Translate this page into:
Lactate Clearance – A surrogate for Mortality in Cardiogenic Shock
*Corresponding author: Dr. Nandikonda Abhinay Reddy, MBBS, DNB, General Medicine, Cardiology Resident, Department of Cardiology, Nizams Institute of Medical Sciences, Hyderabad, Telangana, India. abhinayreddy588@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Nandikonda AR, Bharathi Lakshmi VS. Lactate clearance – A surrogate for mortality in cardiogenic shock. Indian J Cardiovasc Dis Women 2023;8:180-6.
Abstract
Objectives:
Raised blood lactate levels are strongly associated with mortality in patients with cardiogenic shock. Recent practices of the early identification and initiation of mechanical circulatory support have improved outcomes in cardiogenic shock, but therapeutic targets to guide real-time clinical decision making are lacking. Recent evidence suggests that the degree and rate at which blood lactate levels decrease after the initiation of treatment is important in patient prognosis. With this background, lactate clearance has been suggested as a potential treatment target due to its independent association with morality.
Materials and Methods:
Lactate levels were measured at baseline and at 6, 12, and 24 h. Patients were grouped into survivors and non-survivors based on in-hospital mortality. Patients who had normal lactate (<2.0 mmoL/L) at baseline were excluded from the study. Statistical analysis done using appropriate tests.
Results:
Absolute lactate levels were compared between groups at baseline and 6, 12, and 24 h. Lactate clearance was calculated at 6, 12, and 24 h among survivors and non-survivors. In total, 90 patients were enrolled, and 65 (72.2%) of them survived to hospital discharge. Absolute blood lactate levels were 4.71 ± 1.36 mmoL/lit in survivors and 6.17 ± 2.88 mmoL/lit in non-survivors at baseline (P = 0.007). The mean lactate clearance at 6 h was 12.22 ± 85.96% in survivors and 12.98 ± 30.97% in non-survivors (P = 0.3). At 24 h, the mean lactate clearance was 54.63 ± 22.34% and 26.34 ± 19.3% in survivors and non-survivors, respectively (P < 0.01).
Conclusion:
Survivors had significantly greater lactate clearance at 12 and 24 h compared with non-survivors, suggesting that lactate clearance is an important prognostic marker in cardiogenic shock. These results further support the validity of lactate clearance as an appropriate surrogate for mortality and as a potential therapeutic target in clinical practice. Especially in centers lacking invasive hemodynamic monitoring.
Keywords
Lactate clearance
Cardiogenic shock
Absolute lactate values
Lactate in cardiac disease
Prognostic markers in shock
ABSTRACT IMAGE

INTRODUCTION
Physiologically normal activities and many pathological situations result in the production of lactic acid. The severity of the clinical course worsens when increased production coexists with impaired clearance. Importantly, the results of highly raised lactic acid levels can have serious impacts on hemodynamics and can result in death.[1] Blood lactate concentrations can serve as both a risk indicator and a treatment goal.[2,3] Clinicians need to be aware that hyperlactatemia can develop when tissue perfusion and oxygenation are sufficient. On the other hand, lactic acidosis typically happens when there is insufficient tissue perfusion, irregularities in glucose metabolism, and when using certain drugs.[4] Lactic acidosis is one of the major concerns for people who are providing care for severely ill patients.[5] Lactic acidosis with a pH lower than 7.2 negatively affects hemodynamics and calls for supportive care.[4] In addition, to shock and organ failure, high lactate levels are linked to an increased risk of mortality.[6] Higher 30-day in-hospital death rates are observed in patients with mildly elevated and intermediate levels. Through a variety of processes, lactic acidosis can reduce cardiac contractility and result in hyporesponsiveness to vasopressors.[7] Severe cases are more of a precipitator than a direct cause of mortality, though, as there is no proven causal relationship between lactic acidosis and mortality. Lactic acidosis probably causes the underlying comorbidities to get worse, which affects mortality.[8]
Jung et al. discovered that 6% of patients had severe lactic acidosis in their research of 2550 individuals.[9] Mortality in this group was 57%, and 83% of them received vasopressor treatment. Survival was correlated with the time required to reverse lactic acidosis and the severity of lactatemia. The mortality increases with the level and with the period until normalization and if severe lactic acidosis (pH < 7.2) coexists, the death rate is typically 50%. When the pH dropped below 7.0 due to severe lactic acidosis and shock, no survivors had been documented.[7] It is interesting to note that this contrasts with lactic acidosis linked to non-shock situations, where reported mortality was only 25% in metformin-induced lactic acidosis with pH values of 7.0.[10]
Less than two mmoL/L of lactate are considered normal, but lactate levels between 2 and 4 mmoL/L are considered hyperlactatemia. 4 mmoL/L or more of lactate constitutes severe levels. Other definitions of lactic acidosis include lactatemia >2 mmoL/L with a partial pressure of carbon dioxide ≤42 mmHg and pH ≤7.35.
Systemic hypotension, pulmonary congestion, and signs of inadequate end-organ perfusion were used to identify cardiogenic shock.[4] Early prognostic assessment in cardiogenic shock is essential for designing an individualized treatment plan. The most often utilized point-of-care parameter in cardiogenic shock is arterial lactate.[5] In septic shock, lactate reduction over time lactate clearance has been extensively investigated.[11] However, in cardiogenic shock, only limited data exist, and the prognostic value of lactate clearance is unknown.[12] We aim to study the blood lactate levels in patients of cardiogenic shock and to correlate with mortality rates in hospitals and investigate the valuable prognostic role of lactate clearance in cardiogenic shock, in the setting of limited availability of circulatory devices and access to invasive hemodynamic monitoring in average income countries. However, clinical research on this issue has been relatively insufficient, with the majority of studies being retrospective or prospective with limited sample sizes.
MATERIALS AND METHODS
Study design
This prospective observational study was conducted from July 2022 to September 2022 in a single center. The Institutional Ethics Committee approved the protocol for this study, and it was carried out in accordance with the Helsinki Declaration. Before participation, all patients or their legal representatives provided written informed consent. All the patients underwent brief targeted histories obtained from prehospital sources, medical records, and from attendees. The clinical examination is directed toward uncovering the type of shock and obtaining laboratory investigations such as complete blood counts, renal function tests, liver function tests, urine analysis, blood gas analysis, cardiac troponins, N-terminal pro-brain natriuretic peptide (NT pro-BNP) levels, D-dimer levels, C-reactive protein, procalcitonin levels, electrocardiogram and imaging with point of care ultrasound, 2D echocardiogram, chest X-ray, and abdominal X-ray, when indicated clinically. Patients older than 18 years, presenting to the cardiology department with cardiogenic shock whose arterial blood lactate levels were >2 mmoL/lit, were included in the study. Patients more than 90 years of age, pregnant, shock of non-cardiac causes, out-of-hospital cardiac arrest, and lactic acidosis of non-cardiac causes such as drug-induced lactic acidosis, liver disease, malignancy, and alcoholism were excluded from the study. Patients have been categorized according to their clinical status using the society for cardiovascular angiography and interventions (SCAI) shock classification system [Figure 1].[13] All the patients were given guideline-directed management and assessed at appropriate time intervals with clinical, laboratory, and hemodynamic parameters including complete blood count, blood group and typing, blood urea, serum creatinine, serum lipids, electrolytes, liver function tests, blood sugars, thyroid-stimulating hormone, NT pro-BNP, Hs Trop I, chest X-ray, electrocardiogram, echocardiogram, and arterial blood gases. Blood lactate levels of the patients were collected at baseline (L1), after 6 h (L2), 12 h (L3), and 24 h (L4). Lactate clearance was calculated according to the corresponding time points. All the necessary investigations such as coronary angiogram and cardiac catheterization study were performed according to the clinical condition.

- SCAI shock classification pyramid. SCAI: Society for cardiovascular angiography and interventions.
Lactate Clearance(LC) ={lactate initial(L1) − lactate delayed} / lactate initial(L1) × 100 (expressed as percentage).[14]
LC1={(L1-L2)/L1}*100, LC2={(L1-L3)/L1}*100, LC3={(L1-L4)/L1}*100.
Statistical analysis
Data were collected and compiled using Microsoft Excel and statistical analysis will be done using SSPS v20.0. Patients were divided into survivors and non-survivors based on in-hospital mortality. Results on continuous variables will be presented as mean and standard deviation. Results on categorical variables will be presented as numbers or percentages. Paired t-test was used for statistical analysis. P < 0.05 was considered statistically significant.
We analyzed absolute lactate values for both groups and analyzed the lactate clearances according to the time intervals for both groups. Utilizing univariate logistic regression models, the unadjusted connection between baseline characteristics including absolute lactate values and lactate clearances and outcomes was evaluated.
P values for continuous variables were calculated using the paired t-test, and for categorical variables, the Mann– Whitney test was applied. Receiver operator curves were plotted for absolute lactate values and lactate clearance values according to time points [Figures 7 and 8].
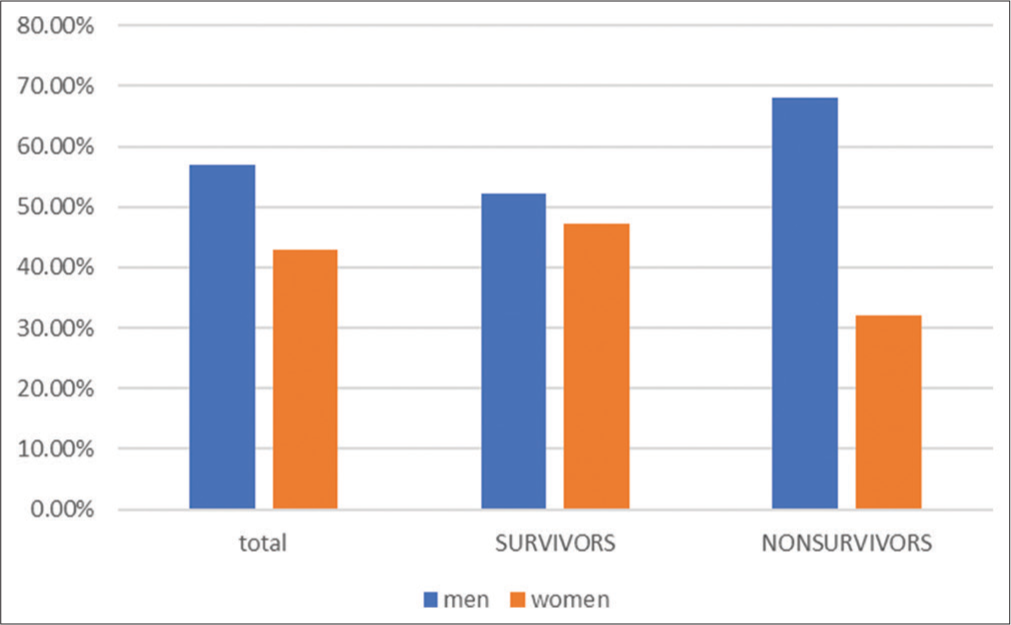
- Gender comparison between the groups (expressed in percentages of total participants).
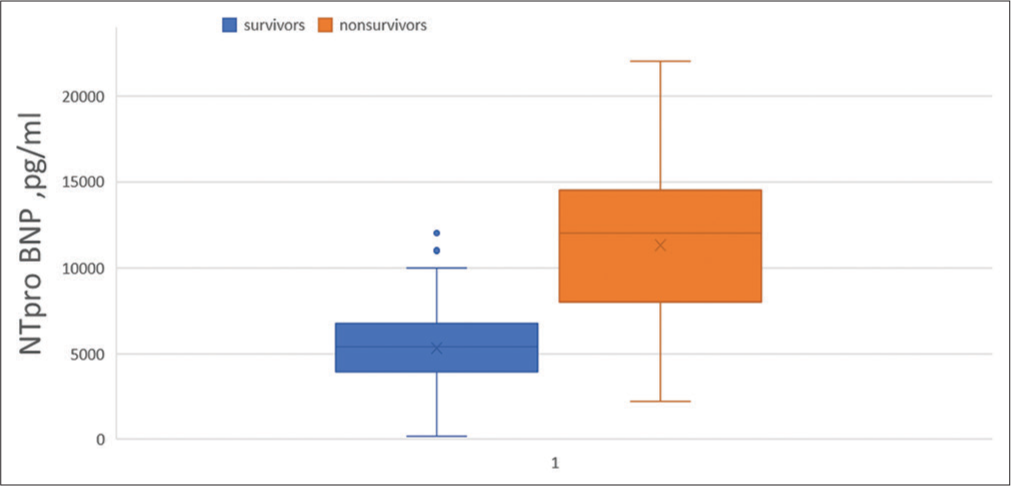
- Box whisker plot diagrams comparing NT pro-BNP levels between groups (expressed in pg/mL). NT pro-BNP: N-terminal pro-brain natriuretic peptide.
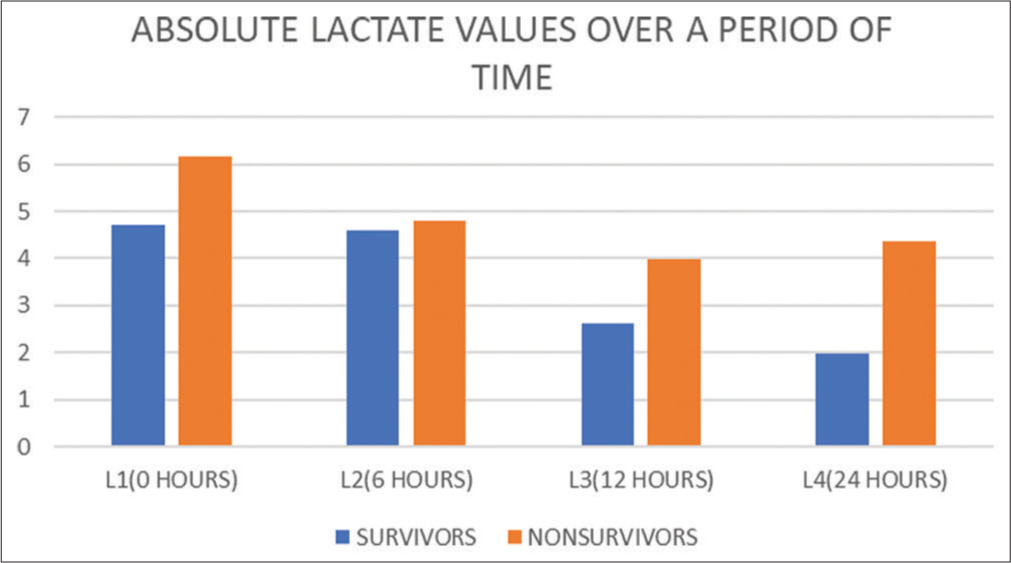
- Bar diagrams comparing absolute lactate values (mmoL/ lit) between groups at various time points.
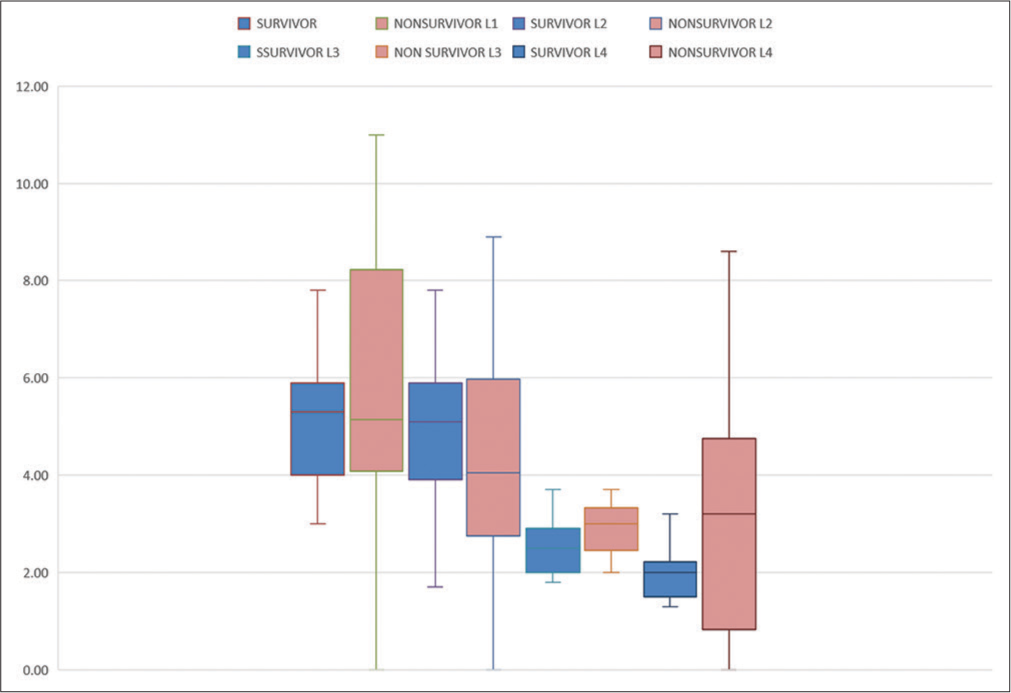
- Box and whisker plots diagrams comparing the absolute lactate values at various time points grouped between survivors and non-survivors (L1: Absolute lactate at baseline, L2: Absolute lactate at 6 h, L3: Absolute lactate at 12 h, and L3: Absolute lactate at 24 h).
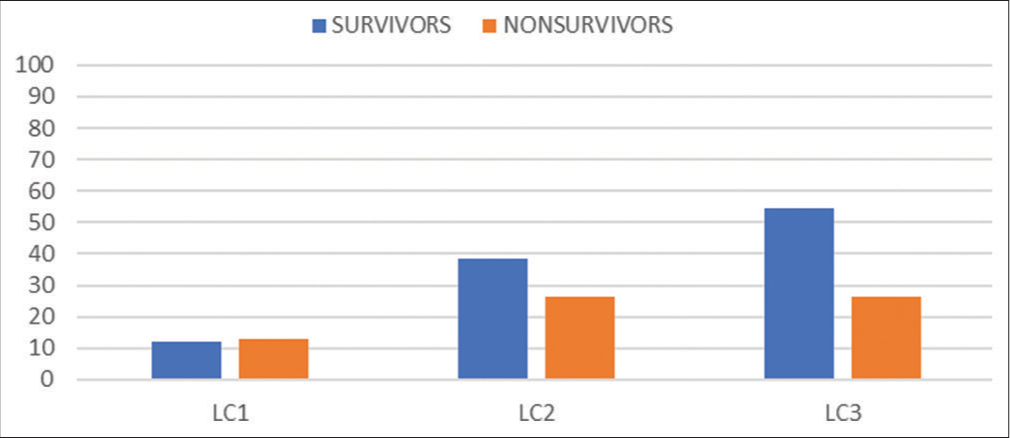
- Bar diagrams comparing the lactate clearances over a period of time between survivors and non-survivors expressed in percentages (LC1: Lactate clearance at 6 h, LC2: Lactate clearance at 12 h, and LC3: Lactate clearance at 24 h).
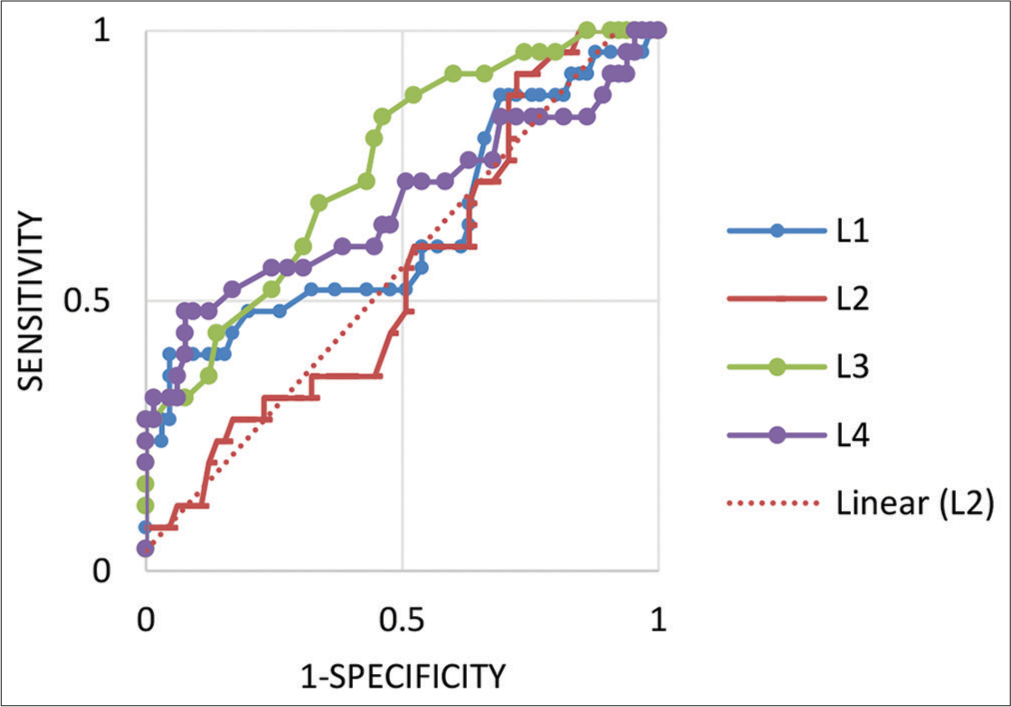
- Receiver operating curves plotted for the absolute lactate values taken over a specified period (L1: Absolute lactate at baseline, L2: Absolute lactate at 6 h, L3: Absolute lactate at 12 h, and L4: Absolute lactate at 24 h).
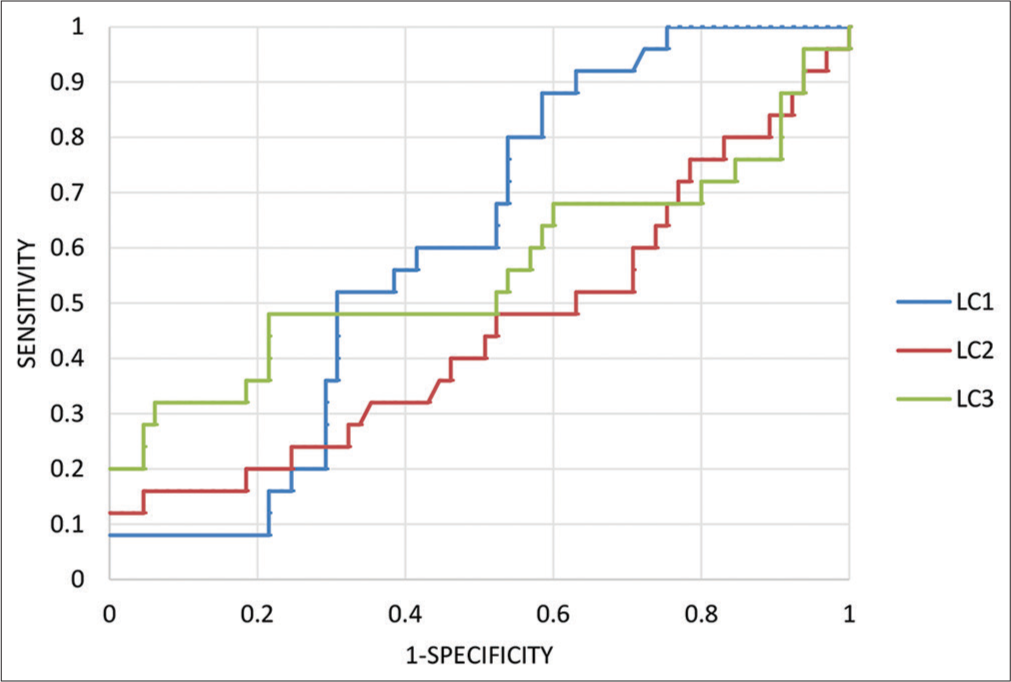
- Receiver operated curves plotted for the lactate clearances at specified period of time (LC1: Lactate clearance at 6 h, LC2: Lactate clearance at 12 h, and LC3: Lactate clearance at 24 h).
RESULTS
Total of 90 patients were enrolled, of those 65 patients (72.2%) survived and 25 patients (27.8%) expired in the hospital. The baseline characteristics of survival and the non-survival group are shown in [Table 1]. The median absolute lactate levels at baseline in the survival group were 4.8 mmoL/lit (interquartile range [IQR] 3.8–5.6 mmoL/lit) and 5.5 mmoL/lit (IQR 4.1–8.2 mmoL/lit) in non-survivors (P = 0.0074). Median absolute lactate values at 12 h (L3) in the survivor’s group were 2.6 mmoL/lit (IQR 2.2–3.1 mmoL/lit) and 3.1 mmoL/lit (IQR 2.8– 3.38 mmoL/lit) in non-survivors (P = 0.0002). Median absolute lactate values at 24 h were 2.0 mmoL/lit (IQR 1.3–2.5 mmoL/lit) in survivors and 3.7 mmoL/lit (IQR 2.8–4.9 mmoL/lit) in non-survivor group (P < 0.05) [Figures 4 and 5]. The median lactate clearance at 24 h was 56.7% (IQR 41.9–69.5%) compared to the 25.36% (IQR 13.62–37.86%) with P < 0.05 [Figure 6]. Among survivors, 47% were women and there are 32% women in the non-survivor group (P = 0.01) [Figure 2]. All the other baseline characteristics were similar between both the groups.
| Baseline characteristics | Total, 90 | Survivors, 65 (72.2%) | Non-survivors, 25 (27.8%) | P-value |
|---|---|---|---|---|
| Age, yrs | 65.58±12.69 | 67.37±11.82 | 60.92±13.66 | 0.1228 |
| Height, cm | 156.87±12.67 | 156.66±13.31 | 157.4±10.83 | 0.5686 |
| Weight, kg | 67.17±14.58 | 68.54±14.8 | 63.6±13.34 | 0.0509 |
| BMI, kg/m2 | 27.85±7.7 | 28.57±8.16 | 25.96±5.97 | 0.1882 |
| Male | 51 (56.7%) | 34 (52.3%) | 17 (68%) | 0.053 |
| Female | 39 (43.3%) | 31 (47.7%) | 8 (32%) | 0.01 |
| HTN | 47 (52%) | 35 (54%) | 12 (48%) | 0.2468 |
| DM | 51 (57%) | 36 (55%) | 16 (64%) | 0.3380 |
| Current smoker | 22 (24%) | 15 (23.1%) | 7 (28%) | 0.5031 |
| Prior CAD with PCI | 36 (40%) | 23 (35.4%) | 13 (52%) | 0.2871 |
| CAD with CABG | 10 (11.1%) | 9 (13.8%) | 2 (8%) | 0.8897 |
| COPD | 9 (10%) | 7 (10.8%) | 2 (8%) | 0.1738 |
| Stroke | 10 (11.1%) | 7 (10.8%) | 3 (12%) | 0.5928 |
| PAD | 10 (11.1%) | 6 (9.2%) | 4 (16%) | 0.2835 |
| CKD | 19 (21.1%) | 14 (21.5%) | 5 (20%) | 0.7689 |
| HR, bpm | 96.32±21.7 | 92.94±20.31 | 105.12±22.72 | 0.0146 |
| SBP, mmHg | 98.56±26.04 | 98.78±28.51 | 97.96±18.09 | 0.8428 |
| DBP, mmHg | 59.39±14.93 | 59.58±15.92 | 58.88±11.94 | 0.5689 |
| MBP, mmHg | 72.44±17.25 | 72.65±18.69 | 71.91±12.74 | 0.6710 |
| CREAT, mg/dL | 1.52±0.93 | 1.55±1.04 | 1.46±0.52 | 0.7600 |
| SCAI class | ||||
| C | 66 (73.3%) | 51 (78.46%) | 15 (60%) | 0.08 |
| D | 20 (22.2%) | 12 (18.4%) | 8 (32%) | 0.003 |
| E | 4 (4.4%) | 2 (3%) | 2 (8%) | 0.007 |
| eGFR mL/min | 54.42±30.01 | 55.07±30.71 | 52.73±28.04 | 0.5397 |
| EF, % | 41±13.23 | 40.82±13.5 | 41.48±12.48 | 0.9742 |
| L1 (0 h), mmoL/lit | 5.11±2.02 | 4.71±1.36 | 6.17±2.88 | 0.0074 |
| L2 (6 h), mmoL/lit | 4.77±2.46 | 4.6±2.65 | 4.79±2.37 | 0.7427 |
| LC1, % | 7.46±75.63 | 12.22±85.96 | 12.98±30.97 | 0.3988 |
| L3 (12 h), mmoL/lit | 3.03±1.43 | 2.63±0.62 | 3.99±2.52 | 0.0002 |
| LC2, % | 34.81±28.15 | 38.27±27.06 | 26.49±30.95 | 0.0986 |
| L4 (24 h), mmoL/lit | 2.53±1.81 | 1.97±0.81 | 4.36±3.01 | 0.0001 |
| LC3, % | 47.97±24.55 | 54.63±22.34 | 26.34±19.3 | 0.0001 |
| HS TROP I, ng/mL | 765.17±1988.26 | 472.8±838.85 | 1525.32±3406.15 | 0.3560 |
| NT pro BNP, pg/mL | 8713±7398 | 5411±2463 | 12044±5097 | <0.05 |
BMI: Body mass index, HTN: Hypertension, DM: Diabetes mellitus, PCI: Percutaneous coronary intervention, CABG: Coronary artery bypass grafting, CAD: Coronary artery disease, COPD: Chronic obstructive pulmonary disease, PAD: Peripheral artery disease, CKD: Chronic kidney disease, HR: Heart rate, SBP: Systolic blood pressure, DBP: Diastolic blood pressure, MBP: Mean blood pressure, CREAT: Creatinine, SCAI: Society for cardiovascular angiography and interventions, eGFR: Estimated glomerular filtration rate, EF: Ejection fraction, HS TROP I: High-sensitivity cardiac troponin I, NT pro BNP: N-terminal pro-brain natriuretic peptide, LC1: Lactate clearance at 6 h, LC2: Lactate clearance at 12 h, LC3: Lactate clearance at 24 h, L1: Absolute lactate at baseline, L2: Absolute lactate at 6 h, L3: Absolute lactate at 12 h, L3: Absolute lactate at 24 h
The non-survival group had higher heart rates of 110 bpm (IQR 94–120 bpm) compared to survivors of 95 bpm (IQR 78–110 bpm) (P = 0.01). However, mean blood pressure was similar between both groups.
Patients were classified based on SCAI cardiogenic shock classification system [Figure 1] into appropriate classes and analyzed between survivors and non-survivors groups.[15] The majority of patients are in SCAI class C (total 73.3%), 78.46% in the survivor’s group, and 60% in the non-survivor group (P = 0.08). The non-survivor group had more patients in SCAI class D and E compared to the survivor group (P = 0.003, P = 0.007, respectively). The non-survivor group had more levels of NTpro BNP than the survivor group ([12044 ± 5097] vs. [5411 ± 2463] pg/mL, P < 0.05) [Figure 3].[16] Our study contains the majority of patients with ischemic cardiomyopathy as a major cause of cardiogenic shock (total = 52%), although no statistically significant differences were found in both group (P > 0.05).
DISCUSSION
There are limited data currently available on the prognostic relevance of lactate clearance in CS patients. Recent evidence has shown that lactate clearance is a clinically reliable tool for risk stratification, mostly established in septic shock. Effective lactate clearance early in the hospital course is actually linked to a lower mortality rate in patients with sepsis and septic shock. In addition, lactate non-clearance-defined as a drop in lactate of <10% from the initial point-was a reliable independent predictor of death in a multicenter cohort of patients with septic shock.[17] Complete lactate clearance is a significant and independent predictor of in-hospital survival in patients with cardiogenic shock, based on a post hoc analysis of the DOREMI (Dobutamine Compared to Milrinone in the Treatment of Cardiogenic Shock) trial.[5,14]
Recently, a large cohort of patients undergoing intra-aortic balloon pump (IABP) therapy for cardiogenic shock investigated arterial lactate’s prognostic significance at various time points, demonstrating that its estimate after 8 h was superior to baseline and clearance levels.[15] However, compared to other MCS like Impella or venoarterial extracorporeal membrane oxygenation (VA-ECMO), IABP offers a lesser improvement in cardiac output.[16-18] The study population and devices used in the previous studies on the effect of arterial lactate in cardiogenic shock with MCS are heterogeneous. However, in this scenario, the optimal cutoff lactate value to identify patients with better prognoses has not yet been established.
We investigated the association between serum lactate clearance, absolute lactate values after initiation of shock treatment, and clinical outcomes in patients with CS. The main finding of our study is that higher 24-h lactate clearance coupled with lower baseline absolute lactate values was associated with reduced risk of in-hospital mortality. Serum lactate fluctuates about ongoing tissue hypoxia. Because lactate clearance suggests that oxygen delivery has been restored, a decrease in serum lactate is a sign of effective resuscitation.[18]
Attaná et al. reported the prognostic role of lactate clearance in CS to identify a subgroup of patients at increased risk for death.[17] The dynamic nature of lactate levels were demonstrated by Slottosch et al. in a study done on patients undergoing ECMO, from the observations of 24 h lactate clearance values and comparing them with 30-day mortality.[19] In our study, women had less mortality than men, in contrast to the worse prognosis in women that is observed.[20-22] Twelve hour median absolute lactate values between both groups were significant revealing the superior performance of 12-h model compared to the 6-h model. These results were similar to the study done by Li et al., who studied the early lactate behavior in patients treated with ECMO.[23] We found that 24-h lactate clearance predicts in-hospital mortality greater than absolute lactate values at baseline and 12 h. There was no significant difference in lactate clearance at 6 h and 12 h in survivors and non-survivors. It indicates that escalating the shock management regimens in patients with high absolute lactate levels by means of escalating the dosage of vasopressors, and timely employment of mechanical circulatory devices such as IABP, IMPELLA, and VA-ECMO may have a mortality benefit.
Limitations
This is a single-center and prospective observational study with a small sample size
We have not included invasive hemodynamic parameters in the analysis
The majority of patients are of ischemic etiology.
CONCLUSION
In contrast to non-survivors, survivors had considerably higher lactate clearance at 24 h, indicating that lactate clearance is a significant prognostic indicator in cardiogenic shock. The validity of lactate clearance as a potential surrogate for mortality and a possible therapeutic target in clinical practice is further supported by these findings. Lactate clearance can be utilized as a therapeutic target to direct treatment plans in facilities without the availability of invasive hemodynamic monitoring and mechanical circulatory devices.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Audio summary available at
Financial support and sponsorship
Nil.
References
- Association between serum lactate levels and mortality in patients with cardiogenic shock receiving mechanical circulatory support: A multicenter retrospective cohort study. BMC Cardiovasc Disord. 2020;20:496.
- [CrossRef] [PubMed] [Google Scholar]
- Lactate: Biomarker and potential therapeutic target. Crit Care Clin. 2011;27:299-326.
- [CrossRef] [PubMed] [Google Scholar]
- The management of cardiogenic shock and hemodynamic support devices and techniques In: Interventional Cardiology. New Jersey, United States: John Wiley and Sons. Ltd; 2022. p. :167-72. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/9781119697367.ch14 [Last accessed on 2023 Jan 02]
- [CrossRef] [Google Scholar]
- Arterial lactate in cardiogenic shock: Prognostic value of clearance versus single values. JACC Cardiovasc Interv. 2020;13:2208-16.
- [CrossRef] [PubMed] [Google Scholar]
- Association between the acidemia, lactic acidosis, and shock severity with outcomes in patients with cardiogenic shock. J Am Heart Assoc. 2022;11:e024932.
- [CrossRef] [PubMed] [Google Scholar]
- Prognostic relevance of serum lactate kinetics in critically ill patients. Intensive Care Med. 2019;45:55-61.
- [CrossRef] [PubMed] [Google Scholar]
- Serial lactate determinations during circulatory shock. Crit Care Med. 1983;11:449-51.
- [CrossRef] [PubMed] [Google Scholar]
- Severe metabolic or mixed acidemia on intensive care unit admission: Incidence, prognosis and administration of buffer therapy. A prospective, multiple-center study. Crit Care. 2011;15:R238.
- [CrossRef] [PubMed] [Google Scholar]
- Metformin-induced lactic acidosis with emphasis on the anion gap. Proc Bayl Univ Med Cent. 2015;28:31-3.
- [CrossRef] [PubMed] [Google Scholar]
- Lactate level versus lactate clearance for predicting mortality in patients with septic shock defined by sepsis-3. Crit Care Med. 2018;46:e489-95.
- [CrossRef] [PubMed] [Google Scholar]
- Blood lactate as prognostic indicator of survival in patients with acute myocardial infarction. Circ Shock. 1982;9:307-15.
- [Google Scholar]
- SCAI clinical expert consensus statement on the classification of cardiogenic shock: This document was endorsed by the American College of Cardiology (ACC), the American Heart Association (AHA), the Society of Critical Care Medicine (SCCM), and the Society of Thoracic Surgeons (STS) in April 2019. Catheter Cardiovasc Interv. 2019;94:29-37.
- [CrossRef] [PubMed] [Google Scholar]
- Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med. 2004;32:1637-42.
- [CrossRef] [PubMed] [Google Scholar]
- SCAI SHOCK Stage Classification Expert Consensus Update: A Review and Incorporation of Validation Studies: This statement was endorsed by the American College of Cardiology (ACC), American College of Emergency Physicians (ACEP), American Heart Association (AHA), European Society of Cardiology (ESC) Association for Acute Cardiovascular Care (ACVC), International Society for Heart and Lung Transplantation (ISHLT), Society of Critical Care Medicine (SCCM), and Society of Thoracic Surgeons (STS) in December 2021. J Soc Cardiovasc Angiogr Interv. 2022;1:100012.
- [Google Scholar]
- NTproBNP: An important biomarker in cardiac diseases. Curr Top Med Chem. 2013;13:82-94.
- [CrossRef] [PubMed] [Google Scholar]
- Lactate clearance in cardiogenic shock following ST elevation myocardial infarction: A pilot study. Acute Card Care. 2012;14:20-6.
- [CrossRef] [PubMed] [Google Scholar]
- Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: A randomized clinical trial. JAMA. 2010;303:739-46.
- [CrossRef] [PubMed] [Google Scholar]
- Lactate and lactate clearance as valuable tool to evaluate ECMO therapy in cardiogenic shock. J Crit Care. 2017;42:35-41.
- [CrossRef] [PubMed] [Google Scholar]
- An Asian perspective on gender differences in in-hospital and long-term outcome of cardiac mortality and ischemic stroke after primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. J Stroke Cerebrovasc Dis. 2022;31:106215.
- [CrossRef] [PubMed] [Google Scholar]
- Sex differences in mortality after an acute coronary syndrome increase with lower country wealth and higher income inequality. Rev Esp Cardiol Engl Ed. 2022;75:392-400.
- [CrossRef] [PubMed] [Google Scholar]
- Gender differences in all-cause mortality after acute myocardial infarction: Evidence for a gender-age interaction. J Clin Med. 2022;11:541.
- [CrossRef] [PubMed] [Google Scholar]
- The early dynamic behavior of lactate is linked to mortality in postcardiotomy patients with extracorporeal membrane oxygenation support: A retrospective observational study. J Thorac Cardiovasc Surg. 2015;149:1445-50.
- [CrossRef] [PubMed] [Google Scholar]







