Translate this page into:
Assessment of Non-Alcoholic Fatty Liver Disease as Risk Factor for Cardiovascular Disease
*Corresponding author: Mounika Mellemputi, Department of Cardiology, Nizams Institute of Medical Sciences, Hyderabad, Telangana, India. mounikamellemputi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Mellemputi DM, Harish H. Assessment of non-alcoholic fatty liver disease as risk factor for cardiovascular disease. Indian J Cardiovasc Dis Women. 2023;8:230-4.
Abstract
Objectives:
Non-alcoholic fatty liver disease (NAFLD) is increasing in prevalence during present obesity pandemic. More than 25% of persons globally are believed to have non-alcoholic fatty liver disease. Many reports claim that there is an increased risk of atherosclerotic cardiovascular disease (ASCVD) among patients with non-alcoholic fatty liver disease. NAFLD is a silent disease in initial stages but progress to severe hepatic disease and increases cardiovascular morbidity in later stages, so identification and management of NAFLD are of paramount importance in preventive aspect of cardiovascular disease (CVD). Hence, the aim of this present study is to assess the risk of CVD in patients with non-alcoholic fatty liver disease in patients with and without diabetes and to evaluate usefulness of non-alcoholic fatty liver disease as a risk factor for CVD.
Materials and Methods:
The present study is a single-center observational study and it included 81 patients with non-alcoholic fatty liver disease.
Results:
In these patients, cardiovascular risk is assessed by ASCVD score, PROCAM score, QRISK 3 score, and atherogenic index of plasma and compared between diabetic and non-diabetic population. The difference has been found between diabetic and non-diabetic in Procom_score, ASCVD_score, and Q-risk_score but not found in AIP_score.
Conclusion:
The outcome of this study is that there is an increased risk of cardio vascular disease in patients with non-alcoholic fatty liver disease and risk is further increased in patients with coexisting diabetes mellitus and NAFLD.
Keywords
Non-alcoholic fatty liver disease
Atherosclerotic cardiovascular disease score
PROCAM Score
QRISK Score
Non-alcoholic fatty liver disease and cardiovascular risk
ABSTRACT IMAGE
INTRODUCTION
Non-alcoholic fatty liver disease (NAFLD) is increasing in prevalence during present obesity pandemic. More than 25% of persons globally are believed to have non-alcoholic fatty liver disease.[1] Non-alcoholic fatty liver disease is established risk factor for development of cirrhosis of liver and hepatic cell carcinoma. Recent studies claim that non-alcoholic fatty liver is not only a risk factor of hepatic disease, but also there is increased risk of atherosclerotic cardiovascular disease (ASCVD). Assessment of the disease’s prevalence and complications is hampered by under diagnosis of NAFLD, which is a major impediment to effective medical care.
The fact that NAFLD is initially asymptomatic and lack of more sensitive tools such as FibroScan, and the lack of knowledge of the ailment among patients are all contributing factors for progression of NAFLD. Ultrasonography of the liver and measurements of hepatic aminotransferase levels in plasma are frequently used screening methods, although they are insensitive for detecting and monitoring NAFLD.[2] This condition is silent, but later manifests as severe hepatic or cardiac disease, so the intention of the present study is to identify whether non-alcoholic fatty liver is a risk factor for cardiovascular disease (CVD) and can be used as screening tool for the same. In this study, various risk calculators are used which includes ASCVD score, PROCAM score, QRISK 3 score, and atherogenic index of plasma. These risk scores also include both well-established and newly emerging risk factors, such as the expanded definition of chronic kidney disease (stage 3, 4, or 5), migraine, corticosteroid use, systemic lupus erythematosus, use of atypical antipsychotics, severe mental illness, impotence, and a measurement of blood pressure (BP) variability which are not included in traditional risk scores.
Aims and objectives
The aim of this study was to assess the risk of CVD in patients with NAFLD with and without diabetes and to evaluate the usefulness of NAFLD as a risk factor for CVD.
MATERIALS AND METHODS
This single-center observational study included 81 patients with NAFLD with an inclusion criteria of age >18 years and patients with hepatic steatosis on ultrasound abdomen based on hepatorenal index, whereas patients with heavy alcohol consumption, viral hepatitis, iron overload, and drug-induced hepatic disease were excluded from the study. Heavy alcohol consumption is defined as consumption of more than four drinks on any day or more than 14 drinks per week in men and more than three drinks on any day or more than seven drinks in a week. After receiving properly informed consent, patients meeting the inclusion and exclusion criteria were enrolled in the research.
Patients visiting to Cardiology and Radiology Department of Nizam Institute of Medical Sciences were evaluated for NAFLD by ultrasound technique. According to (National Cholesterol Education Program-Adult Treatment Panel) III criteria, metabolic syndrome was defined as presence of three or more criteria among the following, the modified waist circumference (>90 cm in men and >80 cm in women), increased triglycerides (TGs) (>150 mg/dL), and low high-density lipoprotein (HDL) cholesterol (<40 mg/dL), high BP (>130/85 mmHg; or on anti-hypertensive drugs), and high fasting blood glucose (>110 mg/dL; or a known diabetic). Hepatic steatosis in its early stages to more advanced phases such as non-alcoholic steatohepatitis (NASH) and hepatic cirrhosis make up spectrum of diseases that define NAFLD. Hepatic steatosis (detected by imaging or liver biopsy) is considered a sign of NAFLD when it occurs without excessive alcohol use or other secondary or monogenic causes of hepatic steatosis. Patients body mass index (BMI), waist hip circumference was calculated, and biochemistry assessment was done for all patients enrolled in the study. Using online risk calculators including QRISK, PROCAM, ASCVD, and atherosclerosis index of plasma score, which have been verified and adopted because they are applicable to Indian population, cardiovascular risk was assessed.
Statistical analysis
Data are gathered, processed, and statistically analyzed using SPSS 20.0 and Microsoft Excel. The mean and standard deviation are used to present the results for continuous variables. Percentages are used to display results for categorical variables. The Chi-square test is used to compare two groups and determine the relevance of study parameters on a categorical scale. To ascertain the degree of association between the various variables, continuous variables are analyzed using independent “t”-test for normal distribution, spearman bivariate correlation, and multivariate analysis. All P values are two tailed and statistical significance is defined as P = 0.05.
RESULTS
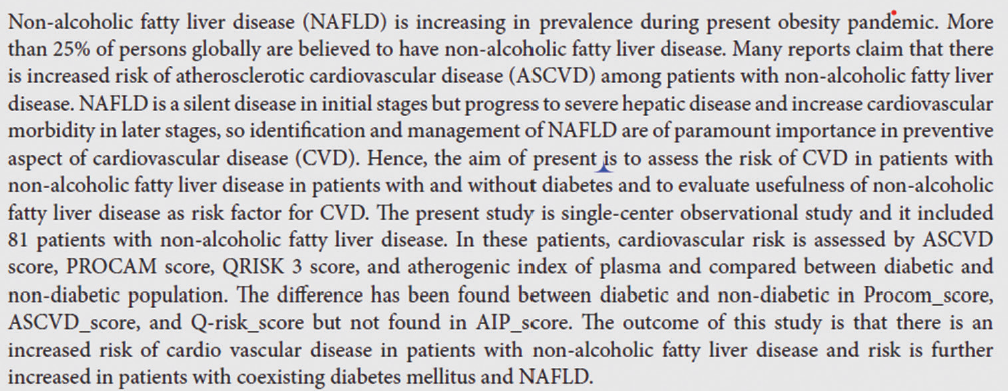
A total 80 patients were included in the study out of which 58 patients were male and remaining 22 patients were female. Among which 34 patients have diabetes and remaining are non-diabetic patients. For all the patients, ASCVD score, PROCAM score, QRISK 3 score, and atherogenic index of plasma are calculated and these scores are compared between diabetic and non-diabetic population [Table 1].
| Under USG (NAFLD Grade) | ||||
|---|---|---|---|---|
| Procam Score | GR-1FL(%) | GR-2FL(%) | Chi square test | P value (significant/Not S) |
| Cardiovascular Risk (1%) | 12 (18.8) | 0 (0) | 16.867 | 0.005 (Highly significant) |
| Cardiovascular Risk (1-2%) | 2 (3.1) | 0 (0) | ||
| Cardiovascular Risk (2-5%) | 6 (9.4) | 8 (50) | ||
| Cardiovascular Risk (5-10%) | 18 (28.1) | 4 (25) | ||
| Cardiovascular Risk (10-20%) | 18 (28.1) | 2 (12.5) | ||
| Cardiovascular Risk (20-40%) | 8 (12.5) | 2 (12.5) | ||
| Total | 64 (100) | 16 (100) | ||
| AIP_Score | GR-1FL(%) | GR-2FL(%) | Chi square test | P value (significant/Not S) |
| Low Risk (<0.11) | 34 (53.1) | 6 (37.5) | 3.125 | 0.210(Not Significant) |
| Intermediate Risk (0.11-0.21) | 6 (9.4) | 4 (25) | ||
| High Risk (>0.21) | 24 (37.5) | 6 (37.5) | ||
| Total | 64 (100) | 16 (100) | ||
| ASCVD_SCORE | GR-1FL(%) | GR-2FL(%) | Chi square test | P value (Significant/Not S) |
| Low Risk (<5%) | 6 (11.5) | 0 (0) | 5.730 | 0.126(Not Significant) |
| Boderline risk (5-7.4%) | 4 (7.7) | 4 (28.6) | ||
| Intermediate (7.5-19.9%) | 18 (34.6) | 4 (28.6) | ||
| High Risk (>=20%) | 24 (46.4) | 6 (42.9) | ||
| Total | 52 (100) | 14 (100) | ||
| Q-risk _score | GR-1FL(%) | GR-2FL(%) | Chi square test | P value (significant/Not S) |
| Low Risk (<10%) | 16 (26.7) | 2 (12.5) | 10.294 | 0.006 (Highly significant) |
| Moderate Risk (10-20%) | 8 (13.3) | 8 (50) | ||
| High Risk (>20%) | 36 (60) | 6 (37.5) | ||
| Total | 60 (100) | 16 (100) | ||
The difference have found between in NAFLD grading among Procom _score, & Q-risk which are statistically highly significant. But the difference have not found in NAFLD grading among ASCVD_ Score, _score & AIP_ score which are not statistically not significant.
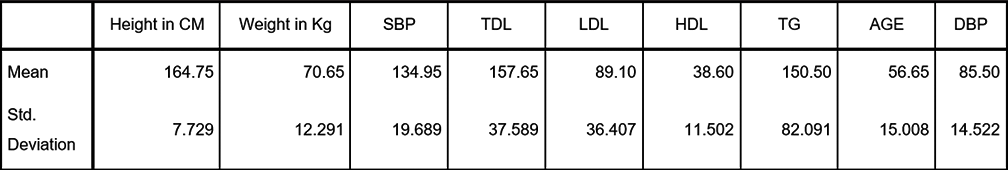
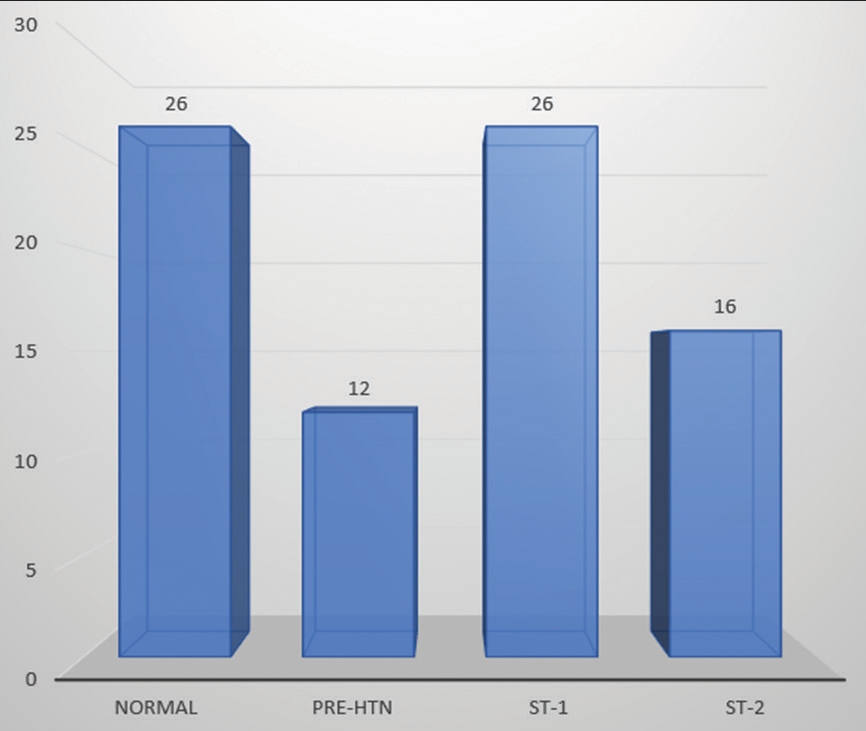
All baseline charecteristics were shown in Figure 1. Among 80 patients, 26 have normal BP, 12 have pre-hypertension and 26 have stage 1 hypertension and 16 patients have stage 2 hypertension [Figure 2]. Grade 1 fatty liver is seen in 64 patients and Grade 2 fatty liver in 16 patients. About 18.8% of patients are smokers, the rest all are non-smokers. In this study, the maximum number of patients belong to 50–60 years age group [Figure 3]. NAFLD is seen even in lean population and in this study most of people with NAFLD are from over-weight group [Figure 4]. The difference has found between diabetic and non-diabetic in Procom_score, ASCVD_Score, and Q-risk_score but not found in AIP_score [Figure 5].
- Baseline characteristics in the study population.
- Blood pressure grading in the study population.
- Age intervals in the study population.
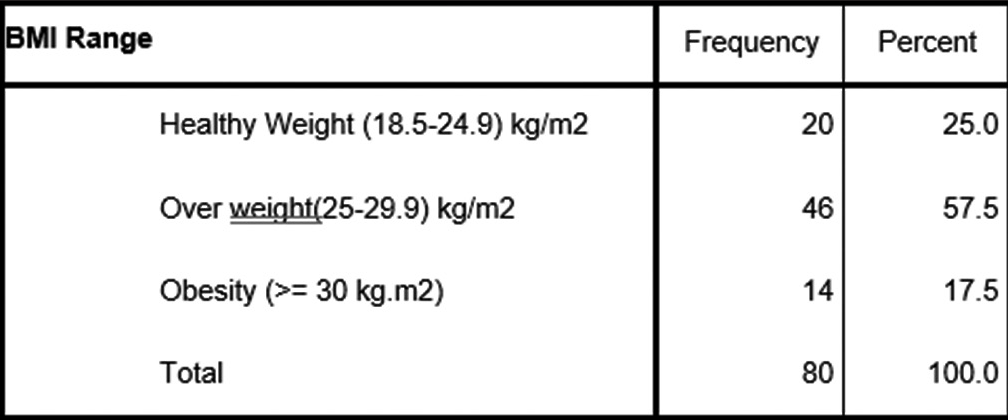
- Body mass index in the study population.
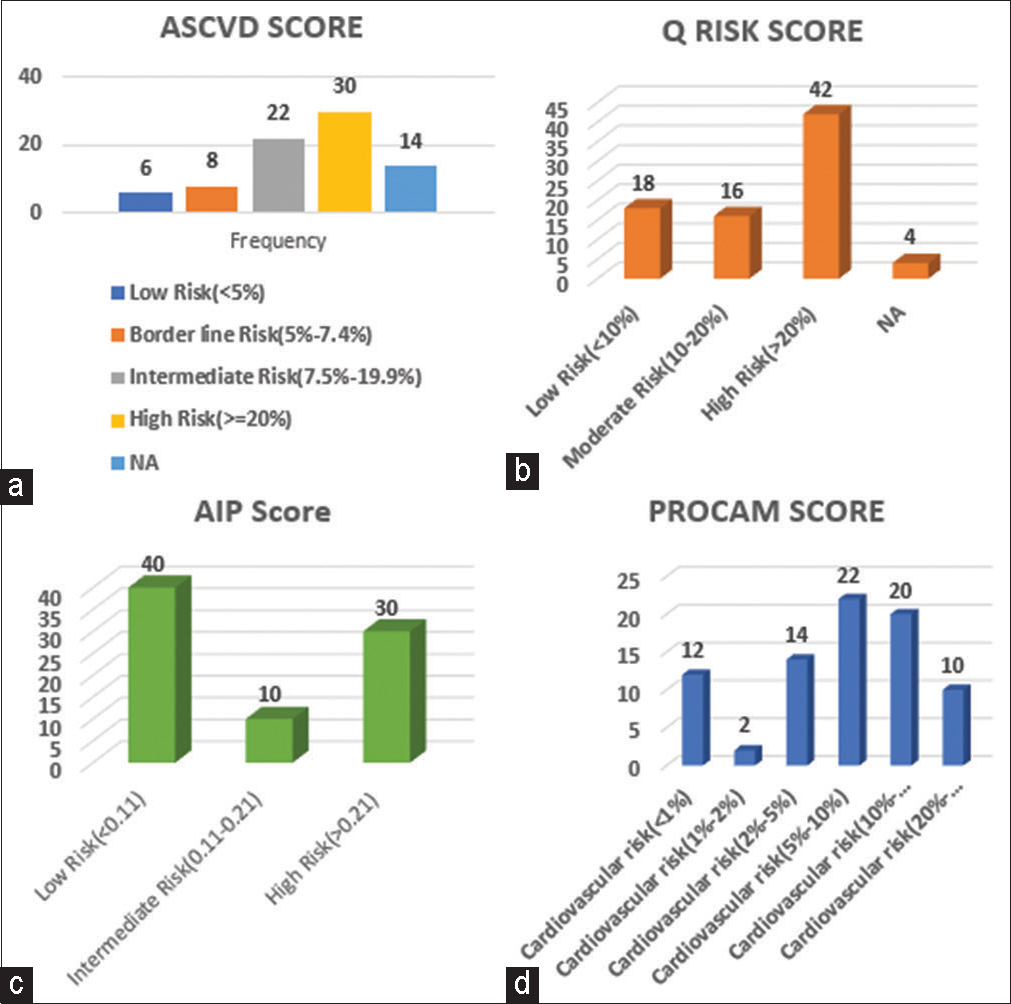
- (a) Atherosclerotic cardiovascular disease score, (b) QRISK 3 score, and (c) AIP score, D-PROCAM score.
Multivariate analysis was done for all the risk scores. The variables in this analysis are TDL, low-density lipoprotein, TG, HDL, BP grading, and BMI. All variables are stastically significant in ASCVD score, QRISK 3 score, and PROCAM risk scores, whereas TG and HDL are significant in AIP score. Subgroup analysis has found that there is no difference in cardiovascular risk between different grades of NAFLD.
DISCUSSION
NAFLD and NASH are becoming more common in the general population, and in obese populations, NAFLD may affect up to 75% of people. In fact, steatosis (NAFLD) has been discovered in nearly all participants who are severely obese, with NASH being prevalent in 25–70% of these people. Current fundamental and epidemiologic data demonstrate that the spectrum of NAFLD, which is a constellation of clinical issues brought on by insulin resistance, is strongly associated with various CVD risk factors including obesity, diabetes, and hyperlipidemia.[3]
NAFLD is prevalent in about 25% of the population overall, whereas the prevalence of obesity-related NAFLD ranges from 30% to 100%, and that of type 2 diabetes ranges from 10% to 75%. The prevalence of NAFLD is expected to rise as increased prevalence of obesity and metabolic syndrome in present day situation. However, in patients without metabolic syndrome, insulin resistance, hyperuricemia, and hypertriglyceridemia are also associated with non-alcoholic liver disease.[3,4] NAFLD is also in increasing trend even in children due to changing dietary habits and sedentary life style.[5] According to Adams et al., who evaluated the effect of NAFLD on mortality among 337 patients with type 2 diabetes followed for 9 years, non-alcoholic liver disease is linked to higher morbidity and death.[6]
Smoking and NAFLD worsen the effects of metabolic syndrome, so people with these conditions need intensive therapy to stop smoking and avoid further cardiovascular events. Several studies showed that there is association between NAFLD and CVD. In both diabetic and non-diabetic patients, NAFLD is associated with increased cardiovascular risk.[7,8] According to one study, main causes of death after 21 years follow-up in biopsy proven NAFLD are CVD and malignancy. According to Targer et al., patients with type 2 diabetes (n = 2809) had a 69.5% uncorrected prevalence of NAFLD diagnosed by ultrasound was the most common cause of hepatic steatosis (81.5%). The prevalence of diabetes in patients with NAFLD and NASH was 22.51% and 43.63%, respectively, according to Khandelwal et al.[9] In comparison to those without NAFLD, NAFLD patients exhibited higher age- and sex-adjusted prevalence of coronary (26.6 vs. 18.3%), cerebrovascular (20.0 compared 13.3%), and peripheral (15.4 vs. 10.0%) vascular disease. Although data from the National Health and Nutrition examination survey iii study showed that CVD was associated independently with NAFLD, after adjusting for major demographic, clinical, and metabolic confounders. The US third National Health and nutrition examination survey (NHANESIII: 1988–94) study showed that NAFLD was not associated with an increase = d risk of death from all causes, CVD, cancer, or liver disease, to the conclusion that although NAFLD is linked to an increase in CVD, it is not linked to an increase in death over a 14-year period.
NAFLD in children is associated with an increased incidence of atherosclerosis.[10] In one study, which included 150 overweight children with biopsy proven NAFLD, children with NAFLD showed increase in fasting glucose, insulin, TG, low-density lipoprotein, systolic, and diastolic BP; therefore, NAFLD is associated with increased cardiovascular risk even in children.
In one study, when comparison was done between NAFLD patients with and without increased ASCVD score >7.5%, there is 3 times increased cardiac specific mortality in the second group.[11] In one study, mean PROCAM score was higher in patients with NAFLD (27.50 ± 13.32 vs. 20.10 ± 7.75) (P = 0.067) with the 10-year risk of acute coronary event being 3.9 ± 6.72% in patients with NAFLD in comparison to 1.44 ± 0.85% in controls (P = 0.042).[12]
Cardiovascular risk assessment in the multidisciplinary NAFLD clinic aids in the detection and treatment of conditions such as hyperlipidemia and type 2 diabetes mellitus, allowing for better management of these comorbidities and, as a result, lowering the cardiovascular risk profile in the NAFLD population.[12]
For every patient included in the study, cardiovascular risk is calculated by various risk scores, which includes ASCVD score, PROCAM score, QRISK score, and atherogenic index of plasma. All the variables which are required for calculation of these scores are collected during the study period. The scores are compared between diabetic and non-diabetic population in patients with NAFLD. The results of all the scores are mentioned above. According to this study, ASCVD is high when NAFLD is associated with diabetes and same is with PROCAM score. These risk calculators are based on established CVD risk variables, and further, research is required to determine the precise role of NAFLD in the development of CVD. Aggressive therapy of CVD risk factors is a crucial treatment option for all NAFLD patients. The questions of whether CVD events will occur before the onset of liver failure in NAFLD patients are being debated. No matter what the pathophysiological process, the goal of treatment should be to lower all risk factors that contribute to cardiovascular mortality. It is necessary to normalize these variances in CVD risk assessment using various methodologies, which also includes particular NAFLD symptoms.
CONCLUSION
In this study, we tried to assess cardiovascular risk in NAFLD, which showed that 10 years cardiovascular risk is increased in patients with increased ASCVD, PROCAM, and QRISK scores. The risk is further increased in patients with diabetes and NAFLD, so in these patients, risk factors should be aggressively treated and dietary modifications should be advised for the optimal outcome and to decrease the morbidity and mortality related to CVD.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Audio summary available at
Financial support and sponsorship
Nil.
References
- Nonalcoholic fatty liver disease and cardiovascular risk: A scientific statement from the American heart association. Arterioscler Thromb Vasc Biol. 2022;42:e168-85.
- [CrossRef] [Google Scholar]
- Nonalcoholic Fatty Liver Disease Clinical Practice Guidelines (AACE 2022) Medscape.
- [Google Scholar]
- Abnormal lipid and glucose metabolism in obesity: Implications for nonalcoholic fatty liver disease. Gastroenterology. 2007;132:2191-207.
- [CrossRef] [PubMed] [Google Scholar]
- Metabolic significance of nonalcoholic fatty liver disease in nonobese, nondiabetic adults. Arch Int Med. 2004;164:2169-75.
- [CrossRef] [PubMed] [Google Scholar]
- Non-alcoholic fatty liver disease in obese children evaluated by magnetic resonance imaging. Acta Paediatr. 2006;95:833-7.
- [CrossRef] [PubMed] [Google Scholar]
- Nonalcoholic fatty liver disease increases risk of death among patients with diabetes: A community-based cohort study. Am J Gastroenterol. 2010;105:1567-73.
- [CrossRef] [PubMed] [Google Scholar]
- Final results of a long-term, clinical follow-up in fatty liver patients. Scand J Gastroenterol. 2009;44:1236-43.
- [CrossRef] [PubMed] [Google Scholar]
- Fatty liver is associated with insulin resistance, risk of coronary heart disease, and early atherosclerosis in a large European population. Hepatology. 2009;49:1537-44.
- [CrossRef] [PubMed] [Google Scholar]
- Non-alcoholic fatty liver disease in diabetes: When to refer to the hepatologist? World J Diabetes. 2021;12:1479-93.
- [CrossRef] [PubMed] [Google Scholar]
- Nonalcoholic fatty liver disease and carotid atherosclerosis in children. Pediatr Res. 2008;63:423-7.
- [CrossRef] [PubMed] [Google Scholar]
- Mortality risk detected by atherosclerotic cardiovascular disease score in patients with nonalcoholic fatty liver disease. Hepatol Commun. 2019;3:1050-60.
- [CrossRef] [PubMed] [Google Scholar]
- Patients with non-alcoholic fatty liver disease (NAFLD) have an increased risk of atherosclerosis and cardiovascular disease. Trop Gastroenterol. 2013;34:74-82.
- [CrossRef] [PubMed] [Google Scholar]







