Translate this page into:
Diagnostic Dilemma of Wide Complex QRS Tachycardia after PCI: A Case Report
Sudhakar Kanumuri, DM Student Department of cardiology NIMS, Hyderabad, 500082, Telangana India mrcardio7@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
The authors report a case of a 64-year-old woman who presented with breathlessness on exertion for 6 months, for which coronary angiogram (CAG) was done, which showed single-vessel disease of the left anterior descending coronary artery (LAD). The patient underwent PTCA + DES (percutaneous transluminal coronary angioplasty + drug-eluting stent) to mid LAD. On the third postprocedural day, she complained of palpitations with chest pain. Electrocardiographic monitor showed wide complex QRS tachycardia and she was hemodynamically stable. Further evaluation showed potassium of 2.8 mEq/L, for which intravenous (IV) KCl (potassium chloride) correction was given, and recheck CAG was done, which showed patent stent. Meanwhile, the patient was evaluated for the cause of hypokalemia, and no definite cause was evident.
Keywords
coronary angiography
hypokalemia
wide complex QRS tachycardia
Introduction
Hypokalemia is a common clinical problem and its cause can usually be determined from the history (as with diuretic use, vomiting, or diarrhea). In some cases, however, the cause is not readily apparent. Ventricular arrhythmias are among cardiovascular side effects of hypokalemia. Ventricular tachycardia (VT) is a life-threatening complication, especially in the elderly. It may manifest as hemodynamic stability or hemodynamic instability.
Hemodynamically unstable VT generally requires DC cardioversion for termination, without which immediate death may occur. Hemodynamically stable VT can be managed with chemical cardioversion or correction of electrolyte abnormality. Supraventricular tachycardia (SVT) with aberrancy always comes with a differential diagnosis of VT.1 This case reports broad QRS tachycardia may be due to hypokalemia of unknown cause, which was hemodynamically stable and managed with hypokalemia correction successfully.
Case Report
A 64-year-old female patient was admitted to the intensive coronary care after complaint of breathlessness on exertion for 6 months, with no history of orthopnea, paroxysmal nocturnal dyspnea (PND) attacks, chest pain, palpitations, syncopal attacks, or productive cough. The patient had no history of diarrhea, vomiting, or diuretic usage. There was no history of diabetes, hypertension, previous cardiac or cerebrovascular disease, or thyroid disorders.
On examination, the patient's pulse rate was 98 beats/min, regular, and normal volume; all peripheral pulses were palpable. Blood pressure (BP) was 140/90 mm Hg in the right upper arm in supine position. There were no signs of dehydration. Cardiac, respiratory, and neurologic examination was normal.
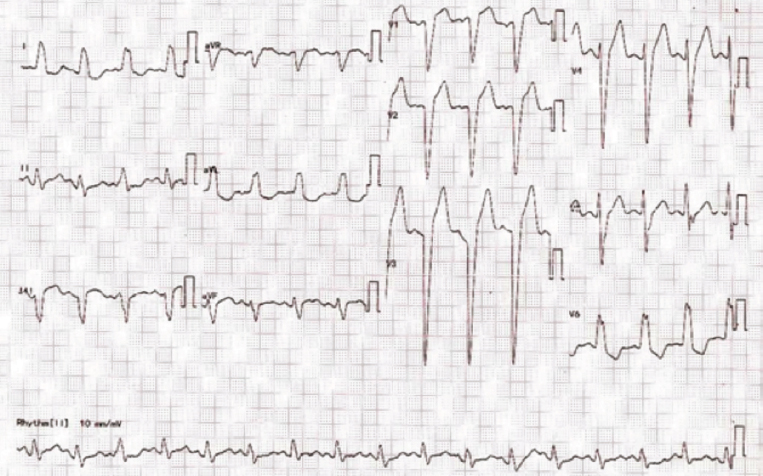
On admission, laboratory results were as follows: hemoglobin 11 g/dL, packed cell volume (PCV) 34%, creatinine 0.8 mg%, potassium 4.6 mmol/L, calcium 9 mg/dL, phosphorus 3.5 mg/dL, and magnesium 1.5 mg/dL. Her cardiac enzymes were within normal limits. Electrocardiogram (ECG) (Fig. 1) was done, which was suggestive of normal sinus rhythm, QS complexes in V1–V3, poor “R” wave progression, with left bundle branch block (LBBB) morphology. Two-dimensional (2D) echo was suggestive of no regional wall motion abnormality (RWMA), good biventricular function with ejection fraction (EF) = 56%, no mitral regurgitation (MR), tricuspid regurgitation (TR), and pulmonary arterial hypertension (PAH).
-
Fig. 1 ECG suggesting normal sinus rhythm, QS complexes in V1–V3, poor “R” wave progression, with LBBB morphology.
Fig. 1 ECG suggesting normal sinus rhythm, QS complexes in V1–V3, poor “R” wave progression, with LBBB morphology.
During the hospital course, the patient underwent coronary angiogram (CAG), which was suggestive of single-vessel disease (SAD) involving the mid left anterior descending coronary artery (LAD), for which PTCA + DES (percutaneous transluminal coronary angioplasty + drug-eluting stent) stenting was done
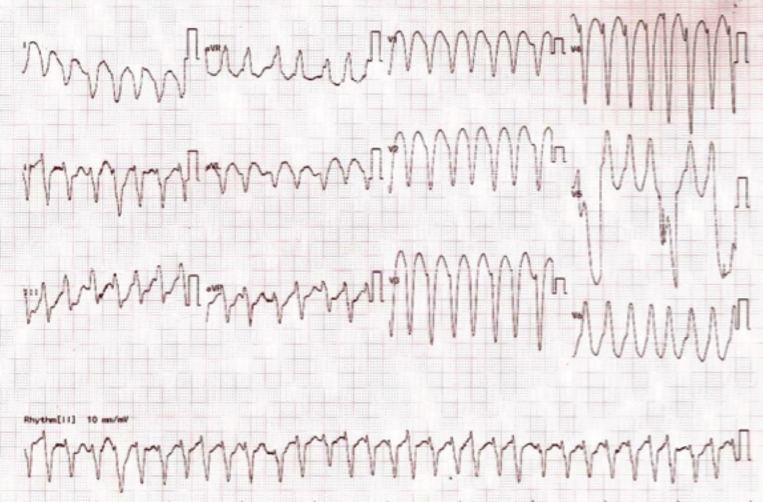
On postprocedural day 3, the patient complained of palpitations. She was hemodynamically stable, and ECG (Fig. 2) was suggestive of monomorphic VT versus SVT with aberrancy. The indications for VT are broad QRS complex tachycardia in an elderly woman, with the history of coronary heart disease with the change in axis (aVR positive) and AV dissociation. The monitor also showed signs of broad QRS tachycardia, with the heart rate of 168 beats/min, and BP was 120/80 mm Hg. Immediately inj. amiodarone 150 mg IV stat was given.
-
Fig. 2 Broad QRS tachycardia on 9.02 AM.
Fig. 2 Broad QRS tachycardia on 9.02 AM.
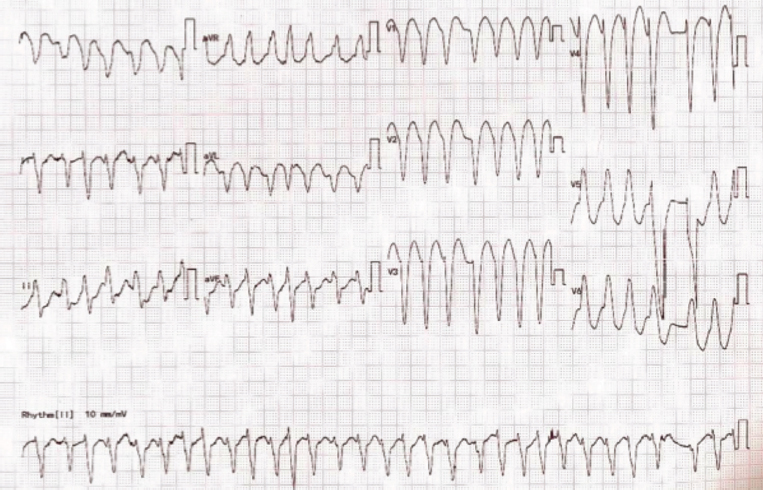
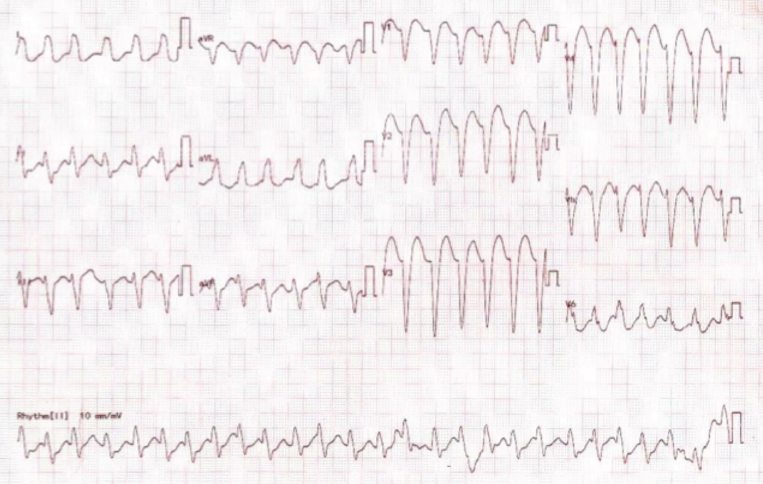
If we compare the ECG for Figs. 2 and 3 with Fig. 4 ECG, two tachycardia ECG morphologies were different with aVR negative in Fig. 4 ECG. Except for some sort of AV dissociation, the morphologic criterion pointed toward SVT with aberrancy. Fig. 5 with increased magnification from Fig. 4, showed the minor irregularity.
-
Fig. 3 The same type of wide QRS tachycardia was persisting latter.
Fig. 3 The same type of wide QRS tachycardia was persisting latter.
-
Fig. 4 ECG after 4 minutes.
Fig. 4 ECG after 4 minutes.

-
Fig. 5 Minor RR irregularity.
Fig. 5 Minor RR irregularity.
After IV amiodarone, the patient was converted to sinus rhythm. She also underwent recheck angiogram, which was suggestive of patent mid-LAD stent. Evaluation for cause of broad QRS tachycardia was initiated, and relevant investigations were done. Arterial blood gas (ABG) was suggestive of hypokalemia (k+: 2.8 mmol/L) with normal acid-base balance, and other electrolytes were within normal range. The patient was started on IV potassium correction at the rate of 10 mEq/h correction with 0.9% normal saline. Approximately 250 mEq/d of potassium replacement was required to maintain serum potassium of 4.5 mmol/L. Again, the patient had broad QRS tachycardia after 24 hours with the similar morphology of Fig. 2. By that time, the patient had received the full dose of amiodarone (bolus followed by infusion). Again, hypokalemia was documented. Then only IV correction of potassium was done without any other antiarrhythmic drugs.
Recurrence of VT with hypokalemia occurred on day 3 also. Therefore, we further investigated for causes of hypokalemia. Evaluation of hypokalemia included ABG analysis, Serum electrolytes: calcium, magnesium, 24-hour urinary potassium, thyroid profile, serum cortisol, serum aldosterone, and all of them came to be normal. Therefore, the definite cause for hypokalemia was not evident in this case.
The patient required 250 mEq of potassium (IV) for 4 days. When serum potassium was maintained constantly above 4 mmol/L, without oral or IV supplementation, the patient had no further episodes of VT. The patient discharged in stable condition, with anti-PCI measures. In 6-month follow-up, the patient did not have any episodes of palpitation. Even Holter monitoring was uneventful.
Discussion
Hypokalemia may cause serious life-threatening complications. It can increase both the duration of the action potential and refractory period with increased automaticity that can trigger and can cause reentry leads to arrhythmias. The clinical manifestations of hypokalemia usually start when serum concentrations decrease 2.5 mEq/L. Ventricular arrhythmias are among cardiovascular side effects of hypokalemia. The elderly and the patients with underlying ischemic heart disease appear to have the highest risk for hypokalemiarelated complications.2 We experienced one of the most serious complications of hypokalemia with a potassium level of 2.8 mEq/L, and the cause of hypokalemia was not evident, even after detailed evaluation.
Clinically the patient was evaluated for gastrointestinal (GI) losses3 and diuretic usage, which can lead to hypokalemia, thereby ventricular arrhythmias. However, the patient had no such history.
Usually, thyroid disorders are common in females, so we evaluated for thyrotoxicosis causing ventricular arrhythmias,4 but the patient was found to have normal thyroid function tests.
Hypokalemia secondary to aldosteronism and other renal causes is also evaluated in our case, as they may increase the risk of ventricular arrhythmias.5
Possible pathogenesis of proarrhythmic effects of hypokalemia upon ventricular muscle may be (1) prolonged ventricular repolarization, (2) slowed ventricular conduction, and (3) abnormal ventricular automaticity.1 Hypokalemia can be an important precipitant of arrhythmia in a patient with additional genetic or acquired causes of QT prolongation.6
However, in our case, it was not pure VT. There were features suggestive of SVT with aberrancy (underlying LBBB). If it were to be SVT with aberrancy, hypokalemia precipitating this condition cannot be explained.7 That is why we preferred to treat this condition as VT.
Conclusion
In any case of broad QRS tachycardia, we have to suspect VT especially if the patient had a history of CAD, elderly age, with hypokalemia as it increases refractory period, and reentry tachycardias. If managed in right time, VT can be successfully terminated, recurrences can be prevented, and untoward life-threatening complications can be avoided, even though the cause of electrolyte disturbance may not be evident in some cases.
Conflict of Interest
None.
References
- Ventricular tachycardia as default diagnosis in broad complex tachycardia. Lancet. 1994;343:386-388. 8894
- [Google Scholar]
- Mechanisms of hypokalemia-induced ventricular arrhythmogenicity. Fundam Clin Pharmacol. 2010;24(05):547-559.
- [Google Scholar]
- Diarrhoea-related hypokalemia induced ventricular arrhythmia in a healthy elderly patient. N Engl J Med. 2004;31:135-136.
- [Google Scholar]
- Thyrotoxic periodic paralysis complicated by near-fatal ventricular arrhythmias. Singapore Med J. 2005;46(02):88-89.
- [Google Scholar]
- Association of hypokalemia, aldosteronism, and renal cysts. N Engl J Med. 1990;322(06):345-351.
- [Google Scholar]
- In: Fluid and electrolyte balance. In: Harrison's Principles of Internal Medicine (19th ed.). New York, NY: McGraw-Hill; 2015. p. :304-306. chap 63
- [Google Scholar]
- Serum potassium and the electrocardiogram and hypokalemia. Circulation. 1973;47:408-418.
- [Google Scholar]







