Translate this page into:
Coronary Bifurcation Lesion–Management
Maddury Jyotsna, MD DM FACC FESC FICC Nizam Institute of Medical Sciences (NIMS) Punjagutta, Hyderabad, Telangana 500082 India janaswamyjyostna@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Coronary bifurcation lesion management is challenging even in this modern era of drug-eluting stents (DES). A debate always exists as to what mode of treatment is better–one-stent or two-stent strategy. As in hospital and major adverse cardiac events (MACE) are more in the follow-up, what improvements in management strategy are required in relation to bifurcation lesions? We have more questions than answers for this type of lesion. In this article, we try to analyze these issues.
Keywords
bifurcation
percutaneous coronary intervention
culotte
proximal optimization
angles
Introduction
Bifurcation lesions constitute nearly one-fourth of all the percutaneous coronary interventions (PCIs).1 Coronary bifurcation stenting, even in the present era of new devices and drug-eluting stents (DES), is still a difficult procedure, due to the complexity of anatomy along with dynamic changes that occur during PCI along with the high-risk of stent thrombosis and restenosis.2 3 Provisional approach (one-stent technique) is a simple and better treatment modality,4 especially for non-left main coronary artery (LMCA) bifurcations lesions, when compared with the elective two-stent technique.5 In addition, provisional stenting is associated with lesser incidence of periprocedural myocardial infarction (MI),6 which make it the standard strategy of coronary bifurcation stenting.7
Basics of Coronary Bifurcation
The coronary arterial tree has a pseudofractal geometry.
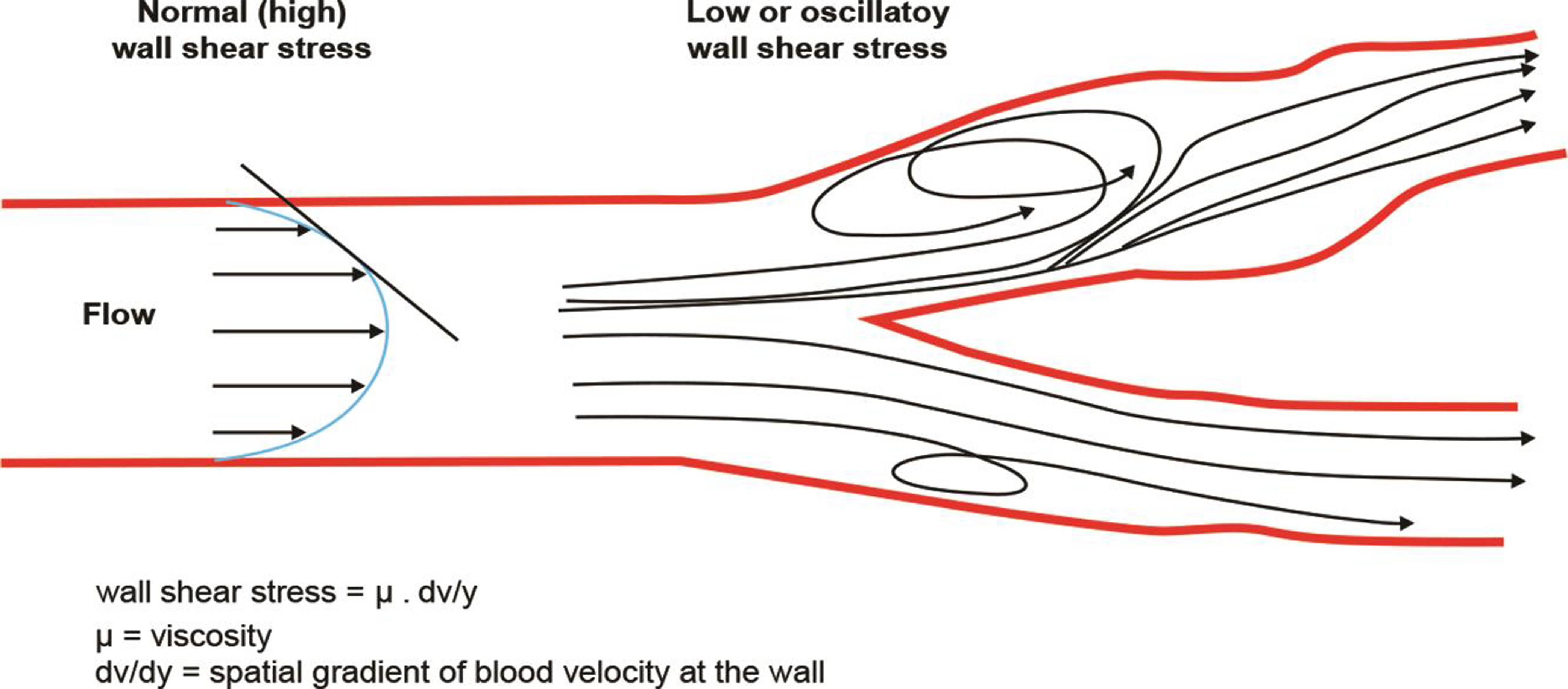
Blood flow is slow with less endothelial shear stress along the lateral walls of main vessel (MV) and side branch (SB), whereas at carina, the shear stress is high (Fig. 1). That is the reason why atheromatous plaque develops more frequently opposite to carina but not at carina.8
-
Fig. 1 Blood flow is depicted at bifurcation site.
Fig. 1 Blood flow is depicted at bifurcation site.
We can calculate the wall shear stress (WSS), WSS gradient and turbulent index in bifurcation lesions with fluid dynamic mechanism.9
Definition and Classification
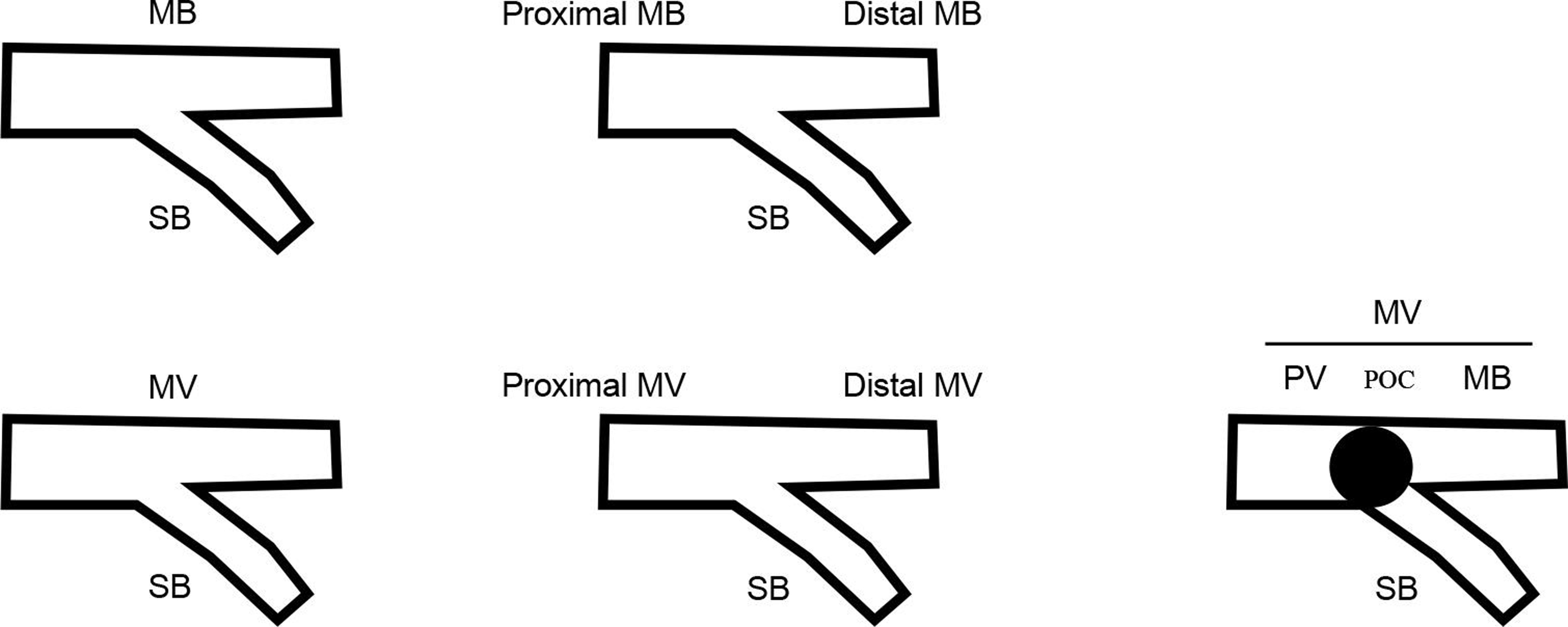
At the division of major arteries, the bifurcation lesions occur. The three main stems of bifurcation lesion are proximal and distal MVs and SB. According to the European Bifurcation Club, a bifurcation lesion is “a coronary artery narrowing occurring adjacent to, and/or involving, the origin of a significant side branch.” In a bifurcation lesion, any arm with > 50% lesion is considered as significant. The two arms of the bifurcation lesion are MV or main branch (MB) and side branch (SB) and polygon of confluence (POC). MV or MB has two components, proximal MB (parent vessel–PV) and distal MB (Fig. 2).
-
Fig. 2 Nomenclature of the arms of bifurcation lesion.
Fig. 2 Nomenclature of the arms of bifurcation lesion.
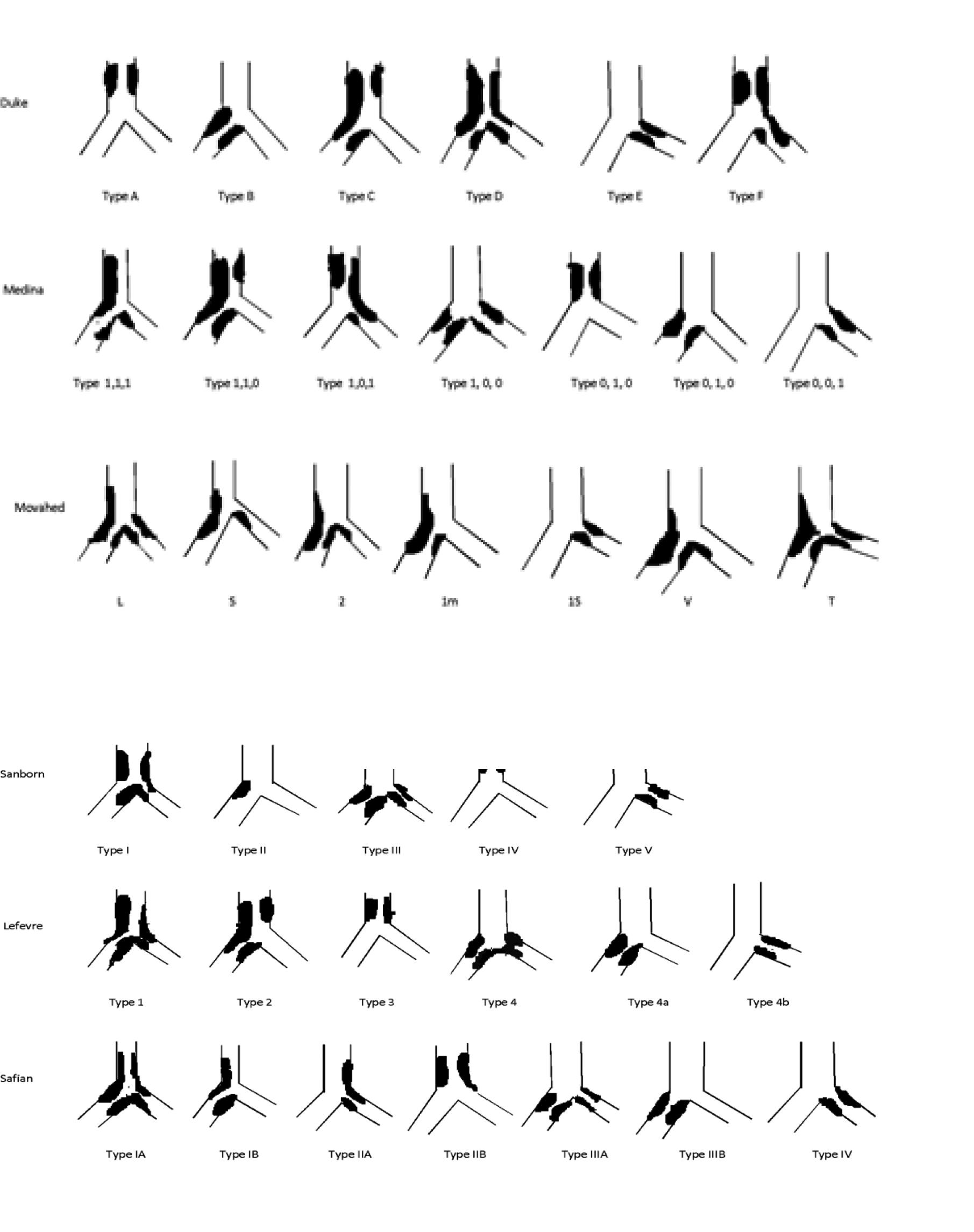
There are multiple bifurcation lesion classifications available.
-
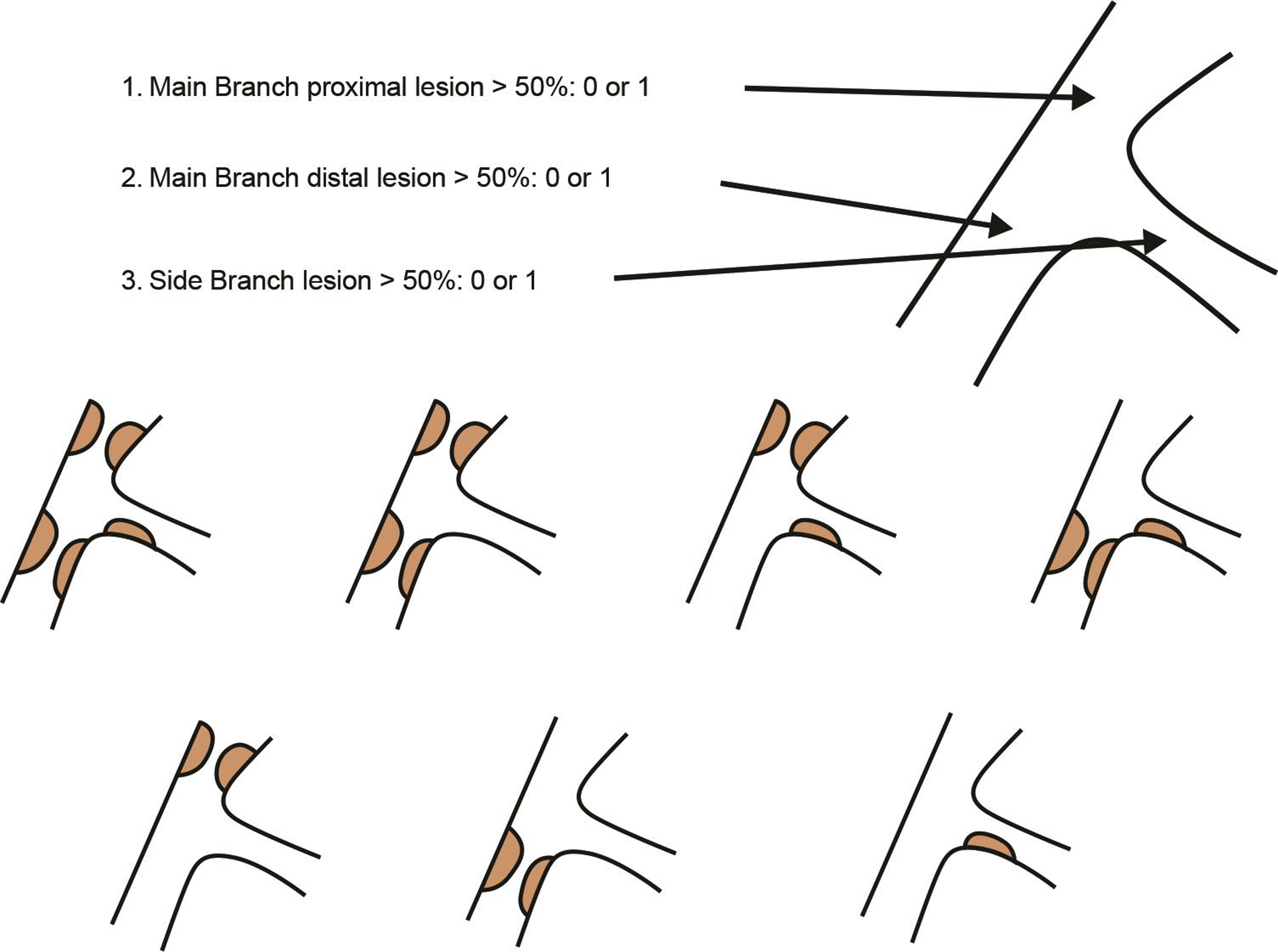
Medina Classification–This system10 11 assesses the plaque burden either present (1) or absent (0) in the three arms of bifurcation (Fig. 3). For example, if there is 60% lesion in proximal MV and 70% in SB without lesion in distal MV, then this bifurcation lesion will be represented as 1,0,1. This Medina classification is useful in representing true versus pseudo bifurcation, which is more reliable on intravascular ultrasound (IVUS) assessment of plaque or by fractional flow reserve (FFR).12
-
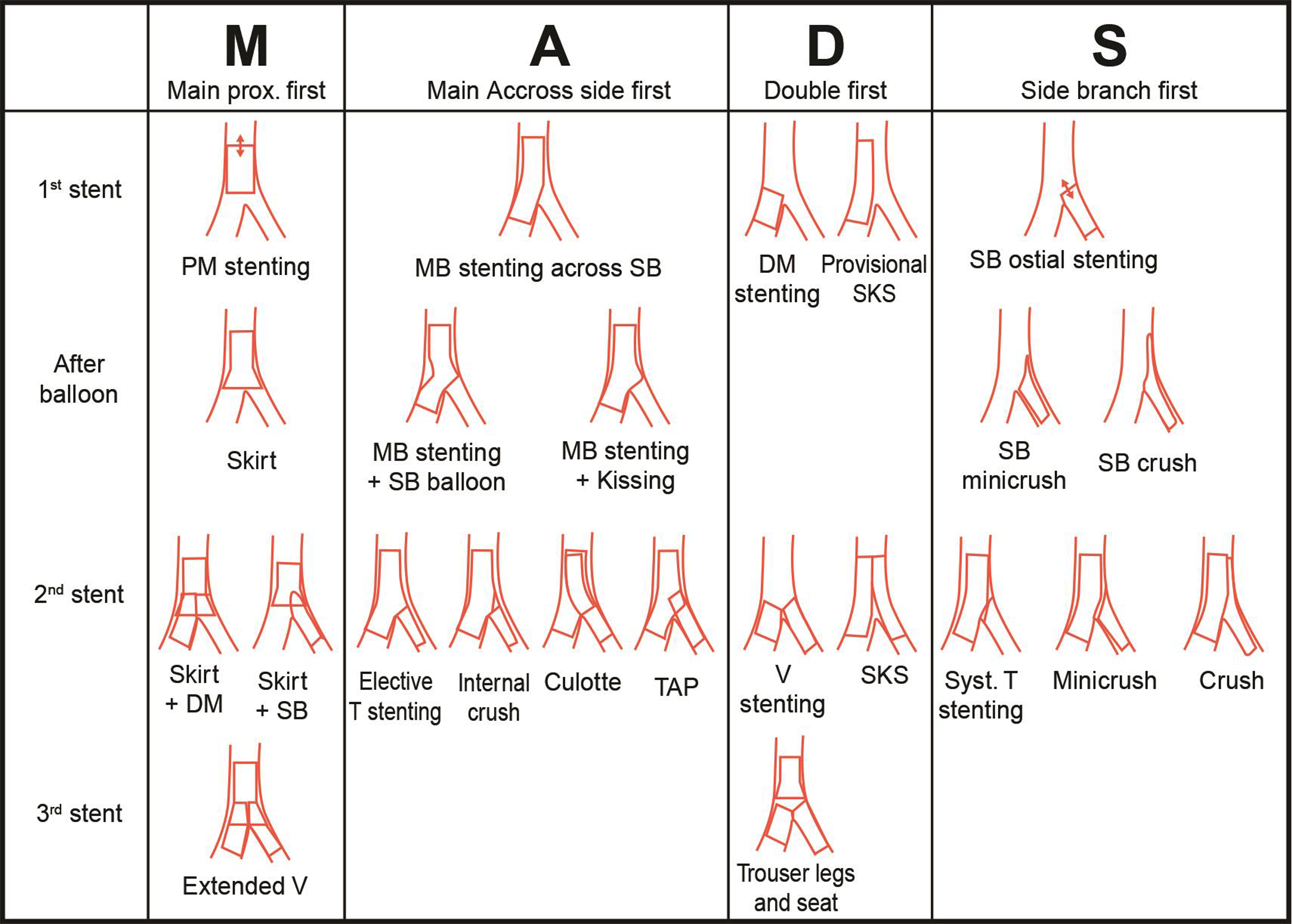
MADS Classification–The MADS (main, across, distal, side) classification mainly depends on the final position of the stent in different bifurcation technologies. M for proximal main, A for across, D for double, S for side branch (Fig. 4).
-
Movahed Coronary Bifurcation Lesion Classification–It has five components.
-
Prefix is B, which means bifurcation lesion.
-
Suffix 1–C = close to bifurcation, N = nonsignificant SB, S = small proximal segment, L=large proximal segment.
-
Suffix 2–1M = only MB ostium is diseased, 1S = only SB ostium diseased, 2=both main and side branch ostia are diseased.
-
Suffix 3–V = angle between branch vessels < 70 degree, T = angle between branch vessels > 70 degree.
-
Suffix 4–CA = calcified, LM = left main bifurcation.
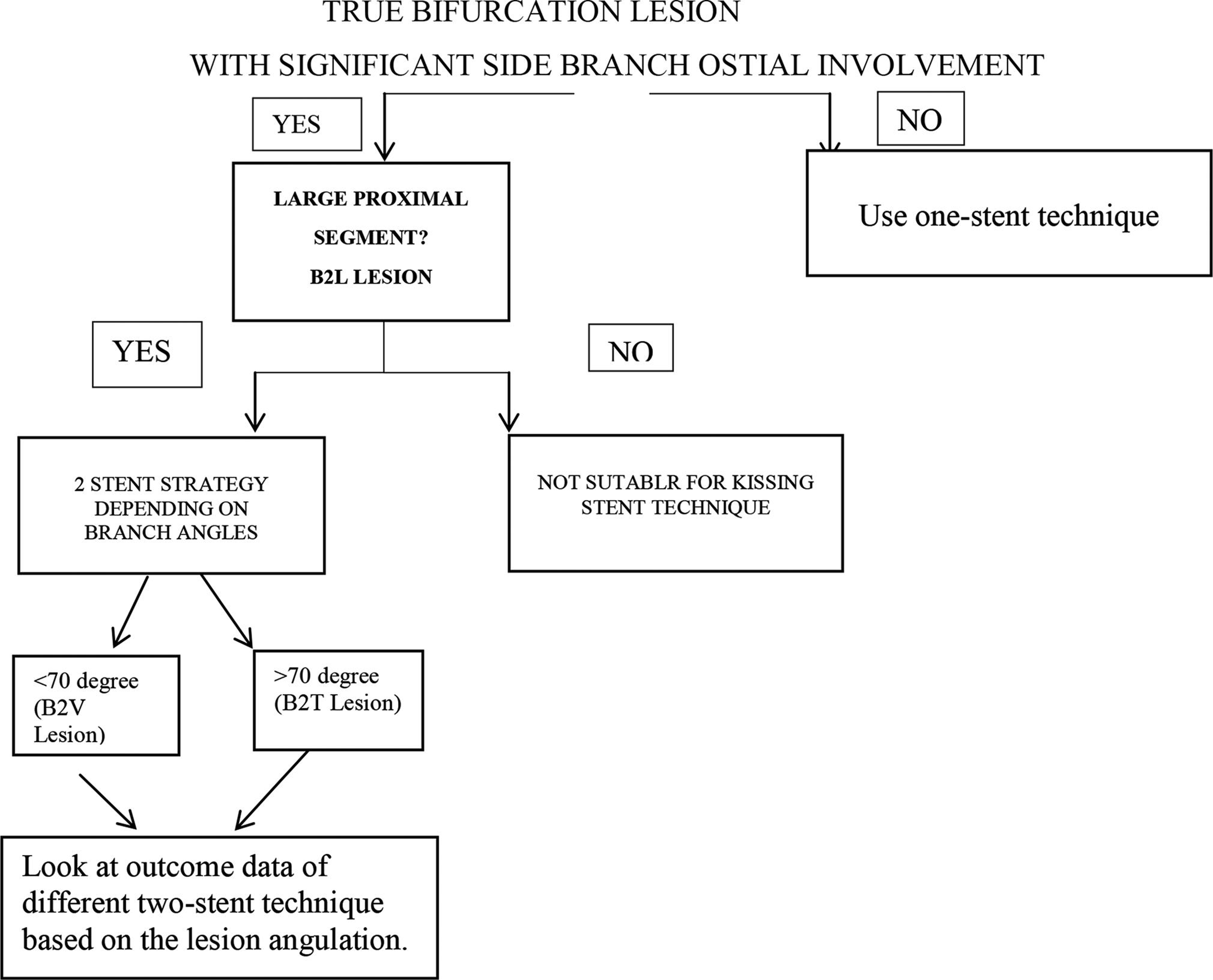
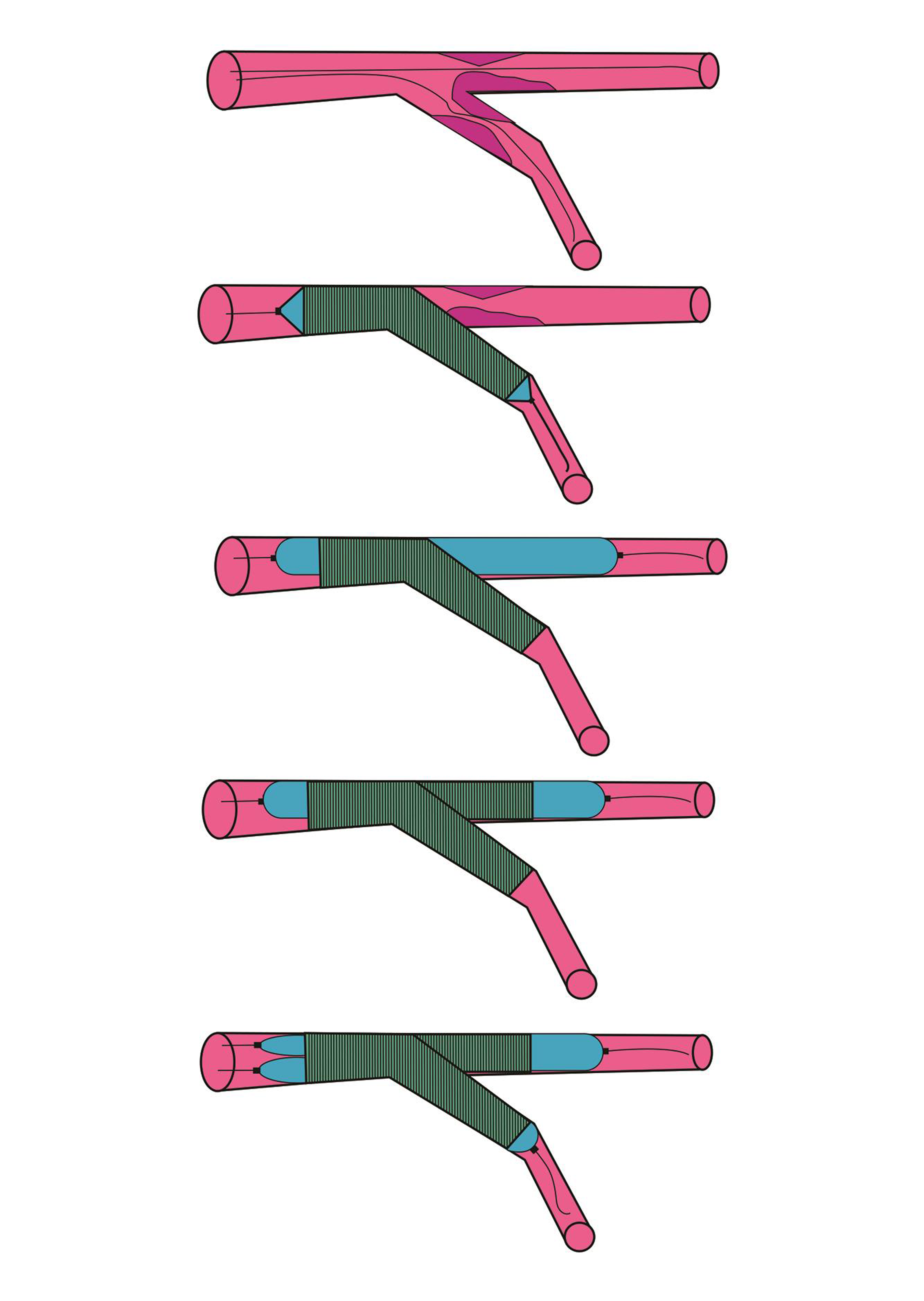
Depending on this classification, even treatment algorithm was proposed (Fig. 5).
-
-
Combined Classification of Coronary Bifurcation Lesions–This was proposed by Thomas Papadopoulos, wherein the size of the vessels and the angulation between them were also included. In this system, he uses the uppercase letters P (proximal), D (distal), S (side branch), and lowercase letters p, d, s, on top of the binary system along with SB angulations (=, <, >, of 70 degrees) and complexity of lesions (C = calcification, T = thrombus, LM = left main). In Fig. 6, comparison of major bifurcation classifications is mentioned.
-
Fig. 3 Graphical representation of Medina classification.12
Fig. 3 Graphical representation of Medina classification.12
-
Fig. 4 MADS classification of bifurcation lesions. Abbreviation: MADS, main, across, distal, side.
Fig. 4 MADS classification of bifurcation lesions. Abbreviation: MADS, main, across, distal, side.
-
Fig. 5 Treatment strategy depending on Movahed classification.
Fig. 5 Treatment strategy depending on Movahed classification.
-
Fig. 6 Comparison of major bifurcation classifications.
Fig. 6 Comparison of major bifurcation classifications.
Procedure of Doing PCI for Bifurcation Lesions
The main aim of successful percutaneous coronary intervention (PCI) of bifurcation lesion is to achieve optimal result on the MV as well as on the SB.13
The steps in PCI of bifurcation lesion producer depend on
a) Bifurcation site–non-LMCA or LMCA bifurcation.
b) Plaque location.14
c) Plaque burden and morphology.
d) Bifurcation angle between MB and SB.
e) Vessel diameter.
In addition to these, the problems specific to bifurcation are
-
Bifurcation anatomy is dynamic and changes during PCI due to plaque or carina shift.
-
Bifurcation angle change.
-
Vessel spasm.
-
Coronary dissection, especially of SB after balloon dilatation.
PCI is mainly done with
-
One-stent approach.
-
Two-stent approach.
Even though provisional one-stent approach is the time-tested methodology, but it is important to remember that 30% of non-LMCA and 50% of LMCA bifurcations require second stent.15
Route of PCI–It can be either radial or femoral, depending on operator’s discretion. If > 6F guide catheter is required, the femoral route is better.
Guide catheter selection–Depends one-stent or two-stent strategy and need for SB stenting; through 6F guide, two stents can be delivered only sequentially.
Guide wire–Bending a wire for SB access requires taking into account the geometry of the MV, angulation of the SB, space for rotation of the wire, distribution of plaque, and presence of a stent. The most difficult branch is wired first. The second branch wire passed with rotatory moments to prevent crisscross.
The advantages of SB wiring initially itself are
-
The wire itself opens the bifurcation angle. Acute bifurcation angle is one of the predictors of SB compromise.
-
It facilitates better flow to the SB.
-
In case of SB compromise after MV stenting, guides for SB rewiring through stent struts after MV wiring.
Methods for SB Wiring
-
For SB wiring, the shape of the tip of the wire should have single bend for Y-shaped and double bend for T-shaped bifurcation. It is better to avoid hydrophilic or polymer tip coating for primary SB wire due to the risk of wire rupture. The shape of the two wires must be adapted to their secondary use if a “wire swap” or recross is needed.
-
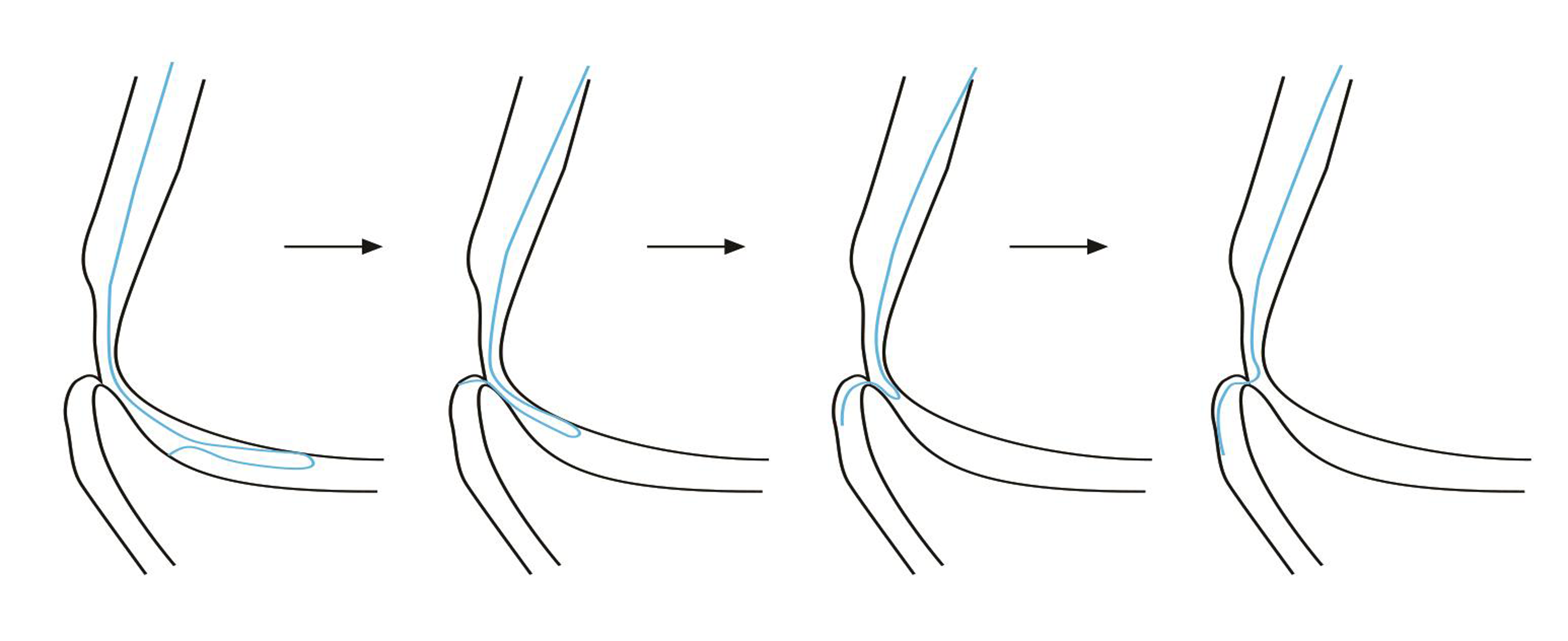
For extreme-angled bifurcations, reverse wire technique is useful (Fig. 7).
-
In some cases, supercross microcatheter is useful.
-
Occasionally, plaque modification by dilatation of undersized balloon proximal to carina or rotational atherectomy may be useful.
-
In cases where direct access is not possible, the wire needs to be bent to reach the contralateral wall as hinge point, in order to direct the tip of the wire into the ostium of the SB. The distal tip of the wire is then usually pushed forward in a rotational movement to reduce the risk of wire prolapse into the MV. This technique to access a SB is supported by either a double-bend or by a long, progressive curve at the tip of the wire.
-
After entering the ostium, the forward push is usually accompanied by a slight rotation to avoid a prolapse of the wire into the distal MB. In case the wire continues to prolapse into the distal MB, it can be considered to block the distal vessel with a balloon at low pressure.
-
Fig. 7 Schematic diagram demonstrating the method of SB wiring with reverse loop technique. Abbreviation: SB, side branch.
Fig. 7 Schematic diagram demonstrating the method of SB wiring with reverse loop technique. Abbreviation: SB, side branch.
A) Provisional one-stent approach 4 16
I). SB preservation depends on multiple factors
a). Vessel size
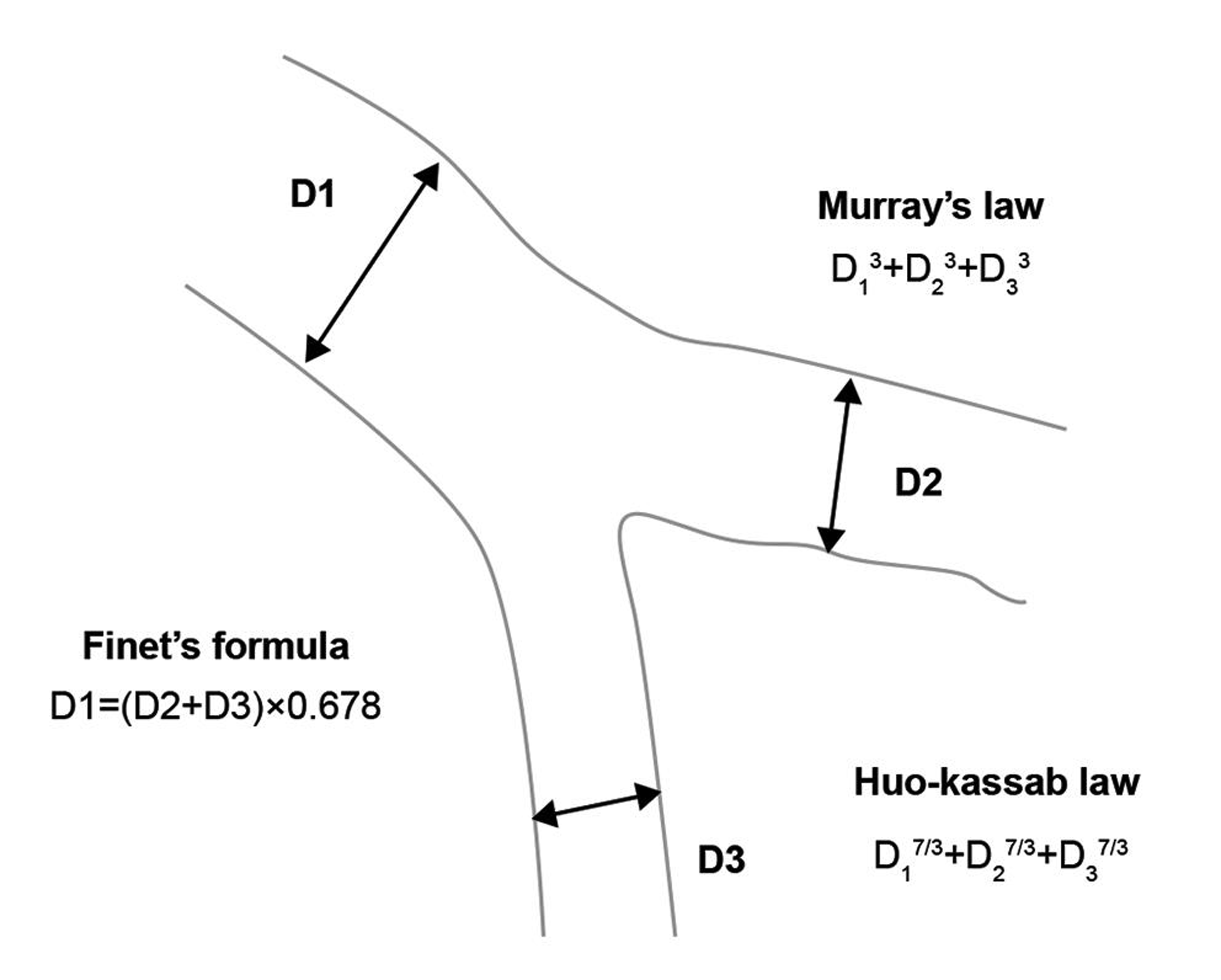
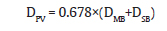
The most important concept to understand a bifurcation lesion is the relationship between the sizes of these vessels (Fig. 8).
-
Fig. 8 Depicting the three different laws depending on size of D1 (diameter of proximal main vessel), D2 (diameter of distal main vessel), and D3 (diameter of SB). Abbreviation: SB, side branch.
Fig. 8 Depicting the three different laws depending on size of D1 (diameter of proximal main vessel), D2 (diameter of distal main vessel), and D3 (diameter of SB). Abbreviation: SB, side branch.
Murray’s Law
According to Murray’s law
D1 3 = D2 3+D3 3, whereas D1 = diameter of proximal MV, D2 = diameter of distal MV and D3= diameter of the SB.17 This law is applicable in normal and diseased bifurcations, which was proved by the IVUS study.18 But this law is not applicable in calcific lesions and in situations like acute coronary syndrome (ACS). In these two conditions, the size of the vessel is to be assessed by IVUS.
We take precautions in two conditions when we are applying this law
-
As the size of the SB increases, there is more discrepancy between the proximal MV and distal MV, which needs proximal optimization technique (POT) to correct the discrepancy.19
-
According to this law, in kissing balloon technique, the cross-sectional area of both balloons together is larger than the cross-sectional area of the proximal MV. So, to prevent injury to the proximal MV, moderate pressure inflation of two balloons is better.20
Finet’s Law
This law is derived from the angiograms of normal bifurcation by quantitative analysis.21
So, it is better to assess the size of the vessels by IVUS, than derive value from these laws.15
Huo–Kassab Law
According to this combiner, 7/3 power of D2 and D3 is equivalent to 7/3 power of D1.
b). Methods to prevent SB occlusion
The definition of SB occlusion is angiographical decrease in thrombolysis in myocardial infarction (TIMI) grade or absence of flow in SB immediately after full-expansion of MV stenting. The SB compromise was associated with the increased risk of periprocedural cardiac mortality and MI,22 even though the peri-procedural MI, was not associated with long-term adverse outcomes.23 Deepti et al demonstrated importance of proximal angle in addition to bifurcation angle, as the coronary artery is an three-dimensional structure. So, proximal angle is not just 180°minus the bifurcation angle.24
The predictors of SB occlusion25 are
-
SB ostial disease and lesion length.
-
PV stenosis.
-
ACS.
-
Nonleft main disease.
-
B2 lesions.
Whereas jailed wire technique, SB predilatation, and IVUS guidance were not predictors for SB occlusion.
Visual estimation for risk prediction of side branch occlusion in coronary bifurcation intervention (V-RESOLVE) is the scoring system to predict the chances of SB occlusion. If this score is > 12, then there is high-risk of SB occlusion (Table 1).
|
Risk Factor |
Level |
Point |
|---|---|---|
|
Abbreviations: MV, main vessel; RESOLVE, risk prediction of side branch occlusion in coronary bifurcation intervention; SB, side branch; TIMI; thrombolysis in myocardial infarction |
||
|
Plaque distribution |
At the opposite side of SB At the same side of SB |
0 1 |
|
MV TIMI flow grade before stenting |
TIMI 3 TIMI 2 TIMI 1 TIMI 0 |
0 6 11 17 |
|
Preprocedural diameter stenosis of bifurcation core (%) |
< 50 50–< 70 ≥70 |
0 2 3 |
|
Bifurcation angle (°) |
<70 70–< 90 ≥90 |
0 4 6 |
|
Diameter ratio between MV/SB |
<1.0 1.0–< 1.5 1.5–< 2.0 ≥2.0 |
0 2 6 9 |
|
Diameter stenosis of SB before MV stenting (%) |
<50 50–< 70 70–< 90 ≥90 |
0 4 6 7 |
The IVUS study gives information about plaque shift in POT and carinal shift in in MB stent expansion. So, it is better to do proximal and distal optimization in bifurcation lesions.26
Conventional versus intentional strategy in lesions with high risk prediction of side branch occlusion in intervention (CIT-RESOLVE), a randomized trial, showed that of SB protection strategy (if SB ≥ 2.5 mm: elective two-stent or SB reference vessel diameter [RVD] < 2.5 mm: jailed balloon technique) is superior in SB occlusion prevention; in turn, periprocedural MI development is better than conventional strategy (SB RVD ≥ 2.5 mm: provisional stenting and if SB RVD < 2.5 mm: jailed wire technique) in patients with coronary bifurcations and high predicted risk of SB occlusion by RESOLVE score.
II) Predilation of SB
Predilation of SB is a controversy. Routine predilation of SB is not advisable. This has to be preserved to high-risk lesions like tight ostial lesion, very calcified SB or difficult to access. Precautions need to be taken to not dissect the SB ostium which experiences more difficult in rewiring.27
III) MV stenting and optimization technique
The large the size of SB, the larger the discrepancy of PV and MB vessel size. The steps in MV stenting are
-
Method to select the size of the stent–MV stenting is the selection of stent with optimal size to distal vessel diameter by IVUS (distal optimization). If stent larger than the proximal MV size is taken, then two disadvantages could materialize. One, distal edge dissection and risk of carinal shifting. Another important point to be consider during the selection of the stent is that the proximal MV stent should accommodate the effective balloon size of the both the branches, in order to prevent the stent fracture. When the distal reference vessel is diseased, then select the stent, depending on the average of lumen and vessel diameters. It is better to take smaller size stent as calcium is there in the reference segment to prevent distal stent edge dissection.
-
Proximal optimization technique (POT)–POT is essential to bring back the normal physiologic anatomy of the bifurcation. POT facilitates to reduce risk of abluminal wiring. This decreases the number of struts across the ostium of SB; the present strut will expand well and approximate the proximal stent portion to the vessel wall at the ostium. POT is postdilating the MV stent just proximal to the carina, with a short noncompliant (NC) balloon sized for the reference diameter of PV. The shoulder of the balloon is more important than the marker. The shoulder is against the SB ostium. So, MV stent has to deployed at least 6 to 8 mm proximal to SB to have good result after POT. POT causes the opening of the strut into the SB and facilitates the rewiring of SB.
The purpose of the POT is
Even though many studies insists on doing POT regularly, prospective randomized study to evaluate proximal optimization technique in coronary bifurcation lesions (PROPOT)30 study showed that there is no benefit of POT as the PV is fully expanded by two balloons used for kissing technique. This study involves zotarolimus stent for bifurcation lesion, and optical coherence tomography (OCT) in POT and non-POT group showed no superiority of POT over kissing balloon dilatation (KBD) for stent apposition.
Plaque Shift and Carina Shift31
Pathological32 and IVUS33 studies demonstrated that there is more plaque at lateral wall than carina. Scanty plaque at carina is less likely to cause the plaque shift when SB is compromised. In this case, the SB compromise is due to carinal shift. But ACS and significant proximal MV diseases in COBIS II4 trial showed that the SB compromise is due to plaque shift. Other papers34 supported the carinal shift accounts for 85% of cases. According to this article, the degree of carina shift depends on the cosine of bifurcation angle. So, more carinal shifts occur in narrow bifurcation angle. FFR is significant in plaque shift cases, but not in carinal shift cases.35 Most of the time, the carinal shift is short and eccentric and may look an angiographically more significant lesion because of two reasons. One, negative shadow of MV stent across SB ostium. Two, the oval configuration of the SB ostium. This is the explanation as to why there is discrepancy many times between the angiographic pinching of SB and functional assessment by FFR.36
IV) SB ballooning–stent balloon technique
SB dilatation is required to open up the jailed ostium of SB from the stent struts of MV.
SB access after MV stenting–Rewiring of SB is difficult after stenting as the access plan is changed. The access plan becomes parallel to the MV, but not perpendicular to the SB. Either the wire in the distal MV or, leaving the jailed wire, third wire can be used to rewire the SB. Precautions need to be taken to prevent the guide movement deep into coronary (may produce dissection), which removes the jailed wire. Tip curvature to be reshaped according to the new carina shape. Better to recross through the stent strut close to the carina than proximal. Proximal recrossing causes the pushing of struts inward toward the MV lumen, whereas distal crossing causes better scaffolding of the ostium of SB. POT of MV stent is mandatory to facilitate SB access.
Methods to Recross of SB
-
Pull back technique–Angulated wire already in MV is pulled back to engage the ostium of SB.
-
Third wire–Hydrophilic or polymer tip coating wires (Hi-Torque whisper or PT2 or Hi-Torque Pilot 50 & 150 wires) or hydrophilic with good torque like Fielder FC, Fielder XT, and Sion may be preferred for the rewiring of SB after stenting.
-
Plaque modification–by POT.
-
Either Super Cross micro catheter or Venture Wire control catheter is helpful in difficult cases.
-
Use of a second buddy wire, guideline catheter (Vascular Solutions), or a low-profile 1.25 mm balloon can be helpful to recross SB through the MB stent struts.
-
Reverse wire technique.
-
Use of double lumen catheter.
-
Inverted crush technique–On jailed wire, bigger size balloon is passed and dilatated to crush the MV stent which is protected with a wire. Then, another stent is implanted from proximal MV to SB, followed by FKB dilatation.
-
Jailed balloon technique (JBT)–Complete SB occlusion following MV stenting as a last resort jailed balloon technique (JBT) can be used.37 In conventional jailed balloon technique, uninflated balloon is left at the carina, extending into the SB, while the MV stent is deployed. This balloon facilitates in decreasing the plaque or carinal shift. If there is no compromise of the SB, then the uninflated balloon in SB is removed. If SB compromise occurs, then the uninflated balloon guides recrossing the SB, as it alters the carinal angle in favor of crossing, or if rewiring could not be done then to dilate to establish flow in the SB, followed by MV stent balloon dilatation. In modified jailed balloon technique, the SB balloon is inflated, keeping just at the ostium without protruding into the MV, so that MV stent deformation does not occur.Then, both the MV stent balloon and SB balloon need to be inflated.
Sometimes, balloons may not be possible to advance over the recrossed wire. The reasons are
-
Wire wrap–This is suspected when the MB wire is seen retracting back while pushing the SB balloon.
-
Poor support.
-
Extreme angulation.
-
Incorrect SB wire positioning.
Advancement into the SB can be facilitated by
-
Use of the lowest profile balloon (0.8 mm and 1.25 mm).
-
The anchoring balloon technique with inflation of a balloon to nominal pressure in the distal stented MB, which will improve catheter support and allow crossing of the balloon into the SB.
-
Re-POT at higher pressure or with a larger balloon to increase strut size at SB.
-
Rewiring the MB to correct wire wrap, which is sometimes required.
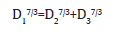
V) Final kissing ballooning (FKB)38
For kiss, short NC balloon to be used for SB with minimal overlap and MV balloon (Fig. 9). Importantly, for POT and kiss, balloon should not be pushed if there is resistance. If there is significant resistance, then see where wire wrap occurred; if not, then better to recross the SB more distally. In case of proximal crossing of the stent strut at carina into SB, then wire may go underneath the SB stent and enter into the proximal SB. This causes the distortion of the SB stent and uncovered stent at the ostium, more so if it is a dilated balloon. Angiographically it may look good, but OCT will demonstrate this deformity, which requires another stent to the SB with internal crushing. OCT is advisable whenever there is problem in crossing the balloon after SB wiring, in order to know the position of the wire and also to direct the wire to the proper position.
-
Fig. 9 Steps in FKB (POT and DOT). Abbreviations: DOT, distal optimization; FKB, final kissing ballooning; POT, proximal optimization.
Fig. 9 Steps in FKB (POT and DOT). Abbreviations: DOT, distal optimization; FKB, final kissing ballooning; POT, proximal optimization.
In general, final KBD for bifurcation lesion is required, but its routine use in provisional stenting is not proved (Table 2). The concern in this KBD is the MV stent deformation produced by SB dilatation is not perfectly corrected by the KBD. The results of the KBD depend on how it was performed. Ideally, SB has to be dilated with short NC balloon. NC is recommended to prevent the dissection of the nonstented SB segment and short balloon, to prevent the oval distortion of MV stent. Inflation in the SB with simultaneous deflation of both balloons is important to avoid distortion of the MV stent.
|
Trial name |
KBI |
Non-KBI |
Follow-up (months) |
MACE KBI versus non-KBI |
p value |
TVR KBI versus non-KBI |
p value |
|---|---|---|---|---|---|---|---|
|
Abbreviations: KBI, kissing balloon inflation; MACE, major adverse cardiac event(s); TVR, target vessel vascularization. |
|||||||
|
Nordic III |
238 |
239 |
6 |
2.1% vs. 2.5% |
NS |
1.3% vs. 1.7% |
NS |
|
COBIS I |
736 |
329 |
22 |
10.0 vs. 4.9%% |
<0.05 |
9.1% vs. 3.4%% |
<0.05 |
|
COBIS II |
620 |
1,281 |
36 |
6.8% vs. 8.6% |
0.048 |
5.8% vs. 6.6% |
NS |
|
CORPAL Kiss |
124 |
120 |
12 |
9% vs. 6% |
NS |
4% vs. 1.7% |
NS |
|
SMART-STRATEGY |
130 |
128 |
36 |
20.8% vs. 11.7% |
0.049 |
16.2% vs. 10.9% |
NS |
Footnotes: COBIS = Korean Coronary Bifurcation Stenting; CORPAL Kiss = Cordoba & Las Palmas Kiss; KBI = kissing balloon inflation; MACE = major adverse cardiac event(s); NS = nonsignificant; SMART-STRATEGY = Smart Angioplasty Research team-Optimal STRATEGY for Side Branch Intervention in Coronary Bifurcation Lesions; TVR = target vessel revascularization.
Modified KBI approach–This method is proposed by Foin et al.38 Proximal stent deformation occurs when long balloon is used in MV in KBI. To decrease this deformation, first SB is dilated to 12 atm, then decreased to 4 atm, followed by simultaneous inflation of both balloons to 12 atm. This type of inflation showed no deformation of proximal stent, no malapposition of stent struts, and less SB ostial stenosis.
In COBIS I trail, the KBD caused more event rates related to MV stent, but in COBIS II trail, the same KBD showed less event rate. The difference is due to the size of the SB. In COBIS I, SB size was ≥ 2 mm whereas in COBIS II, the SB size was ≥ 2.3 mm.39 40 So, bigger the SB size, the more long-term good results KBD gives. According to SMART-STRATEGY trail, non-LMCA lesions in SB is < TIMI 3 flow or LMCA lesions if SB has > 70% stenosis then KSB is required. But KSB does not improve the long-term event rate; moreover, it was associated with increase in periprocedural MI. Even FFR-guided treatment to SB has not shown improved long-term results.41
VI) POT-SIDE-POT (RE-POT)
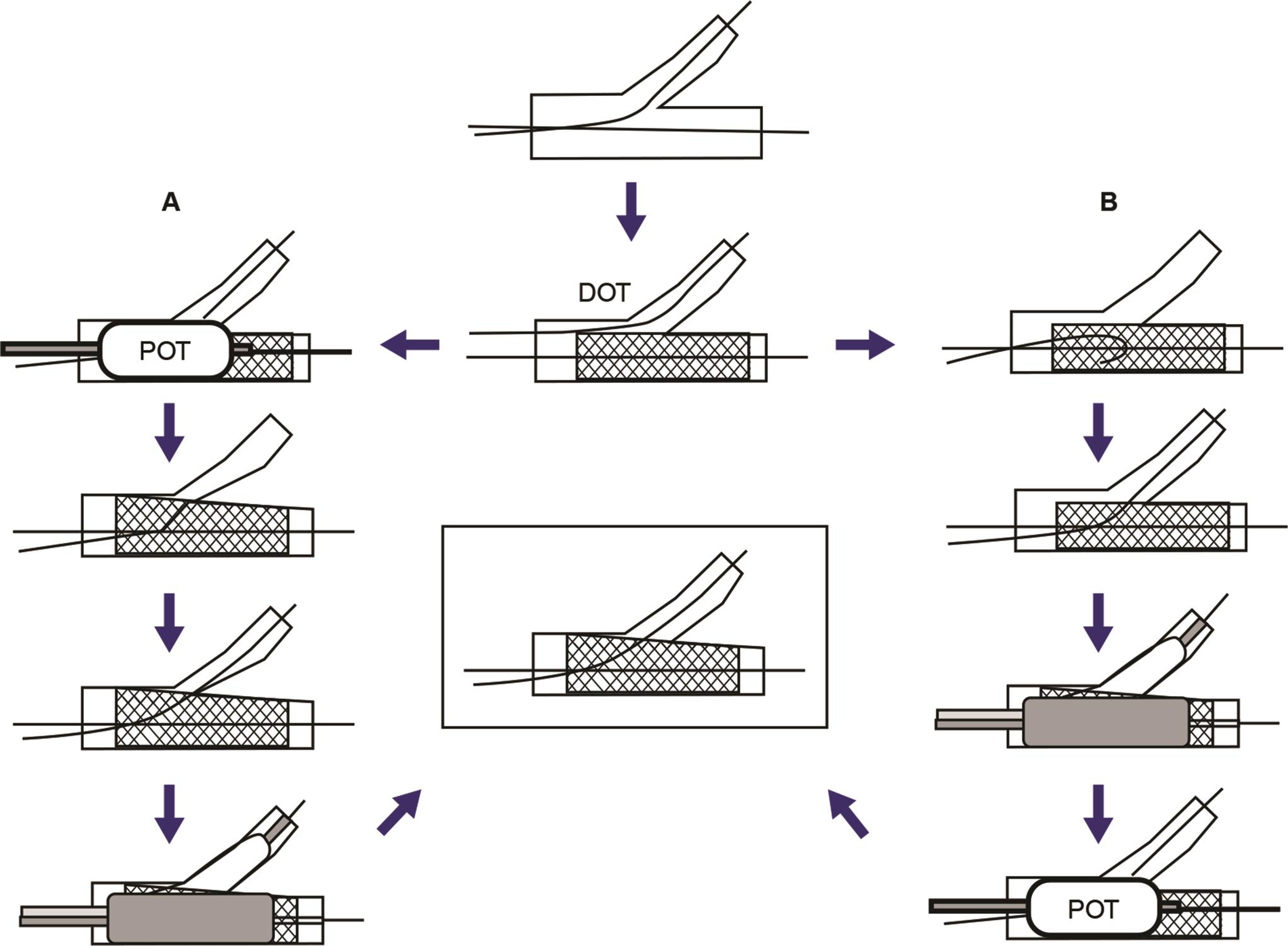
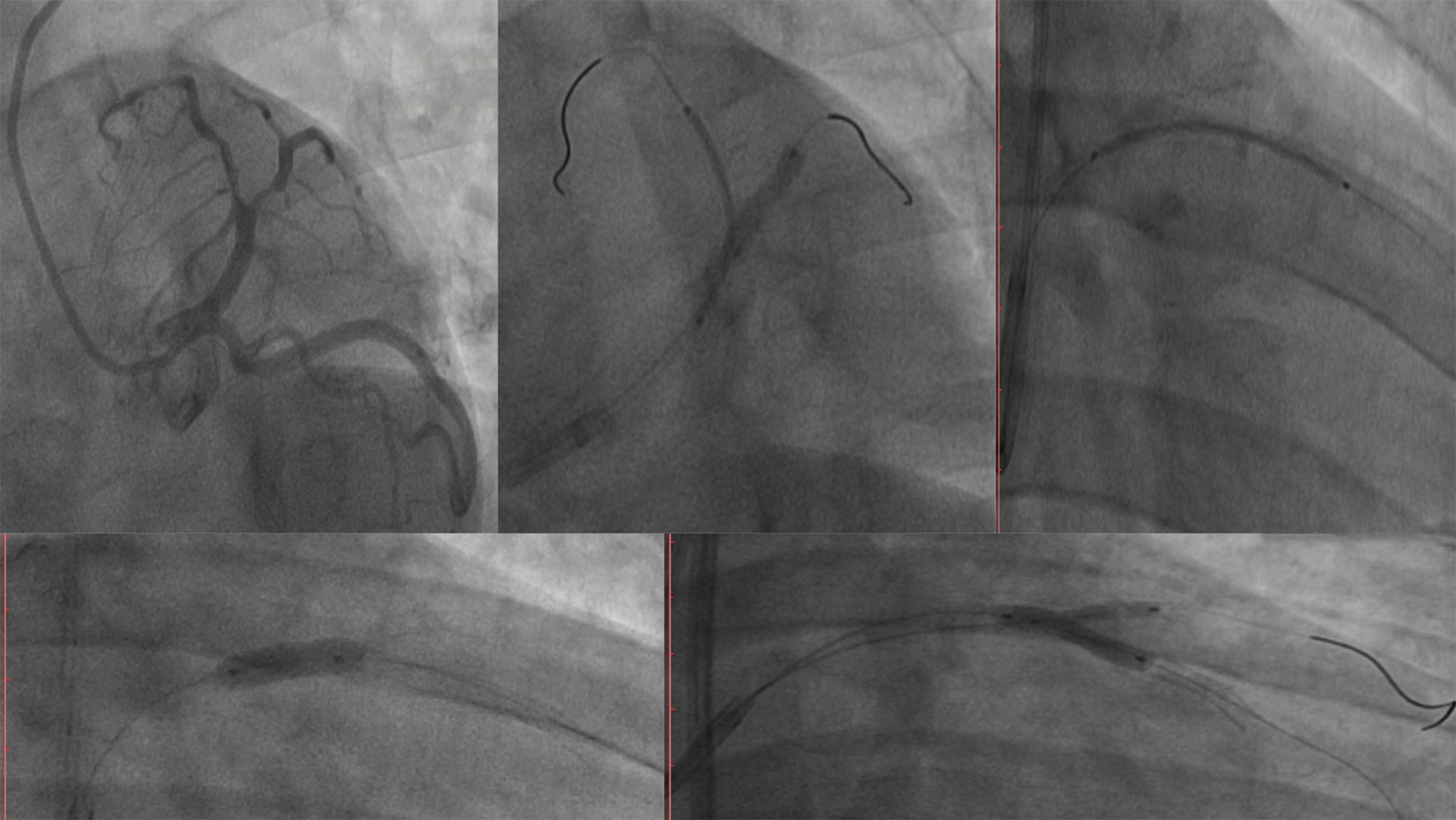
As already mentioned, bench testing showed that KSB does not expand the deformed MV stent by SB dilatation. So, re-POT to get final good circular expansion of the MV stent. For this, position of the re-POT balloon is important, which is different from POT. The distal end of the balloon should be in the proximal to the carina, covering the proximal edge of the stent carina and should not cover the carina, as it again causes the SB plaque shift.42 In Fig. 10, we showed a case of left circumflex artery (LCX)–obtuse margin artery (OM) bifurcation management with single-stent strategy.
-
Fig. 10 LCX–OM bifurcation lesion. (a) Both LCX and OM were wired. (b) Stent deployed in the main vessel (LCX). (c) POT with short balloon. (d) Stent strut opening with short NC balloon covering ostium of the SB (OM). (e) Final result with TIMI 3 flow in the SB. Abbreviations: LCX, left circumflex artery; NC., noncompliant; OM, obtuse marginal artery; POT, proximal optimization; SB, side branch; TIMI; thrombolysis in myocardial infarction.
Fig. 10 LCX–OM bifurcation lesion. (a) Both LCX and OM were wired. (b) Stent deployed in the main vessel (LCX). (c) POT with short balloon. (d) Stent strut opening with short NC balloon covering ostium of the SB (OM). (e) Final result with TIMI 3 flow in the SB. Abbreviations: LCX, left circumflex artery; NC., noncompliant; OM, obtuse marginal artery; POT, proximal optimization; SB, side branch; TIMI; thrombolysis in myocardial infarction.
VII) Indication of SB stenting in the provisional approach
As such, provisional stenting is the choice of treatment for bifurcation lesion.43 There are no clear-cut guidelines for SB stenting in provisional stenting.
A. Indications to SB stenting
a) Residual ≥75% stenosis.
b) SB FFR ≤0.80.
c) TIMI flow grade < 3 in SB.
d) Plaque shift into the SB.44
e) Clinical symptoms.
f) When future access toward the SB may be important.
g) SBs that can cause ≥10% ischemia
h) Fractional myocardial mass (FFM)–Myocardial mass supplied by a specific vessel. This is calculated from vessel length in CT. FMM was computed using stem and crown model based on allometric system.45 Only one out of every five non-LM SB supplies %FMM ≥10%
There is a scoring system to calculate whether the SB ischemia is significant other than the FFR and CT scan. SNuH score46 depends on the size (S) (vessel diameter ≥ 2.5 mm), Number (Nu) (number of diagonal branches ≤ 2) and highest (H) (No branch below the target branch).47 For each variable, one point was given. In modified SNUH (Table 3), If total score is 0, then − 1 is not added. The lowest total score is 0.
|
Variables |
Description |
Score |
|---|---|---|
|
Abbreviations: LAD, left anterior descending artery; OM, obtuse marginal artery; SNUH, size, number, ubiety, highest. |
||
|
Size |
Vessel diameter ≥ 2.5 mm |
1 |
|
Number of diagonal branches = 1 |
2 |
|
|
Number |
Number of diagonal branches = 2 |
1 |
|
Number of diagonal branches ≥ 3 |
0 |
|
|
Ubiety |
Left dominant or apical area reaching OM branch |
− 1 |
|
Highest |
No branch below the target branch in proximal to mid-LAD |
1 |
Indication of SB stenting in NORDIC48 trail was very conservative (only in TIMI 0 flow) versus more aggressive in SIRIUS bifurcation49 (residual stenosis ≥50%). CACTUS study50 suggested to stent the SB if residual stenosis ≥50% or type B dissection, whereas in SMART-STRATEGY trail, it differs (non-LMCA lesions in SB is < TIMI 3 flow or in LMCA lesions, if SB has > 70% stenosis). There is no long-term difference in conservative versus aggressive stenting strategies, but periprocedural MI was more in aggressive stenting strategies. Even EBC TWO51 trails showed same results even when SB size is ≥2.5 mm. Current EBS recommends, depending on experts consensus, to stent the SB when there is calcium and lesion length of SB is ≥5 mm. EBC MAIN52 trail involves head-to-head comparison of one- versus two-tent strategy in LMCA bifurcation, not in non-LMCA bifurcation lesion. In conclusion, till now non-LMCA bifurcation favors one-stent strategy.
B. Provisional SB stenting techniques
-
T-stent technique–No stent protrusion into the MV stent. So, there is risk of incomplete coverage of ostium of SB.
-
T and protrusion (TAP)–SB stent projects 1 to 2 mm into MV stent. SB stent and MV balloon are inflated simultaneously. TAP covers the SB ostium completely.
-
Other techniques are the reverse, internal crush or the provisional Culotte.
-
VIII) Alternatives for SB lesion management–drug-coated balloon (DCB) for SB
DCB to SB has gained more importance as the one-stent strategy became the best modality of the treatment for bifurcation lesions. In addition, DCB delivers the drug at ostium of SB, and there is less distortion of the carina and stent deformation, so it may require shorter duration of dual antiplatelet therapy (DAPT). The available balloons are Dior II (Eurocor), Sequent please (B Braun), In.Pact Falon (Medtronic-Invatec), Pantera Lux (Biotronics), Danubio (Minivasys), RESTORE DEB (cardionovum) and MOXY (Lutonix). The PEPCAD-BIF,53 BABILON54 and DEBIUT55 studies on the usage of drug-eluting balloons (DEB) for bifurcation could not conclusively demonstrate superiority of DEB over stent; in addition, target vessel failure (TVF) was more with DEB with suboptimal angiographic results even at the time of PCI. So, conclusion from these studies was DCB in the setting of bifurcations require further evaluation.
B). TWO -STENT STRATEGY
Even though one-stent strategy is a well-accepted modality for bifurcation lesion, there are some situations where, from the beginning, the plan is to use two-stent strategies.56 Such indications are true bifurcation lesions with
-
> 70 degrees of the bifurcation angle.
-
Long SB lesions (≥ 10 mm).
Different Techniques in Two Stent Strategies
-
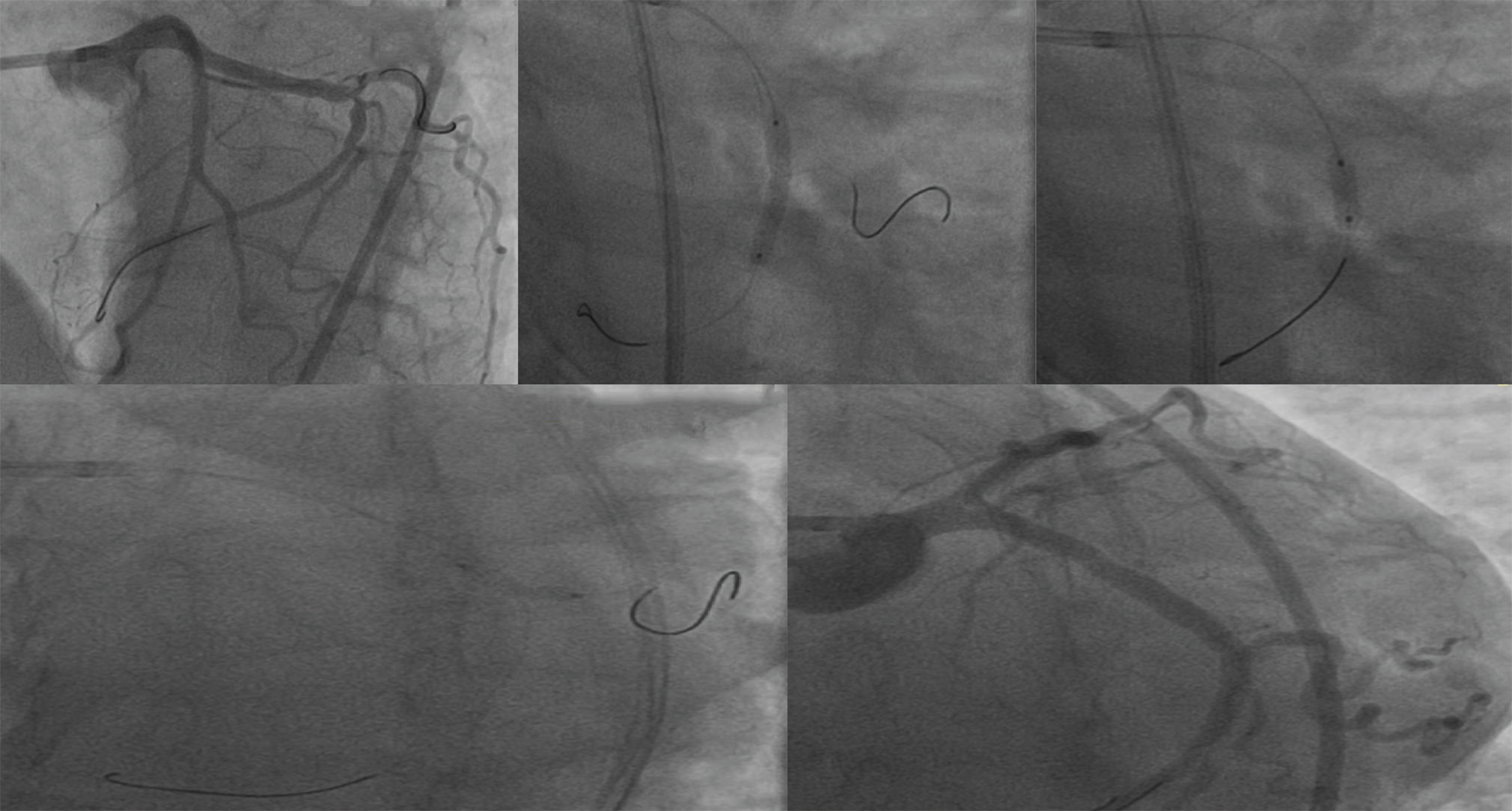
Classic T-stent and modified T-stent technique–After dilatation of MB and SB, SB stent to be deployed with (classical T-stent) or without protrusion (modified T-stent) and low-pressure dilatation of MV. After assessing the good result of SB, the wire of the SB is removed, and MB stent is deployed. Final kissing inflation (FKI) or side-main-side (SMS) inflation to be done after rewiring the SB though stent struts. The drawback of classical T-stent is chance of ostium of SB uncoverage and excess metal in proximal MB in modified T-stent technique. This technique is ideal for bifurcation of 90 degree. InFig. 11, a case of left anterior descending artery (LAD)–D1 bifurcation lesion management by modified T-stent technique was demonstrated.
-
Tap technique–This technique is typically used in provisional stent strategy but can be used in two-stent strategy also. The main problem with this technique is sometimes it is difficult to cross the SB through MV stent, resulting in suboptimal result of SB.
-
Culotte stent technique (CUT)–There are two distinct Culotte techniques. The Culotte can be done as a part of the provisional strategy, or in the second strategy, the stent is deployed from proximal MV to SB to prevent the SB occlusion.
In this, more angulated branch is stented, extending from the MV. Then wire is crossed though the stent to the MV and stented. FKI or SMS is done finally (Fig. 12). The advantage of the technique is complete lesion coverage, and it is better to do the procedure with open cell technology. The major disadvantage is double-layered stent in the proximal MV, which limits the maximal achievable diameter. To get better results, Culotte requires three times POT and one-time kiss. This technique should not be performed when there is lot discrepancy of the vessel sizes, as this causes malapposition of the stent in the proximal MB. The incidence of periprocedural MI and stent restenosis are less than crush technique.
-
Mini-crush and step-crush techniques–In mini-crush technique, after wiring both MV and SB, two stents are advanced. The stent in MV to be placed proximally and there is minimal protrusion of SB stent into MV. First, SB stent is to be deployed, then both wire and SB stent balloon to be removed after checking the result of SB. Then, MV stent is to be deployed, crushing the SB stent. Then, SB has to rewired and high-pressure dilatation is done, followed by FKI. This method also ensures good coverage of the ostium of SB and requires only SB recrossing instead of both branches in Culotte.
In step-crush or reverse crush technique, the SB stent is crushed with balloon first and then there is MV stent deployment. So, 6F guide is sufficient for this. Some operators do KBI before MV stent deployment. The advantage in this procedure is SB has to be rewired through the crushed two-stent struts of SB and after first KBI. SB now looks like a new sleeve, giving the name “sleeve” technique or “double kiss step-crush.”
-
V-stent AND SKS Techniques–In both the techniques, two stents are deployed simultaneously. In V-stent, there is minimal protrusion of the stents, whereas in simultaneous kissing stent (SKS), there is significant stent protrusion (≥ 5 mm). This is useful for Medina 0,1,1 bifurcation lesion. But the problem is malapposition in the proximal MB. In both techniques, both stents are deployed at low pressure (6–8 atmospheres), then separate high pressure inflation (14–16 atmospheres) of both stent balloons, followed again by simultaneous low-pressure inflation of both stent balloons. If subsequently intervention is needed for proximal MB, then crush technique is required.
-
Double kissing crush and modified double kissing crush technique–First, SB stent will be deployed with minimal protrusion into the MV. After crushing the protruded SB stent by MV balloon, recrossing of SB and balloon dilatation with first KBD is done. After removing the balloon and wire from the SB, deployment of MV stent, POT, recrossing of SB, final KBD, and re-POT is done. In this method, the recrossing of the SB happens from the proximal stent struts instead of distal most stent struts of the carina, as in provisional SB stenting. To have better results with DK crush, two POT and two kisses are optimal.
-
Fig. 11 Two-stent strategy–modified T-stent technique. (a) LAD–D1 bifurcation lesion. (b) After parking both LAD and D1 stent, first, D1 stent is deployed with minimal protrusion. (c) Then, LAD stent is deployed, crushing the DI minimally protruded stent struts. (d) POT. (e) Rewiring of SB and FKB dilatation. Abbreviations: FKB, final kissing ballooning; LAD, left anterior descending; POT, proximal optimization; SB, side branch.
Fig. 11 Two-stent strategy–modified T-stent technique. (a) LAD–D1 bifurcation lesion. (b) After parking both LAD and D1 stent, first, D1 stent is deployed with minimal protrusion. (c) Then, LAD stent is deployed, crushing the DI minimally protruded stent struts. (d) POT. (e) Rewiring of SB and FKB dilatation. Abbreviations: FKB, final kissing ballooning; LAD, left anterior descending; POT, proximal optimization; SB, side branch.
-
Fig. 12 Steps in Culotte technique.
Fig. 12 Steps in Culotte technique.
The major difference between provisional and double crush is how the SB is recrossed. In provisional crush, recrossing the SB is done through the distal stent struts at carina, whereas in double crush, it is done through proximal stent struts.57
The superiority of double crush over the classical crush are
-
First, KBI facilitates second KBI, as there is only one stent strut to cross and less distortion at the ostium of SB.
-
According to DK-CRUSH I, II, and III studies, the success rate is more with double crush with good access for repeat intervention if required.58
-
It is not to be affected by the angle, but stent fractures may play a role in the occurrence of SB ostial restenosis
Modified double kissing crush–The first kiss after crushing is replaced by balloon dilation of the SB through the crushed MB stent.
Preferred Stent Strategy
Although it is always difficult to determine which two-stent technique is the best for a given bifurcation lesion, the following guidelines can be used:
-
For Medina 0,1,1 lesions–V-stent technique.
-
For true bifurcation lesions with a bifurcation angle approximately 90 degrees–modified T-stent technique.
-
For true bifurcation lesions with a bifurcation angle < 70 degrees–mini-crush technique.
In BBK II59 trail, Culotte was better than T-stenting, whereas in NORDIC Stent Technique study,60 both Culotte and crush technique results were same. In DK-CRUSH III trail,61 Culotte was inferior to double kissing crush technique. At present, minimal protrusion of SB stent and minicrash is practiced more. Ultimately, the choice remains with whatever technique the operator is familiar with and achieve good expansion of both MV and SB stent.57
Comparative Studies of One- Versus Two-Stent Strategies
In Table 4, major studies done with one- or two-stent strategies were mentioned, and majority of them showed no difference in MACE except BBC-ONE study. Previously SB restenosis after intervention might have been dependent on the type of stenting strategy, but with better newer generation of DES, the situation is different32. In Nordic and other studies, the SB restenosis was dependent on severity of SB stenosis before intervention. If basal SB stenosis was > 50%, then chances of restenosis was 11 to 19% versus basal SB stenosis was < 50%, then chances of restenosis was 4.6 to 5%.62
|
First author/trial |
MACE with two-stent strategy |
MACE with one-stent strategy |
p value |
|---|---|---|---|
|
Abbreviations: BBC-ONE, British Bifurcation Coronary Study One; BBK-1, Bifurcation Bad Krozingen trial; CACTUS, Coronary bifurcations: Application of the Crushing Technique Using Sirolimus-eluting stents; DK-CRUSH II, Double Kissing Crush versus Provisional Stenting Technique for Treatment of Coronary Bifurcation Lesions trial; EBC TWO, European Bifurcation Club Trial; MACE, major adverse cardiac event (s); NS, nonsignificant; PERFECT, Optimal Stenting Strategy For True Bifurcation Lesions study. Follow-ups were variable from 6 to 60 months. |
|||
|
Colombo et al. |
23% |
22% |
NS |
|
Pan et al. |
8.5% |
7% |
NS |
|
Nordic-I |
3.4% |
2.9% |
NS |
|
Ferenc et al. |
12.9% |
11.9% |
NS |
|
CACTUS |
15.8% |
15% |
NS |
|
BBC-ONE |
15.2% |
8.0% |
0.009 |
|
Nordic-II |
21.8% |
15.8% |
NS |
|
DK-Crush II |
10.3% |
17.3% |
NS |
|
Nordic - Baltic IV |
8.3% |
12.9% |
NS |
|
EBC TWO |
8% |
10% |
NS |
|
BBK-1 |
16.3% |
16.2% |
NS |
|
PERFECT |
17.9% |
18.5 |
NS |
Dedicated Bifurcation Stents
Dedicated bifurcation stents were designed mainly to access the SB without recrossing. There are currently four dedicated stents commercially available worldwide: The BIOSS stent (Bifurcation Optimization Stent System, Balton, Warsaw, Poland- studied in POLBOS 3 study), the Stentys device (STENTYS, Princeton, New Jersey), the Axxess stent (Biosensors International, Singapore), and the Tryton stent (Tryton Medical, Durham, North Carolina).63 But these stents have not shown superiority over the provisional stenting.
Bifurcation Stenting with Bioabsorbable Scaffolds
There are limitations of BRS usage in bifurcation stents, mainly because of increased strut thickness.64 Thicker struts of BVS poses challenges for deliverability along with greater chances of SB occlusion. It is better to go in for provisional stenting than two-stent strategy with BVS.
Imaging in Bifurcation Lesions
Indications of Imaging
a) Angiographic ambiguity–in bifurcation lesions, nearly 50% of cases were other vessel lesions that were detected with imaging.
b) Most left mains.
c) Significant calcium–requires plaque modification before stenting.
d) Procedural guidance/complications.
e) Stent failure.
-
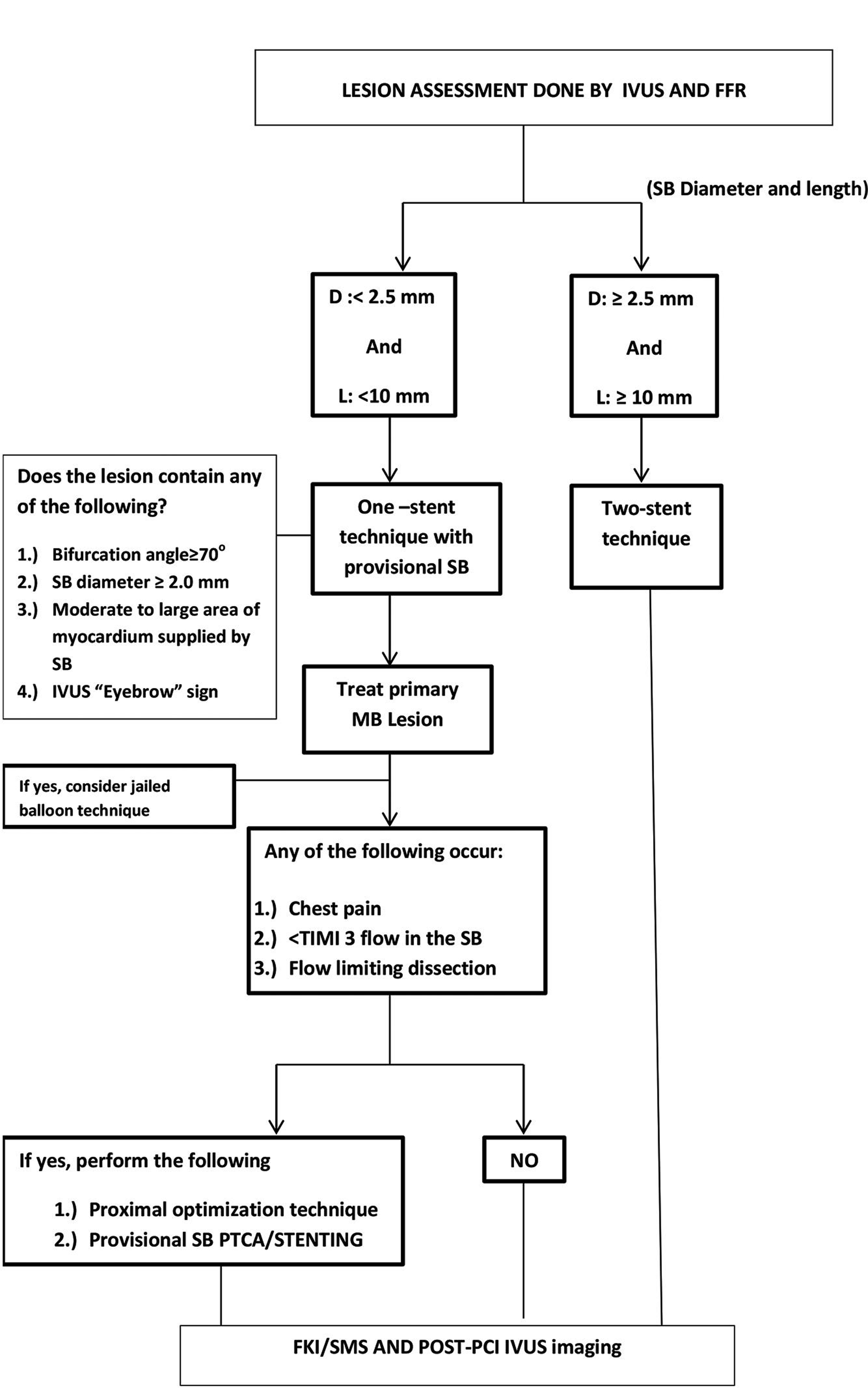
IVUS is useful before and after PCI in bifurcation lesions (Fig. 13).
Before PCI–
-
Assess plaque distribution and appropriately characterize the lesion (“IVUS Medina”).
-
Evaluate the extent of SB disease (especially for ostial lesions).
-
Appropriately size the vessel diameters of the MB and SB.
-
Recognition of the IVUS “eyebrow” sign (spiky appearance): a presenting marker for SB compromise.
After PCI–
-
SB compromise.
-
Stent deformation of the MB.
-
Plaque shift in the MB or SB.
-
Proximal or distal edge dissection.
-
Stent mal-apposition.
-
Stent under expansion.
-
Stent lesion coverage including gaps.
-
-
FFR indications in bifurcation lesion are
-
To find out the functional significance of SB ostial disease.
-
To assess the functional significance of SB pinching after MB stenting.
Limitation of FFR–A Medina “FFR index” has also been considered, although this is not feasible as FFR can only be used to analyze two vessels and not three segments.64
-
-
OCT is useful for evaluating lumen diameter, stent apposition and expansion, and lesion coverage.
-
Fig. 13 Flow chart to determine the type of PCI depending on IVUS and FFR. Abbreviations: FFR, fractional flow reserve; IVUS, intravascular ultrasound; PCI, percutaneous coronary intervention.
Fig. 13 Flow chart to determine the type of PCI depending on IVUS and FFR. Abbreviations: FFR, fractional flow reserve; IVUS, intravascular ultrasound; PCI, percutaneous coronary intervention.
Complications of Bifurcation Lesion Treatment
During Procedure
-
SB dissection.
-
Failure of SB wiring or ballooning.
-
Failure to do final KBD.
-
Suboptimal result of MV at carina of ostium of SB.
-
Stent distortion.
-
All general complications of PCI like bleeding from the access site (more in bifurcation as bigger sheath size is required), etc.
Early and/or Late
-
Stent thrombosis.
-
MV stent restenosis.
-
SB restenosis–This can be predicted by OCT imaging and fluid dynamics. If WSS is < 0.5 Pa, then risk of restenosis is there. Pathological findings showed that there was more neointimal thickness at lateral wall than flow divider, whereas fibrin deposition and uncovered struts were more common at flow divider.
Outcomes
Already in Tables 2 4, the short- and long-term outcomes in major clinical trials were mentioned. Overall outcomes of bifurcation lesions are suboptimal. Target vessel revascularization (TVR) occurs in 40% of cases. Operator should ensure that results on all branches of bifurcation are good angiographically and, if required, even imaging wise (IVUS or OCT or FFR).
Future Perspectives
More computational fluid dynamics (CFD) studies to compare the acute and long-term results of the different stent strategies in bifurcation lesions. The aim should be minimal detrimental flow conditions to have a long-term good results.65 Local fluid dynamics such as low and oscillating wall shear stress may facilitate the development of in-stent restenosis and stent thrombosis. So, in future we should able to detect these abnormalities at the time of PCI itself with machine learning process, and develop better technical improvement with help of artificial intelligence.
Summary
The coronary artery bifurcation anatomy and physiology are complex. To determine the size of the different components of bifurcation, intravascular assessment is better than applying Murray or Finet’s law. Both distal and proximal optimization of the stent gives good immediate and long-term results. In doubtful cases of SB pinching after MV stenting, it is better to see its functional significance. The main aim of the bifurcation treatment is to have best results in all segments. Although optimization and maintenance of SB in bifurcation treatment procedures are much discussed about topics, the long-term results depend on the MV management. So, in order to know the optimal results, it is advisable to do invasive imaging during and at the end of the procedure. The flow chart (Fig. 14) may guide in the performing the bifurcation lesion treatment. Even though there are different studies favoring one strategy over the other, the best accepted strategy is the single-stent technique.
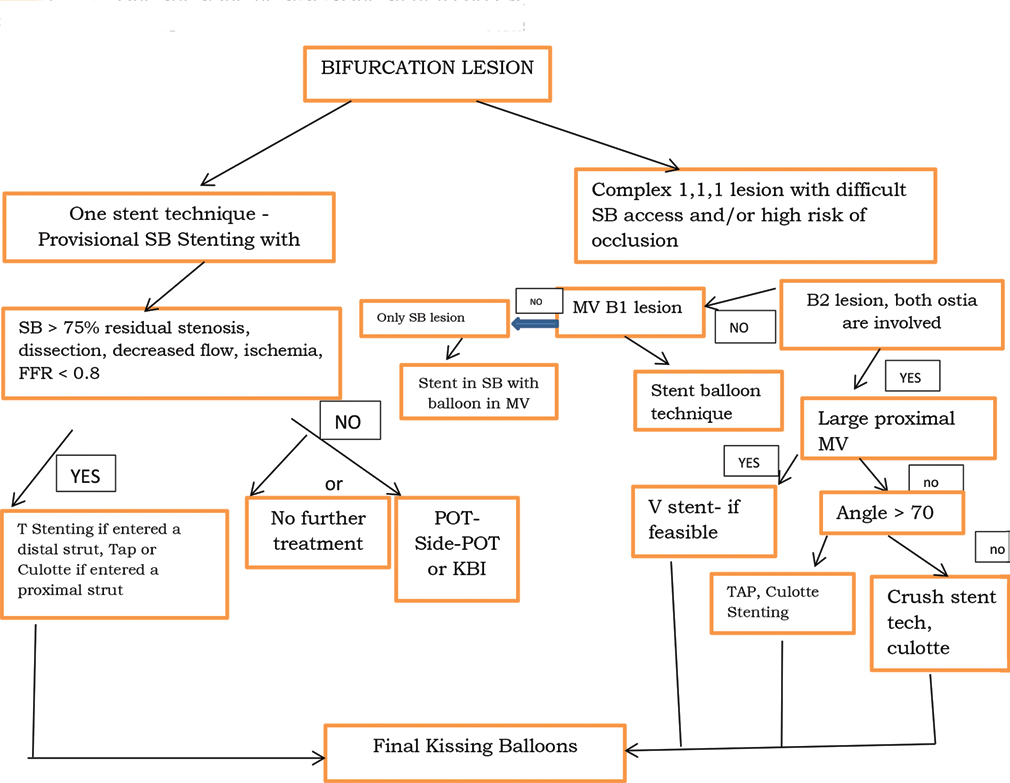
-
Fig. 14 Condensed flow chart for coronary bifurcation lesion management.
Fig. 14 Condensed flow chart for coronary bifurcation lesion management.
Conflict of Interest
None declared.
References
- ARTS II Investigators. 5-year clinical outcomes of the ARTS II (Arterial Revascularization Therapies Study II) of the sirolimus-eluting stent in the treatment of patients with multivessel de novo coronary artery lesions. J Am Coll Cardiol. 2010;55(11):1093-1101.
- [Google Scholar]
- Restenosis rates following bifurcation stenting with sirolimus-eluting stents for de novo narrowings. Am J Cardiol. 2004;94(01):115-118.
- [Google Scholar]
- Clinical and angiographic outcome after implantation of drug-eluting stents in bifurcation lesions with the crush stent technique: importance of final kissing balloon post-dilation. J Am Coll Cardiol. 2005;46(04):613-620.
- [Google Scholar]
- Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations: the CACTUS (Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus-Eluting Stents) Study. Circulation. 2009;119(01):71-78.
- [Google Scholar]
- Long-term outcomes of provisional stenting compared with a two-stent strategy for bifurcation lesions: a meta-analysis of randomised trials. Heart. 2017;103(18):1427-1434.
- [Google Scholar]
- Simple or complex stenting for bifurcation coronary lesions: a patient-level pooled-analysis of the Nordic Bifurcation Study and the British Bifurcation Coronary Study. Circ Cardiovasc Interv. 2011;4(01):57-64.
- [Google Scholar]
- Bifurcation lesions: no need to implant two stents when one is sufficient! Eur Heart J. 2016;37(24):1929-1931.
- [Google Scholar]
- Prediction of the localization of high-risk coronary atherosclerotic plaques on the basis of low endothelial shear stress: an intravascular ultrasound and histopathology natural history study. Circulation. 2008;117(08):993-1002.
- [Google Scholar]
- [A new classification of coronary bifurcation lesions] Rev Esp Cardiol. 2006;59(02):183.
- [Google Scholar]
- Reproduced with permission from Latib et al. JACC Cardiovasc Interv. 2008;1:218-226.
- [Google Scholar]
- The treatment of coronary bifurcations: a true art form. EuroIntervention. 2015;11:V7. (Suppl V)
- [Google Scholar]
- Long-term outcomes with use of intravascular ultrasound for the treatment of coronary bifurcation lesions. Am J Cardiol. 2012;109(07):960-965.
- [Google Scholar]
- The physiological principle of minimum work: I. The vascular system and the cost of blood volume. Proc Natl Acad Sci U S A. 1926;12(03):207-214.
- [Google Scholar]
- Potential predictors of side-branch occlusion in bifurcation lesions after percutaneous coronary intervention: a coronary CT angiography study. Radiology. 2014;271(03):711-720.
- [Google Scholar]
- Randomized comparison of conservative versus aggressive strategy for provisional side branch intervention in coronary bifurcation lesions: results from the SMART-STRATEGY (Smart Angioplasty Research Team-Optimal Strategy for Side Branch Intervention in Coronary Bifurcation Lesions) randomized trial. JACC Cardiovasc Interv. 2012;5(11):1133-1140.
- [Google Scholar]
- Contemporary approach to coronary bifurcation lesion treatment. JACC Cardiovasc Interv. 2016;9(18):1861-1878.
- [Google Scholar]
- Comparison of vessel geometry in bifurcation between normal and diseased segments: intravascular ultrasound analysis. Atherosclerosis. 2008;201(02):326-331.
- [Google Scholar]
- Krams R, Di Mario C. Final proximal post-dilatation is necessary after kissing balloon in bifurcation stenting. EuroIntervention. 2011;7(05):597-604.
- [Google Scholar]
- Fractal geometry of arterial coronary bifurcations: a quantitative coronary angiography and intravascular ultrasound analysis. EuroIntervention. 2008;3(04):490-498.
- [Google Scholar]
- Randomized comparison of final kissing balloon dilatation versus no final kissing balloon dilatation in patients with coronary bifurcation lesions treated with main vessel stenting: the Nordic-Baltic Bifurcation Study III. Circulation. 2011;123(01):79-86.
- [Google Scholar]
- Impact of intravascular ultrasound guidance on long-term clinical outcomes in patients treated with drug-eluting stent for bifurcation lesions: data from a Korean multicenter bifurcation registry. Am Heart J. 2011;161(01):180-187.
- [Google Scholar]
- Predictors and outcomes of side branch occlusion after main vessel stenting in coronary bifurcation lesions: results from the COBIS II Registry (COronary BIfurcation Stenting) J Am Coll Cardiol. 2013;62(18):1654-1659.
- [Google Scholar]
- Periprocedural myocardial infarction is not associated with an increased risk of long-term cardiac mortality after coronary bifurcation stenting. Int J Cardiol. 2013;167(04):1251-1256.
- [Google Scholar]
- Importance of proximal angle in generation of abnormal plaque at coronary bifurcation lesions. Indian Journal of Cardiovascular Diseases Journal in Women. 2016;1(01):1-6.
- [Google Scholar]
- Natural history of small and medium-sized side branches after coronary stent implantation. Am Heart J. 2002;143(04):627-635.
- [Google Scholar]
- Carina shift versus plaque shift for aggravation of side branch ostial stenosis in bifurcation lesions: volumetric intravascular ultrasound analysis of both branches. Circ Cardiovasc Interv. 2012;5(05):657-662.
- [Google Scholar]
- Assessment of side branch predilation before a provisional T-stent strategy for bifurcation lesions. A randomized trial. Am Heart J. 2014;168(03):374-380.
- [Google Scholar]
- Technical aspects of the provisional side branch stenting strategy. EuroIntervention. 2015;11:V86-V90. (Suppl V)
- [Google Scholar]
- Provisional side branch-stenting for coronary bifurcation lesions: evidence of improving procedural and clinical outcomes with contemporary techniques. Catheter Cardiovasc Interv. 2013;82(04):E437-E445.
- [Google Scholar]
- PROPOT (PROspective randomized study to evaluate Proximal Optimaization Technique in coronary bifurcation lesions). Presented at TCT conference , September 28, 2019
- Techniques for Palmaz-Schatz stent deployment in lesions with a large side branch. Cathet Cardiovasc Diagn. 1995;34(04):353-361.
- [Google Scholar]
- Pathological findings at bifurcation lesions: the impact of flow distribution on atherosclerosis and arterial healing after stent implantation. J Am Coll Cardiol. 2010;55(16):1679-1687.
- [Google Scholar]
- Pattern of instent neointimal formation compared to native atherosclerosis in the coronary bifurcation lesions: volumetric intravascular ultrasound analysis. Chin Med J (Engl). 2013;126(18):3505-3510.
- [Google Scholar]
- Relative dependence of diameters of branches in coronary bifurcations after stent implantation in main vessel–importance of carina position. Kardiol Pol. 2008;66(04):371-378, discussion 379.
- [Google Scholar]
- Hemodynamic impact of changes in bifurcation geometry after single-stent cross-over technique assessed by intravascular ultrasound and fractional flow reserve. Catheter Cardiovasc Interv. 2013;82(07):1075-1082.
- [Google Scholar]
- Physiologic assessment of jailed side branch lesions using fractional flow reserve. J Am Coll Cardiol. 2005;46(04):633-637.
- [Google Scholar]
- A modified provisional stenting approach to coronary bifurcation lesions: clinical application of the “jailed-balloon technique”. J Interv Cardiol. 2012;25(03):289-296.
- [Google Scholar]
- Kissing balloon or sequential dilation of the side branch and main vessel for provisional stenting of bifurcations: lessons from micro-computed tomography and computational simulations. JACC Cardiovasc Interv. 2012;5(01):47-56.
- [Google Scholar]
- [Six-month intravascular ultrasound follow-up of coronary bifurcation lesions treated with rapamycin-eluting stents: technical considerations] Rev Esp Cardiol. 2005;58(11):1278-1286.
- [Google Scholar]
- Randomized comparisons between different stenting approaches for bifurcation coronary lesions with or without side branch stenosis. JACC Cardiovasc Interv. 2015;8(04):550-560.
- [Google Scholar]
- Physiological evaluation of the provisional side-branch intervention strategy for bifurcation lesions using fractional flow reserve. Eur Heart J. 2008;29(06):726-732.
- [Google Scholar]
- Comparative analysis of sequential proximal optimizing technique versus kissing balloon inflation technique in provisional bifurcation stenting: fractal coronary bifurcation bench test. JACC Cardiovasc Interv. 2015;8(10):1308-1317.
- [Google Scholar]
- Double versus single stenting for coronary bifurcation lesions: a meta-analysis. Circ Cardiovasc Interv. 2009;2(05):409-415.
- [Google Scholar]
- Anatomic and functional evaluation of bifurcation lesions undergoing percutaneous coronary intervention. Circ Cardiovasc Interv. 2010;3(02):113-119.
- [Google Scholar]
- HY Kim, JACC Cardiovasc Interv 2017 (to write the full reference)
- Kim HL, Koo BK, Nam CW, et al. Clinical and physiological outcomes of fractional flow reserve-guided percutaneous coronary intervention in patients with serial stenoses within one coronary artery. JACC Cardiovasc Interv 2012;5(10):1013-1018
- Stenting of bifurcation lesions: classification, treatments, and results. Catheter Cardiovasc Interv. 2000;49(03):274-283.
- [Google Scholar]
- Nordic PCI Study Group. Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic bifurcation study. Circulation. 2006;114(18):1955-1961.
- [Google Scholar]
- Randomized study to evaluate sirolimus-eluting stents implanted at coronary bifurcation lesions. Circulation. 2004;109(10):1244-1249.
- [Google Scholar]
- European Bifurcation Coronary TWO (EBC TWO) trial
- Chieffo A, Hildick-Smith D. The european bifurcation club left main study (EBC MAIN): rationale and design of an international, multicentre, randomised comparison of two stent strategies for the treatment of left main coronary bifurcation disease. EuroIntervention 2016;12(1):47-52
- Drug eluting balloons as stand alone procedure for coronary bifurcational lesions: results of the randomized multicenter PEPCAD-BIF trial. Clin Res Cardiol. 2016;105(07):613-621.
- [Google Scholar]
- A prospective randomised study of the paclitaxel-coated balloon catheter in bifurcated coronary lesions (BABILON trial): 24-month clinical and angiographic results. EuroIntervention. 2014;10(01):50-57.
- [Google Scholar]
- A multicenter randomized comparison of drug-eluting balloon plus bare-metal stent versus bare-metal stent versus drug-eluting stent in bifurcation lesions treated with a single-stenting technique: six-month angiographic and 12-month clinical results of the drug-eluting balloon in bifurcations trial. Catheter Cardiovasc Interv. 2012;80(07):1138-1146.
- [Google Scholar]
- Definitions and classifications of bifurcation lesions and treatment. EuroIntervention. 2015;11:V23-V26. (Suppl V)
- [Google Scholar]
- The “crush” technique for coronary artery bifurcation stenting: insights from micro-computed tomographic imaging of bench deployments. JACC Cardiovasc Interv. 2008;1(04):351-357.
- [Google Scholar]
- Comparison of double kissing crush versus Culotte stenting for unprotected distal left main bifurcation lesions: results from a multicenter, randomized, prospective DKCRUSH-III study. J Am Coll Cardiol. 2013;61(14):1482-1488.
- [Google Scholar]
- Understanding the coronary bifurcation stenting. Korean Circ J. 2018;48(06):481-491.
- [Google Scholar]
- Coronary artery bifurcation lesion classifications, interventional techniques and clinical outcome. Expert Rev Cardiovasc Ther. 2008;6(02):261-274.
- [Google Scholar]
- Culotte stenting vs. TAP stenting for treatment of de-novo coronary bifurcation lesions with the need for side-branch stenting: the Bifurcations Bad Krozingen (BBK) II angiographic trial. Eur Heart J. 2016;37(45):3399-3405.
- [Google Scholar]
- Randomized comparison of coronary bifurcation stenting with the crush versus the culotte technique using sirolimus eluting stents: the Nordic stent technique study. Circ Cardiovasc Interv. 2009;2(01):27-34.
- [Google Scholar]
- Bifurcation stenting: current strategies and new devices. Heart. 2009;95(06):495-504.
- [Google Scholar]
- A. ColomboBioresorbable scaffolds for the management of coronary bifurcation lesions. JACC Cardiovasc Interv. 2016;9(10):989-1000.
- [Google Scholar]
- Histopathologic and physiologic effect of bifurcation stenting: current status and future prospects. Expert Rev Med Devices. 2020;17(03):189-200.
- [Google Scholar]
- Local fluid dynamics in patients with bifurcated coronary lesions undergoing percutaneous coronary interventions. Cardiol J 2020 e-pub ahead of print
- [CrossRef] [Google Scholar]







