Translate this page into:
Heart Failure in Pregnancy
Asha Mahilmaran, MD, DNB, DM, IFESC, FCSI, FACC 21/7A, Thandavarayan Mudali Street, Washermanpet, Chennai 600021, Tamil Nadu India drashamahil@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Cardiovascular mortality remains an important cause of maternal mortality other than the obstetric direct causes. Most cardiovascular deaths occur due to heart failure. Rheumatic heart diseases (RHD) account for more than two-thirds of heart diseases in pregnancy in low–middle income countries. Among RHD patients, 49% of patients with severe mitral stenosis, 31% with moderate mitral stenosis, and 23% with moderate to severe mitral regurgitation present with heart failure during pregnancy. In the U.K. registry, 25% of patients had heart failure due to cardiomyopathy. Congenital heart diseases such as atrial septal defect with severe pulmonary hypertension, significant atrioventricular valve regurgitation, peripartum, or dilated cardiomyopathy are less common causes of heart failure in pregnancy. Coronary artery diseases usually present as acute coronary syndromes during pregnancy, and heart failure as presentation is a rare occurrence. Preeclampsia and chronic hypertension can lead to increased vascular resistance, diastolic dysfunction, acute pulmonary edema, and acute heart failure. Two-thirds of heart diseases are diagnosed during the antepartum period itself. Preconception counseling, optimal medical therapy and avoidance of teratogens, and planning interventional or surgical therapies in patients with severe or moderate valvular diseases and congenital heart diseases will enable patients to enter the pregnancy well compensated. During pregnancy and postpartum, close surveillance and a multidisciplinary approach involving the obstetrician, cardiologist, physician, and anesthetist will lead to better maternal and fetal outcomes.
Keywords
mitral stenosis
mitral regurgitation
peripartum cardiomyopathy
rheumatic heart disease
Introduction
Heart failure (HF) is a common cause of maternal mortality and morbidity. Cardiac disorders are an indirect cause of maternal mortality that contributes to about 25% of the total mortality during pregnancy. Congenital heart diseases (CHDs) are the leading cause of cardiac mortality in developed countries. Rheumatic heart diseases (RHDs) are the dominant cause of HF and cardiac death in underdeveloped and developing nations. There is an increasing prevalence of diabetes, hypertension, and obesity in younger women, and women with advanced age are getting into pregnancy due to cultural changes and assisted reproductive technologies offered to older women. Combination of these two factors is likely to result in increased cardiac events due to coronary artery disease (CAD).
Physiologic Changes during Pregnancy
There is an increase in cardiac output, decrease in systemic vascular resistance (SVR), and tachycardia during pregnancy, all of which can jeopardize the delicate balance in a previously compromised patient and precipitate overt HF and result in increased morbidity and mortality. Cardiac output increases by 30 to 50%. The increase starts in the first trimester and peaks toward the end of the second trimester. Both the ventricles increase in mass and volume during pregnancy. During delivery, there is an increase in heart rate (HR), blood pressure, and SVR with each uterine contraction that places enormous stress on a failing heart. Postpartum, there is a sudden increase in preload due to decompression of the inferior vena cava by the uterus and emptying of placenta into the maternal circulation.1
Symptoms and Signs of Heart Failure in Pregnancy
The diagnosis of HF is challenging, as some of the common symptoms such as breathlessness, palpitation, swelling legs and elevated JVP, and systolic functional murmurs are common in a normal pregnancy. However, breathlessness that lasts for a longer time after exertion, orthopnea, paroxysmal nocturnal dyspnea, presence of thrill, and diastolic murmurs are uncommon in a normal pregnancy, which should alert to the presence of pathologic heart disease. Syncope and excessive palpitations require evaluation. There should be a low threshold to order for an echo during pregnancy.
Investigations
-
Electrocardiogram (ECG) may be used to diagnose chamber enlargement, arrhythmias, and conduction defects.
-
Echo is the most important investigation to assess the left and right ventricular function, valve disease, congenital defects, and diseases of the aorta. It is very important to look for pulmonary hypertension, the severity of which is an important determinant of outcomes in many of the conditions.
-
Chest X-ray is not routinely required for the diagnosis as it is better to avoid radiation.
-
Ultrasound of the chest can be used to diagnose pulmonary congestion.
-
N-terminal pro-brain natriuretic peptide (NT-proBNP) may be slightly elevated in normal pregnancy, but gross elevation is abnormal.2
-
Magnetic resonance imaging (MRI) can be used in myocarditis evaluation.
Etiology of Heart Failure in Pregnancy
The most common cause of HF in pregnancy is RHD in 90% of cases in India and other low-middle-income countries. In the developed nations, cardiomyopathy, and CHD are the leading causes. Approximately 75% of the cases are diagnosed in the antenatal period, whereas 25% are diagnosed during pregnancy.3 The prognosis is worse in patients diagnosed during pregnancy or labor.
Rheumatic Heart Disease
Moderate or severe mitral stenosis (MS), mixed valvular lesions, aortic stenosis, mitral regurgitation (MR), and tricuspid stenosis can all predispose to HF. Presence of atrial fibrillation (AF) and anemia can increase the chance of HF.
In the REMEDY study (Global Rheumatic Heart Disease Registry), 25% of the RHD women had HF and 20% of them had left ventricular dysfunction before pregnancy.4
Among patients with severe MS, that is, mitral valve area (MVA) < 1 cm2, 49% develop HF, moderate MS, MVA 1 to 1.5 cm2, 31% develop HF. HF occurs in 15% of patients with mild MS.
β-Blockers and diuretics should be used. Digoxin and anticoagulants are recommended in AF patients.
Hence, the current European Society of Cardiology (ESC) guidelines on heart disease in pregnancy advocate percutaneous mitral valvuloplasty in asymptomatic patients with severe MS or symptomatic patients with moderate MS before pregnancy.5
Severe MS can be subjected to percutaneous transvenous mitral commissurotomy (PTMC) during the second trimester of pregnancy after the fourth month.6 In my experience, I have done PTMC for two women with severe MS and severe pulmonary hypertension during the second trimester with good maternal and fetal outcomes. It is important to minimize radiation by decreasing the fluoroscopy time, the avoidance of cineangiogram, use of echo guidance and pelvic shield, and planning the procedure after the period of organogenesis.7
Mixed MS and moderate MR have a prognosis similar to severe MS. They present with greater challenge as only surgical option is available. Before pregnancy, bioprosthetic valve option should be discussed.
Mitral regurgitation is tolerated better than stenosis, but patients entering pregnancy with New York Heart Association (NYHA) class III or IV symptoms, severe pulmonary hypertension, or left ventricular dysfunction are World Health Organization (WHO) class III risk patients and have a worse outcome in pregnancy. In the REMEDY study, 23% of patients with severe MR developed HF.
A 27-year-old woman, primigravida, presented with severe MR, paroxysmal nocturnal dyspnea, and orthopnea at 6 weeks of pregnancy. She had RHD, severe MR, severe pulmonary hypertension, and normal left ventricular function. She underwent a mitral valve prolapse (MTP), followed by mitral valve replacement (MVR) with a bioprosthetic valve.
Aortic stenosis in asymptomatic individuals may be tolerated. Severe symptomatic aortic stenosis tolerates pregnancy poorly and should have an intervention before pregnancy. Balloon aortoplasty can be done in severely symptomatic patients during pregnancy.8
Aortic regurgitation is generally well tolerated in the absence of left ventricular dysfunction. Acute aortic regurgitation or MR may be poorly tolerated and present as acute decompensated heart failure (ADHF) and may necessitate termination of pregnancy.
RHD patients should continue the rheumatic secondary prophylaxis and take precautions to avoid infection and sepsis.
In patients with postoperative valve, the major issue is management of anticoagulation. Warfarin is avoided in the first trimester to prevent the teratogenic effect. Low-molecular-weight heparin (LMWH) in the first trimester and after 36 weeks and stopping 24 hours before delivery is recommended. If the warfarin dose required is more than 5 mg or phenocoumarol dose > 3 mg, it is recommended not to use vitamin K antagonist (VKA) during the second trimester and use only LMWH throughout the pregnancy. HF occurs only when there is severe left ventricular dysfunction (Table 1).
|
Drug |
Safety during pregnancy |
|---|---|
|
Abbreviations: ACEI, angiotensin-converting enzyme inhibitor; ADHD, acute decompensated heart failure; ARB, angiotensin receptor blocker; ARNI, angiotensin receptor-neprilysin inhibitor; LMWH, low-molecular-weight heparin; NOAC, novel oral anticoagulant; UFH, unfractionated heparin; VKA, vitamin K antagonist. |
|
|
ACEI/ARB |
Contraindicated because of renal and other fetal toxicity |
|
Hydralazine and long-acting nitrates |
Safe to use |
|
β-Blocker |
β1 Selective drugs preferred, β2-receptor blockers have antitocolytic effect. |
|
Diuretics |
Should be used sparingly as can cause reduced placental flow |
|
Frusemide and hydrochlorothiazide |
Can be used |
|
Aldosterone antagonists |
Teratogenic, to be avoided |
|
Amiloride |
Can be used, not teratogenic |
|
Digoxin |
Can be used |
|
Ivabradine |
No known data, to be avoided |
|
ARNI |
Contraindicated |
|
Amiodarone |
Contraindicated, hypothyroidism in 9%, hyperthyroidism, growth retardation, premature birth |
|
UFH, LMWH |
Can be used in th prevention and treatment of thromboembolism, mechanical valve, atrial fibrillation |
|
NOACs |
Contraindicated |
|
VKA |
Teratogenic, to be avoided in first trimester, can be used in second trimester if dose of acenocoumarol < 3 mg or phenocoumarol < 5 mg. |
|
Nitroglycerine |
Can be used in ADHF management secondary to hypertension, left ventricular dysfunction, or severe valve regurgitation |
In the sub-Saharan African study, the causes of maternal death in valvular heart disease during pregnancy were HF in 47%, pulmonary embolism in 17%, cardiogenic shock in 12%, septic shock in 12%, and fatal hemorrhage in 12%. Maternal death was associated with severe MS, advanced NYHA class, severe tricuspid regurgitation, and HF.9
Congenital Heart Disease
Operated congenital defects such as ventricular septum defect (VSD), atrial septum defect (ASD), and patent ductus arteriosus (PDA) carry a low risk. The prognosis is majorly dependent on the presence of pulmonary hypertension. The prognosis in CHD is dependent on residual lesions, ventricular function, and pulmonary hypertension. HF in CHD is rather uncommon. Myxomatous valve with regurgitation, severe congenital bicuspid aortic stenosis, ASD with severe pulmonary hypertension, systemic ventricular dysfunction, or atrioventricular valve regurgitation are some of the causes of HF during pregnancy due to congenital diseases.
Cardiomyopathy
Dilated cardiomyopathy (DCM), peripartum cardiomyopathy (PPCM), hypertrophic cardiomyopathy, and arrhythmogenic right ventricular dysplasia have been reported during pregnancy.
Peripartum cardiomyopathy is the most common type of cardiomyopathy during pregnancy characterized by left ventricular ejection fraction (LVEF) < 45% and symptoms of HF in the last trimester or first 6 months postpartum.
In PPCM, the prognosis is poor in patients with LVEF < 20%, NYHA class III or IV, biventricular dysfunction, and severe pulmonary hypertension. More than 60% of patients recover their left ventricular function over a period of 1 year. Future pregnancies carry a very high risk of recurrence in patients with residual left ventricular dysfunction and should be avoided.10 In patients who recover LVEF to normal, there is still a risk of recurrence and these patients preferably should also avoid future pregnancies, or if they choose to get pregnant, they require close monitoring.
Dilated cardiomyopathy can be present prior to pregnancy or detected during pregnancy. The prognosis is poor in patients with LVEF < 20% and advanced NYHA class.
Hypertrophic cardiomyopathy is generally well tolerated during pregnancy. Genetic counseling and sudden death risk assessment are similar to other nonpregnant patients.
Patients with right ventricular dysplasia tolerate pregnancy reasonably well, but if at high risk for sudden cardiac death (SCD), automatic implantable cardioverter-defibrillator (AICD) implantation can be done during pregnancy with echo guidance only or minimal use of fluoroscopy.
Hypertension
Chronic hypertension is present in 3% of pregnancies, and they are more prone to preeclampsia and eclampsia that may cause acute pulmonary edema due to diastolic dysfunction. Chronic hypertension may be associated with left ventricular dysfunction rarely and can lead to HF.
Coronary Artery Disease
Coronary artery disease (CAD) usually presents as acute coronary syndrome (ACS) due to atherosclerotic CAD. It is a rare cause of HF. Younger women with multiple cardiovascular risk factors or older women may pose challenge in future. Mortality is decreased by revascularization by angioplasty and heparin, and antiplatelet agents have been used. Spontaneous coronary dissection is more common in pregnancy and labor.
Diseases of Aorta
Takayasu’s arteritis can present with hypertension and HF during pregnancy. Ischemic symptoms can occur due to involvement of coronary ostia by arteritis. Marfan’s syndrome can be associated with aortic root dilatation, aortic dissection, or acute aortic regurgitation resulting in acute HF. Syphilis is uncommon nowadays but is a cause of coronary arteritis and aortic root enlargement with aortic regurgitation. Coarctation of aorta can present with hypertension, HF, or dissection.
Management of Heart Failure during Pregnancy
-
Diet—salt and water restriction.
-
Loop diuretics are the cornerstone of therapy for decongestion.
-
Potassium-sparing diuretic amiloride can be used. Aldosterone antagonists are teratogenic and should be avoided in pregnancy.
-
Angiotensin-converting enzyme inhibitor/angiotensin receptor blocker (ACEI/ARB) are contraindicated due to risk of renal agenesis in the fetus. ACEI can be used during lactation.
-
β-Blockers can be used. Only cardioselective agents such as metoprolol or bisoprolol should be used. They are beneficial in MS and DCM or PPCM with left ventricular dysfunction and also in AF patients.
-
Digitalis can be used safely in patients with overt HF and AF rate control.
-
Hydralazine drugs can be used in HF due to regurgitant lesions or left ventricular dysfunction.
-
Thromboprophylaxis is recommended in patients with severe left ventricular dysfunction and failure with LMWH, enoxaparin 40 mg once daily.
-
Patients with RHD and AF or prosthetic valve need anticoagulation with LMWH during the first trimester and after 36 weeks of pregnancy may use acenocoumarol or warfarin during the second and third trimesters, if the dose required is less than 5 mg warfarin or 3 mg of acenocoumarol. If the dose required is high, they should continue on LMWH with factor X a level monitoring once a week5
-
Rheumatic secondary prophylaxis with penicillin should be continued throughout the pregnancy. Infective endocarditis prophylaxis before surgery is recommended.11
Comorbidities
Iron deficiency anemia should be corrected. Thyroid diseases should be addressed.
Acute Decompensated Heart Failure
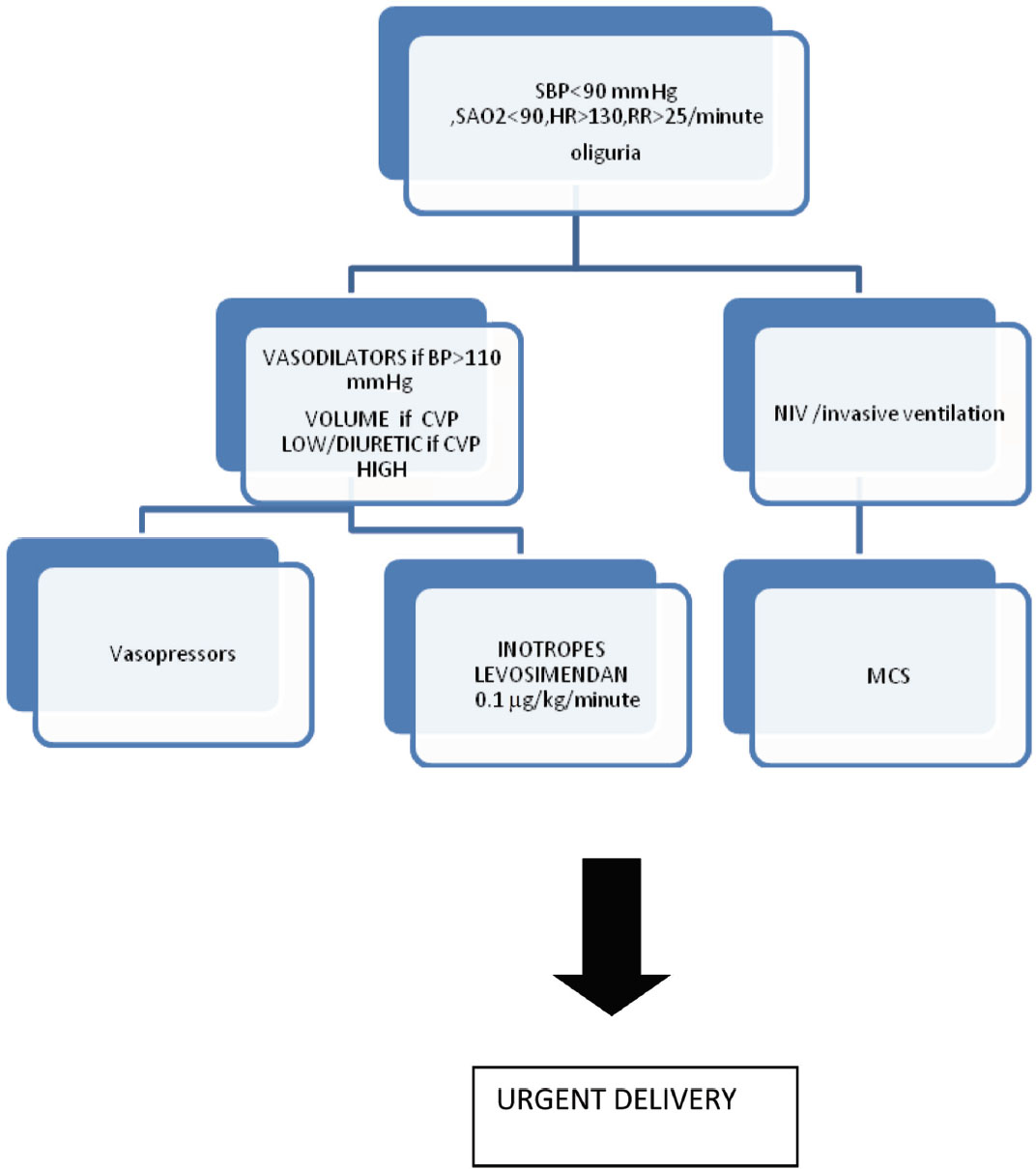
In case of ADHF with systolic blood pressure (SBP) > 110 mm Hg, vasodilators may be given.
Heart failure severity is assessed by presence of SBP < 90 mm Hg, HR > 130 or < 45 beats/min, respiratory rate (RR) > 25 breaths/min, systemic arterial saturation (SPO2) < 90%, lactate > 20 mmol/L or central venous oxygen saturation (SCVO2) < 60%, cold skin, and oliguria.
Acute decompensated heart failure patients with shock may require inotropes and mechanical circulatory support and should be shifted to a tertiary care center. Volume expansion may be required in volume depleted patients. Levosimendan may be used 0.1 µg/kg/min over 24 hours, and urgent delivery by cesarean section is advocated.
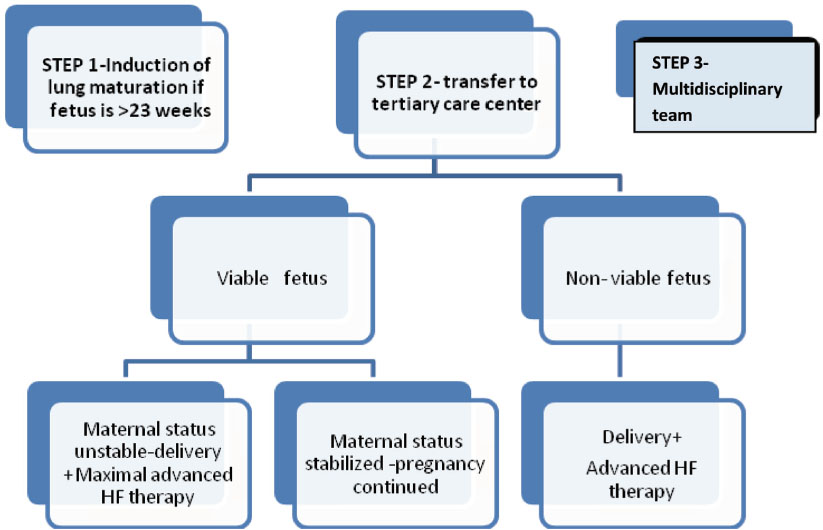
Urgent delivery is recommended in nonviable fetus. If the fetus is viable, dexamethasone is recommended for fetal lung maturity after 28 weeks, and to induce delivery in unstable patients. In stabilized patients, pregnancy may be continued with careful monitoring. (See Figs. 1, 2.)
-
Fig. 1 Algorithm for management of ADHF during pregnancy. HF, heart failure. (Adapted from ESC 2018 Guidelines on CVD during pregnancy.)
Fig. 1 Algorithm for management of ADHF during pregnancy. HF, heart failure. (Adapted from ESC 2018 Guidelines on CVD during pregnancy.)
-
Fig. 2 Management of acute heart failure during pregnancy. CVP, central venous pressure; HR, heart rate; MCS, mechanical circulatory support; NIV, noninvasive ventilation; RR, respiratory rate; SBP, systolic blood pressure; SAO2, systemic arterial saturation. (Adapted from ESC 2018 Guidelines on CVD during pregnancy.)
Fig. 2 Management of acute heart failure during pregnancy. CVP, central venous pressure; HR, heart rate; MCS, mechanical circulatory support; NIV, noninvasive ventilation; RR, respiratory rate; SBP, systolic blood pressure; SAO2, systemic arterial saturation. (Adapted from ESC 2018 Guidelines on CVD during pregnancy.)
Management during Labor
The timing of delivery should be before 40 weeks of pregnancy to avoid risk of still birth by 50% and emergency cesarean section by 12%. Labor induction can be done by misoprostol or dinoprostone. Vaginal delivery is generally preferred because of less blood loss, less risk of infection, and thromboembolism. Cesarean section is advised for ADHF, labor on oral anticoagulants, aortic pathology, severe pulmonary hypertension, or obstetric reasons.5
Oxytocin can be used to reduce postpartum hemorrhage, but ergometrine and prostaglandin F analogues should not be used.
At the time of labor, there is a sudden increase in cardiac output and SVR due to removal of placenta and uterine contractions resulting in emptying of blood into the systemic circulation, which can result in ADHF. Intravenous diuretics may be of benefit to manage the fluid overload state.
Prognosis
Heart diseases are associated with increased maternal mortality and precipitation of HF. AF occurs in about 10% of RHD patients. The maternal mortality was 1.95% in the REMEDY study. There is a substantial increase in prematurity about 20 to 30%, intrauterine growth retardation 5 to 20%, and fetal death in about 5%.12
Conclusion
Preconception counseling and preparation and correction of cardiac diseases that require percutaneous or surgical intervention and optimization of heart disease management and avoidance of teratogens before pregnancy will help patients go through the pregnancy without complications. In situations in which there is a very high risk of pregnancy such as Eisenmenger’s syndrome, severe pulmonary hypertension and severe residual left ventricular dysfunction in PPCM, future pregnancies should be avoided. Tissue valve option should be discussed in patients requiring valve replacement surgery. Patients with cardiac disease should be risk-stratified, and high-risk patients require a multidisciplinary approach involving the cardiologist, obstetrician, and anesthetist working together. Delivery can be vaginal in uncomplicated cases, and cesarean section should be reserved for complications due to obstetric reasons and in patients with decompensated HF.
References
- NT-proBNP is increased in healthy pregnancies compared to non-pregnant controls. Acta Obstet Gynecol Scand. 2009;88(02):234-237.
- [Google Scholar]
- Rheumatic heart disease in pregnancy: global challenges and clear opportunities. Circulation. 2018;137(08):817-819.
- [Google Scholar]
- Characteristics, complications, and gaps in evidence-based interventions in rheumatic heart disease: the Global Rheumatic Heart Disease Registry (the REMEDY study) Eur Heart J. 2015;36(18):1115-22a.
- [Google Scholar]
- 2018 ESC guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J. 2018;00:1-83.
- [Google Scholar]
- Rheumatic heart disease in pregnancy: strategies and lessons learnt implementing a population-based study in Australia. Int Health. 2018;10(06):480-489.
- [Google Scholar]
- Management of mitral valve stenosis during pregnancy center. About 83 cases at the Oran university hospital. Ann Cardiol Angaol. 2018;67(04):274-279.
- [Google Scholar]
- Reducing late maternal death due to cardiovascular disease—a pragmatic pilot study. Int J Cardiol. 2018;272:70-76.
- [Google Scholar]
- Pregnancy in women with heart disease in sub-Saharan Africa. Arch Cardiovasc Dis. 2011;104:370-374. 6-7
- [Google Scholar]
- Pregnancy outcomes in women with dilated cardiomyopathy. J Am Coll Cardiol. 2010;55:45-52.
- [Google Scholar]
- Global, regional, and national burden of rheumatic heart disease, 1990–2015. N Engl J Med. 2017;377(08):713-722.
- [Google Scholar]
- Pregnancy outcomes in women with rheumatic mitral valve disease. Results from the registry of pregnancy and cardiac disease. Circulation. 2018;137(08):806-816.
- [Google Scholar]







