Translate this page into:
Association of Oral Health and Periodontal Disease with Hypertension: A Cross-Sectional Study
*Corresponding author: Prerna Goyal, Department of Medicine, RG Stone and Super Speciality Hospital, Ludhiana, Punjab, India drprerna156@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Uppal B, Goyal P, Walia NK. Association of Oral Health and Periodontal Disease with Hypertension: A Cross-Sectional Study. Indian J Cardiovasc Dis Women. 2024;9:206-12. doi: 10.25259/IJCDW_5_2024.
Abstract
Objectives:
The association of orodental and cardiovascular health has been an area of extensive research for many years. As per American Heart Association hypertension 2017 guidelines, good periodontal health is associated with better systolic blood pressure control. However, there have been conflicting results for hypertension and dental correlation in a few other studies. Moreover, there are no recognized oral manifestations, seen in patients with hypertension. Indian data on this subject are scarce. Therefore, the present study was contemplated to determine the frequency and nature of oral manifestations in hypertensive patients as compared to normotensive patients.
Materials and Methods:
In this observational cross-sectional study, participants were divided into two groups. Group A included 40 hypertensive subjects and group B included 40 healthy normotensive volunteers. Oral symptoms such as dry mouth, altered taste sensation, mouth odor, and bleeding from gums were noted. An oral examination was performed to check periodontal pockets, lichenoid reactions, and gingival hyperplasia. Russell’s Periodontal Index was used to estimate gingival and periodontal health.
Results:
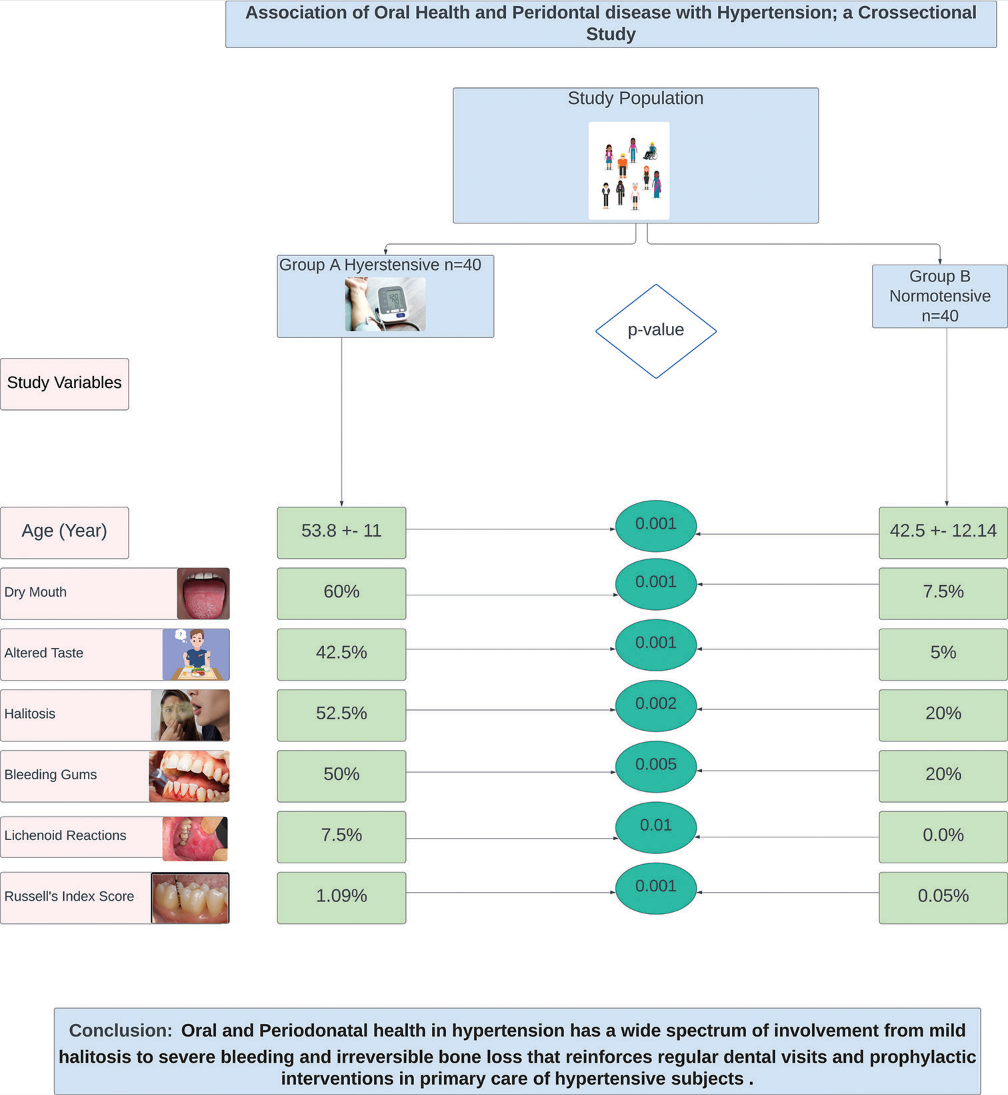
The mean age of patients in the hypertensive group was higher than normotensive groups (53.8 ± 11 vs. 42.45 ± 12, P = 0.001). Oral symptoms in the form of dry mouth, halitosis, and altered taste were reported in 60%, 52.5%, and 42.5% of hypertensive patients which were significantly higher as compared to the control group. Bleeding gums, lichenoid reactions, and gingival enlargement were also significantly higher in hypertensive than normotensive groups. The mean value of Russell’s index was 1.09 ± 0.41 in group A which was significantly different from group B (0.05 ± 0.10). Gingival hyperplasia and gum bleeding were predominantly found in patients on calcium channel blockers, whereas lichenoid reactions were significantly present in patients on angiotensin receptor blockers. Hyposalivation was reported with all four classes of antihypertensive drugs, predominantly diuretics.
Conclusion:
The orodental involvement in hypertensive subjects has a wide spectrum from mildly symptomatic halitosis and dryness of mouth to severe bleeding gums, lichenoid lesions, irreversible bone loss, and periodontitis that may require dental visits and interventions. The documented mucosal changes can also be attributed to antihypertensive drugs. Regular dental examinations should be made part of routine screening programs of hypertensive patients to protect them from various oral complications and subsequent inflammation-mediated changes in vasculature endothelium.
Keywords
Periodontal health
Hypertension
Gingival hyperplasia
Dryness mouth
Periodontitis
ABSTRACT IMAGE
INTRODUCTION
Hypertension has been attributed as the leading cause of cardiovascular (CV) morbidity and mortality with rising prevalence worldwide. Uncontrolled high blood pressure (BP) has become a major health concern both in developed as well as developing nations. It is common and may remain asymptomatic and undetectable in the vast majority. Therefore, it remains untreated despite easily available and affordable treatment options.
Numerous epidemiological studies have reported that many systemic diseases such as hypertension, diabetes, fatty liver, and infections are incidentally discovered during a routine visit to a dentist.[1] The human oral cavity is an ideal breeding area for bacteria, especially in patients with poor orodental hygiene. Periodontitis is one such chronic infectious disease of the gums, in which bacteria may gain entry into the bloodstream through oral mucosa and can contribute to fatal systemic infections.[2,3] Apart from this, locally formed inflammatory mediators may set the ground for low-grade systemic inflammation, leading to increased CV risk.
The association between orodental health and CV health has been extensively discussed in the literature. However, there have been conflicting results for hypertension and dental correlation. Unhealthy oral and periodontal health have been associated with high BP in a few studies. The American Heart Association (AHA) in its 2017 hypertension guidelines also mentions that good periodontal health is associated with better systolic BP control.[1,4] Whereas a population-based study by Galit et al. found no such significant association between hypertension and dental status.[5]
Moreover, there are no recognized oral manifestations which have been documented in patients with hypertension but the patients who are on anti-hypertensive drugs can exhibit various oral side effects such as gingival overgrowth, salivary gland swelling, xerostomia, pain, lichenoid drug reactions, erythema multiforme, halitosis, and altered taste sensations. Indian data on this subject are scarce. Kumar et al.[6] reported the association of gingival and periodontal pathologies in hypertensive Indian subjects.
Therefore, the present study was contemplated to know the association between oral health and periodontal state with hypertension and anti-hypertensive drugs.
Aims and objectives
The objectives of this study were as follows:
Primary objective
To determine the frequency and nature of oral manifestations in hypertensive patients as compared to normotensive patients.
Secondary objective
To study the effect of antihypertensive drugs on orodental mucosa.
MATERIALS AND METHODS
Study design
This was an observational cross-sectional study. In this study, we enrolled known hypertensive patients in group A and healthy normotensive volunteers in group B who visited our dental outpatient department.
Inclusion criteria
The following criteria were included in the study:
For cases
Adults above 18 years of age with confirmed hypertension.
For controls
Healthy adults above 18 years of age in the absence of any systemic disease.
Exclusion criteria
The following participants were excluded from both groups – pregnant females, epileptic patients, patients having diabetes, chronic kidney disease, chronic liver disease, cancer patients, those on radiotherapy or chemotherapy, or those who were on any other drug therapy that could have affected oral health (especially statins and aspirin).
The study protocol was approved by the Research Ethics Committee of Baba Jaswant Singh Dental College and Hospital, Ludhiana. Written informed consent was obtained from all participants.
Clinical assessment
After taking signed informed consent, complete clinical and anthropometric assessments were done. Information on height, weight, diabetes, smoking, alcohol, BP, duration of hypertension, and types of anti-hypertensives taken was collected. BP of all the patients was recorded. Hypertension was defined by systolic BP >140 and diastolic BP >80 mm of Hg or patients who were on anti-hypertensive drugs. Oral symptoms such as dry mouth, altered taste sensation, mouth odor, and bleeding from gums were noted. This was followed by a complete oral examination.
Clinical examination was performed using a mouth mirror, probe, and Williams periodontal probe to check periodontal pockets. Buccal mucosa was checked for the presence of lichenoid reactions, which looked as bilateral whitish linear striations in the posterior region. Gingival hyperplasia was noted which appeared as firm to hard nodular gingival overgrowth.
Russell’s Periodontal Index (PI) was used to estimate gingival and periodontal health. Oral changes such as gingivitis and periodontitis were observed. All teeth were examined and gingival tissue surrounding each tooth was taken as a single unit for calculation of individual tooth score. A person’s overall PI was calculated by adding all individual tooth scores and dividing it by the total number of teeth.
PI is a very reliable clinical assessment tool to measure periodontal health, named after an American Dentist A. L. Russell. This is a composite index which estimates the spectrum of periodontal disease from milder, reversible gingival inflammation to more severe, deeper, and irreversible bone loss in the form of periodontitis on a scale of 0–8. The index has been validated in epidemiological surveys. Table 1 shows an interpretation of Russell’s score according to the extent of periodontal disease.
| Russel’s Periodontal Index score | Clinical condition | Stage of involvement |
|---|---|---|
| 0–0.2 | Clinically normal tissue | |
| 0.3–0.9 | Simple gingivitis | |
| 1.0–1.9 | Beginning of destructive periodontal disease | Reversible |
| 2.0–4.9 | Established destructive periodontal disease | Irreversible |
| 5.0–8.0 | Terminal disease | Irreversible |
Statistical analysis
The data were analyzed using the Statistical Package for the Social Sciences Version 24 software. Descriptive statistics in the form of mean and standard deviation were used for continuous variables and inter-group comparisons were done with t-test. Frequency (n) and percentage (%) were calculated for categorical variables with inter-group comparison performed by Chi-square (χ2) test. Two-tailed P < 0.05 was considered statistically significant.
RESULTS
A total of 116 patients were enrolled in the study over 4 month period. Forty patients with a history of hypertension, who were consuming regular anti-hypertensives were included in group A, while 40 patients with no systemic disease were included in group B, as controls. The mean age of patients in the hypertensive group was 53.8 ± 11 years whereas the mean age in the control group was 42.45 ± 12 years with a significant P-value [0.001, Table 2]. The mean duration of hypertension in group A was 6.81 ± 3.16 years. Both the groups differed significantly in their mean systolic BP (130.43 ± 14 vs. 123.75 ± 6, P = 0.011), but not in mean diastolic BP (81.10 ± 4.98 vs. 80.2 ± 3.9). There were 22 (55%) males and 18 (45%) females in group A, whereas 25 (62.5%) males and 15 (37.5%) females in group B, without any statistical significance. Body weight, smoking, and alcoholism were not found to be significantly different between both groups. Table 2 shows the various demographic and clinical variables between the two groups.
| Variable | Group A (Hypertensive) |
Group B (Normotensive subjects) |
Chi-square/z-value | P-value |
|---|---|---|---|---|
| Age (years) | 53.8(11) | 42.45(12.14) | 4.383 | 0.001 |
| Males | 22(55.0%) | 25(62.5%) | 0.464 | 0.496 |
| Weight (kg) | 66.5(11.3) | 63.08(7.92) | 1.559 | 0.123 |
| SBP (mm Hg) | 130.4(14.7) | 123.75(6.48) | 2.622 | 0.011 |
| DBP (mm Hg) | 81.1(4.98) | 80.00(0.00) | 1.397 | 0.166 |
| Alcohol | 0(0.0%) | 1(2.5%) | 1.013 | 0.314 |
| Smoking | 0(0.0%) | 2(5.0%) | 2.051 | 0.152 |
| Thyroid | 2(5.0%) | 1(2.5%) | 0.346 | 0.556 |
| Dry mouth | 24(60.0%) | 3(7.5%) | 24.654 | 0.001 |
| Altered taste | 17(42.5%) | 2(5.0%) | 15.53 | 0.001 |
| Halitosis | 21(52.5%) | 8(20.0%) | 9.141 | 0.002 |
| Bleeding gums | 20(50.0%) | 8(20.0%) | 7.912 | 0.005 |
| Lichenoid reactions | 3(7.5%) | 0(0.0%) | 15.522 | 0.01 |
| Russel’s index | 1.09(0.41) | 0.05(0.10) | 15.788 | 0.001 |
| Intervention required | 28(70.0%) | 1(2.5%) | 70.4 | 0.001 |
Data are expressed as mean (standard deviation) or number (percent). SBP: Systolic blood pressure, DBP: Diastolic blood pressure
Oral and periodontal health assessment
Oral symptoms in the form of dry mouth, halitosis, and altered taste were reported in 60%, 52.5%, and 42.5% of hypertensive patients which were significantly higher as compared to the control group [P = 0.001, 0.002, and 0.001, respectively, Table 2 and Figure 1].
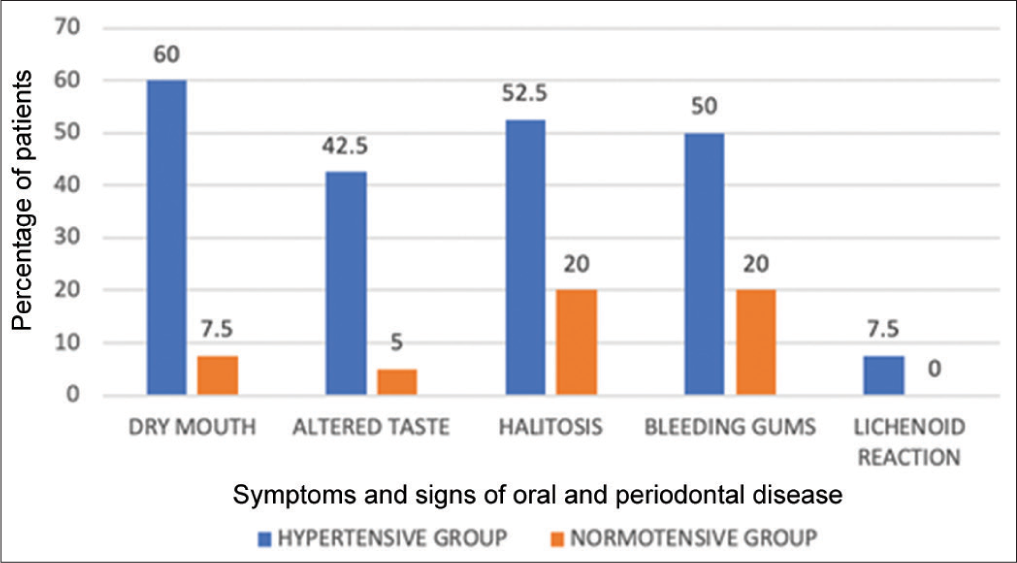
- Graph showing periodontal signs and symptoms of statistical significance in hypertensives and normotensives.
Bleeding gums due to gingival inflammation was seen in half (50%) of participants in hypertensive group which was significantly different from the control group (P = 0.005). Similarly, lichenoid reactions were seen in 3 (7.5%) of hypertensives whereas not a single participant in the control group had a lichenoid-type lesion in the oral cavity (P = 0.001) [Figure 2]. Gingival enlargement was seen in 7 (17.5%) of hypertensive patients. The mean value of Russell’s Index was 1.09 ± 0.41 in group A which was significantly different from group B (0.05 ± −0.10) [Table 3]. Thereby, all 40 (100%) patients in hypertensive group had been advocated prophylactic intervention according to their score, whereas only 1 (2.5%) patient in control group had advocated intervention [Table 2]. Twenty-eight (70%) patients from group A had Russel’s score of 1–1.9 and 12 (30%) patients had a score of 0.3–0.9.
| Number of patients (n, %) | Number of patients with oral manifestations | |
|---|---|---|
| Class of anti-hypertensive drugs | ||
| ARBs alone | 5 (12.5) | Lichenoid lesions – 1 Dry mouth – 4 |
| CCBs alone | 6 (15) | Gingival overgrowth – 3 Bleeding gums – 6 Dry mouth – 3 |
| Combination of drugs | ||
| ARBs+CCBs | 12 (30) | Gingival overgrowth – 4 Dry mouth – 6 Bleeding gums – 9 |
| ARBs+Diuretics | 9 (22.5) | Dry mouth – 7 |
| ARBs+ Beta-blockers +CCBs | 8 (20) | Lichenoid lesions – 2 Dry mouth – 4 Bleeding gums – 5 |
ARBs: Angiotensin receptor blockers, CCBs: Calcium channel blockers

- Lichenoid lesion in a hypertensive adult.
All patients were taking antihypertensive drugs mainly in the form of angiotensin re ceptor blockers (ARBs), calcium channel blockers (CCBs), beta-blockers, and diuretics (hydrochlorothiazide). Beta-blockers were used in 8 (20%) patients only as a part of triple combination therapy and diuretics were also given as a part of dual combination therapy in 9 (22.5%) patients. Table 3 shows the frequency distribution of patients on treatment with different classes of antihypertensive therapies. Combination therapies were used by the majority of patients in the following frequency – ABRs in combination with CCBs in 12 (30%), ARBs and diuretics in 9 (22.5%), and ARBs in combination with CCBs and diuretics in 8 (20%) patients. ARBs and CCBs were used alone in 5 (12.5%) and 6 (15%) patients. Gingival hyperplasia and gum bleeding were predominantly found in patients on CCBs, whereas lichenoid reactions were significantly present in patients on ARBs. Hyposalivation was reported with all four classes of antihypertensive drugs, predominantly diuretics.
DISCUSSION
This study conducted in a dental institute, found a significant association between antihypertensive drugs and oral-dental manifestations. The majority of the subjects included in our study were middle-aged adults with an average duration of hypertension of 6 years. The highest age reported was 62 years with a maximum number of patients found in the age group 40–50 years, which was similar to a study by Elmi Rankohi et al.[7] Hypertensive males were relatively more in number than hypertensive females, but the orodental involvement did not show any significant gender differences. Similar gender-neutral results had been shown by Habbab et al.[8] and Elmi Rankohi et al.[7] in their research papers.
The most common symptom noted in hypertensive patients in our study was dryness of the mouth (60%) whereas a study by Kumar et al.[6] had reported hyposalivation in 16.9% and Elmi Rankohi et al.[7] in 40% of patients. The reported differences can be attributed to differences in the parameters which were used to assess salivation and the effect of pharmacotherapies, predominantly diuretics in different study groups. The dryness of mouth was reported more in higher age groups whereas no significant correlation was found between age and other periodontal findings. The findings are similar to the study by Shirzaiy and Bagheri[9] and Elmi Rankohi et al.[7] who also reported an age-related increase in the dryness of mouth, most likely due to changes in oral mucosa with increasing age.
We reported gingival bleeding, lichenoid lesions, and gum hyperplasia in 50%, 7.5%, and 17.5% of hypertensive patients, respectively. The corresponding figures were 85.38% for gum bleeding, 4.5% for lichenoid, and 16.9% for gum hyperplasia in a study by Kumar et al.[6] Elmi Rankohi et al.[7] reported lichenoid lesions in only 0.7% of patients. Lichenoid lesions are lupus-like whitish changes in the buccal mucosa, characterized by basal cell degeneration, hyperkeratosis, acanthosis, and chronic inflammatory infiltration on histopathology. Harting and Hsu[10] and Kumar et al.[6] reported a correlation between arterial hypertension and oral lichen planus-like lesions similar to our study but Christensen et al.[3] did not find any significant association between both.
The average Russell’s Index was 1.09 ± 0.41 in our study population. In a study by Kumar et al.[6] and Maiborodin et al.,[2] the Russell’s Index was shown to be 2.0–4.9. Our 70% of hypertensive patients had Russell’s Index of 2, which means that they had established destructive periodontal disease and 30% had Russell’s Index of 1, which means that they had the beginning of destructive periodontal disease. Thus, all hypertensive study participants had some degree of destructive periodontal involvement, the majority being in an irreversible stage. Hypertension has been implicated in the pathophysiology of periodontitis. The proposed mechanisms include lymho-hemocirculatory changes in gingival mucosa with widening of lymphatic and interstitial spaces and inflammatory reaction leading to a higher risk of periodontitis in hypertensive subjects.[2,11]
We did not find any case of angioedema in our study population. With regard to antihypertensive drugs, we found a greater use of ARBs and CCBs in our study population. This is in contrast to previous studies where beta-blockers have been reported in a greater number of studied populations. Arunkumar et al., in their study, reported greater use of beta-blockers and CCBs.[12] In another study, simultaneous use of ARBs and beta-blockers followed by ARBs alone had the highest frequency of use in the study population.[7] William and Elliott reported beta-blockers and angiotensin-converting enzymes alone as the main drug used in their study group.[13] The dissimilarities can be explained by the differences in the respective national hypertension guidelines, personal preferences, and expertise of the regional health-care providers along with geographical differences in the availability.
Gum hyperplasia and bleeding were found to be significantly more in patients on CCBs, dryness of mouth in patients on diuretics, and lichenoid reactions in patients on ARBs with beta-blockers. Tenovuo[14] and Kumar et al.[6] also reported hyposalivation in patients on diuretics similar to our results.
The strength of our study was that we examined a wide spectrum of oral and periodontal involvement in patients of hypertension which included dryness, altered taste, halitosis, mucosal bleeding, gum hyperplasia, angioedema, and lichenoid lesions along with Russell’s Index which provided a robust measure of periodontal health. We have limited Indian data on hypertension and periodontal health. Our study provides a comprehensive overview of types of oral manifestations in Indian hypertensive patients, which remains neglected in the majority. The limitation is that we cannot rule out whether the orodental involvement is secondary to antihypertensive drug effects or hypertension per se as all study participants were already taking antihypertensive drugs.
CONCLUSION
We conclude that there is a significant association between consumption of antihypertensive drugs and oral manifestations. The orodental involvement has a wide spectrum from mildly symptomatic halitosis and dryness of mouth to severe bleeding gums, lichenoid lesions, irreversible bone loss, and periodontitis which may require dental visits and interventions. As almost all our study patients had periodontitis, thus, it became the responsibility of the clinician to advise them of regular dental examinations as a part of their annual screening programs to protect from various oral complications. The documented mucosal changes can be attributed to antihypertensive drugs. It might not be easy to stop the offending antihypertensive drug which is providing so many other CV benefits but regular dental prophylaxis can be offered to them to avoid these adverse dental complications. Moreover, by preserving the orodental milieu, we may achieve better BP control in our difficult-to-control hypertensive subjects by suppressing the inflammatory surge and confer our hypertensive population long-term CV protection.
Ethical approval
The research/study was approved by the Institutional Review Board at Baba Jaswant Singh Dental College Hospital and Research Institute, number EC/BJS/04/23, dated 4th November 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Prerna Goyal is on the editorial board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Audio summary available at
Financial support and sponsorship
Nil.
References
- Poor Oral Health NEGATES Benefits of Antihypertensive Treatment: A Re-analysis of NHANES Data Based on 2018 ESC/ESH Hypertension Guidelines. J Hypertens. 2019;37:e11.
- [CrossRef] [Google Scholar]
- Changes in Gum in Cases of Arterial Hypertension Combination with Periodontitis. Stomatologiia (Mosk). 2005;84:15-9.
- [Google Scholar]
- Arterial Blood Pressure in Patients with Oral Lichen Planus. J Oral Pathol. 1977;6:139-42.
- [CrossRef] [Google Scholar]
- Association between Periodontitis and Blood Pressure Highlighted in Systemically Healthy Individuals: Results from a Nested Case-Control Study. Hypertension. 2021;77:1765-74.
- [CrossRef] [PubMed] [Google Scholar]
- Hypertension and Its Associations with Dental Status: Data from the Dental, Oral, Medical Epidemiological (DOME) Nationwide Records-Based Study. J Clin Med. 2021;10:176.
- [CrossRef] [PubMed] [Google Scholar]
- Oral Manifestations in Hypertensive Patients: A Clinical Study. J Oral Maxillofac Pathol. 2012;16:215-21.
- [CrossRef] [PubMed] [Google Scholar]
- Oral Manifestations of Patients Taking Anti-Hypertensive Medications. J Islam Dent Assoc Iran. 2020;32:83-8.
- [CrossRef] [Google Scholar]
- Potential Oral Manifestations of Cardiovascular Drugs. Oral Dis. 2010;16:769-73.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of Xerostomia and Its Related Factors in Patients Referred to Zahedan Dental School in Iran. DCE J. 2016;2:e7138.
- [CrossRef] [Google Scholar]
- Lichen Planus Pemphigoides: A Case Report and Review of the Literature. Dermatol Online J. 2006;12:10.
- [CrossRef] [PubMed] [Google Scholar]
- Severity of Periodontal Disease and Number of Remaining Teeth are Related to the Prevalence of Myocardial Infarction and Hypertension in a Study Based on 4,254 Subjects. J Periodontal. 2006;77:1173-8.
- [CrossRef] [PubMed] [Google Scholar]
- Adverse Oral Manifestations of Cardiovascular Drugs. J Dent Med Sci. 2013;7:64-71.
- [CrossRef] [Google Scholar]
- Drug Interactions and Drugs that Affect Blood Pressure. J Clin Hypertens (Greenwich). 2006;8:731-7.
- [CrossRef] [PubMed] [Google Scholar]
- Salivary Parameters of Relevance for Assessing Caries Activity in Individuals and Populations. Community Dent Oral Epidemiol. 1997;25:82-6.
- [CrossRef] [PubMed] [Google Scholar]







