Translate this page into:
“All that Glitters like Gold is Not Good.” Pericardial Effusion with Cardiac Tamponade in Hypothyroidism
*Corresponding author: Iragavarapu V. M. R. Tammiraju, Department of Cardiology, Asram Hospital, Eluru, Andhra Pradesh, India. vmrtraju.mbbs@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Tammiraju IV, Bhupathi M. “All that glitters like gold is not good.” Pericardial effusion with cardiac tamponade in hypothyroidism. Indian J Cardiovasc Dis Women 2023;8:215-9.
Abstract
Among various cardiac manifestations of hypothyroidism, pericardial effusion is not an uncommon finding. But effusion leading to Tamponade is a rare complication owing to its slow collection due to increased capillary permeability. Most of the times patient can be managed conservatively but in case of hemodynamic compromise tapping of fluid will give immediate relief of symptoms. To discuss various pathophysiological issues and management options of pericardial effusion with Tamponade in hypothyroidism. Six cases of hypothyroidism with pericardial effusion and Tamponade were studied. Their demographic features and treatment issues were assessed. Five out of six cases underwent pericardiocentesis. One case was manged conservatively. All the cases were stable on follow up. Prompt diagnosis with early pericardiocentesis with thyroid supplementation will have better prognosis.
Keywords
Hypothyroidism
Pericardial effusion
Tamponade
Tapping
INTRODUCTION
Hypothyroidism is an endocrine disorder with multiorgan involvement and various complications. Weight gain, constipation, cold sensitivity to cold, and easy fatiguability are some of the symptoms of hypothyroidism. Less common signs include myopathy, carpal tunnel syndrome, and hoarseness of voice. Although hypothyroidism is an established cause of pericardial effusion, cardiac tamponade is an uncommon manifestation. Here, we present six cases of hypothyroidism with pericardial effusion and tamponade treated promptly with pericardiocentesis and thyroid supplements.
CASE SERIES
CASE 1
A 55-year-old female hypertensive patient presented with complaints of shortness of breath of 2 days duration. She had drug-induced Stevens–Johnson Syndrome. Her thyroid-stimulating hormone (TSH) was 13.46 (0.4–6.1) and low triiodothyronine (T3). Other laboratory parameters were in normal range. Transthoracic echocardiography showed large pericardial effusion with tamponade, mild TR mild PAH, Trivial MR, normal LV Systolic function, and mild thickened AV with mild AR [Figure 1]. She was admitted and pericardiocentesis was done. Pericardial fluid was having golden sheen like color and analysis showed exudate. She was managed with thyroxine supplementation (50 mcg OD). The patient was stable after a few days of treatment.
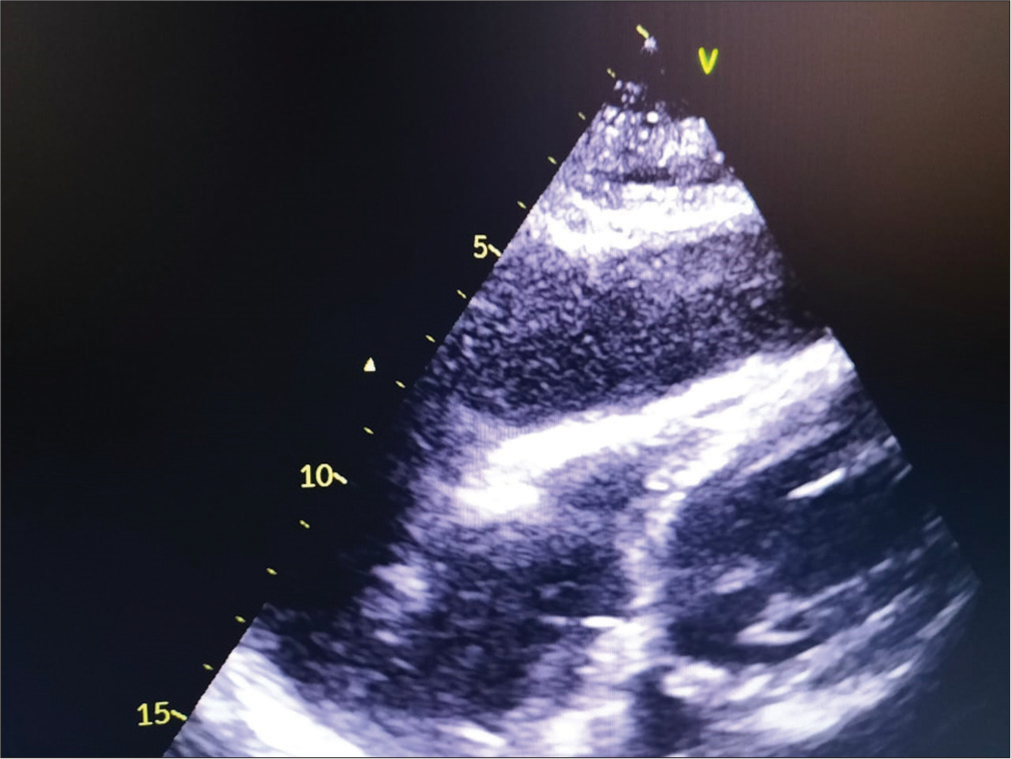
- 2D ECHO showing pericardial tamponade in a patient with hypothyroidism.
CASE 2
A 21-year-old female patient was diagnosed to have acute tubular interstitial nephritis and pericardial effusion, for which she was on regular medication. She had a past history of epilepsy since childhood and hypothyroidism but on irregular medication. There was sudden increase in breathlessness. On laboratory investigation, thyroid function test revealed high TSH >26 (0.4–6.1) and low T3. Transthoracic echocardiography revealed large pericardial effusion with tamponade. Pericardial tapping was done which showed golden hue color exudative effusion. The patient was stable after a few days of treatment. Levothyroxine 100 mcg once daily and is on regular follow-up with nephrologist.
CASE 3
A 62-year-old female diabetic and hypertensive patient presented with complaints of shortness of breath of 10 days duration, grade IV. SOB was slow in onset and gradually progressive. It was associated with sweating. There was sudden onset of chest heaviness, palpitation, and orthopnea/PND. On examination, her pulse was 127/min, regular, and normal in volume. Her blood pressure was 90/70 mm of Hg, respiratory rate was 40/min, and she was afebrile. She had pallor and bilateral pedal edema. On evaluation, she had high TSH and low T3 and large pericardial effusion with tamponade, left side massive pleural effusion. She was admitted to the ward and pericardiocentesis and thoracocentesis were done. She was managed with diuretics and thyroxine supplementation.
CASE 4
A 41-year-old female presented to our institution with complaints of insidious onset of shortness of breath of 10 days duration. However, there was no history of cough, pain, palpitation, swelling of legs, and syncope. Except for abnormal thyroid profile (TSH) >48 (0.4–6.1) and low T3, her laboratory investigations were within the normal range. Radiology of chest PA view showed enlarged cardiac silhouette suggestive of pericardial effusion. Transthoracic echocardiography revealed large pericardial effusion with tamponade, fair LV systolic dysfunction, trivial MR, mild TR, and Grade 1 diastolic dysfunction. Pericardiocentesis was done and is on regular follow-up.
CASE 5
A 35-year-old female presented with insidious onset of shortness of breath class II since 6 months. On evaluation, pericardial effusion was diagnosed. Laboratory investigative profile was suggestive of hypothyroidism. As patient denied admission, she was managed with oral Thyroxine supplements. On follow-up, effusion decreased and symptoms relieved.
CASE 6
A 40-year-old male referred to us with breathlessness and enlarged cardiac silhouette in chest X-ray. On evaluation, it was turned out to be large pericardial effusion with tamponade. Emergency tapping of effusion relieved the symptoms. Evaluation of blood and pericardial fluid is suggestive of hypothyroidism. The patient was discharged on oral thyroxine.
The various demographic features of the patients with pericardial fluid analysis are mentioned in [Table 1].
| S. No. |
Age | Sex | Risk factors | Diagnosis | Pericardial fluid analysis | Treatment | Outcome |
|---|---|---|---|---|---|---|---|
| 1. | 55 year | F | HTN, TB, hormones, H/O pericardiocentesis in 2018, k/c/o SJS | Pericardial effusion, HTN, hypothyroidism | Glucose - 70 mg/dL ADA - 6.5U/L Total protein - 3.8 g/dL |
Pericardiocentesis, Thyroxine | Survived |
| 2. | 21 year | F | Epilepsy since childhood, hypothyroidism since may 2019 | Cardiac tamponade, hypothyroidism, CKD | Glucose - 93 mg/dL ADA - 20.8U/L Total protein - 4.2 g/dL |
Pericardiocentesis, levothyroxine supplementation | Survived |
| 3. | 62 year | F | DKA, DM, HTN, Hypothyroidism | CAD/Pericardial effusion with Pleural effusion | Glucose - 405 mg/dL ADA - 54U/L Total protein - 6.8 g/dL Montaux and CBNAAT - Negative |
Pericardiocentesis, thyroxine | Survived |
| 4. | 41 year | F | HTN | Large pericardial effusion with tamponade, hypothyroidism, B/L pleural effusion | Glucose - 73 mg/dL ADA - 26 U/L Total protein - 5.2 g/dL |
Pericardiocentesis, levothyroxine supplementation | Survived |
| 5. | 35 year | F | Nil | Pericardial effusion, hypothyroidism | Exudate | Oral levothyroxine | Survived |
| 6. | 40 year | M | HTN | Large pericardial effusion with tamponade, hypothyroidism | Exudate | Pericardiocentesis, levothyroxine | Survived |
HTN: Hypertension, ADA: Adenosine deaminase
DISCUSSION
Hypothyroidism occurs due to low or absent functional thyroid hormone and is diagnosed when secretion of TSH is increased due to decreased T3 and T4 hormones. T3 causes tissue thermogenesis increases systolic contraction, diastolic relaxation, and reduces vascular resistance. In a healthy individual, the pericardial fluid (15–50 mL) was secreted by mesothelial cells through plasma ultrafiltration process and drained mainly by the lymphatic system.[1] Abnormal collection of pericardial fluid within the pericardial cavity leads to Pericardial effusion. Such liquid can be either exudate, transudate, pyopericardium, or hemopericardium.[1] Pericardiac cavity of more than 1000 cc fluid leads to decreased cardiac output and cardiac tamponade.
There are many causes of pericardial effusion. They include inflammatory, neoplastic, infectious, trauma, cardiac, vascular, idiopathic, and others such as chronic kidney disease, renal failure, radiation, and drug induced.[2] Hypothyroidism is associated with many cardiovascular manifestations including exercise intolerance, dyspnea, bradycardia, diastolic hypertension, and edema. Hypothyroidism and cardiac manifestations are tabulated in [Table 2].
| S. No. | Cardiac manifestations | Pathophysiological mechanisms | |
|---|---|---|---|
| 1. | Decreased Cardiac output |
a) Decreased cardiac contractility b)↑ Vascular resistance c) Hear rate- |
•Increase in after load •Decrease in expression of Ca dependent ATPase and Phospholamban •Decrease in beta-adrenergic receptor expression •↑PVR - decrease in EDRF, promotes contraction of vascular smooth muscle cells. •↑SVR - decreased nitric oxide production •Decrease in beta adrenergic receptor expression. |
| 2. | Dyslipidemia | •↑Total cholesterol •↑LDL •↑Apo B •↑CPR •↑Homocysteine |
•↓Number of LDL receptors •↓LDL receptor activity •↓LDL clearance |
| 3 | Decreased renin angiotensin system activation | •↓Renin •↓Diastolic blood pressure •↓Pulse Pressure |
|
| 4. | Decreased erythropoietin | Normocytic, normochromic anemia | |
| 5. | Heart failure | •Diastolic Dysfunction •↑Isovolumetric relaxation time •↓E/A |
|
| 6. | Pericardial effusion | ↑Vascular permeability | |
| 7. | Arrhythmia | •Prolonged QT •Tdp •AV blocks •Low Voltage complexes |
Due to prolonged ventricular Action potential →Ventricular irritability |
| 8. | Amiodarone-induced hypothyroidism | •Iodine rich benzofuranic (37% iodine by WT) •Wolf-Chaikoff effect inhibition of oxidation of iodine •Increase Hashimoto’s thyroiditis •Inhibits deiodinase I, II activity |
|
| 9. | Increased atherosclerosis | Dyslipidemia |
Pathophysiology of hypothyroidism and pericardial effusion
Incidence of pericardial effusion is around 3–6%[3-5] in the current literature. It is more common in females. Our series also showed female preponderance with 5:1 ratio. Khaleeli and Nemon (1982) found an incidence between 30% and 78% in different series. In their study group, five out of six patients presented pericardial effusion.[6] The salient feature of pericardial fluid in hypothyroidism is its “gold paint appearance” as first described by Alexander in 1919.[7] This is due to the presence of cholesterol crystals due to altered lipid metabolism and churring effect of heart. The elasticity of the pericardium and the slow rate of accumulation of fluid are the two factors which makes cardiac tamponade a very rare complication of hypothyroidism.
Hypothyroidism causes pericardial effusion through increased permeability of the epicardial vessels and decreased lymphatic drainage of albumin, resulting in accumulation of fluid in the pericardial space.[1,8] The pathophysiology of pericardial effusion is depicted in [Figure 2]. Autoimmunity does not play a major role in the pathophysiology. The classic Beck’s triad in tamponade is less seen in hypothyroid patient, instead they present with bradycardia, diastolic hypertension, and normal heart rate. When thyroid levels get corrected and normalized, pericardial effusion typically gets resolved. Aljadir, in a study performed in Iraq, reported nine out of 22 patients had pericardial and pleural effusions, besides ascites.[9,10] In the present study, two out of six patients had both pericardial and pleural effusion. The salient features of hypothyroidism and pericradial effussion were mentioned in Table 3.
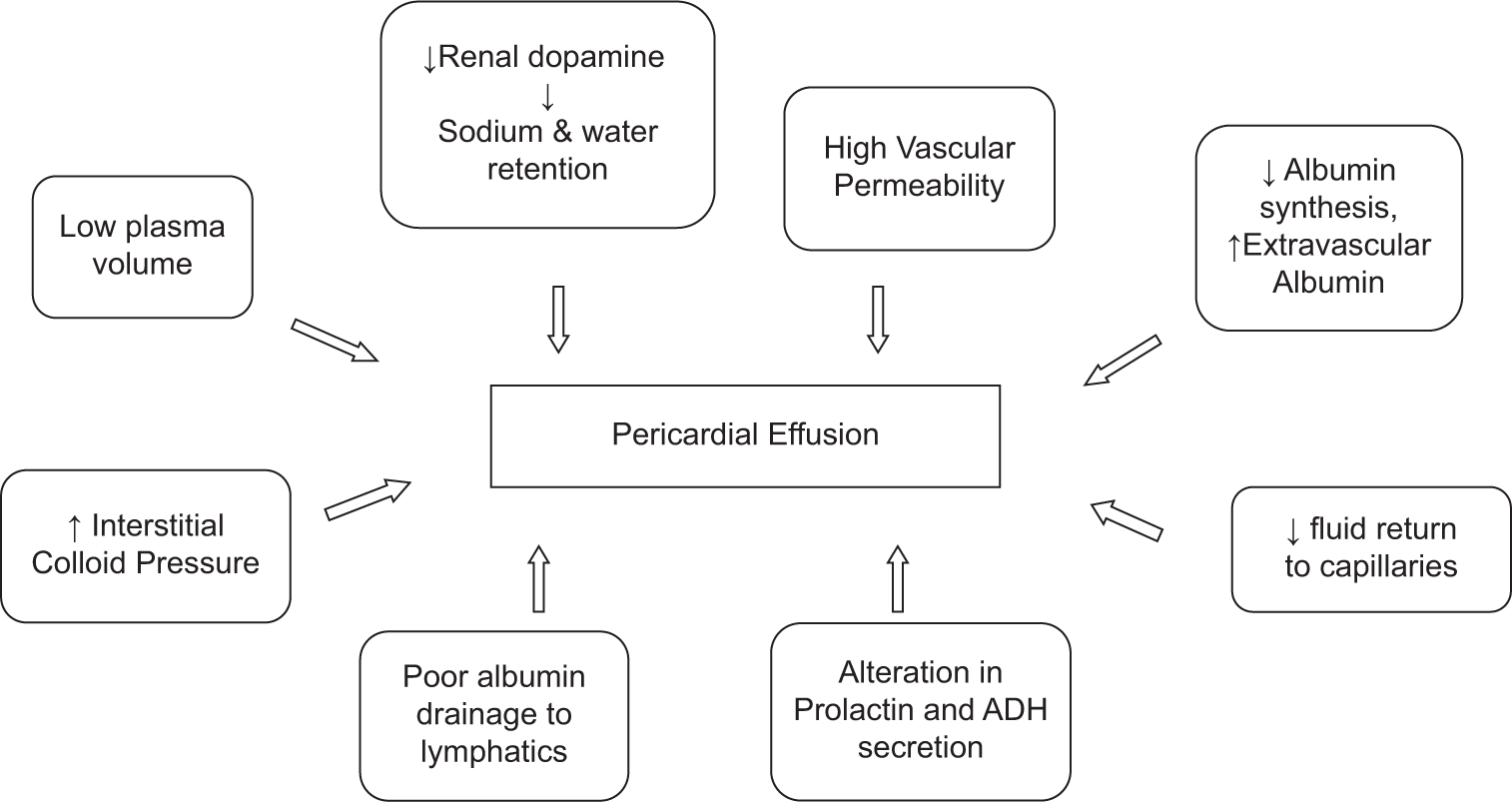
- Pathophysiology of pericardial effusion.
| Pathophysiology | •Low plasma volume •Decrease renal dopamine synthesis •High vascular permeability •Decreased albumin (decreased synthesis) •Increased albumin in extra vascular •Increased interstitial colloid pressure •Reduced fluid return to capillaries •Poor albumin drainage into lymphatics •Alteration in Prolactin and ADH secretion •Failure of handling water load like SIADH |
| Symptoms | •Very insidious onset of symptoms •Shortness of breath •low volume pulse •Bradycardia (unlike Tachycardia) •hypertension (instead of hypotension) |
| Fluid analysis | •Can be exudate or transudate •cholesterol crystals |
| Management | •Mostly conservative •Pericardiocentesis if hemodynamic compromise |
Management
The characteristic feature of effusion in hypothyroidism is its insidious onset due to slow collection of fluid. Hence, most of the patients do not have hemodynamic compromise. Hence, conservative management with oral or intravenous levothyroxine is sufficient in many of the cases.[11-14] However, if there is significant collection with tamponade and hemodynamic compromise in a symptomatic patient pericardiocentesis should not be delayed.[15] There are many case studies which showed successful management of pericardial effusion in both the ways depending on the situation. Baldwin et al.[15] reported a series of three cases with large pericardial effusions in hypothyroidism which was managed conservatively with intravenous levothyroxine. Wang et al.[16] reported 22.2% of patients underwent pericardiocentesis in his series of 36 patients. Kaur et al.[17] described four cases of tamponade in hypothyroidism managed with emergency pericardiocentesis. Tudoran and Tudoran[18] conducted study on 192 cases, 156 among them were hypothyroid and found to have effusions which were treated with no surgical intervention. Hardisty et al.[13] conducted study on 39 hypothyroid patients, 12 among them were found to have effusions and were on conservative treatment which showed decline in effusion later.
In five out of six of our patients, pericardiocentesis was done, and then, the patients were given the hormone supplements to maintain thyroid levels. One case was managed with levothyroxine alone. The outcome of all the patients turned out to be good and they were stable and on regular follow-up. [Table 4] summarizes various case series and case reports of hypothyroidism and pericardial effusion.
| Study | Year of study | No. of cases | Management |
|---|---|---|---|
| Hardisty et al.[13] | 1980 | 39 cases | 12 cases - Conservative |
| Wang et al.[16] | 1998 2008 |
36 cases | 28 cases - Conservative 8 cases – Pericardiocentesis. |
| Tudoran and Tudoran[18] | 2011 | 192 cases | 156 cases - Conservative |
| Baldwin et al.[15] | 2020 | 3 cases | All conservative |
| Kaur et al.[17] | 2020 | 4 cases | Pericardiocentesis in all four cases |
| Our series | 2022 | 6 cases | Five out of six pericardiocentesis |
CONCLUSION
Although mild pericardial effusion is common in hypothyroidism, large pericardial collection leading to tamponade can happen in rare instances. Prompt diagnosis with pericardial tapping and appropriate hormone supplementation will save the patients and prevent the recurrences.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Pericardiocentesis in massive pericardial effusions due to hypothyroidism. IOP Conf Ser Earth Environ Sci. 2018;125:12172.
- [CrossRef] [Google Scholar]
- Triage and management of pericardial effusion. J Cardiovasc Med (Hagerstown). 2010;11:928-35.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac tamponade in hypothyroidism. BMJ Case Rep. 2014;2014:bcr2014204076.
- [CrossRef] [PubMed] [Google Scholar]
- Pericardial effusion in primary hypothyroidism. Am Heart J. 1990;120:1393-5.
- [CrossRef] [PubMed] [Google Scholar]
- Massive pericardial effusion as initial manifestation of hypothyroidism. Arq Bras Endocrinol Metabol. 2012;56:383-7.
- [CrossRef] [PubMed] [Google Scholar]
- Factors affecting resolution of pericardial effusions in primary hypothyroidism: A clinical, biochemical and echocardiographic study. Postgrad Med J. 1982;58:473-6.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac tamponade in a patient with primary hypothyroidism. Indian J Endocrinol Metab. 2011;15(Suppl 2):S144-6.
- [CrossRef] [PubMed] [Google Scholar]
- A case of primary hypothyroidism initially presenting with massive pericardial effusion. J Clin Transl Endocrinol Case Rep. 2016;2:1-2.
- [CrossRef] [Google Scholar]
- Pericardial and serous effusions in primary hypothyroidism. Endocrinol Metab Int J. 2018;6:61-3.
- [CrossRef] [Google Scholar]
- Pericardial effusion with cardiac tamponade as a form of presentation of primary hypothyroidism. Arq Bras Cardiol. 2002;78:580-5.
- [CrossRef] [PubMed] [Google Scholar]
- Echocardiographic evaluation of pericardial effusion in myxedema. Incidence and biochemical and clinical correlations. Circulation. 1975;52:823-7.
- [CrossRef] [PubMed] [Google Scholar]
- Pericardial effusion in hypothyroidism. Clin Endocrinol (Oxf). 1980;13:349-54.
- [CrossRef] [PubMed] [Google Scholar]
- Pericardial diseases in patients with hypothyroidism. Heart. 2019;105:1027-33.
- [CrossRef] [PubMed] [Google Scholar]
- Myxedema heart and pseudotamponade. J Endocr Soc. 2020;5:bvaa125.
- [CrossRef] [PubMed] [Google Scholar]
- Hypothyroid cardiac tamponade: Clinical features, electrocardiography, pericardial fluid and management. Am J Med Sci. 2010;340:276-81.
- [CrossRef] [PubMed] [Google Scholar]
- Peculiar aspects of pericardial effusion in hypothyroid patients. Indian J Appl Res. 2011;3:1-2.
- [CrossRef] [Google Scholar]








