Translate this page into:
Clinical and Angiographic Profile of Women with Acute Coronary Syndrome from a Large Tertiary Cardiac Care Center in South India – An Observational Study
*Corresponding author: Dr. Veena Nanjappa, Department of Cardiology, Sri Jayadeva Institute of Cardiovascular Science and Research Centre, Mysuru, Karnataka, India. drdchaitra84@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Doddamadaiah C, Nanjappa V, Raveesh H, Javaregowda DC, Sadananda KS, Nanjappa MC. Clinical and angiographic profile of women with acute coronary syndrome from a large tertiary cardiac care center in South India – An observational study. Indian J Cardiovasc Dis Women 2022;7:180-7.
Abstract
Objectives:
Acute coronary syndrome (ACS) is the leading cause of death in women. There are limited studies exclusively in Indian women presenting with ACS. This is the first largest study in south Indian women. To assess Demographic, clinical and angiographic profile of women with ACS.
Materials and Methods:
We collected data regarding baseline clinical, demographics, laboratory investigations, electrocardiogram, echocardiographic assessment, coronary angiogram details, treatment data, and outcomes in women presenting with ACS.
Results:
Majority were in the age group between 55 and 65 year (35.886%). Most common comorbidity seen in our study group is hypertension (59.90%), followed by Diabetes milletus (DM) (54.80%). ACS patients most frequently presented with ST-elevation myocardial infarction (STEMI)-AWMI in postmenopausal group, premenopausal women presented more commonly with non-STEMI. Though SVD is the most common presentation in our study, TVD is most commonly seen in premenopauasal (25.45%) compared to postmenopausal women (11.81%).
Conclusion:
Hypertension is the most common comorbidity seen in our study group, followed by DM. STEMI is the most common presentation. Higher mortality is seen in patients presenting late to the hospital and with higher Killip’s class. More studies are needed in women with ACS.
Keywords
Acute coronary syndrome
Coronary angiogram
ST-elevation myocardial infarction
Non-ST-elevation myocardial infarction
Unstable angina
ABSTRACT IMAGE
INTRODUCTION
Coronary artery disease is the leading cause of mortality in both developed and developing countries. Women have a longer time from symptom onset to presentation and are less likely to have guideline-directed treatment. This causes poor outcome in women as compared to men. There are limited studies regarding the clinical and angiographic profile of acute coronary syndrome in women in Indian scenario.
Cardiovascular disease has emerged as a major public health burden and a major cause of mortality in women in both developed and developing countries.[1,2] Significant differences in the prevalence of coronary artery disease (CAD) exist concerning gender, ethnicity, and age. It is predicted that more than half the worldwide cardiovascular disease risk burden will be borne by the Indian subcontinent in the next decade, according to a recent epidemiological study.[1] At any given age, the prevalence of CAD is greater in men than in women. As compared to men, women receive less medical attention in both rural and urban areas. Atherosclerotic plaque characteristics may differ by gender. It is said that women are protected from CAD by the protective hormones till menopause. However, recently, we are seeing a changing trend with acute coronary syndrome (ACS) increasing even in premenopausal women. Certain risk factors such as diabetes, metabolic syndrome, low high-density lipoprotein cholesterol and smoking are more causally related to CAD in women.[2,3]
A randomized sub-study of the Organization to Assess Strategies in Acute Ischemic Syndromes 5 trial in women presenting with an ACS suggests that women do worse with an early invasive strategy.[4] Although large trials including the women’s health initiative and the women’s ischemia syndrome evaluation have shed light on clinical characteristics, diagnosis, and outcome in women, they are largely western studies. In a study undertaken in Kerala at a tertiary center, women with ST-elevation myocardial infarction (STEMI) had higher mortality rates than males with STEMI.[5] In Kerala ACS registry,[6] the largest ACS data till date in the Indian scenario involving 25,748 patients over 2 years and across 125 centers had 22.6% women enrolment. There are limited studies on ACS exclusively in Indian women. Most of the data were taken from combined studies. In the present study, we aim to prospectively analyze the demographic, clinical risk factors, and angiographic profile of ACS in South Indian women presenting with the ACS in a tertiary cardiac care center.
Aim
The aim of this study was to assess the clinical profile, demographic factors, risk factors profile, angiographic profile, and severity of CAD in women presenting with the ACS and to compare the clinical profile, risk factors, and angiographic profile in premenopausal and postmenopausal age groups.
MATERIALS AND METHODS
It is a prospective observational single-center study conducted at Sri Jayadeva Institute of Cardiovascular Science and Research center, a tertiary cardiac center in Mysuru, Karnataka, India during the year 2020. Five hundred and twenty-nine consecutive women with a diagnosis of ACS after satisfying inclusion and exclusion criteria were chosen for the study. Baseline clinical, demographics, laboratory investigations, electrocardiogram, echocardiographic assessment, coronary angiogram (CAG) details, treatment data, and outcomes were recorded. STEMI, non-ST-elevation myocardial infarction (NSTEMI), and unstable angina (UA) were diagnosed following current guidelines. The data were collected from the patients and recorded in a pre-prepared case report form. Baseline data were recorded. The primary outcome was the overall rate of hospital admissions for ACS and deaths associated with ACS.
Inclusion criteria
The following criteria were included in the study:
Subjects willing to provide written informed consent.
All women presenting with ACS greater than 18 years of age were included in the study.
Exclusion criteria
Subject not willing to provide written informed consent.
Statistical analysis
The data are analyzed using Microsoft Excel and R-4.1.0 software. All the tests of significance are carried out at 5% level of significance. The descriptive results are displayed as subgroups of premenopausal and postmenopausal groups.
The numerical data are presented as mean and standard deviations. All the categorical data are presented as frequency and percentages. Descriptive statistics are used for frequency tables, summary statistics, and inferential statistics for independent sample t-test, which were used.
RESULTS
The mean age of patients is 43.94 ± 6.85 years in premenopausal age and 63.89 ± 9.51in the postmenopausal age group. There are 21 patients with age less than 45 years of age. There are 72 patients with age above 75 years. About 80.3% of patients belonged to the below poverty line group. About 89.6% of patients had attained menopause.
The mean BMI in the premenopausal group is 22.16 ± 5.287 kg/m2 and in the postmenopausal age group is 23.66 ± 4.584 kg/m2. Underweight is seen in 27.27% in the premenopausal group and 12.66% in the postmenopausal group. Overweight is seen in 27.8% and class II obesity seen in 1.9% of the study population. There are 85.1% non-vegetarians. There are 55.4% patients from the rural area [Table 1].
| Variable | Frequency | Percentage |
|---|---|---|
| Age | ||
| Range | 28–91 years | |
| Mean±SD | 43.94±6.85 years in premenopausal age and 63.89±9.51 in postmenopausal age group | |
| Less than 45 years | 24 | 4.5 |
| 45–55 | 97 | 18.3 |
| 55–65 years | 173 | 32.7 |
| 65–75 years | 163 | 30.8 |
| 75 years and above | 72 | 13.6 |
| Diet | ||
| Non-vegetarian | 450 | 85.1 |
| Vegetarian | 79 | 14.9 |
| Education | ||
| 10th or lower | 393 | 74.3 |
| Higher secondary | 83 | 15.7 |
| Degree | 40 | 7.6 |
| Postgraduation | 2 | 0.4 |
| Illiterate | 11 | 2.1 |
| BMI {kg/m2} | ||
| Range | ||
| Mean±SD | 22.16±5.29 kg/m2 | |
| Under weight (<18.5) | 75 | 14.2 |
| Normal weight (18.5–25) | 262 | 49.5 |
| Over weight (25–30) | 147 | 27.8 |
| Obese class I (30–35) | 34 | 6.4 |
| Obese class II (35–40) | 10 | 1.9 |
| Religion | ||
| Hindu | 475 | 89.8 |
| Islam | 51 | 9.6 |
| Christianity | 3 | 0.6 |
| Occupation | ||
| Home maker | 519 | 98.1 |
| Working | 10 | 1.9 |
| Area of living | ||
| Rural | 293 | 55.4 |
| Urban | 236 | 44.6 |
| Marital status | ||
| Not married | 2 | 0.5 |
| Married | 527 | 99.5 |
| Menstrual history | ||
| Premenopausal | 55 | 10.4 |
| Postmenopausal | 474 | 89.6 |
| Socio-economic status | ||
| Above poverty line | 104 | 19.7 |
| Below poverty line | 425 | 80.3 |
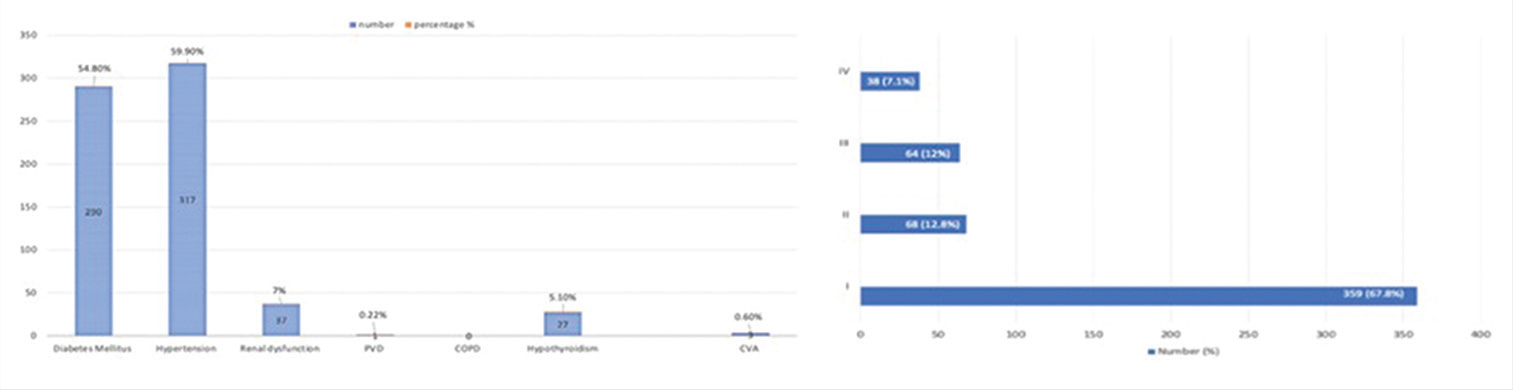
Time of onset of symptoms to reach the hospital: 178 patients (33.65%) with ACS reached hospital in less than 24 hours after symptom onset. 119(22.49%) patients presented within 24-48hours time period. 95(17.96%) presented in 48-72hours time period. 25.9% patients presented late after 72 hours. Typical chest pain during presentation seen in 97.5% of the study population. Atypical chest pain seen in 2.5%. Exertional dyspnea and exertional fatigue seen in 23.5% and 50% of the patients, respectively. Hypertension (59.90%) followed by diabetes mellitus (DM) (54.80%) is the most common comorbidity in our study group [Figure 1].
- Distribution of comorbidities among the study population.
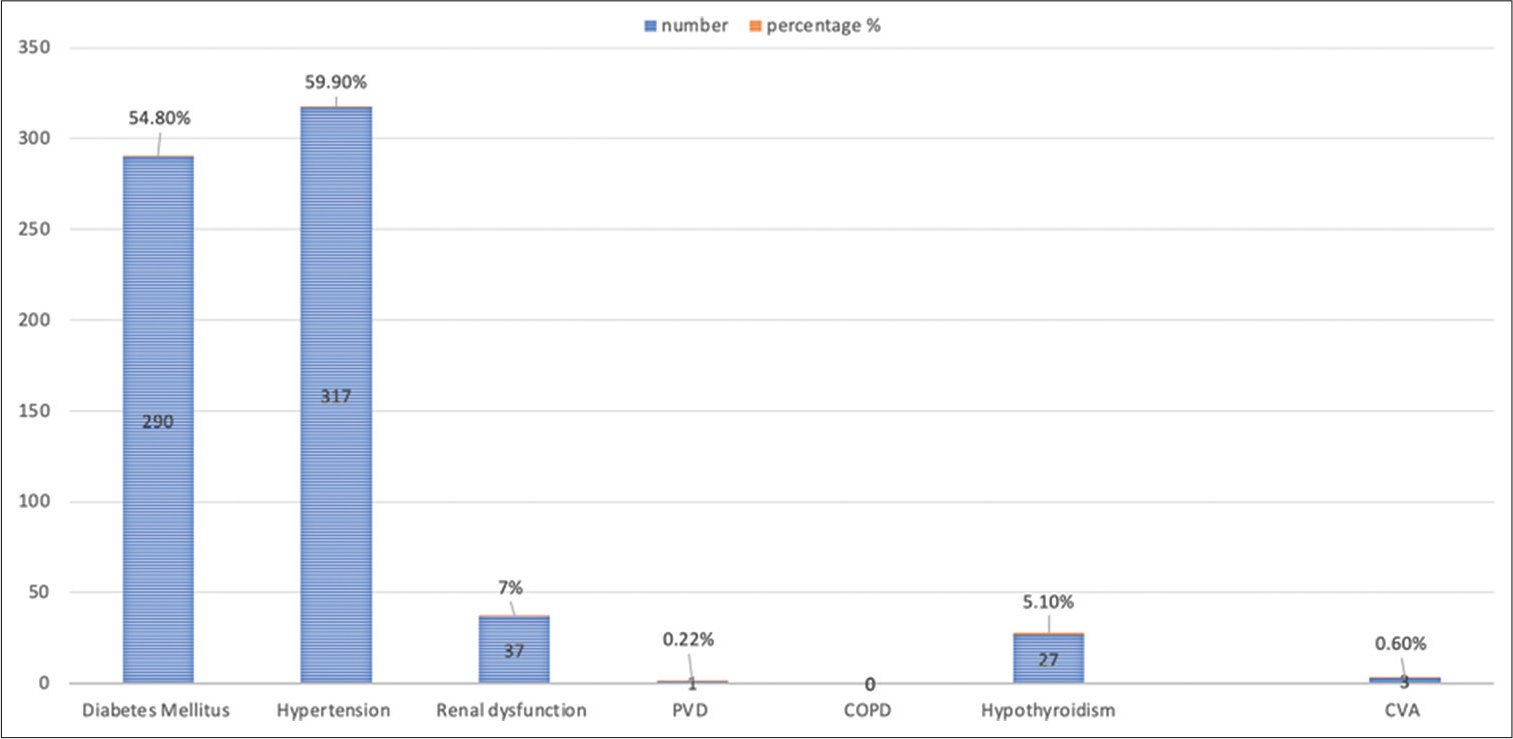
The presentation of ACS in our study group is STEMI – 62.38%, followed by NSTEMI – 24% and UA – 13.6%. Most common presentation is acute Anterior wall MI in the STEMI group followed by Inferior wall MI. Killip I presentation seen in 67.8% of the study population [Figure 2], followed by Killip’s III (5.8%) and Killip’s class IV (3.6%). In STEMI patients, moderate LV dysfunction seen in 25.7% and severe LV dysfunction seen in 2.27% [Tables 2 and 3].

- Killip’s score distribution among the study population.
| KILLIPS I | KILLIPS II | KILLIPS III | KILLIPS IV | |
|---|---|---|---|---|
| STEMI (330 [62.38%]) | ||||
| AWMI | 143 (27.0%) | 40 (7.5%) | 31 (5.8%) | 19 (3.6%) |
| IWMI | 16 (3.0%) | 3 (0.56%) | 3 (0.56%) | 2 (0.37%) |
| IWMI+RVMI | 14 (2.6%) | 6 (1.1%) | 5 (0.9%) | 3 (0.56%) |
| PWMI | 5 (0.9%) | 1 (0.1%) | 3 (0.56%) | 0 |
| IWMI+PWMI | 14 (2.6%) | 4 (0.7%) | 7 (1.3%) | 11 (2.0%) |
| NSTEMI | ||||
| Total 127 (24%) | 104 (19.6%) | 11 (2.0%) | 9 (1.7%) | 3 (0.56%) |
| UA | ||||
| Total 72 (13.6%) | 63 (11.9%) | 3 (0.56%) | 6 (1.1%) | 0 |
STEMI: ST-elevation myocardial infarction, NSTEMI: Non ST-elevation myocardial infarction, UA: Unstable angina
| EF % | Normal | Mild LV Dysfunction (40–49%) |
Moderate LV Dysfunction (30–39%) |
Severe LV Dysfunction (<30%) |
|---|---|---|---|---|
| STEMI | ||||
| AWMI | 31 (5.8%) | 70 (13.23%) | 124 (23.44%) | 8 (1.5%) |
| IWMI | 8 (1.5%) | 11 (2.0%) | 4 (0.75%) | 1 (0.18%) |
| IWMI+RVMI | 12 (2.2%) | 12 (2.2%) | 4 (0.75%) | 0 |
| PWMI | 4 (0.75%) | 5 (0.94%) | 0 | 0 |
| IWMI+PWMI | 15 (2.8%) | 16 (3.0%) | 2 (0.37%) | 3 (0.56%) |
| NSTEMI | 85 (16.0%) | 31 (5.8%) | 10 (1.8%) | 1 (0.18%) |
| UA | 58 (10.9%) | 8 (1.5%) | 6 (1.1%) | 0 |
STEMI: ST-elevation myocardial infarction, NSTEMI: Non ST-elevation myocardial infarction, UA: Unstable angina
CAG is done in 240 patients, in which non-obstructive CAD seen in 10.83%. About 36.67% presented with single-vessel disease. About 5.83% had LMCA involvement. Most common vessel involved is left anterior descending artery (LAD) (76.25%). PTCA procedure done in 69.17% of the patients who underwent CAG. Only 1% underwent CABG. Postprocedure access site hematoma is seen in three cases (0.75%) [Table 4].
| Total | Percentage | |
|---|---|---|
| CAG | 276 | 52.17 |
| n=276 | ||
| Normal Coronaries | 5 | 1.81 |
| Mild CAD | 24 | 8.7 |
| SVD | 128 | 46.38 |
| DVD | 67 | 24.28 |
| TVD | 70 | 25.36 |
| LMCA | 10 | 3.62 |
| LAD | 217 | 78.62 |
| LCX | 120 | 43.47 |
| RCA | 134 | 48.55 |
| RI | 7 | 2.54 |
| Advised – PTCA | 182 | 65.94 |
| Advised – OMT | 66 | 23.91 |
| Advised – CABG | 28 | 10.14 |
Diabetes is seen in 42.86% in premenopausal versus 54.59% in the postmenopausal age group. Hypertension was seen in 47.61% of premenopausal women and in 63.5% of post menopausal women. About 66.67% presented with STEMI in premenopausal group versus 54% in the postmenopausal group. NSTEMI seen in 36.5% of the postmenopausal group. About 9.07% patients presented with Killip’s IV in the postmenopausal group [Table 5].
| Premenopausal group (n=55) | Postmenopausal group (n=474) | P-value | |
|---|---|---|---|
| Age | 43.95±6.85 | 63.88±9.51 | <0.05 |
| BMI | 22.16±5.29 | 23.66±4.58 | >0.05 |
| Troponin T | 0.87±1.44 | 1.09±1.7 | |
| EF % | 48.53±9.50 | 44.57±10.54 | <0.05 |
| RBS | 160.0 9±101.54 | 201.29±126.15 | <0.05 |
| Total cholesterol | 177.05±33.36 | 177.6±44.32 | >0.05 |
| LDL | 105.42±17.76 | 116.26±34.6 | <0.05 |
| HDL | 41.93±4.90 | 41.71±10.91 | >0.05 |
| TG | 181.07±61.30 | 184.3 9±99.54 | >0.05 |
| Hb % | 12.2±1.69 | 12.1±1.67 | >0.05 |
| Blood urea | 34.49±13.94 | 33.92±17.29 | >0.05 |
| Serum creatinine | 0.99±0.40 | 1.04±0.41 | >0.05 |
| STEMI | |||
| AWMI | 13 (23.64%) | 220 (46.41%) | |
| IWMI | 6 (10.9%) | 18 (3.8%) | |
| IWMI+RVMI | 3 (5.45%) | 25 (5.27%) | |
| PWMI | 1 (1.82%) | 8 (1.69%) | |
| IWMI+PWMI | 5 (9.09%) | 31 (6.54%) | |
| NSTEMI | 15 (27.27%) | 112 (23.63%) | |
| UA | 12 (21.82%) | 60 (12.66%) | |
| DM | 22 (40%) | 268 (56.54%) | |
| Hypertension | 25 (45.45%) | 292 (61.6%) | |
| Hypothyroidism | 3 (5.45%) | 24 (5.06%) | |
| Killip’s score I | 49 (89.09%) | 310 (65.4%) | |
| Killip’s score II | 4 (7.27%) | 64 (13.5%) | |
| Killip’s score III | 0 | 64 (13.5%) | |
| Killip’s score IV | 2 (3.64%) | 48 (9.07%) | |
| Normal LV function | 29 (52.73%) | 180 (37.97%) | |
| Mild dysfunction | 14 (25.45%) | 136 (28.69%) | |
| Moderate dysfunction | 12 (21.82%) | 144 (30.38%) | |
| Severe dysfunction | 0 | 14 (2.95%) | |
| CAG | |||
| SVD | 8 (14.55%) | 102 (21.52%) | |
| DVD | 9 (16.36%) | 58 (12.24%) | |
| TVD | 14 (25.45%) | 56 (11.81%) | |
| Mild disease | 10 (18.18) | 14 (2.95%) | |
| Normal Coronaries | 1 (1.82%) | 4 (0.84%) | |
| PTCA | 22 (59.46%) | 160 (66.95%) | |
| OMT | 12 (21.81%) | 54 (11.39%) | |
| CABG | 4 (10.81%) | 24 (10.04%) | |
| Death | 2 (3.64%) | 81 (17.09%) | <0.05 |
STEMI: ST-elevation myocardial infarction, NSTEMI: Non ST-elevation myocardial infarction, UA: Unstable angina, CAG: Coronary angiogram, DM: Diabetes mellitus
Antiplatelets aspirin and clopidogrel are given as loading doses across all ACS groups; it was switched over to ticagrelor in 57.28% of cases. About 0.75% was on Prasugrel. Rest of the patients were continued on clopidogrel. About 59.35% were on beta-blockers and 51.22% were on ACE inhibitors. All patients received Statins.
Eighty-three patients died in hospital. Most common age group is 65–75 years (38.55%). No mortality seen in patients aged <45 years. Eighty-one (97.59%) patients were postmenopausal. About 87.95% belonged to below poverty line socioeconomic group. In patients who died, 56.62 % were hypertensive and 60.24% were diabetics. About 24.09% of patients had prior IHD. Chronic kidney disease seen in 3.61%. Fourteen (16.86%) patients had free wall rupture. Two (2.4%) patients had ventricular septal rupture. Twenty-nine (34.93%) and 34 (40.96%) patients had severe and moderate LV dysfunction, respectively. Twenty-three (27.71%) were in Killip’s class III and 55 (66.26%) were in Killip’s IV at presentation. About 89.15% had STEMI, with majority having AWMI (57.83%). Sixty-six patients (79.5%) patients died within 24 h of admission. About 33.73% of patients died within 6 h of admission. Of the ten patients in the mortality group who underwent CAG, four of them had triple-vessel disease. Killip’s classes III and IV, moderate LV dysfunction, underweight patients, and those from the urban area were found to be independent predictors of death on risk estimate analysis of in-hospital mortality.
DISCUSSION
The present study is the largest single-center data of ACS in women from the country. Cardiovascular disease is presently the most common cause of mortality in women. The major ACS trials that guide daily clinical practice disproportionately enrolled men. Women with ACS have more comorbidities than men and traditional risk factors affect the cardiovascular system differently in women[7] due to which the prognosis is also very poor in women. Receptors for estrogen, progesterone, and testosterone are expressed in varying numbers in both the endothelium and vascular smooth muscle of multiple vascular systems[8] and are one of the proposed mechanisms responsible for gender difference in vascular tone.
The mean age of presentation in the present study is 43.94 ± 6.85 years in premenopausal age and 63.89 ± 9.51 years in the postmenopausal age group as compared to 64.4 + 11 years in a study done by Nanjappa et al.[8] The mean age is higher when compared to a study done by Mahajan et al.[8,9] Most women, in our study, were postmenopausal (84.25%), whereas it was 79.7% in a study by Mahajan et al.[10] and Rissam et al.[11] and 90.2% in Nanjappa et al.[8] About 36.1% patients had obesity (BMI >25 kg/m2).
About 40% of premenopausal and 56.54% of the postmenopausal group had DM and 45.45% of premenopausal and 61.6% in the postmenopausal group had hypertension.
These were the most common comorbidities, which were comparable other studies.[9] This contrasts with Mahajan et al.[10] study, in which the prevalence of diabetes was only 20.6% and hypertension was 69.7%. This shows that diabetes was more prevalent in women in South India compared to North India. About 30.4% and 37.7% in CREATE registry[12] and 30.2% and 29.6% in INTERHEART[7] study had diabetes and hypertension, respectively. These registries encompassed both men and women.
In our study, LDL cholesterol level is above 100 mg/dl in both pre- and post-menopausal women with P-value being significant. We could not find significant increase in total cholesterol triglyceride level in our study which highlights that though there is no major dyslipedimia, but still females in our study group suffered ACS.
Majority of our patients were in postmenopausal age group. Killip class IV presentation is predominantly seen in postmenopausal women. About 38.6% of women had Killip’s class II–IV in SWEDEHEART study.[13] Associations between higher androgen and lower estrogen levels with CAD risk factors in postmenopausal women, including, insulin resistance, C-reactive protein, and blood pressure exist.[15-16] In the present study, anemia is seen in 55% of cases and dyslipidemia with elevated LDL cholesterol was seen in 66% cases.
STEMI (62.38%) is the most common presentation in our study, followed by NSTEMI (24%) and UA (13.6%) which are comparable to other studies.[8] About 50.9% of premenopausal women and 54% of postmenopausal patients had STEMI at presentation.
In the present study, 45.36% of patients underwent CAG; the rest were treated medically. This contrasts with Nanjappa et al.[8] study. The reason could be that the present study involved more of rural than urban population compared to the latter study which was conducted in purely urban population. Among patients who underwent CAG, majority had single-vessel disease (76.25%) with LAD being the most common culprit vessel in 36% of cases, which is comparable to a study from Singapore, where 90% of women with Indian ethnicity had single-vessel disease.[14] Double-vessel disease and triple-vessel disease were seen in 25.83% and 25.41%, respectively. About 69.17% of CAG patients underwent percutaneous coronary intervention (PCI) procedure. In comparison, PCI was done in only 11.9% of patients in the Kerala ACS registry and 7.5% in CREATE registry. About 47.8% underwent PCI in a study by Sadowski et al.[15]
LMCA involvement was seen in 5.83% which is comparable to Mahajan et al.[9] study and 3.4% in a study by Ezhumalai and Jayaraman[16] In the CADILLAC trial,[17] female gender was an independent predictor of MACE and bleeding complications, although comorbid risk factors and body surface area, and not gender, predicted 1-year mortality.
Eighty-three deaths were noted. Deaths noted in our study were higher compared to the registry data. This could be explained by the fact that our center caters to 5–6 surrounding districts with a predominantly agrarian population. Most of the deaths happened within 24 h of admission. About 75.89% were in Killip’s classes III and IV at presentation. Delayed recognition of symptoms and presentation to the hospital at a later severe stage of the illness could explain the higher deaths. This study period overlapped with the COVID pandemic, and this could have also influenced the health-seeking behavior of patients. About 3.9% in the Kerala ACS[6] registry had in-hospital mortality with 8.2% in the STEMI group. In the AMI-FLORENCE registry, the in-hospital mortality for women was 16%.[18]
CONCLUSION
This prospective observational study in a large tertiary cardiac care center of South India illustrates significant differences in the clinical risk profile and angiographic disease pattern among premenopausal and postmenopausal women. Majority of the patients belonged to 55–65 years age group. Majority of the patients had typical chest pain and fatiguability as clinical manifestation. The most common comorbidities seen in our study group which is hypertension followed by DM. There is only a marginal difference in distribution of patients from urban and rural areas which are alarming, highlighting the fact that CAD is no more a disease limited to urban population. This fact will have cascading effect on health economic policies and the need for stringent addressal of risk factors and prevention of these risk factors at primary health-care level and robust system of linking the primary care to tertiary centers for better health-care delivery. The most common presentation is STEMI. Higher mortality is seen in patients presenting late to the hospital and with higher Killip’s class. More studies involving women with the focus on demographic, clinical risk profile, CAD, and treatment strategies pattern would help in the formulation of evidence-based guidelines to prevent and treat optimally.
“A heart-healthy woman for a healthy society.”
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflict of interest.
Audio summary available at
https://doi.org/10.25259/mm_ijcdw_349
References
- Epidemiological and causation of coronary heart disease and stroke in India. Heart. 2008;94:16-26.
- [CrossRef] [PubMed] [Google Scholar]
- Excess risk of fatal coronary heart disease associated with diabetes in men and women: Meta-analysis of 37 prospective cohort studies. BMJ. 2006;332:738.
- [CrossRef] [PubMed] [Google Scholar]
- Metabolic syndrome and risk of incident cardiovascular events and death: A systematic review and metaanalysis of longitudinal studies. J Am Coll Cardiol. 2007;49:40314.
- [CrossRef] [PubMed] [Google Scholar]
- Early invasive compared with a selective invasive strategy in women with non-ST-elevation acute coronary syndromes: A sub study of the OASIS 5 trial and a meta-analysis of previous randomized trials. Eur Heart J. 2012;33:51-60.
- [CrossRef] [PubMed] [Google Scholar]
- The clinical spectrum of acute coronary syndromes: Experience from a major center in Kerala. J Assoc Physicians India. 2009;57:377-83.
- [Google Scholar]
- Presentation, management, and outcomes of 25 748 acute coronary syndrome admissions in Kerala, India: Results from the Kerala ACS Registry. Eur Heart J. 2013;34:12129.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): Case-control study. Lancet. 2004;364:937-52.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical profile and 30-day outcome of women with acute coronary syndrome as a first manifestation of ischemic heart disease: A single-centre observational study. Indian Heart J. 2016;68:164-8.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and coronary angiographic profile in women presenting with anginal chest pain: Results from a single-centre prospective observational study. J Nat Sci Biol Med. 2019;10:60-7.
- [CrossRef] [Google Scholar]
- Gender differences in the management of acute coronary syndrome patients: One year results from HPIAR (HP-India ACS Registry) Int J Cardiol. 2017;248:1-6.
- [CrossRef] [PubMed] [Google Scholar]
- Coronary artery disease in young Indians: The missing link. J Indian Acad Clin Med. 2001;2:128-32.
- [Google Scholar]
- Treatment and outcomes of acute coronary syndromes in India (CREATE): A prospective analysis of registry data. Lancet. 2008;371:1435-42.
- [CrossRef] [PubMed] [Google Scholar]
- Time trends in STEMI-improved treatment and outcome but still a gender gap: A prospective observational cohort study from the SWEDEHEART register. BMJ Open. 2012;2:e000.
- [CrossRef] [PubMed] [Google Scholar]
- Acute myocardial infarction in young Asian women: A comparative study on Chinese, Malay and Indian ethnic groups. Singapore Med J. 2011;52:835-9.
- [Google Scholar]
- Gender-related differences in mortality after ST-segment elevation myocardial infarction: A large multicentre national registry. Euro Interv. 2011;6:1068-72.
- [CrossRef] [PubMed] [Google Scholar]
- Angiographic prevalence and pattern of coronary artery disease in women. Indian Heart J. 2014;66:422-6.
- [CrossRef] [PubMed] [Google Scholar]
- Gender differences in outcomes after primary angioplasty versus primary stenting with and without abciximab for acute myocardial infarction: Results of the controlled abciximab and device investigation to lower late angioplasty complications (CADILLAC) trial. Circulation. 2005;111:1611-8.
- [CrossRef] [PubMed] [Google Scholar]
- In-hospital management and outcome in women with acute myocardial infarction (data from the AMI-Florence Registry) Am J Cardiol. 2004;94:1118-23.
- [CrossRef] [PubMed] [Google Scholar]







