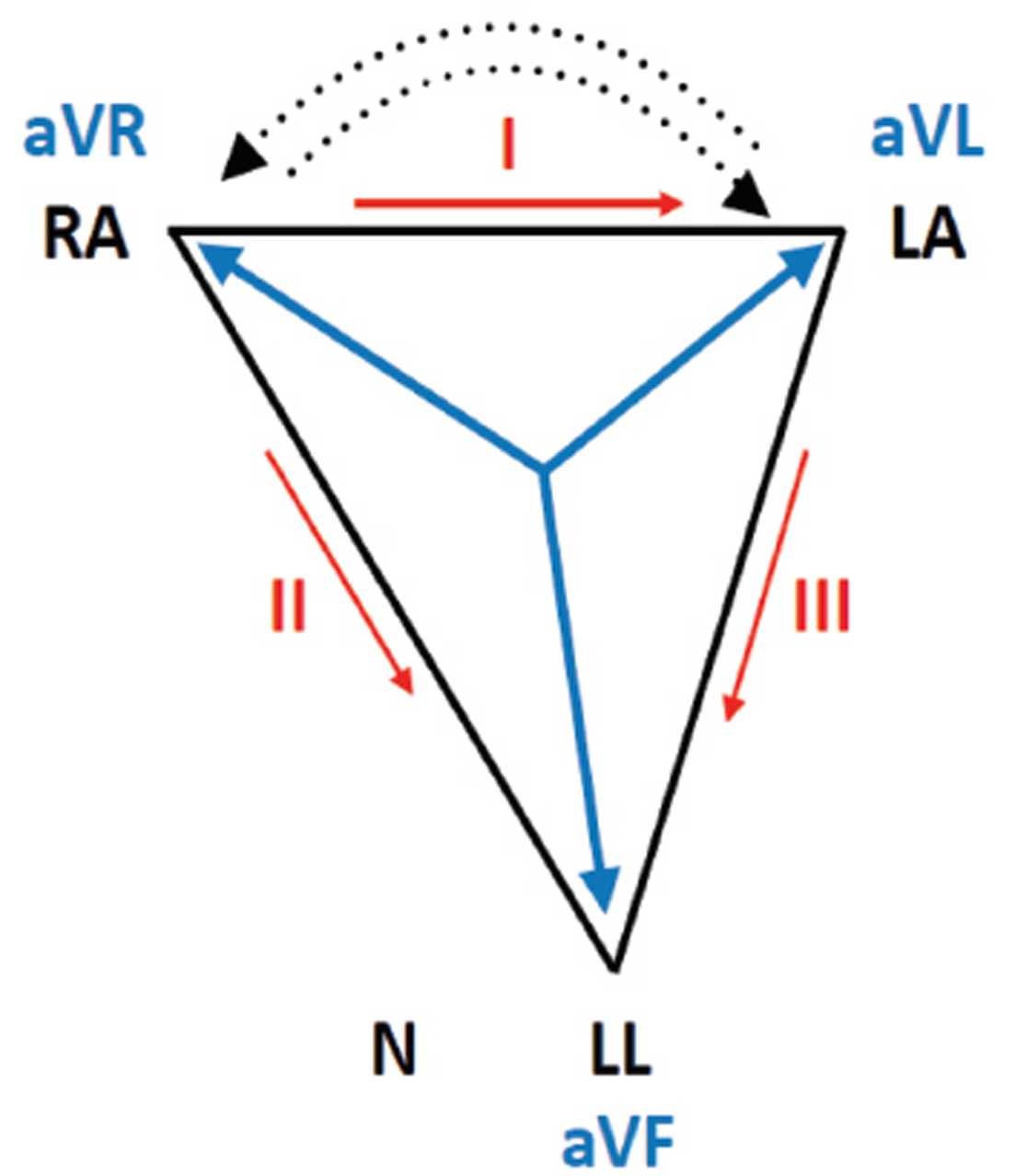
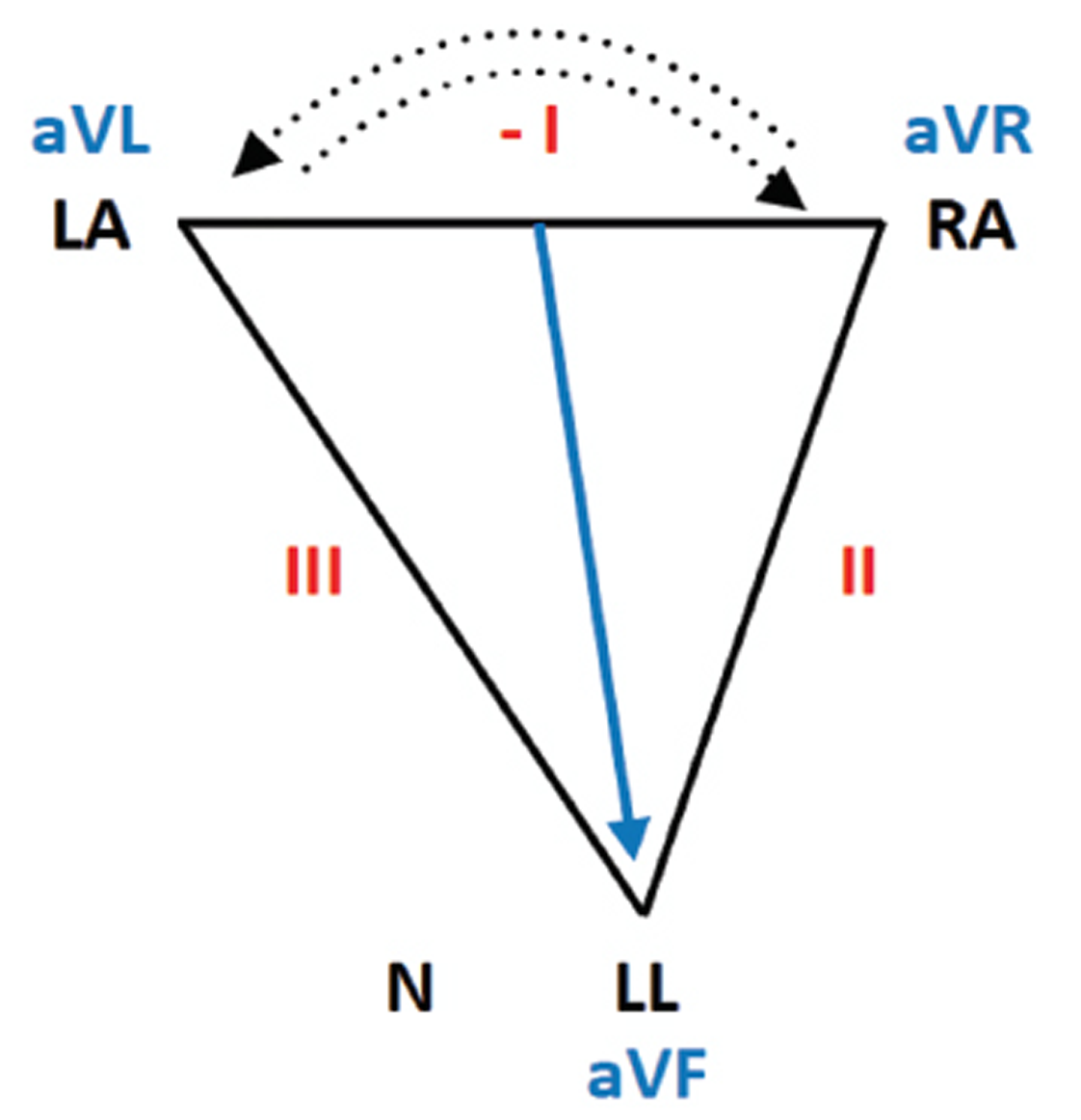
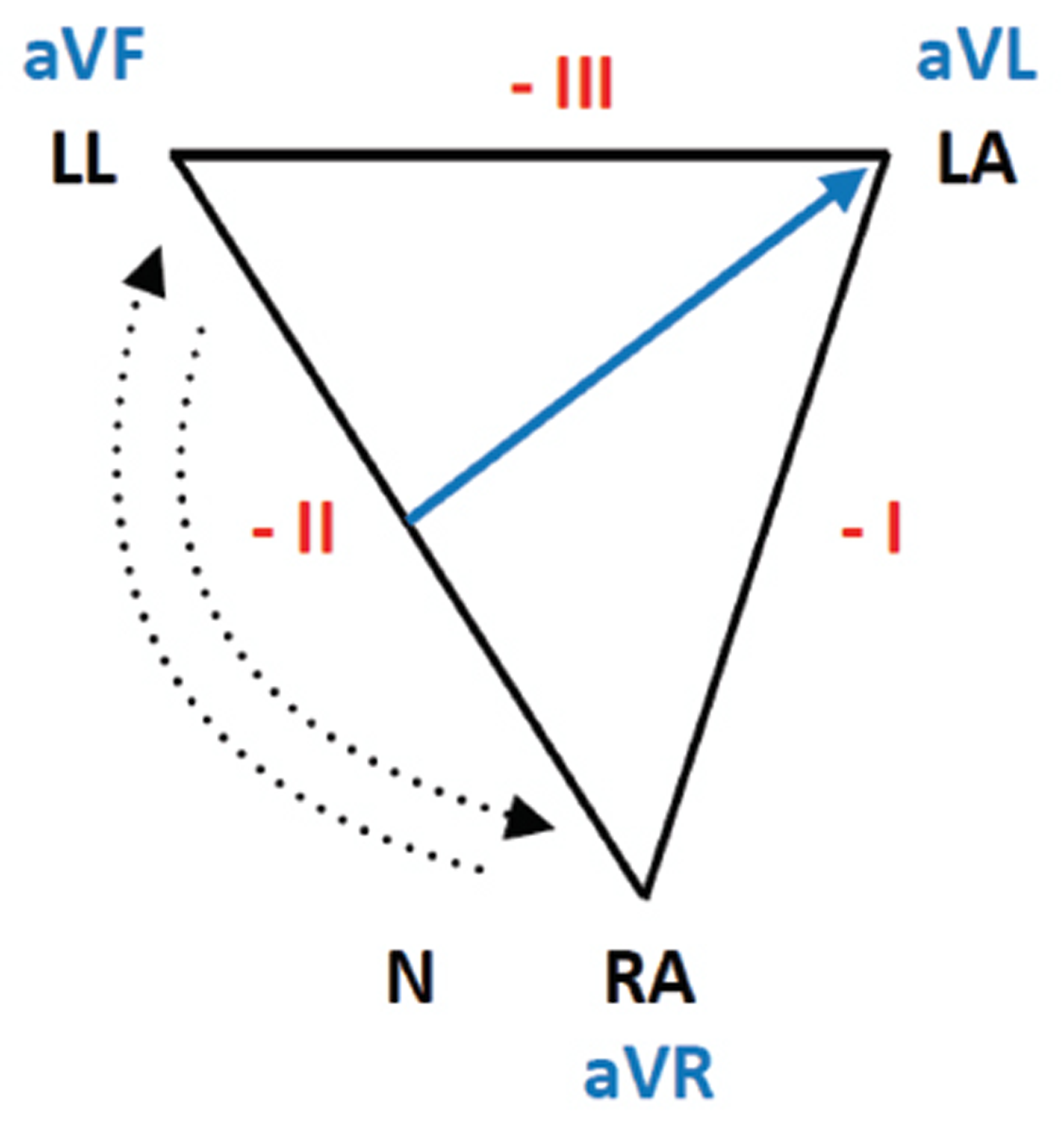
In RA/LA arm reversal (Figs. 3 and 4), the Einthoven triangle rotates horizontally by 180°along axis of aVF. The following changes occur in ECG:
-
Fig. 3 Einthoven triangle.
Fig. 3 Einthoven triangle.
-
Fig. 4 RA/LA reversal.
Fig. 4 RA/LA reversal.
-
Lead I: becomes total negative.
-
aVR and aVLswitch.
-
Lead II and III switch.
-
aVF: unchanged.
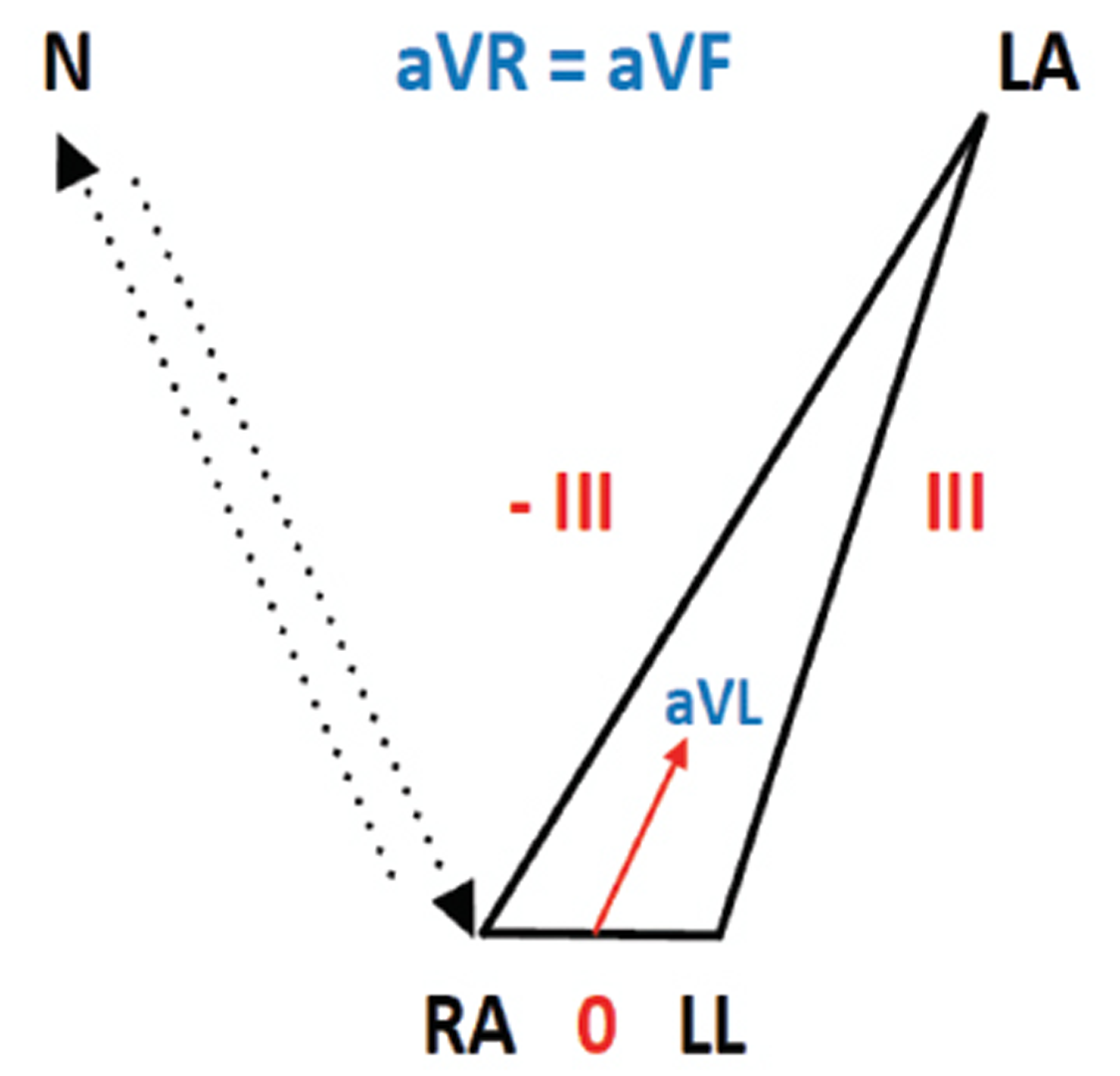
In RA/LL reversal ( Fig. 5 ), the Einthoven triangle flips vertically by 180°along the axis formed by a VL. The following changes occur:
-
Fig. 5 RA/LL lead reversal.
Fig. 5 RA/LL lead reversal.
-
Lead II: becomes negative.
-
Lead I, III: switch places and become negative.
-
aVF and aVR: switch places—aVF becomes negative, avR becomes positive.
-
aVL: unchanged.
In RA/RL or N reversal (Fig. 6), the following occur:
-
Fig. 6 RA/RL or N (neutral) lead reversal.
Fig. 6 RA/RL or N (neutral) lead reversal.
-
Lead I: is now inverted III.
-
Lead II: flat line.
-
Lead III: unchanged.
-
aVR, aVF: identical.
-
aVL: similar to inverted III.
In Figs. 1 and 2 both ECGs show RT axis so it is unlikely that the mistake of lead reversal the second time too. Also, aVF shows a change in P wave, which is inverted in Fig. 1 then becomes upright post thrombolysis in Fig. 2. So, it is not RA/LA arm lead reversal because aVF shows no change in lead reversal.
II, III, aVF show positive QRS, so it is not RA/LL reversal.
Lead II is not a flat line, so it is not RA/RL reversal.
-
2. Why not dextrocardia?
In dextrocardia, along with RT axis there is progressive diminution of QRS across chest leads. In Figs. 1 and 2, initially from v1 to v3 there is progressive increase in QRS then in v5, v6 it diminishes due to lateral MI. Also, there is positive terminal P seen after careful examination in most of the complexes in lead I, which suggests that it is not dextrocardia.
Other causes of RT axis deviation were not relevant in this case.
Cardiac Arrhythmia and Acute MI
-
Cardiac arrhythmias are more commonly associated with STEMI than non-STEMI.
-
In acute MI, 90% cases develop some form of cardiac arrhythmia, and 25% such rhythm abnormalities occur within first 24 hour.
-
Most peri-infarction arrhythmias are benign and self-limiting.
-
Common arrhythmias are sinus tachycardia, premature ventricular complexes (PVCs), premature atrial complexes (PACs), sinus bradycardia, atrioventricular (AV) blocks, ventricular tachycardia (VT), atrial fibrillation, ventricular fibrillation (VF).
-
Incidence of atrial tachycardia is low, 1.2 to 3.9% in various studies.2
Atrial Tachycardia
It is a supraventricular tachycardia, originating from different sites in atrium, other than sinus node.
-
Its narrow complex regular tachycardia, unless underlying BBB or intraventricular aberration is seen.
-
It does not need AV node or accessory pathway or ventricles for its initiation or maintenance.
-
The usual atrial rate is 150 to 200; it can vary from 100 to 250/min.3
-
P wave axis and morphology differs from sinus P.
-
There is isoelectric line in between two P waves.
-
It is a long RP tachycardia.
-
The usual sites of origin of P waves—approximately 60% arise in RA, 40% in LA.
-
Right atrium (RA) sites: crista terminalis, TV annulus, coronary sinus OS, and near AV junction.
-
Left atrium (LA) sites: 67% of LA tachycardia arises near pulm vein (PV) orifices, other sites are MV annulus and CS body.
-
Common in all ages, both sexes; can occur in normal hearts and in hearts with structural disease, especially complex congenital heart disease.
-
It is most common PSVT, one-fourth of the elderly people undergoing Holter monitoring reveal atrial tachycardia.
-
AV conduction can be 1:1 or if atrial rate is too fast and AVN becomes refractory, then 2:1 or Wenckebach block is also possible.4
-
Atrial tachycardia with 2:1 conduction is called PAT with block, classically seen with digi toxicity.
IMP leads used to assess origin of tachycardia (percentage is variable in different studies)5
-
aVL: positive [+] or biphasic P wave [−/+ ]—RA tachycardia sensitivity specificity (direction of P toward left) 88% 79%.
-
V1: positive [+] or biphasic P [−/+] : LA tachycardia 93 to 100% 88% (direction of P toward right).
-
V1: negative [-] or biphasic P [+/−] : RA tachycardia 60 to 70% 100% (direction of P away from right).
-
Lead I: negative [-] or isoelectric P : LA tachycardia 50% 100% (direction of P away from left).
Clinical Types of Atrial Tachycardia
-
FAT: Focal atrial tachycardia.
Arises from single ectopic focus in atrium, as in this case. Overall, its benign.6
-
MAT: Multifocal atrial tachycardia.
Arises from multiple sites in atrium, common in chronic obstructive airway disease (COAD) or severe congestive heart failure (CHF).
-
Incessant atrial tachycardia: type of FAT.
-
They represent 25% of FAT.
-
-
Incessant tachycardia means a tachycardia that is present at least 50% of the time the patient is being monitored.
-
It is mostly automatic, common focus being atrial appendage (84%), PV (59%).
-
Cardiomyopathy is seen in one-third of cases.
-
It causes cardiomyopathy because this tachycardia is slower, so symptoms are negligible and go unrecognized.
Pathophysiological Classification of Atrial Tachycardia7
-
Automaticity
-
Due to enhanced automaticity in a focus, for example, in ischemic heart disease, chronic lung disease with acute exacerbation, and acute alcohol ingestion.
-
-
In children due to enhanced automaticity in atrial tissue remnants.8
-
Atrial tachycardia due to enhanced automaticity is uncommon in geriatric age group as with age automaticity decreases.8
-
Tachycardia due to this mechanism generally arises in atrial appendages, or near PV orifices.
-
There is “warm up” phenomenon, (means tachycardia slowly picks up speed) at the start of tachycardia due to enhanced automaticity and “cool down” phase (means slows down for some time before terminating), towards the end.
-
Electrophysiologically it is not initiated or terminated by single PAC.
-
First P wave of tachycardia is the same as the subsequent P waves of tachycardia.
-
AVN is not part of tachycardia circuit so AVN blockers have no effect in this tachycardia; they can only slow down ventricular rate and reveal P waves better.
-
Carotid sinus massage and adenosine are not effective in terminating this tachycardia. They will slow down ventricular rate.
-
Usually terminated by β-blocker (because automaticity is due to excess catecholamines).
-
Isoproterenol induces it.
-
DC cardioversion is ineffective!
-
Triggered activity
-
Atrial tachycardia due to triggered activity is due to delayed after depolarization (DAD). DAD is a low-amplitude potential just at the end of action potential; if it reaches threshold, it can give rise to depolarization and spontaneous action potential and if it is repeated it can give rise to atrial tachycardia. For example, Digoxin toxicity.
-
-
Tachycardia due to triggered activity generally arises from crista terminalis, TV, and MV annulus.
-
The first P wave of tachycardia differs from other tachycardia beats.
-
There is no warm up or cool down phase.
-
Response to AVN blocking drugs is variable. Significant proportion respond to adenosine! Vagal maneuvers may terminate it.
-
This tachycardia is initiated and terminated by rapid atrial pacing and PACs.
-
RX of atrial tachycardia due to digi toxicity: withhold digoxin, give potassium, digoxin antibody.
-
Micro re-entry
-
This is an uncommon mechanism of atrial tachycardia commonly seen post surgery for congenital heart disease, or post ablation; scar and patches serve as substrate for re-entry.
-
-
As a rule tachycardia due to re-entry is initiated by PAC and terminated by PAC.
-
It has abrupt onset and abrupt offset. There is no warm up and cool down phase.
-
First P wave morphology differs from subsequent P waves during tachycardia.
-
Generally it is not affected by adenosine or other AVN blockers such as β-blocker or calcium channel blockers, because AV node is not a part of tachycardia circuit in atrial tachycardia. But tachycardia arising from perinodal region will respond.
Causes of atial tachycardia in MI are as follows:
-
It could be due to atrial infarction.
-
Due to excess catecholamine release, enhancing automaticity. Increased automaticity of His–Purkinje system can lead to NPJT.
-
Hypoxemia.
-
In inferior wall MI, sinus node ischemia, sinus bradycardia, or arrest along with raised ventricular end diastolic pressure (EDP) and atrial stretch are also important mechanisms.
Thrombolysis leads to reperfusion of sinus node and/or normalization of ventricular EDP, both leading to restoration of sinus rhythm.
Treatment of Atrial Tachycardia9 10
-
Due to acute myocardial ischemia, PCI or thrombolysis will take care of arrhythmia, as in this case.
-
Drugs:Used in hemodynamically stable cases, they have modest efficacy, effective in 30 to 50% cases, may terminate or slow the tachycardia rate.
-
◦ A—AV nodal blocker; B—Class I C antiarrhythmic; C—Class III.
-
A. AV nodal blockers:
-
β-blockers (class I indication).
-
Dilzem (class I indication).
-
Verapamil (class I indication).
-
Adenosine (class II a).
-
Digoxin has not been well studied in atrial tachycardia.
Remember, if we give calcium channel blocker in atrial tachycardia, it may cause precipitous fall in BP and hemodynamic collapse due to peripheral vasodilatation.In such cases prior injection of 10 mL of 10% 1 g calcium gluconate may be given slow IV before giving the calcium channel blocker.
-
B. Class I C antiarrhythmic drugs: (Flecainide/propafenone, in cases with no structural heart disease) (class IIb). They are given in recurrent atrial tachycardia or if tachycardia is not responding to AVN blockers.
-
C. Class III(amiodarone/sotalol): They are given for maintenance of sinus rhythm.
Nonpharmacological
DC cardioversion: (For hemodynamically unstable, class I; automatic atrial tachycardia may not respond.
Chronic Management of Atrial Tacycardia10
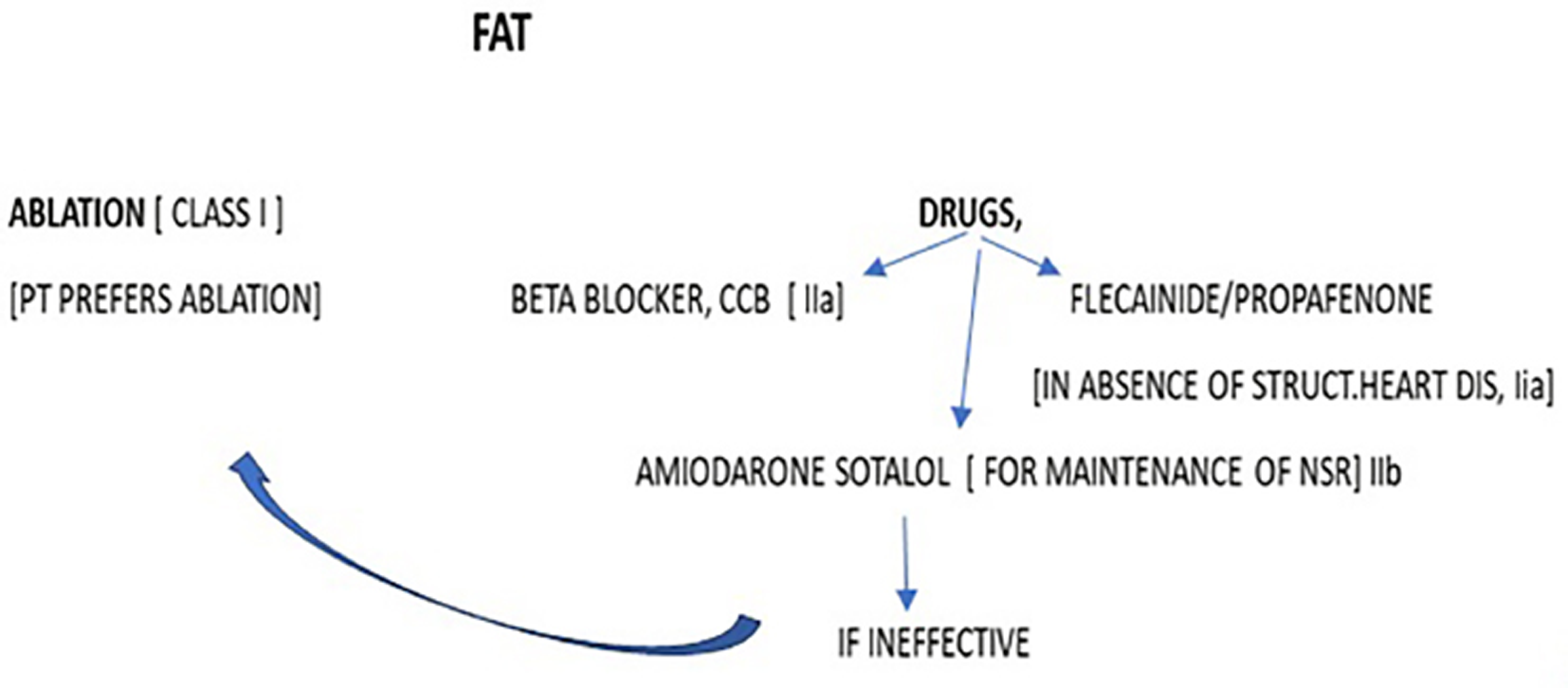
Rx of choice is catheter ablation (Fig. 7).
-
Fig. 7 Focal atrial tachycardia, management.
Fig. 7 Focal atrial tachycardia, management.
Catheter ablation: Radiofrequency/cryothermal ablation is the preferred choice of treatment.
-
Success rate: more than 90%.
-
Recurrence rate: 9%.
-
Complication rate: 1 to 3%.
Cryothermal ablation is used in atrial tachycardia in vicinity of AV node and in pediatric group.
References
- Chapter 22: Specific arrhythmias: diagnosis and treatment. In: Braunwald Heart Disease: A Textbook of Cardiovascular Medicine. 5th edition. A prism Indian edition (volume 1) 1997:657-58.
- [Google Scholar]
- Ranjith Kumar GK, Ranganatha M, Virupak-shappa V. Study of arrhythmias in acute myocardial infarction. Int J Med Res Rev. 2015;3(07):682-690.
- [Google Scholar]
- ABC of clinical electrocardiography: atrial arrhythmias. BMJ. 2002;324(73/37):594-597.
- [Google Scholar]
- ABC of clinical electrocardiography: atrial arrhythmias. BMJ. 2002;324(73/37):594-597.
- [Google Scholar]
- Chapter 14: Atrial rhythms. In: Chou’s Electrocardiography in Clinical Practice. 6th edition. Saunders Elsevier 2008:349-350.
- [Google Scholar]
- Atrial tachycardia treatment and management. Available at: https://emedicine.medscape.com/article/151456-treatment. Accessed November 16
- Study of arrhythmias in acute myocardial infarction. https://ijmrr.medresearch.in/index.php/ijmrr/article/view/303/592. Accessed July 27.
- [Google Scholar]
- ECG limb lead reversal. Available at: https://litfl.com/ecg-limb-lead-reversal-ecg-library/. Accessed February 7.
- [Google Scholar]
- Use of p wave configuration during atrial tachycardia to predict site of origin. Available at: https://pubmed.ncbi.nlm.nih.gov/7594049. Accessed November 1.
- [Google Scholar]
- Clinical Arrhythmology and Electrophysiology: A Companion to Braunwald Heart Disease. 3rd edition. Elsevier Saunders 2018:214-215.
- [Google Scholar]








