Translate this page into:
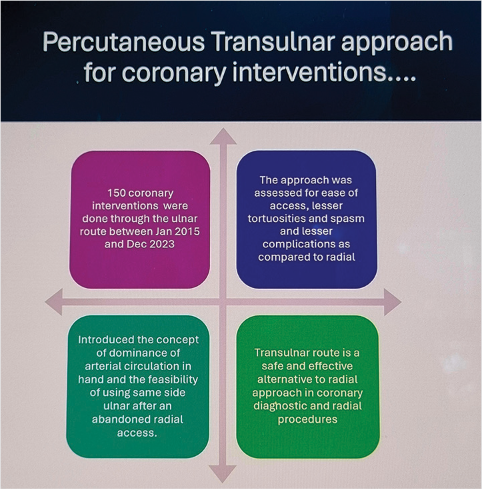
Percutaneous Transulnar Arterial Approach for Coronary Interventions
*Corresponding author: Neelam Kaul, Department of Cardiology, Amandeep Hospital, Pathankot, Punjab, India. drneelamkaul@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Kaul N, Kaul S. Percutaneous Transulnar Arterial Approach for Coronary Interventions. Indian J Cardiovasc Dis Women. doi: 10.25259/IJCDW_37_2024
Abstract
Objectives:
Coronary diagnostics and interventions have come a long way. For decades the femoral artery has been the access of choice , until radial artery was found to be a viable alternative for coronary and non coronary interventions. We present here our experiences and an analytical review of our transulnar journey, spanning nearly a decade of inhibitions and tentativeness of using it as an alternative , to an upfront route of choice based on arterial dominance.
Methods:
We did a retrospective analysis based on interventions done through the transulnar route between Jan 2015 and Dec 2023. Both the operators in the study were experts in transradial procedures with an experience of more than 5000 each radial procedures.
Results:
Arterial dominance was assessed by palpation , and was defined as the more intensely palpable pulse at the wrist. Ulnar dominance was seen in 57.6 percent of the cases. Spasm was encountered in the ulnar artery in just a single case, and 4 cases (2.6%) had loops and tortuosities. The mean fluoroscopy time for coronary angiography was 1.5 mins.
Conclusion:
Transulnar route is a safe and effective alternative to radial approach in coronary diagnostic and interventional procedures. The principle of arterial dominance at the wrist is a good way for selection of access routes.
Keywords
Transradial
Transulnar
Coronary interventions
ABSTRACT IMAGE
INTRODUCTION
Coronary diagnostics and interventions have come a long way. For decades, the femoral artery has been the access of choice, until the radial artery was found to be a viable alternative for coronary and non-coronary interventions. Early mobility, ease of access, easy hemostasis, and early ambulation were the major advantages that made this route a favorite for most of the interventionists globally. Catheters and hardware were designed particularly for a radial route, but the challenges that lay ahead were to come from its anatomy itself. Tortuosities and loops in the artery became one of the reasons for crossover to the femoral route, and thus giving away the advantages again owing to anatomical and physiological bottlenecks. Those who had mastered performing procedures through the wrist were not satisfied by crossovers. And thus, it gave birth to the usage of ulnar artery as an alternative to radial artery for coronary interventions. We present here our experiences and an analytical review of our transulnar journey, spanning nearly a decade of inhibitions and tentativeness of using it as an alternative, to an upfront route of choice based on arterial dominance.
MATERIALS AND METHODS
This retrospective analysis is based on interventions done through the transulnar route between January 2015 and December 2023. Both the operators in the study were experts in transradial procedures with experience of more than 5000 each radial procedures. A total of 150 percutaneous coronary interventions were assessed and analyzed. The cocktail regimen used for the ulnar artery was the same that we have been using for the radial artery: 4000 units of unfractionated heparin, 100 mcg of Nitroglycerine (NTG), and 250 mcg of diltiazem. The demographics were studied and some anatomical and physiological variables were reviewed. We also introduce, “the concept of dominance’’ for the first time and its relevance in choosing the route for access. The parameters that were analyzed were ease of access, fluoroscopy time, anatomical variables like loops and tortuosities, access site complications such as pseudoaneurysms and hematomas, and post-procedural spasms and occlusions. We also assessed the feasibility of the same-side ulnar access after a failed radial attempt.
RESULTS
Demographics and risk factors
The mean age of the study group was 58 ± 10 years with a female preponderance, who constituted 56% of the total. Dyslipidemia (hypercholesterolemia) was the most common risk factor in our group. Among the risk factors for coronary artery disease, type 2 diabetes and hypertension were also common, alongside obesity and smoking [Table 1].
| S. No. | Variables | Incidence (n=150) | % age |
|---|---|---|---|
| 1. | Age (Mean±SD) | 58±10 years | – |
| 2. | Gender (Females) | 84 | 56% |
| 3. | Smokers | 53 | 35.3 |
| 4. | Dyslipidemia | 92 | 61.3 |
| 5. | Hypertension | 78 | 52 |
| 6. | Diabetes | 88 | 58.6 |
| 7. | Obesity | 35 | 23.3 |
| 8. | Peripheral arterial disease | 22 | 14.6 |
| 9. | Right ulnar artery usage | 123 | 82 |
| 10. | Arterial dominance (Ulnar) | 86 | 57.3 |
| 11. | Vascular access time | 124 s±30 | – |
| 12. | Fluoroscopy time (DIAG) | 1.5 min | – |
| 13. | Loops and tortuosities | 4 | 2.6 |
| 14. | Spasm | 1 | 0.66 |
| 15. | Cross over left ulnar | 27 | 18 |
| 16. | Cross over femoral | 0 | 0 |
| 17. | Same side ulnar | 16 | 10.6 |
| 18. | Access site swellings | 11 | 7.3 |
| 19. | Access site hematomas | 1 | 0.66 |
| 20. | Forearm hematomas | 0 | 0 |
| 21. | Post-procedure occlusions | 0 | 0 |
| 22. | Pseudoaneurysms | 0 | 0 |
SD: Standard deviation, DIAG: Diagnostic
Efficacy and anatomical factors
Arterial dominance [Figure 1] was assessed by palpation and was defined as the more intensely palpable pulse at the wrist. Ulnar dominance was seen in 57.6% of the cases. It took approximately 124 ± 30s to cannulate the artery. The right ulnar artery was the preferred route in 82% of cases. In 4% of the cases, crossover was done to the left radial route in 18%. No crossover was done to the femoral route. In 16 cases (10.7%), the same side (right side ulnar) ulnar was used after an abandoned radial route, owing to small caliber, spasm, or radial loops. We encountered spasm in the ulnar artery in just a single case, and 4 cases (2.6%) had loops and tortuosities. The mean fluoroscopy time for coronary angiography was 1.5 min [Table 1].
- The concept of arterial dominance.
Post-procedure observations
Minor swellings at the access site were witnessed in 11 (7.3%) cases. Major swellings and hematomas around the puncture site were seen in only one case, which was managed with pressure hemostasis. Interestingly enough we did not encounter any post-procedure spasm, forearm hematomas, or ulnar artery occlusions in our study.
DISCUSSION
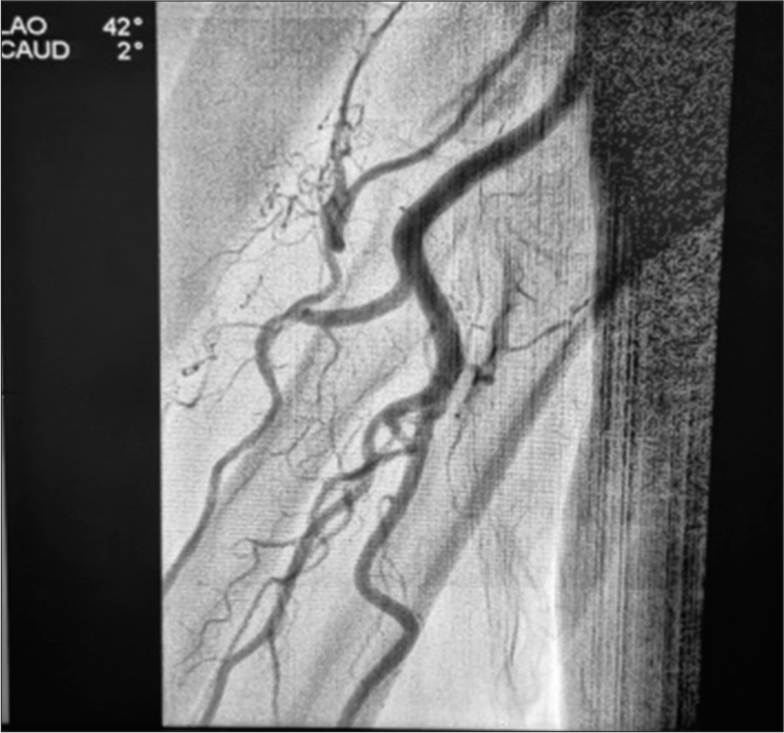
Ulnar artery because of its deep location as compared to the radial artery has not been used as a route of access for coronary angiographies and interventions, although there have been anatomical studies to prove that it may be bigger in size than its radial counterpart, especially at the wrist [Figure 2]. One of the most common reasons of cross-overs from the wrist to the groin has been a failed radial access owing to spasm, loops, and tortuosities. We in our study observed that these anatomical aberrations were seen far less in the ulnar approach.

- The ulnar route.
The superiority of radial approach over the femoral route has long been established, and complications at the groin and retroperitoneal bleeds through the femoral route have been one of the reasons higher mortality and major adverse cardiac event (MACE).[1-4] The perception of radial being the only route to heart through the wrist needs a change, and interestingly enough the paradigm is shifting.
Dahal et al. in their meta-analysis compared the success rates, efficacy, and safety of transradial and transulnar access.[5] A total of 2744 patients from five clinical trials were included in this meta-analysis, with nearly an equal number of patients undergoing transradial and transulnar catheterizations (1360 and 1384, respectively).[5-8] The primary outcomes were MACE, and the secondary outcome was the composite endpoint of access-related complications. Although the transulnar route resulted in higher rates of access site failure and crossover, it had similar efficacy (similar MACE rates), safety (similar access site complications), and procedural times as the transradial route. Another meta-analysis conducted by Fernandez et al., of six randomized controlled trials also supported the use of ulnar artery as an alternative to the radial access for cardiac catheterization.[9] Transulnar access is associated with fewer vascular complications, less patient discomfort, and consequently shorter durations of hospitalization.[9] Transradial access is not superior to transulnar approach when performed by an experienced operator.[10,11] In 535 consecutive patients, in a study conducted by Geng et al., to assess the two approaches, a successful puncture of the target artery was achieved in 95.1% and 91.5% of the patients in the transradial and transulnar groups, respectively (P > 0.05).[12] The utilization of ulnar artery (UA) as an access site increases the chance of success with forearm access and reduces the need for crossover to the femoral approach.[13] Moreover, the artery is large enough to accommodate 7F sheaths and enable left main and bifurcation percutaneous coronary interventions (PCIs) with ease [Figures 3 and 4]. The learning curve of this approach after appropriate guidance could be fast and safe.

- Same side ulnar route after an abandoned radial.

- Same side ulnar hemostasis.
We introduce the concept of dominance, meaning thereby that invariably one of the two arteries at the wrist is bigger. Hence, palpating both arteries should become a habit, and the more volume one can be chosen for cannulation. For interventionists who have been performing coronary interventions through the radial route, learning curve for mastering the skills for ulnar approach is fast and safe. There are however certain hindrances and challenges that need attention. The first is the deep location of the artery, and the second is its proximity to the ulnar nerve which may be injured while cannulation. Multiple jabs to the artery should be avoided and xylocaine for local anesthesia should be administered carefully. Post-procedure the wrist should be observed more carefully for any hematomas, as compression is sometimes not as snug as it is on the radial site.
The incidence of spasm and loops and tortuosities was almost none, which could perhaps give the ulnar route an initial advantage over the radial route. Our effort has been to find whether the ulnar route can be used as an upfront approach while performing coronary interventions through the wrist. Another issue closely related to this is the use of the same side ulnar approach after abandoning a failed radial attempt owing to spasms, loops, or difficult anatomy. Agostoni et al. in their study (the SWITCH registry) observed that in cases of failed radial sheath insertion, switching directly to the homolateral ulnar artery for percutaneous coronary procedures is feasible and appears to be safe, without cases of symptomatic hand ischemia in this series.[14] In our study, we took homolateral ulnar artery approach in 16 cases and did not encounter any hand ischemia later [Figures 5 and 6]. However, there are certain technical modifications that can be done like taking out radial sheath just after the procedure and ulnar sheath once the hemostatis of the radial artery is completely achieved. In case of peripheral arterial disease, same-side cannulation should be best avoided.

- 7F and LMCA Intervention

- 7F and ulnar route.
A study to compare ulnar with the radial approach is underway and shall put more light on the advantages of transulnar approach
CONCLUSION
Transulnar route is a safe and effective alternative to radial approach in coronary diagnostic and interventional procedures. The principle of arterial dominance at the wrist is a good way for selection of access route. With fewer tortuosities, loops and spasms, and a larger caliber than the radial artery, the ulnar route can be the first choice for coronary interventions through the hand/wrist.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Audio summary available at
Financial support and sponsorship
Nil.
References
- Radial Versus Femoral Approach for Percutaneous Coronary Diagnostic and Interventional Procedures; Systematic Overview and Meta-analysis of Randomized Trials. J Am Coll Cardiol. 2004;44:349-56.
- [CrossRef] [PubMed] [Google Scholar]
- Radial Versus Femoral Access for Coronary Angiography and Intervention in Patients with Acute Coronary Syndromes (RIVAL): A Randomised, Parallel Group, Multicentre Trial. Lancet. 2011;377:1409-20.
- [CrossRef] [PubMed] [Google Scholar]
- Major Improvement of Percutaneous Cardiovascular Procedure Outcomes with Radial Artery Catheterisation: Results from the PREVAIL Study. Heart. 2009;95:476-82.
- [CrossRef] [PubMed] [Google Scholar]
- Radial Versus Femoral Access in Patients with Acute Coronary Syndromes Undergoing Invasive Management: A Randomised Multicentre Trial. Lancet. 2015;385:2465-76.
- [CrossRef] [PubMed] [Google Scholar]
- Transulnar Versus Transradial Access for Coronary Angiography or Percutaneous Coronary Intervention: A Meta-analysis of Randomized Controlled Trials. Catheter Cardiovasc Interv. 2016;87:857-65.
- [CrossRef] [PubMed] [Google Scholar]
- Transulnar Approach as an Alternative Access Site for Coronary Invasive Procedures after Transradial Approach Failure. Am Heart J. 2012;164:462-7.
- [CrossRef] [PubMed] [Google Scholar]
- Transulnar Compared with Transradial Artery Approach as a Default Strategy for Coronary Procedures: A Randomized Trial. The Transulnar or Transradial Instead of Coronary Transfemoral Angiographies Study (the AURA of ARTEMIS Study) Circ Cardiovasc Interv. 2013;6:252-61.
- [CrossRef] [PubMed] [Google Scholar]
- Real Time Intraprocedural Ultrasound Measurements of the Radial and Ulnar Arteries in 565 Consecutive Patients Undergoing Cardiac Catheterization and/or Percutaneous Coronary Intervention via the Wrist: Understanding Anatomy and Anomalies May Improve Access Success. J Interv Cardiol. 2015;28:574-82.
- [CrossRef] [PubMed] [Google Scholar]
- Safety and Efficacy of Ulnar Artery Approach for Percutaneous Cardiac Catheterization: Systematic Review and Meta-analysis. Catheter Cardiovasc Interv. 2018;91:1273-80.
- [CrossRef] [PubMed] [Google Scholar]
- Ulnar Artery Interventions Non-Inferior to Radial Approach: AJmer Ulnar ARtery (AJULAR) Intervention Working Group Study Results. J Invasive Cardiol. 2016;28:1-8.
- [Google Scholar]
- Transulnar Versus Transradial Artery Approach for Coronary Angioplasty: The PCVI-CUBA Study. Catheter Cardiovasc Interv. 2006;67:711-20.
- [CrossRef] [PubMed] [Google Scholar]
- Safety and Feasibility of Transulnar Versus Transradial Artery Approach for Coronary Catheterization in Non-selective Patients. Chin Med J (Engl). 2014;127:1222-8.
- [CrossRef] [PubMed] [Google Scholar]
- Safety and Efficacy of Transulnar Approach for Coronary Angiography and Intervention. Chin Med J (Engl). 2010;123:1774-9.
- [CrossRef] [Google Scholar]
- Same Wrist Intervention Via the Cubital (Ulnar) Artery in Case of Radial Puncture Failure for Percutaneous Cardiac Catheterization or Intervention: The Multicenter SWITCH Registry. Int J Cardiol. 2013;169:52-6.
- [CrossRef] [PubMed] [Google Scholar]







