Translate this page into:
Coronary Balloons of 2024 and Future
*Corresponding author: Anshu Kumar Jha, Department of Cardiology, Maharaja Krushna Chandra Gajapati Medical College and Hospital, Berhampur, Odisha, India. akj2410@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Satpathy C, Jha AK. Coronary Balloons of 2024 and Future. Indian J Cardiovasc Dis Women. doi: 10.25259/IJCDW_57_2024
Abstract
Since 1977, when Dr. Grüntzig performed the first Percutaneous Coronary Intervention (PCI), this science has completely changed the way coronary lesions were treated earlier. Initially, it started with Plain Old Balloon Angioplasty which was replaced by stents in 1990s and then again the reemergence of coronary balloon came with the introduction of drug-coated balloons. There are various types of balloon – non-complaint, semi complaint, high pressure, proximal optimization technique balloon, cutting, scoring, chocolate, ostial flash, drug coated, perfusion, and intravascular lithotripsy. Every balloon has a particular function and a different structure. Today, drug-eluting balloons have become the standard of care for in-stent restenosis and trials are going on with the vision of “stentless PCI.” Coronary balloons have now become an indispensable tool in the cath lab but like with any other instrument, there are complications which may occur. Balloon rupture, shaft fracture, indeflatable balloon, entrapped deflated balloon, and coronary dissection are few complications which may occur during usage of these coronary balloons. In this review article, we have dealt in detail about different types of balloon, their usage and complications and ways to deal with those complications.
Keywords
Coronary balloon
Drug-coated balloon
Coronary intervention
Chocolate balloon
INTRODUCTION
In 1974, at University of Zurich, Switzerland, a German physician Dr. Andreas Grüntzig (1939–85) did the world’s first balloon angioplasty for severe femoral artery stenosis. It was this procedure which completely changed the treatment prospect of coronary artery disease patients. In 1977, the first percutaneous transluminal coronary angioplasty (PTCA)/percutaneous coronary intervention (PCI) was done by Grüntzig in a 38-year-old Adolf Bachman for a left anterior descending (LAD) stenotic lesion.[1] Confidence was instilled by cardiac surgeon Dr. Senning who said “Herr Grüntzig: Machen Sie es, falls etwas passiert, operiere ich!” meaning “Mister Grüntzig: Do it, if something happens, I will operate.”[2] Since then, the evolution of coronary balloons has always been on a rise with no looking back. In 1980s and 90s, the stent era began because the restenosis in plain old balloon angioplasty (POBA) was nearly 40%.[3] Initially, bare metal stents were introduced and Dr. Puel with Dr. Sigwart performed the first stent implantation in coronary artery in 1986.[4,5] By 2001, drug-eluting stents (DES) came up and by the end of 2006, trials were published with results of treating in-stent restenosis (ISR) with drug-coated balloon (DCB).[6] In todays era of looking at stentless PCI and not much success with bioresorbable stents, DCB is coming up in a big way. At present, as per guidelines, DCB is only indicated for treatment of ISR or small vessel lesions, i.e., <3.0 mm but potential expansion for larger vessels may expand its use in a wider range of lesion.[7]
BASIC STRUCTURE OF CORONARY BALLOON
Coronary balloon were earlier made of polyvinyl chloride but the thickness of this material proved to be a hindrance in developing large profile balloons and posing as a challenge for balloon to be delivered to target lesion. With the advent of newer materials such as nylon and polyethylene terephthalate (PET), the profile of balloons has decreased and crossing the lesion has become easier. These materials are used in making non-compliant balloon. Even softer materials like low density copolymer polyether block amide (PBA) are used in making of semi-compliant balloons. They easily cross through torturous vessels but they have low rate burst pressure (RBP).[8] A few basic terms related to coronary balloons are elaborated here. Coronary balloon is present at the distal tip of a catheter. The various components of a catheter are (proximal to distal) - inflation port, proximal shaft, central lumen for guide, distal shaft, balloon with either single or double radiopaque marker and tip. Balloon has a working length - distance between proximal and distal marker, diameter - distance between its opposite walls, a shoulder - the point onward from where the tapering starts and end at the catheter, cone angle - the angle at the ends of the balloon on either sides, compliance - it is the ability of balloon diameter to change with pressure, nominal pressure - refers to the pressure at which when balloon is inflated, it achieves the listed balloon diameter, RBP - the pressure at which 99.9% of balloons will not burst with 95% confidence but after that point vessel may be damaged. The balloon catheters are of two types - over the wire balloon catheter (OTW) and rapid exchange (RX)/Monorail. The advantages and disadvantages of OTW versus RX are shown in Table 1.
| Balloon Catheters | Advantages | Limitations |
|---|---|---|
| Over The Wire (OTW) | Distal wire position is stable | Two people needed for device exchange |
| Multiple wires can be accepted | Larger cath diameter | |
| Contrast or drug can be injected through distal port | ||
| Rapid Exchange (RX) (Monorail) |
Ease of use by single operator | Needs good guide support |
| Enhanced visualization | Wire cannot be changed | |
| Smaller cath diameter | Blood loss occurs at Y-valve during wire exchange |
TYPES AND FUNCTION
There are various types of coronary balloons and each has its own special use. They mainly differ based on their structure, any additional coating of cutting blades/drugs and compliance.
Non-compliant (NC) balloon
These balloons are made of PET so they have thick walls which allows the balloon to work at higher pressure. As pressure is increased the balloon does not expand much and conforms less to the vessel architecture. This allows the operator to instill more pressure on the vessel wall without much increase in diameter of the balloon. This property helps to crack heavily calcified lesions and post dilation of the stent. As there is minimal longitudinal expansion of the balloon, dilation outside the stented area does not occur. This also decreases the chance of malapposed stents. NC balloons have a high RBP of around 18–20 atm. In the MOZECTM NC study, procedural success was achieved in 100% patients. Major adverse cardiac events (MACE) or target lesion failure (TLF) was 0%. Mozec™ NC Rx PTCA balloon dilatation catheter showed better outcomes for the dilatation in routine cases as well as complex coronary lesions.[9]
Semi compliant (SC) balloon
These balloons are made of softer materials like PBA of polyolefin copolymer. So when the operator dilates the balloon it grows and conforms to the area of least resistance. As the pressure is increased, the size of the balloon increases proportionately but “dog boning” occurs as it does not expand in an area with tight stenosis. It is used for POBA, pre-dilation of very tight lesions and to deliver drugs to the endothelium when used as DCB. Because it offers a good rewrap, it can be used multiple times unlike NC balloon. RBP of the SC balloon is about 12–14 atm. Recently, newer insight from two randomized controlled trials have shown that instead of using SC balloon in simple coronary lesion for stent bed preparation, using NC balloon yielded better results and was found to be safe.[10]
High pressure balloon (OPN)
This is a special type of NC balloon made up of double-layered polyamide material which can withstand very high pressure. This balloon is basically used when NC fails. An international study at three centers involving 326 calcified coronary lesions has shown OPN balloon to be a safe and effective alternative strategy.[11] When compared with other techniques like rotational/orbital atherectomy, excimer laser, cutting/scoring balloon using OPN is very economical for such lesions. In the ComparIson of Strategies to PrepAre SeveRely CALCified Coronary Lesions: the ISAR-CALC randomised (ISAR-CALC) trial, it was seen that inpatients with severe calcified lesion when compared to scoring balloon OPN balloon increased the minimum lumen diameter more (2.83 ± 0.34 mm vs. 2.65 ± 0.36 mm; P = 0.03) and better reduced the diameter stenosis (11.6 ± 4.8% vs. 14.4 ± 5.6%; P = 0.02). The angiographic and procedural success was same in both the groups.[12]
Proximal optimization technique (POT)TM balloon
This is a special form of NC balloon which is designed especially for the POT. The main difference lies in the structure of this balloon. Here, the shoulder of the balloon is ultrashort, about 0.6 mm, unlike normal NC balloon in which shoulder length is 3.2 mm (these comparisons are for a diameter of 3 mm NC and a 3 mm POT balloon). Due to this typical structure, there is reduced longitudinal growth thus minimizing trauma outside the treatment area and focusing exactly at the site where pressure is warranted. Analysis of the e-ULTIMASTER trial shows that over and above a low 1-year failure rate in the bifurcation stenting cohort, the POT further reduced the event rate and showed a uniform benefit across subgroups, thus strengthening the recommendation for the POT balloon technique irrespective of the bifurcation anatomy and stenting technique.[13]
Cutting balloon
This is a type of NC balloon with three to four microsurgical blades mounted along its longitudinal length. It helps to expand target lesion by severing the elastic and fibrotic continuity of the vessel with tiny incisions. The micro-incisons also help to get controlled and focused micro fractures in the calcified lesions with as low as 12 atm pressure [Figure 1]. A plane NC balloon shows much lower stress distribution at same pressure and even when inflated to higher pressure it leads to uncontrolled fractures.[14] It is ideally advised to take size which is 0.5–0.75 mm less than the reference vessel diameter (calculated by IVUS). Slow inflation/deflation at 1 atm/s for 60 s is advised to achieve an optimal result. Studies have shown that stent delivery is better with a cutting balloon as compared to a scoring balloon (90.8% vs. 79.5%; P = 0.006).[15] This balloon is highly useful for ISR, fibrotic plaque, and calcific lesions. Adding to the already present advantages, the Cutting Balloon to Optimize Predilatation for Stent Implantation (COPS) trial showed that cutting balloon angioplasty was associated with larger stent area when compared to NC balloon angioplasty in calcified coronary lesions. Stent area was 8.2 mm2 versus 7.3 mm2 in cutting balloon versus NC balloon group.[16]
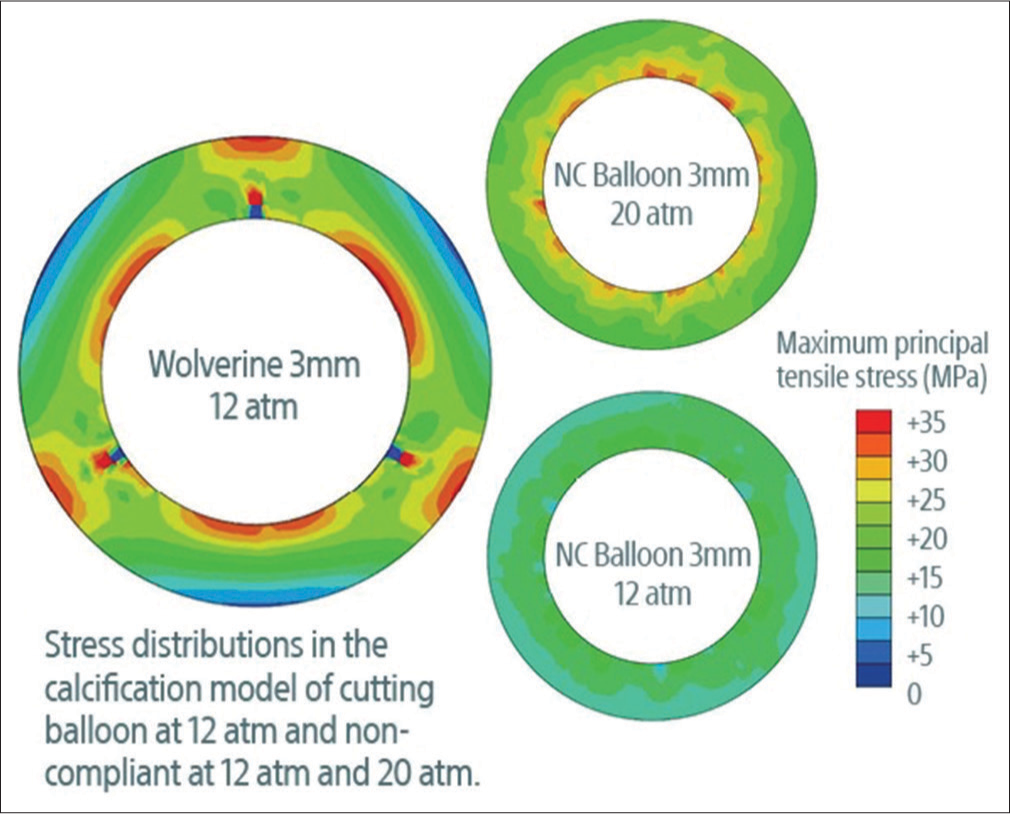
- Difference in the stress generated by the WOLVERINETM cutting balloon when compared to a noncompliant balloon. (Courtesy Boston scientific). (NC: Non-compliant)
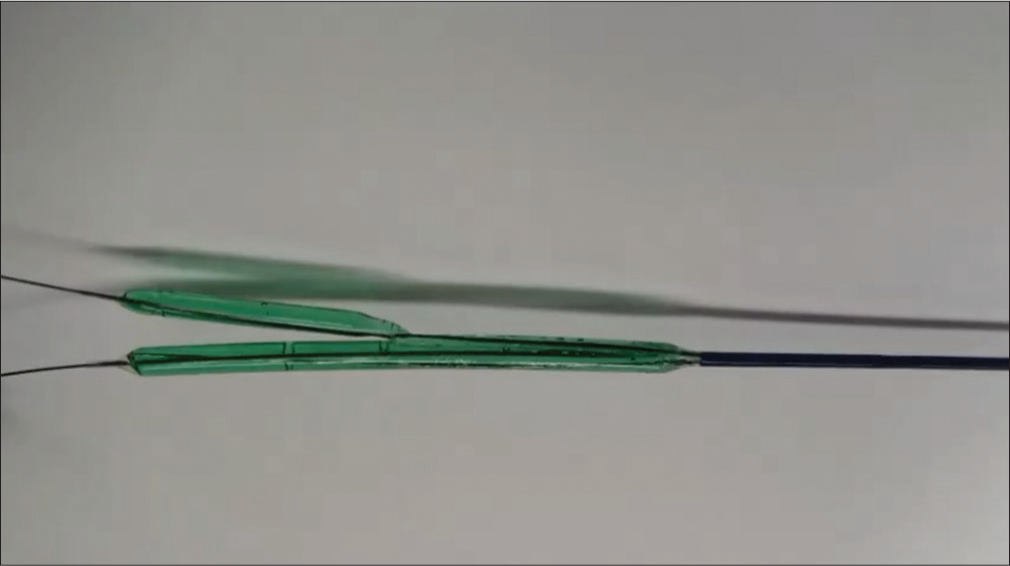
Scoring balloon
It is a form of SC balloon over which there are laser cut nitinol frames (AngioSculpt™) wrapped around in a helical fashion or it may have a knob like arrangement (GRIP™). The rectangular edges of the scoring element lock the device in place to minimize device slippage during inflation. The expansion properties of the three rectangular spiral struts are influenced by a fixed distal end and a semiconstrained proximal end. Due to this design, the scoring balloon drives an outward expansion with force 15–20 times more than the conventional balloon an point of contact of nitinol frame and the vessel wall [Figure 2]. Being a SC balloon, it has a better profile, better deliverability, and lower chance of dissection. Difference between scoring and cutting balloon is shown in Table 2. Although talking about the advantages of scoring and cutting balloons for preparing of the stent bed, a meta-analysis showed that in patients treated with PCI for severely calcific coronary artery disease lesion preparation with either scoring or cutting balloon before stenting did not improve outcomes when compared with the control group.[17]
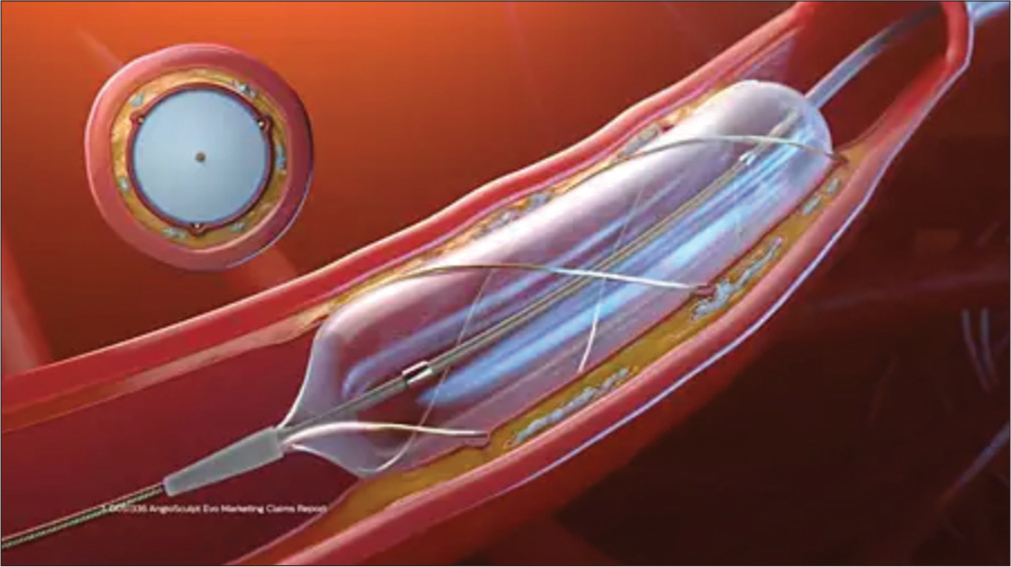
- The helical nitinol scoring elements wrap the balloon circumferentially to minimize slippage and lock itself to the lesion. This scoring element can deliver up to 25 times the force of a non-compliant balloon. (AngioSculptEvoTM courtesy Philips).
| Scoring balloon | Cutting balloon |
|---|---|
| Semicompliant balloon | Non compliant balloon |
| High pressure balloon | Lower pressure balloon |
| Nitinol wire - 125 µm / Dot | Microblades or atherotomes around balloon |
| Data adequate for clinical use | Data limited |
| Better profile, flexible, easily delivered, lower dissection / perforation | Bulkier, higher crossing profile, less flexible, difficult to deliver |
Chocolate balloon
The Chocolate PTCA balloon is a SC balloon which is caged in a nitinol-constraining structure that allows for 1:1 vessel sizing. While inflating, the cage causes the balloon to dilate in a controlled manner, preventing dog-boning (common in SC balloons) and overinflation. This arrangement also causes the balloon to form a series of alternating segmented pillows and grooves throughout the lesion. The pillow areas apply force to create small dissections which are required for effective dilatation and grooves act as stress relievers for dissection to propagate[18] [Figure 3 and 4]. Another advantage of chocolate balloon is that there is no “watermelon seed effect” and less barotrauma. The first in-human study of paclitaxel coated chocolate balloon (Chocolate Heart DCB, TriReme Medical, Pleasanton, California) was done in 2019 at Dominican Republic. There was 100% procedural success achieved with zero mortality at the end of 1 month. Late lumen loss (LLL) was −0.01 mm ± 0.35 mm which was better than what was demonstrated in BELLO trial using paclitaxel coated DCB which was 0.08 ± 0.38 mm.[19,20]
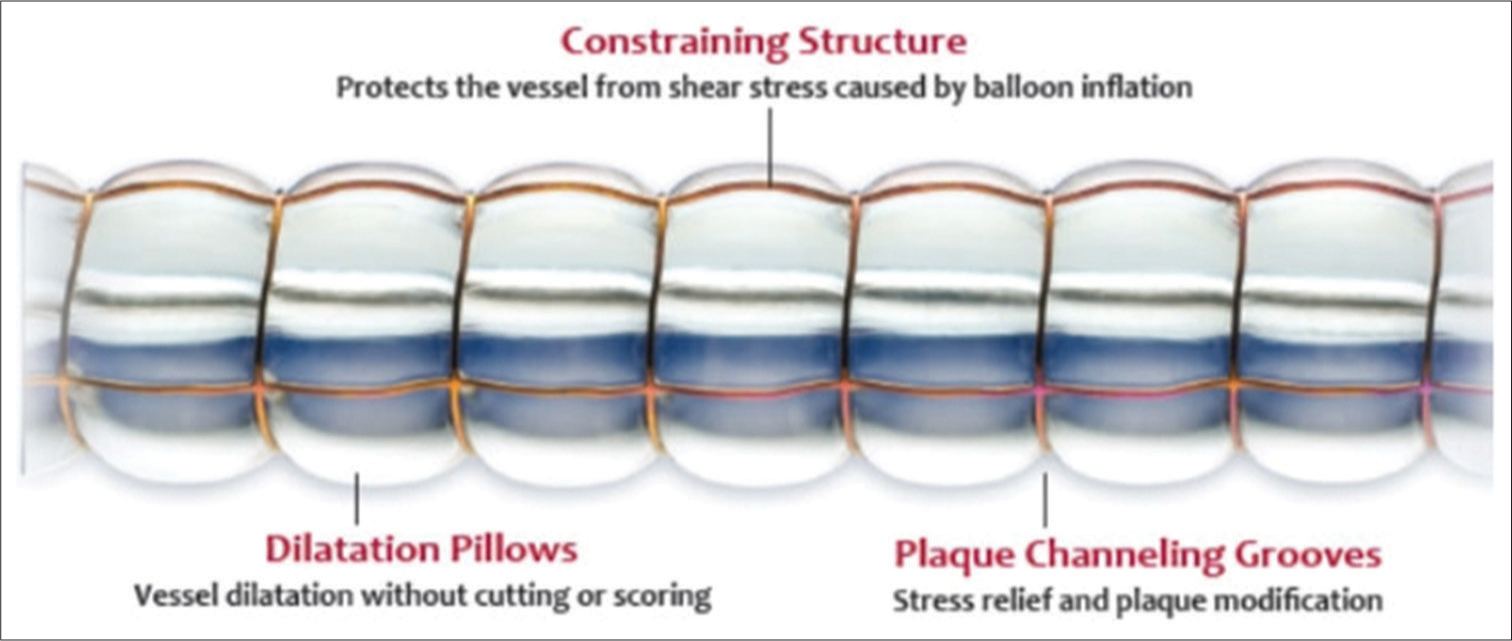
- Chocolate balloonTM with advantage of its typical structure (courtesy TriReme Medical LLC, Teleflex).
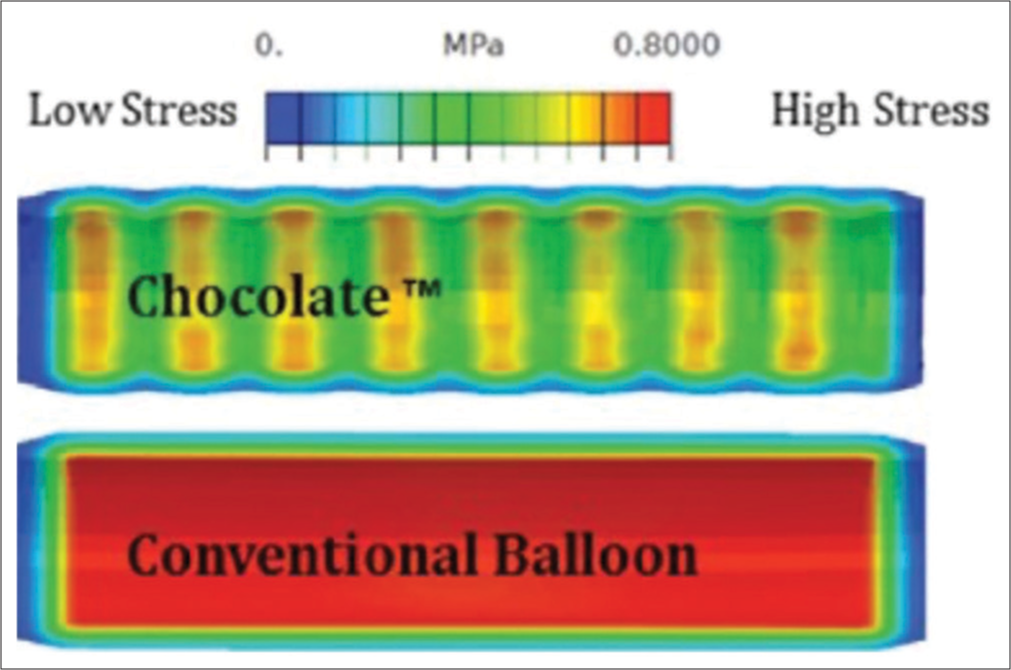
- Pressure distribution along the vessel wall while using a chocolate balloon as compared to a conventional balloon. (courtesy Cordis corporation).
Ostial flash balloon
This is a dual balloon (outer compliant and inner SC balloon) catheter which comprises of an outer compliant proximal balloon, oriented coaxially over an inner semi-compliant distal balloon. The proximal balloon has a larger diameter and is spherical in shape. Because of this dual balloon design ostial flash balloons achieve stent wall apposition after post dilatation and provide stability during angioplasty of challenging aorto - ostial lesion. It has 3 markers unlike other balloons. The distal marker is proximal to the distal edge of the stent, middle marker is at the ostium and proximal marker is outside the guide catheter. First the distal balloon is inflated so that the system is well anchored inside the stent. After this the proximal spherical balloon is inflated resulting in the stent edges opposed to the side wall of the main vessel (MV). Post dilation with this balloon, future intervention, if at all required, becomes easy as the guidewires can easily cross through the stent [Figure 5a-d].
![(a) the placement of markers while using an ostial flash balloon. Mid-marker: At the ostium (placed 2 mm distal to the proximal edge of the stent). Distal marker: At least 2–3 mm within the stent. Never beyond the distal edge of the stent. Proximal marker: In the aorta, outside the guide catheter. (b) The distal balloon is inflated upto desired pressure. (c) inflation of the proximal spherical balloon. (d) Deflation of proximal balloon followed by deflation of distal balloon. (coutesy Ostial Corporation [Osital]).](/content/148/2025/0/1/img/IJCDW-57-2024-g005.png)
- (a) the placement of markers while using an ostial flash balloon. Mid-marker: At the ostium (placed 2 mm distal to the proximal edge of the stent). Distal marker: At least 2–3 mm within the stent. Never beyond the distal edge of the stent. Proximal marker: In the aorta, outside the guide catheter. (b) The distal balloon is inflated upto desired pressure. (c) inflation of the proximal spherical balloon. (d) Deflation of proximal balloon followed by deflation of distal balloon. (coutesy Ostial Corporation [Osital]).
DCB
These are SC balloon with the coating of the desired drug which may be either Paclitaxel/Sirolimus. After the invention of DES the value of DCB had declined but now the interest has renewed. Initially DCBs were limited to those patients where POBA was not sufficient or DES could not be implanted. Though they remained the treatment of choice for ISR, in today’s time DCB is emerging as an alternative to DES. It has advantage of releasing and embedding the drug during angioplasty without leaving anything behind thus avoiding the demerits of putting a stent and impairing the motility of a vessel and exposing patient to risk of stent restenosis.[21] As there is no metal in the coronaries the de-escalation of dual anti platelet therapy (DAPT) can be done early in high bleeding risk (HBR) cases. Despite these advantages the use of DCB has some limitations - the elastic recoil of the vessel wall after balloon angioplasty, the risk of coronary dissections, arterial remodeling, and patient to patient variability of response to the drug still needs to be answered.[22] There are multiple components of a DCB - the drug, the carrier, the polymer and the excipient. There are two drugs approved for coating over the balloon. Paclitaxel, which is an anti-neoplastic drug with cytotoxic properties and is most widely used. It is lipophilic so it easily penetrates the cell membrane. Sirolimus, is a mTOR (mammalian Target Of Rapamycin) inhibitor which arrests cell growth in G1/S transition phase. As it is non-lipophilic in nature so requires a carrier molecule to let the drug penetrate the vessel wall.[23] Carrier molecules and polymer allow the drug to maintain its concentration during vascular transit and also act as an adhesive for the drug while it attaches to the vessel wall. Various carrier molecules used are - urea, ipopromide, acetyl tributyl citrate.[24] For sirolimus these are still more important and require a little more advanced technology like - nano carriers with sirolimus nanoparticles, micro reservoirs and crystalline coating.[25] Another difference is that Paclitaxel coated balloon may sometimes lead to myonecrosis and embolization which has not been observed with sirolimus coated balloon. The 3 years follow up PICCOLETO - II study done in small coronary vessel (≤2.5 mm) de novo stenosis showed that LLL was more with DES arm than DCB (0.17 ± 0.39 vs. 0.04 ± 0.28, P = 0.03) at 6 months. Another 3 year follow up trial, the BASKET - SMALL 2 trial showed that there was no difference in MACE between DCB and DES regardless of bleeding risk (HBR, hazard ratio: 1.16 [0.51–2.62]; P = 0.719 versus nonHBR, 0.96 [0.62–1.49]; P = 0.863).[26] This showed that there was no difference between DCB and DES results in treatment of coronary artery disease irrespective of bleeding status. Though there are no direct trials for DCB in large vessels but some clarity comes from the sub-analysis of larger observational prospective and retrospective studies like the Safety of PAclitaxel dRug-coaTed balloon-only Angioplasty of de novo Left Main Stem coronary disease (SPARTAN-LMS).[27] Potential advantages of DCB in larger vessels (≥2.75 mm) are - avoiding stent strut malapposition especially in irregular vessel wall or in a bifurcation lesion, early de-escalation of DAPT in HBR patients, in long diffuse atherosclerotic lesion and lastly in young patients DCB should be initially tried with the strategy of “intervention without implantation.”[28-31] There are two ongoing trials which will determine if DCB is non-inferior/superior to DES in large vessels - TRANSFORM II, SELUTION.[32,33] The most recent A Clinical Trial to Assess the Agent Paclitaxel Coated PTCA Balloon Catheter for the Treatment of Subjects With In-Stent Restenosis Disrupt (AGENT IDE) trial showed that patients treated with Paclitaxel DCB was superior to plain balloon with respect to TLF at 1 year in patients who underwent angioplasty for ISR. TLF in DCB group was 17.9% as compared to 28.6% in plain balloon (P = 0.003).[34]
Perfusion balloon
Perfusion balloons were invented in the 1980s for prolonged inflations required to “tack up” dissection planes but fell out of favor with the introduction of bare metal stents. Unlike the SC/NC balloons, perfusion balloons allow distal coronary perfusion while dilating a lesion. This is possible as this balloon has multiple proximal and distal holes. More recently, with the advent of DCB, balloon angioplasty is back in picture to determine whether a stentless strategy can deliver the same procedural result. Fukuoka and colleagues report results from a proof-of-concept study in which 30 patients were treated with prolonged inflation (over 10 min) with a perfusion balloon prior to paclitaxel DCB inflation and results were good.[35] Studies have evaluated Primary Perfusion Balloon Angioplasty in Primary PCI for ST-Segment Elevation Myocardial Infarction in order to prevent reperfusion injury. Those patients who underwent this new procedure as compared to conventional balloon angioplasty had better prognosis and the difference was driven by a lower incidence of no-reflow/slow flow (P = 0.0001).[36]
Intravascular lithotripsy balloon
Intravascular lithotripsy balloon [Figure 6] consist of an angioplasty balloon catheter with a 12 mm fluid filled balloon. There are two shockwave emitter in the shaft of the balloon. These shockwaves travel through the vessel’s soft tissue and cause a fracture in the calcium. The heat generated is neutralized by the fluid present in the balloon. This plaque modification helps in better stent expansion. About 4–6 atm pressure is applied so that the balloon is fully opposed to the vessel wall and then the IVL pulses are applied at the rate of 10 pulses over 10 s after which 10 s pause is given before repeating the pulses. Maximum 80 pulses are recommended. It is used in preparing beds for stent placement at places where there is severely calcified plaque (approved by food and drug administration in 2017). Disrupt CAD series of study (I, II, III, IV) have shown that coronary IVL safely and effectively facilitates stent implantation in calcified lesions. Lately there have been advancements in the IVL with an increased in the number of pulses delivered. The new next generation Shockwave C2+ offers 50% more pulses than its previous version. So, we get in total of 120 pulses which becomes handy when treating diffuse long lesions.[37] Off label use is also seen in ISR, stent under expansion and lesions post coronary artery bypass graft (CABG).[38] There are a few disadvantages which need to be overcome by further modification of this technology. A few of them are - larger balloon profile, limited size options, limited pulses per catheter which increases the cost of procedure, effect on eccentric and nodular calcium is limited and long term results are awaited.

- Intravascular lithotripsy balloon with console (courtesy Shockwave medicals).
Glider balloon
This is a special form of SC balloon with a skived tip and low entry profile. It has got a unique tip design and has a hydrophilic coating over it. The shaft of the balloon has good torquability and this helps it to cross complex lesions and through the stent struts while dealing with bifurcation lesions. Though this special morphology gives it an added advantage but it is contraindicated for use in unprotected left main coronary artery and coronary artery spasm without significant stenosis.[39] Figure 7 shows the balloon with the skived tip.
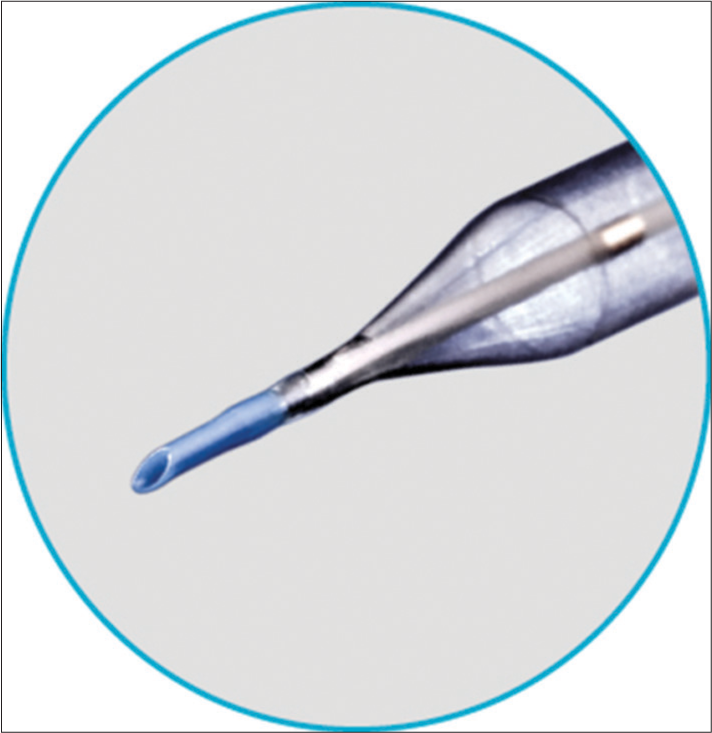
- Glider balloon with its skived tip (courtesy Teleflex).
Chronic total obstruction (CTO) balloon
When dealing with a CTO lesion which is uncrossable, there arises a need for an extra support. CTO balloons have proved to be of much help to overcome in such situations. There are various dedicated CTO balloons like - Mozec™ CTO balloon, ACCROSS CTO balloon, AlveoHP, NIC Nano Hydro. NIC Nano Hydro CTO balloon has a crossing profile of 0.0195 inch and an inflated diameter of 0.85 mm. The shaft thickness is reduced in the balloon area. AlveoHP balloon has a crossing profile of 0.0184 inch and an inflated diameter of 0.75–2.0 mm. ACROSS CTO balloon is a SC balloon which has a tapered 4mm tip, low crossing profiles, and a puncture resistant design. It has a RX design. Mozec™ CTO balloon has a 90.9% success rate in crossing CTO lesions. It also has a 93.3% success rate in crossing tight and severely calcified lesions. This was observed in the MOZec™ CTO balloon in complex coronary interventions (MOZART) Registry. Other CTO balloons include Sapphire 3, Ikazuchi Zero, and Ryurei.[40]
Bifurcation balloon
This is a special type of balloon which is used exclusively in cases of bifurcation lesions. It consists of one proximal balloon for MV, one balloon for the main branch and another balloon for the side branch. With the use of current techniques like DK Crush or Culotte, the lumen of proximal part becomes ellipsoidal which necessitates for 2nd POT to get a circular lumen, but this being a single system so MV is circular. Also, usually with kissing balloon technique, we tend to oversize the proximal vessel but this can be avoided with this single system balloon. This unique system may replace the final kissing balloon step and also avoid jailing of the second wire. The angle of the carina will also be preserved. Though this looks promising, the delivery of balloons is difficult because of its large profile. Different sizes of vessels, different angles of carina and varying branch diameters make it difficult for one single balloon complex to fit in all. Many permutations and combinations shall be required. Also, a marker will be required to showcase the exact point of bifurcation[41,42] [Figure 8].
- Dedicated bifurcation balloon filled with colored dye.
A few real time images of coronary balloons used at our center are shown in Figures 9a-c, 10a-d, 11. Table 3 shows advantages and disadvantages of all the above discussed balloons.
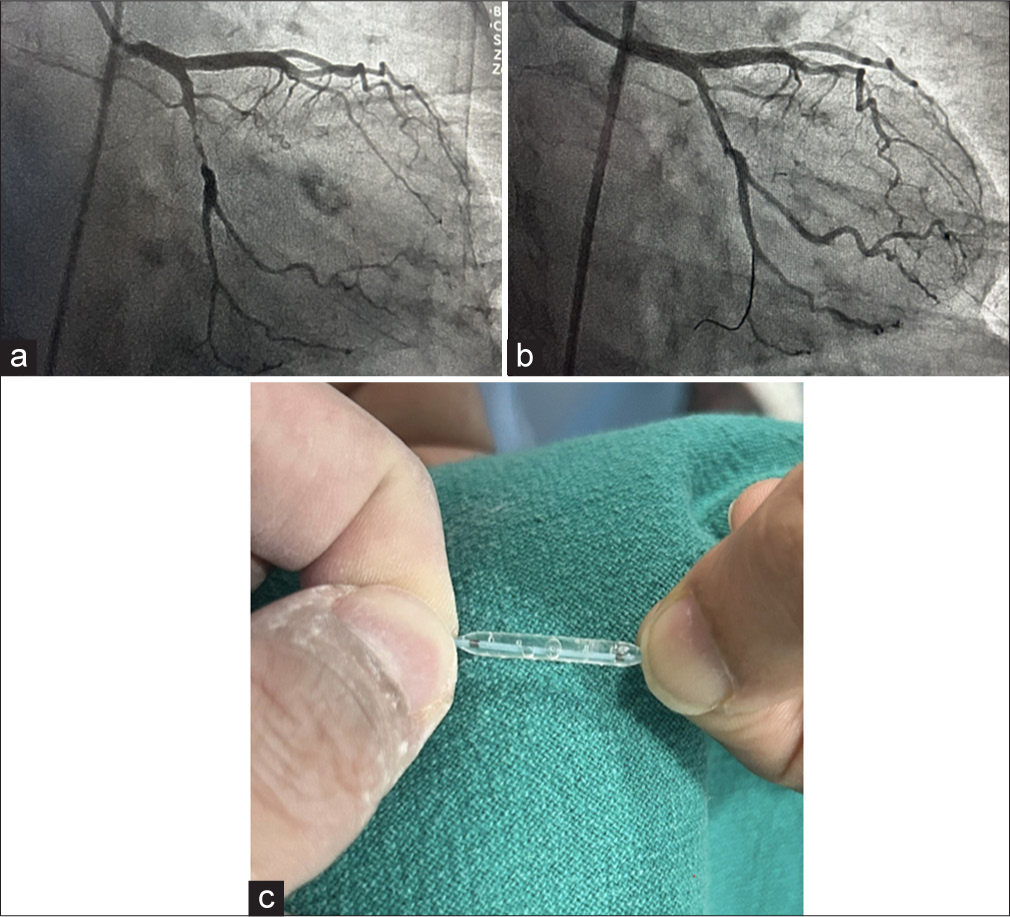
- (a) Coronary angiogram before using GRIP TT (Acrostak) balloon, (b) Coronary angiogram before using GRIP TT (Acrostak) balloon, (c) Image showing the rows of focal knobs positioned across the body of the balloon. The Focal knobs act as pressure points to treat difficult to crack plaque at the same time helping the balloon to grip, reducing the risk of slippage.
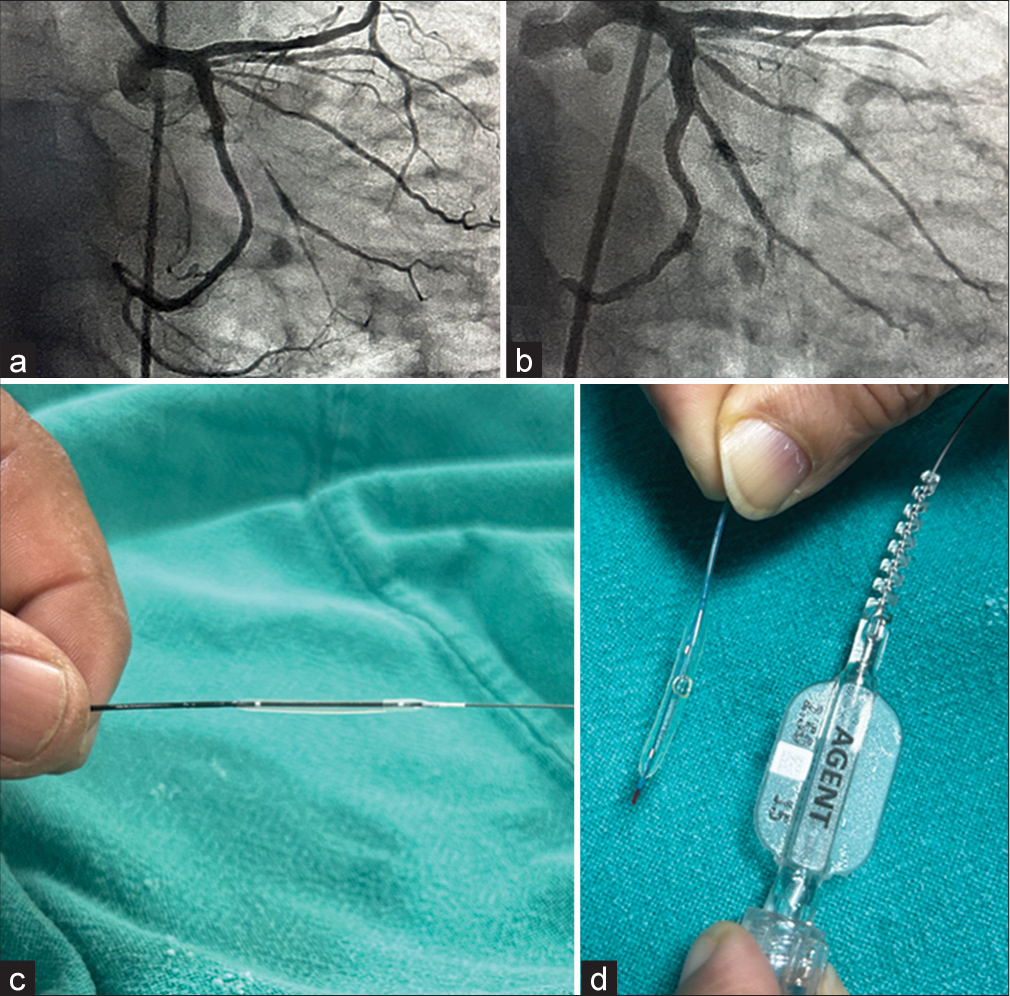
- (a) Coronary angiogram before using the drug coated balloon, (b) Coronary angiogram after using drug coated balloon, (c) Sirolimus coated Magic Touch balloon, (d) Paclitaxel coated AGENT balloon.
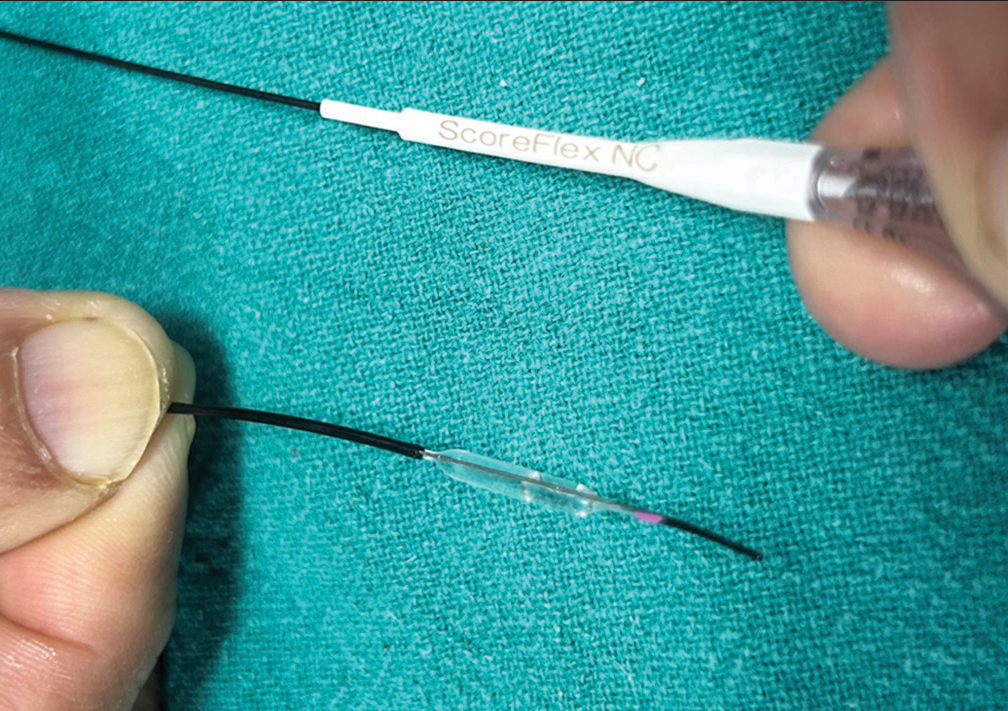
- Scoreflex is a focused force dilatation balloon with a dual-wire system which creates a focal stress pattern to facilitate safe and controlled plaque modification at lower resolution pressure. The sharp edge of wire can be seen on the upper side of the balloon.
| Coronary balloons | Advantage | Disadvantage |
|---|---|---|
| SC balloon | Easily expandable at low pressure and crossability is good, less cost, reusable after dilating once | Higher chances of edge dissection |
| NC balloon | Higher pressure produces lesser expansion | Bulkier and difficult to cross lesion once used |
| High pressure (OPN) balloon | Very high pressure upto 50 atm can be obtained which helps to crack fibrotic and calcified lesion | Bulkier and difficult to cross lesion once used |
| POT balloon | Working length and Balloon length same making cone angle less acute so precise dilatation | Not easily available |
| Cutting balloon | Helps open tough fibrotic and calcified lesion | Bulkier and difficult to cross lesion once used |
| Scoring balloon | Grips the lesion so less chance of slippage avoiding dissection of normal segment | Bulkier and difficult to cross lesion once used |
| Chocolate balloon | Less barotrauma as pressure is equally distributed on grooves and grooves act as stress buster | Costly |
| Ostial flash balloon | Covering of whole osmium, struts in main vessel will be completely apposed by proximal SC spherical balloon | Not easily available |
| Drug coated balloon | Metal free angioplasty is possible, ideal for small vessels, ISR, HBR | Transit time for distal delivery too short, dilation needs to be slow to avoid dissection |
| Perfusion balloon | Prolong inflation possible specially in case of perforation | Not easily available |
| IVL balloon | Avoids dissection, distal embolization, cracks both superficial and deep calcium | Costly and bulkier |
| Glider balloon | Easily crosses through small area and stent struts due to skived tip and short balloon length | Not easily available |
| Bifurcation balloon | Natural shape of artery preserved avoiding 2ndPOT, carina deformity avoided | Multiple sizes with various angulations required, still in stage 1 of research |
HBR: High bleeding risk, ISR: Instant restenosis, IVL: Intravascular lithotripsy, NC: Non-compliant, POT: Proximal optimization technique, SC: Semi-compliant
COMPLICATIONS
While using coronary balloons there are a few complications which need to be kept in mind. A few of them are discussed here.
Balloon rupture
It occurs most commonly when the operator goes beyond the RBP of the balloon or if it is a calcified plaque or it may also occur due to frequent use of the same balloon after sterilization leading to material fatigue. The sign of material fatigue is that there will be some point of focal bulge over the balloon. Balloon rupture can be of three types - pin hole, in which there is a jet of contrast forcing itself through the pinhole and staining the vessel wall. Circumferential/Radial rupture, in which balloon separates into two half circumferentially. Longitudinal/Axial tear, in which rupture occurs along the longitudinal length of balloon but there is minimum risk of vessel injury or component detachment in this type of rupture. Rupture is easily recognized by sudden drop in pressure with blood seeping into indeflator.
Balloon shaft fracture
This is of two types, one in which the shaft is broken but still in the guiding catheter and another in which shaft is broken and outside the guiding catheter. This mostly occurs due to excessive twisting of the balloon. Now, for the former one the best way to come out of situation is to use the balloon trapping technique and take out the assembly. In the latter case, if the shaft is in aorta we can try snaring technique and if unsuccessful then surgery. In case when the shaft is in coronary artery then we can either snare it or fix it with a stent or go for surgical removal.[43]
Undeflatable balloon
It occurs when we twist the balloon catheter by more than 360° to cross a tight lesion and usually it gets stuck after inflation in the distal portion of the lesion. Another mistake for this complication to happen is using undiluted contrast. Options available with us for this situations are - advancing a coronary guide wire into the balloon inflation port with the hope that it will burst the balloon, cutting of distal braid of a 5F guiding catheter and advance it like a guide extension catheter. The braided part may perforate the balloon, using ultra high filtration to burst the balloon (be ready for damage control like dissection/perforation). Last option is surgery.[44]
Entrapped deflated balloon
It mostly occurs in tortuous, calcified or angulated coronary lesions. Initially when methods of multiple inflation - deflation cycles, pushing and twisting the balloon to rewrap it and then pulling it back into a guide extension catheter to liberate the balloon, are unsuccessful we can go for a micro snare. Using micro snare we should go as close to the balloon shaft as possible and then tighten the snare and try to pull back the balloon. Surgery is the last resort.[45]
Coronary dissection
When the balloon is dilated to high pressures coronary dissection may occur. This holds true even for pressures below the RBP. There are six types of dissection from A-F. Type A being the least and type F with total lumen occlusion. In his interventional board review Dr. Lloyd W. Klein stated that type A and B were not usually dangerous, types C and D could be serious, and types E and F might well require early surgical intervention. Treatment is based on what type of coronary dissection has occurred. It varies from observation in intensive care unit to using of vasopressor and Intra Aortic Balloon Pulsation for hemodynamic support and placing a PCI or even performing an open heart surgery if deemed necessary.[46]
CONCLUSION
Coronary balloon has been one of the backbone of interventions in cardiology. Starting in the 1980s it has undergone many modifications as per the need of the operating physician and disease pathology. Currently, various options are available starting from NC balloons to IVL balloons which in many ways have changed the treatment protocol. There is a special focus on DCB which is seen as a resurrection of an old technology. In the coming future the concept of “Stentless PCI” might be a reality. Like with every hardware there are some complications which, if the operator is well aware of, can be mitigated easily.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent is not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Balloon Angioplasty-The Legacy of Andreas Grüntzig, M.D (1939-1985) Front Cardiovasc Med. 2014;1:15.
- [CrossRef] [Google Scholar]
- 30 years of balloon catheters: Andreas Grüntzig a Pioneer in Zurich. Switzerland Ärztezeit. 2004;85:346-5.
- [CrossRef] [Google Scholar]
- The History of Balloon Angioplasty. Available from: https://www.conceptmedical.com/blog/history-of-balloon-angioplasty [Last accessed on 2024 Sep 16]
- [Google Scholar]
- Endo-prothèses Coronariennes Auto-expansives dans la Prévention des Resténoses Après Angioplastie Transluminale. Etude Clinique Préliminaire [Self-Expanding Coronary Endoprosthesis in the Prevention of Restenosis Following Transluminal Angioplasty. Preliminary Clinical Study] Arch Mal Coeur Vaiss. 1987;80:1311-2.
- [Google Scholar]
- Intravascular Stents to Prevent Occlusion and Restenosis After Transluminal Angioplasty. N Engl J Med. 1987;316:701-6.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of Coronary in-stent Restenosis with a Paclitaxel-coated Balloon Catheter. N Engl J Med. 2006;355:2113-24.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical Expert Consensus Document on Drug-coated Balloon for Coronary Artery Disease from the Japanese Association of Cardiovascular Intervention and Therapeutics. Cardiovasc Interv Ther. 2023;38:166-76.
- [CrossRef] [PubMed] [Google Scholar]
- Design of Percutaneous Transluminal Coronary Angioplasty Balloon Catheters. Biomed Eng Online. 2023;22:94.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical Outcomes of a Non-compliant Balloon Dilatation Catheter: MOZEC™ NC Study. Int J Environ Res Public Health. 2022;19:16231.
- [CrossRef] [PubMed] [Google Scholar]
- Performing Percutaneous Coronary Interventions with Predilatation using non-compliant Balloons at High-pressure Versus Conventional Semi-Compliant Balloons: Insights from Two Randomised Studies using Optical Coherence Tomography. Open Heart. 2020;7:e001204.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical Experience with Very High-Pressure Dilatation for Resistant Coronary Lesions. Cardiovasc Revasc Med. 2019;20:1083-7.
- [CrossRef] [PubMed] [Google Scholar]
- Super High-pressure Balloon Versus Scoring Balloon to Prepare Severely Calcified Coronary Lesions: The ISARCALC Randomised Trial. EuroIntervention. 2021;17:481-8.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical Outcomes of the Proximal Optimisation Technique (POT) in Bifurcation Stenting. EuroIntervention. 2021;17:e910-8.
- [CrossRef] [PubMed] [Google Scholar]
- Finite Element Analysis of the Cutting Balloon with an Adequate Balloon-to-artery Ratio for Fracturing Calcification While Preventing Perforation. Circ Rep. 2020;3:1-8.
- [CrossRef] [PubMed] [Google Scholar]
- Improved Crossability with Novel Cutting Balloon Versus Scoring Balloon in the Treatment of Calcified Lesion. Cardiovasc Interv Ther. 2021;36:198-207.
- [CrossRef] [PubMed] [Google Scholar]
- Cutting Balloon to Optimize Predilation for Stent Implantation: The COPS Randomized Trial. Catheter Cardiovasc Interv. 2023;101:798-805.
- [CrossRef] [PubMed] [Google Scholar]
- Modified Balloons to Prepare Severely Calcified Coronary Lesions Before Stent Implantation: A Systematic Review and Meta-analysis of Randomized Trials. Clin Res Cardiol. 2024;113:995-1005.
- [CrossRef] [PubMed] [Google Scholar]
- For Percutaneous Transluminal Angioplasty. Available from: https://europe.medtronic.com/xd-en/healthcare-professionals/products/cardiovascular/ptaballoons/chocolate.html [Last accessed on 2024 Sep 18]
- [Google Scholar]
- First-in-Human Study of Paclitaxel Drug-Coated Chocolate Coronary Percutaneous Transluminal Coronary Angioplasty Balloon Catheter in De Novo Coronary Artery Lesions. JACC Cardiovasc Interv. 2019;12:2568-70.
- [CrossRef] [PubMed] [Google Scholar]
- A Randomized Multicenter Study Comparing a Paclitaxel Drug-Eluting Balloon with a Paclitaxel-Eluting Stent in Small Coronary Vessels: The BELLO (Balloon Elution and Late Loss Optimization) study. J Am Coll Cardiol. 2012;60:2473-80.
- [CrossRef] [PubMed] [Google Scholar]
- Drug-Coated Balloon for De Novo Coronary Artery Disease: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;75:1061-73.
- [CrossRef] [PubMed] [Google Scholar]
- The Fate of Coronary Dissections Left After Sirolimus-coated Balloon Angioplasty: A Prespecified Sub analysis of the EASTBOURNE Study. Catheter Cardiovasc Interv. 2023;102:979-86.
- [CrossRef] [PubMed] [Google Scholar]
- Should Paclitaxel be Considered an Old Generation DCB? The Limus Era. Rev Cardiovasc Med. 2021;22:1323-30.
- [CrossRef] [PubMed] [Google Scholar]
- The Evolution and Revolution of Drug Coated Balloons in Coronary Angioplasty: An up-to-date Review of Literature Data. Catheter Cardiovasc Interv. 2023;102:1069-77.
- [CrossRef] [PubMed] [Google Scholar]
- "Leave Nothing Behind" Strategy in Coronary and Peripheral Artery Disease: An Insight into Sirolimus-Coated Balloons. EMJ Int Cardiol. 2022;10:60-71.
- [CrossRef] [Google Scholar]
- Drug-Coated Balloon for Small Coronary Artery Disease in Patients with and without High-Bleeding Risk in the BASKET-SMALL 2 Trial. Circ Cardiovasc Interv. 2022;15:e011569.
- [CrossRef] [Google Scholar]
- Drug-Coated Balloon vs. Drug-Eluting Stents for De Novo Unprotected Left Main Stem Disease: The SPARTAN-LMS Study. J Cardiovasc Dev Dis. 2023;10:84.
- [CrossRef] [PubMed] [Google Scholar]
- Paclitaxel Drug-coated Balloon-only Angioplasty for De Novo Coronary Artery Disease in Elective Clinical Practice. Clin Res Cardiol. 2023;112:1186-93.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and Angiographic Outcomes of Elective Paclitaxel-Coated Balloon Angioplasty in Comparison with Drug-Eluting Stents for De Novo Coronary Lesions in Large Vessels. Int Heart J. 2023;64:145-53.
- [CrossRef] [PubMed] [Google Scholar]
- Drug-Coated Balloon Angioplasty for De Novo Lesions on the Left Anterior Descending Artery. Circ Cardiovasc Interv. 2023;16:e013232.
- [CrossRef] [PubMed] [Google Scholar]
- A New Frontier for Drug-Coated Balloons: Treatment of “De Novo” Stenosis in Large Vessel Coronary Artery Disease. J Clin Med. 2024;13:1320.
- [CrossRef] [PubMed] [Google Scholar]
- Sirolimus-coated Balloon Versus Everolimus-eluting Stent in De Novo Coronary Artery Disease: Rationale and Design of the TRANSFORM II Randomized Clinical Trial. Catheter Cardiovasc Interv. 2022;100:544-552.
- [CrossRef] [PubMed] [Google Scholar]
- Comparing a Strategy of sirolImus-eluting Balloon Treatment to Drug-eluting Stent Implantation in De Novo Coronary Lesions in all-comers: Design and Rationale of the SELUTION De Novo Trial. Am Heart J. 2023;258:77-84.
- [CrossRef] [PubMed] [Google Scholar]
- Paclitaxel-Coated Balloon vs Uncoated Balloon for Coronary in-Stent Restenosis: The AGENT IDE Randomized Clinical Trial. JAMA. 2024;331:1015-24.
- [CrossRef] [PubMed] [Google Scholar]
- Plain Old Perfusion Balloon Angioplasty: Can We Do Without Stents? J Soc Cardiovasc Angiogr Interv. 2023;3:101189.
- [CrossRef] [PubMed] [Google Scholar]
- Abstract 13394: Primary Perfusion Balloon Angioplasty in Primary Percutaneous Coronary Intervention for St-Segment Elevation Myocardial Infarction-The Novel Cardioprotective Revascularization Strategy. Circulation. 2022;146:13394.
- [CrossRef] [Google Scholar]
- An “IVL-First” Strategy Using 120 Pulses With the Next-Gen C2+ Shockwave Catheter. Available from: https://www.hmpgloballearningnetwork.com/site/cathlab/calcium-corner/ivl-first-strategy-using-120-pulses-next-gen-c2-shockwave-catheter [Last accessed on 2024 Oct 22]
- [Google Scholar]
- Intravascular Lithotripsy during Percutaneous Coronary Intervention: Current Concepts. Expert Rev Cardiovasc Ther. 2022;20:323-38.
- [CrossRef] [PubMed] [Google Scholar]
- Glider™ PTCA Balloon Catheter. Available from: https://www.teleflex.com/usa/en/product-areas/interventional/coronary-interventions/glider-ptca-balloon-catheter/index.html# [Last accessed on 2024 Oct 22]
- [Google Scholar]
- Complex Coronary Interventions with the Novel Mozec™ CTO Balloon: The MOZART Registry. Clin Med Insights Cardiol. 2015;9:91-6.
- [CrossRef] [PubMed] [Google Scholar]
- Bifurcation Percutaneous Coronary Intervention: Novel Techniques and Devices, what is their Future Application? EuroIntervention. 2018;14:e255-7.
- [CrossRef] [PubMed] [Google Scholar]
- Dedicated Bifurcated Balloon for Coronary Bifurcation Lesions: A Preclinical Proof of Concept. EuroIntervention. 2018;14:e314-5.
- [CrossRef] [PubMed] [Google Scholar]
- Coronary Balloon Shaft Fracture. Available from: https://www.pcronline.com/cases-resources-images/complications/implant-loss/coronary-embolised-devices/balloon-fracture/balloon-shaft-fracture [Last accessed on 2024 Sep 19]
- [Google Scholar]
- Coronary Balloon Fracture: Balloon Dysfunction (Undeflatable Balloon) Available from: https://www.pcronline.com/cases-resources-images/complications/implant-loss/coronary-embolised-devices/balloon-fracture/balloon-dysfunction [Last accessed on 2024 Sep 19]
- [Google Scholar]
- Coronary Entrapped Deflated Balloon During PCI. Available from: https://www.pcronline.com/Cases-resources-images/complications/implant-loss/coronary-embolised-devices/balloon-fracture/entrapped-balloon [Last accessed on 2024 Sep 19]
- [Google Scholar]
- Coronary Complications of Percutaneous Coronary Intervention: A Practical Approach to the Management of Abrupt Closure. Catheter Cardiovasc Interv. 2005;64:395-401.
- [CrossRef] [PubMed] [Google Scholar]







