Translate this page into:
Screening of Cardiac Rhythm Disorders in Women Working at Information Technology Sector Using Continuous Ambulatory Wireless Cardiac Monitoring – A Community-Based Study
*Corresponding author: Sudha Bala, Department of Community Medicine, ESIC Medical College, Hyderabad, Telangana, India. dr.sudhabala78@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bala S, Agarwal S, Bandaru RK, Mirza MA, Kampally M, Animalla V, et al. Screening of cardiac rhythm disorders in women working at information technology sector using continuous ambulatory wireless cardiac monitoring – A community-based study. Indian J Cardiovasc Dis Women 2023;8:11-7.
Abstract
Objectives:
The role of screening cardiac arrhythmias provides continuum of care to rediscover the causes and prevention strategies. This study was taken up to screen women working in the information and technology sector for cardiac rhythm disorders using continuous ambulatory cardiac monitoring and asses various risk factors along with work-related stress.
Materials and Methods:
A cross-sectional study was taken up at the workplace to screen women for cardiac rhythm disorders using wireless continuous ambulatory cardiac monitoring. Various risk factors and work-related stress were assessed using a standardized questionnaire. Differences in ECG parameters such as heart rate, heart rate variability (HRV), and frequency corrected QT (QTc) were compared on working and non-working days.
Results:
A total of 109 women were screened to find a proportion of 4.58% having cardiac arrhythmias. We found two cases of second-degree AV block (type 1), two cases of atrial tachycardia in the age group of 21–30 years, and one case of sinus pauses. Risk factors such as alcohol usage were statistically associated with cardiac arrhythmias. Others included a sedentary lifestyle, being underweight, a lesser number of sleep hours, no physical activity, work-related stress, and the presence of past-COVID-19 infection, but these were not statistically significant. There were significant changes in heart rate, HRV, and QTc prolongation on working day compared to non-working days. Among the domains of work-related stress, the influence at work and perceived stress due to individual demands and commitments contributed the highest mean score. Moreover, those with higher work-related stress scores were at 3.66 times the increased risk of QTc prolongation.
Conclusion:
The present study implies the combination of the need for the screening tool in younger age groups and lifestyle factors with more elucidation of work-related stress on autonomic cardiac function.
Keywords
Cardiac rhythm disorders
Work-related stress
Corrected QT prolongation
ECG parameters
Lifestyle
ABSTRACT IMAGE

INTRODUCTION
Technological development has brought out the epidemiological transition and with this, we also bring up a new trend of women working in different sectors. This exposes women to increased work stress both at home and at the workplace, leading to an increased risk of cardiac rhythm disorders which are significantly silent killers.
The mechanism linking stress to this development and exacerbation is not fully understood. There are complex connections between the autonomic nervous system and the hypothalamic-pituitary-adrenal axis that may be involved with an immediate effect on heart rate by the sympathetic and parasympathetic nerves’ intrinsic activity on the sinoatrial node resulting in increasing, and the second in decreasing heart rate.[1-3] Furthermore, the activation of the sympathetic nervous system promotes the release of catecholamines which bring heart rate variability (HRV). The autonomic nervous system control of cardiac function also might play a specific role; therefore, monitoring the QT interval in the electrocardiogram can highlight an autonomic imbalance induced by occupational stressors.[4,5]
In today’s world to screen these parameters, there has been a paradigm shift toward non-invasive devices-ambulatory continuous monitoring has the potential of capturing multiple data streams of vital physiological parameters which are easy to operate and maintain.
Keeping this in mind, an attempt has been made to take up this study with an objective to screen women working in Information and Technology for cardiac rhythm disorders using continuous ambulatory cardiac monitoring and assess various risk factors along with work-related stress.
MATERIALS AND METHODS
An observational and community-based study was taken up at Cyberabad for a 3 months duration among women working in the Information Technology sector for the past year in a particular establishment. Women aged between 21 and 58 years of age group were included without any comorbidities such as diabetes, thyroid problems, hypertension, and coronary diseases.
Exclusion criteria
Those who are pregnant and lactating women, anemia, who are on hormonal replacement therapy, oral contraceptives, and drugs causing changes in QR interval were excluded from the study.
Sample size
n = 1+2c(SD/d)2 reference by Sharma et al.;[6] n = sample size, d = difference in means of two groups = 12 (assumed), c = commonest value 7.85, s = common SD = 30 (assumed) n = 1+2×7.85(30/12)2 = 99.12 with non-response rate of 10%; n = 109.
Methodology in detail
All the women fulfilling the criteria were assessed for sociodemographic variables, body mass index, lifestyle, physical activity, food timings, sleeping hours, water intake, alcohol/smoking intake, and work stress questionnaire. ECG was recorded on working days and non-working days for a total of 48 h using multi-vital monitoring (MVM) wireless machine.
The health-care MVM system comes with smart, portable, rechargeable, and reusable devices that measure multiple vitals in real-time using the software. The MVM model consists of three components: (1) a wearable sensor collecting the data on physiological parameters; (2) a network and communications interface that enables the transfer of these data to a remote monitoring station such as a nurse or physician’s terminal or a smartphone; and (3) a remote cloud analytics platform that enables integration of large volumes of data, extracts useful information, identifies key patterns and parameters critical for patient’s health. [Figure 1] represents the workflow. Historic graphs were used to accurately determine the patient’s clinical conditions over a period of time. Validation of this particular device has been conducted at our institute among healthy volunteers.[7]

- Schematic representation of work flow.
Operational definitions
Bradyarrhythmia – heart rate <40 for >30 s in a day, second degree AV block, complete heart block, wide QRST(Heart rate >100 for 30 s), atrial fibrillation, atrial tachycardia, ectopic >10% of the total burden, non-sustained ventricular tachycardia, and sinus pause were considered clinically significant. Other subtypes as clinically non-significant and regular sinus rhythm are normal.[8]
The work stress questionnaire was developed by Frantz and Holmgren[9] which is a self-administered questionnaire with the purpose of early identification of individuals at risk of being sick-listed due to work-related stress. This consisted of 21 questions with five domains related to indistinct organization, conflicts, perceived stress due to individual demands and commitments, influence at work, and work to leisure time interference pointed on 1–4 Likert scale scoring. The higher the score the higher the stress perceived. This makes it convenient for the field set up to administer easily.
Prior permission from human resource managers was obtained from the information and technology (IT) centers, the Institutional Ethical Committee permission was obtained and the protocol was approved with the number ESICMC/ SNR/IEC-F493/09-2022. Informed consent was taken individually on the hard copies and preserved with the principal investigators.
Data analysis
Data were entered in Microsoft Excel 2020 and analyzed. Descriptive statistics were described in frequency, mean, and standard deviation. A Chi-squared test was performed to test the statistical significance of the presence of arrhythmia for the various risk factors (P < 0.05). Analysis of variance was calculated for the domains of the work stress questionnaire. A comparison of ECG parameters such as heart rate, HRV, and corrected QT (QTc) on working day and non-working day using paired t-tests was done. (P < 0.05) Risk estimate with odds ratio was included for QTc prolongation and abnormal work stress score.
On the reliability analysis test, Cronbach’s alpha was found with subscales as 0.757 value which is validated and acceptable to be used in our set up which is a measure of internal consistency that refers to the degree of interrelatedness among the items.
RESULTS
We approached 150 women working in the IT Sector of Cyberabad from three centers, out of which 30 have removed the device after onboarding for the inconvenience, 15 removed due to their myths associated in spite of briefing them about the device with the fear of stealing their data from phones as it was app-based, one of their device patches got loosened. Hence, total of 109 women were screened with wireless continuous ambulatory cardiac monitoring.
The mean age of our study subjects was 30.53 + 8.542 years and the highest number of cardiac rhythm disorders were observed in the age group of 21–30 years [Figure 2]; highest educational status was found among 3 (2.7%) with a doctorate, Master’s degree 30 (27.5%), and Bachelor’s degree 76 (69.8%).
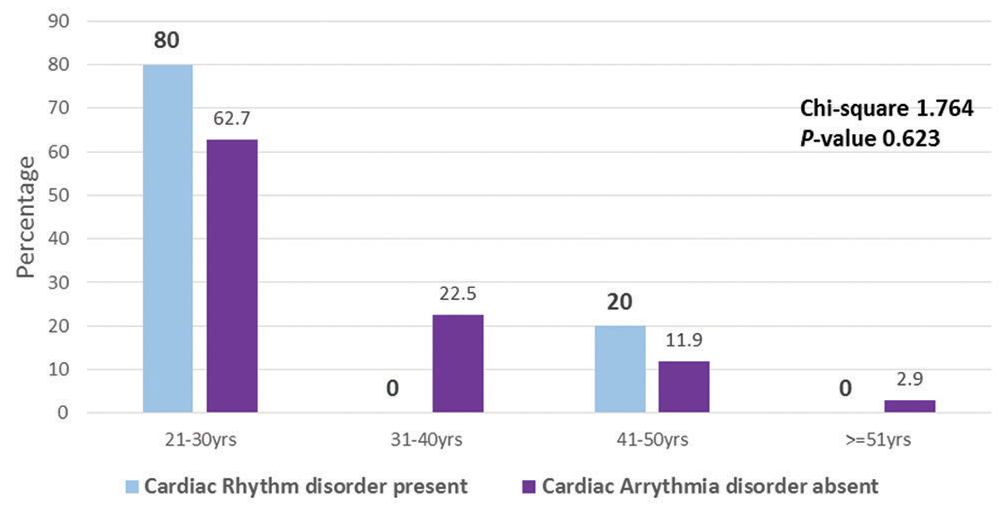
- Age group distribution of cardiac rhythm disorders.
Our study found five cases contributing to 4.58% of significant cardiac rhythm disorders. This consists of two cases of second-degree atrioventricular block (Type 1), two cases of atrial tachycardia, and one case of sinus pauses (two episodes). Second-degree AV block and atrial tachycardia cases were found in the age group of 21–30 years and sinus pauses were in the age group of 41–50 years. There were 11 cases of premature ventricular complexes, supraventricular premature complex couplets-4, and supraventricular premature complex-16 cases, but as the total burden was <10% in 24 h, it was considered insignificant. [Figures 3-5] depicts the ECG changes of the cardiac rhythm disorders.

- ECG graph with second degree AV block (Type 1).

- ECG graph with atrial tachycardia.

- ECG graph with sinus pause.
[Table 1] illustrates the various risk factors in association with cardiac rhythm disorders. Sedentary lifestyle, <7 h sleep, underweight, and past-COVID-19 infection were found to be higher among those with arrhythmic disorders compared to those without but, however, there was no statistical significance. Alcohol usage was found to be associated statistically among arrhythmic disorder subjects (P < 0.05). Tobacco usage was not found among the study subjects.
| Variables | Cardiac arrhythmia Present (n=5) (%) | Cardiac arrhythmia Absent (n=104) (%) | Chi-square | P-value |
|---|---|---|---|---|
| Lifestyle | ||||
| Sedentary | 3 (60) | 70 (67) | 0.525 | 0.913 |
| Moderate | 2 (40) | 30 (29) | ||
| Heavy | 0 (0) | 4 (4) | ||
| Alcohol usage | ||||
| Yes | 4 (80) | 10 (9) | 21.338 | 0.0001 * |
| No | 1 (20) | 94 (91) | ||
| Sleep hours | ||||
| <7 h | 3 (60) | 37 (35) | 1.225 | 0.354 |
| >7 h | 2 (40) | 67 (65) | ||
| Physical activity | ||||
| Yes | 2 (40) | 33 (32) | 0.150 | 0.517 |
| No | 3 (60) | 71 (68) | ||
| Body mass index (WHO Asian BMI Classification) | ||||
| Underweight | 2 (40) | 17 (17) | 2.342 | 0.505 |
| Normal weight | 1 (20) | 25 (26) | ||
| Overweight | 0 (0) | 19 (20) | ||
| Obese | 2 (20) | 36 (37) | ||
| COVID-19 infection in the past | ||||
| Yes | 3 (60) | 28 (27) | 0.442 | 0.802 |
| No | 2 (40) | 76 (73) |
Histogram showing the mean range of distribution of work-related stress [Figure 6]. On ANOVA, the highest scores were found to influence work and perceived stress due to individual demands and commitment domains among those with cardiac arrhythmia disorder. However, there was no statistically significant association between total stress score with their subgroup domains and the occurrence of arrhythmia [Table 2].
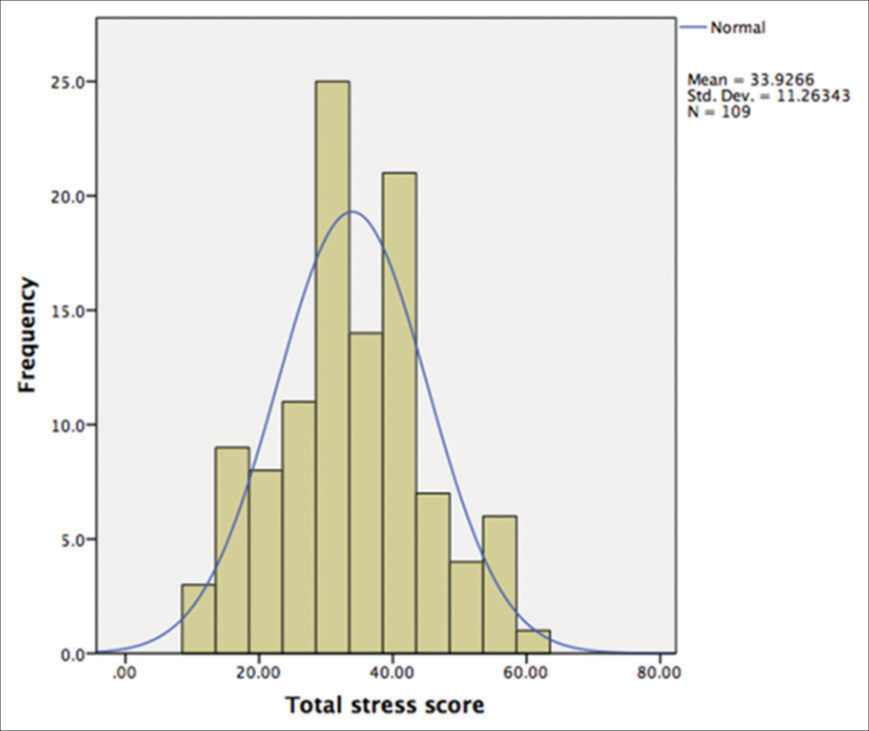
- Distribution of work-related stress among study subjects.
| Domains of work stress questionnaire | Mean±SD | P-value |
|---|---|---|
| Influence at work | ||
| Cardiac arrhythmia – Present | 7.40±1.140 | 0.603 |
| Cardiac arrhythmia – Absent | 6.83±2.310 | |
| Indistinct organization | ||
| Cardiac arrhythmia – Present | 4.70±3.189 | 0.087 |
| Cardiac arrhythmia – Absent | 2.20±2.489 | |
| Conflicts | ||
| Cardiac arrhythmia – Present | 2.80±3.701 | 0.881 |
| Cardiac arrhythmia – Absent | 2.59±2.944 | |
| Perceived stress due to individual demands and commitment | ||
| Cardiac arrhythmia – Present | 5.29±1.219 | 0.175 |
| Cardiac arrhythmia – Absent | 4.87±2.180 | |
| Work to leisure time interference | ||
| Cardiac arrhythmia – Present | 2.77±0.271 | 0.947 |
| Cardiac arrhythmia – Absent | 2.77+1.240 | |
| Total Stress score | ||
| Cardiac arrhythmia – Present | 34.15±11.247 | 0.930 |
| Cardiac arrhythmia – Absent | 29.2±11.777 | |
On application of paired t-test, there was a statistically significant change in the maximum and minimum heart rates on working and non-working day among the study subjects with higher values on a working day. Mean values of QTc interval and HRV were also statistically significant on working and non-working days [Table 3].
| ECG Parameters | Working day | Non-working day | P-value |
|---|---|---|---|
| Maximum heart rate | 147.38±15.068 | 136.74±17.894 | 0.00001 |
| Minimum heart rate | 60.38±9.818 | 58.45±9.327 | 0.00002 |
| QTc | 450.14±17.08 | 430.12±10.04 | 0.0000001 |
| HRV | 701.16±43.39 | 730.4±52.42 | 0.049 |
Risk estimate analysis has depicted that those with higher work stress scores had 3.66 times of having QTc prolongation in the ECG. QTc values of >460 ms for women were considered prolonged [Table 4]. Grading of the work stress score was obtained after calculating the median which was 33, anything above 33 was considered high.
| Parameter | QTc Normal (n=94) | QTc Prolonged (n=15) | Odds ratio (CI) | Chi-square and P value |
|---|---|---|---|---|
| Total stress score | ||||
| Low (0–33) | 54 (57%) | 4 (26%) | 3.669 (1.117–10.19) | 3.764 (0.03) |
| High (>33) | 40 (43%) | 11 (74%) |
QTc: Corrected QT
DISCUSSION
The study comprised 109 women employees working in three establishments in the IT hub of Hyderabad. The sample predominately had employees of the age group 21–30 years which made up 64% of the total sample size. The majority of the participants were not native dwellers of the city and had migrated from different parts of India to work in the study settings. Incidental findings of significant rhythm disorders, two cases of second-degree AV block, two cases of Atrial tachycardia, and one case of sinus pause, in otherwise apparent non-symptomatic patients, have raised questions on the hidden cases of cardiac rhythm disorders in a population under study.
Lifestyle conditions and heart health are related proportionally. A good lifestyle involving healthy eating habits and exercise has a positive effect on heart health thus causing less cardiac morbidity.[10,11] Alcohol usage, sedentary lifestyle, less sleep, and lower physical activity showed significant association with changes in rhythm conditions.
Bukata et al., conducted study among Ethiopians and found significant cardiac arrhythmia’s among 34.2% of participants. Among these ,conduction abnormalities and sinus bradycardia were the commonest findings (25.4%) followed by Premature beats (ventricular 1.9%, atrial 1.1%) and atrioventricular nodal reentrant tachycardia (2.1%). The risk factors which were independently associated were smoking, hypertension, heart failure, prior stroke, previous history of MI, vigorous intensity activities, solidified vegetable oil consumption, and occupation (pensioner, none).[12] This variation of the higher proportion is explained by the inclusion of the already known cases of cardiac arrhythmia and this was not a continuous cardiac monitoring method.
Similar to our study, Lee et al. also demonstrated the increased risk of rhythm disorders, particularly atrial fibrillation in people dwelling in unhealthy lifestyle factors, involving alcohol consumption, less frequent physical activity, and smoking.[11]
Novel factor including past-COVID-19 infection of greater than 6 months duration in the present study subjects illustrated slightly higher proportion of cardiac arrhythmia but was not statistically significant. Contrary findings by Dewland et al. in their prospective arrhythmia surveillance using Holter cardiac monitoring for a median period of 13.2 days found that none of the participants had significant arrhythmia after COVID-19 infection for the past 34–126 days. Nearly 96% had ectopic burden of <1% and majority had experienced palpitations which was mostly of sinus rhythm.[13] Pranata et al., in their systematic review and meta-analysis of 4 studies including 784 patients, uncovered the incidence of arrhythmia in patients with COVID-19 as 19% and with fatal outcome of 48%.[14] It is too early to comment on this aspect as we need more studies to support the proarrhythmic effect of COVID-19 infection.
The study demonstrated that there is a significant change in heart rhythm patterns on working days in comparison to non-working days. The changes were seen in heart rate, HRV, and QT changes. Telman et al. study demonstrated the reduced HRV on days of mental stress,[15] which was also demonstrated in the current study, where HRV showed significant changes on non-working and working days. Work-related stress has shown an association with cardiovascular disease (CVD) and in the population, where clinical CVD is not established, QTc can be a great indicator of the risk estimate.[10,11] Bhide et al. in their study to evaluate electrophysiological changes during acute stress among healthy male volunteers of the 18–24 years age group reported higher heart rate and prolonged QTc interval. This can be explained by increased sympathetic activity induced by stress and also inhomogeneity of repolarization, thereby inducing prolongation of QTc interval.[16]
The present study showed that with higher scores on the stress scale, there are 3.66 times of risk of QT prolongation. Stress precepted by psychosocial reasons adversely affects autonomic homeostasis and, in turn, can trigger various ventricular arrhythmias.[17] The study investigated the impact of psychosocial factors like work-related relocation, and work-leisure balance on any changes to the rhythm, and could not show any statistically significant association. However, on the stress scale, it was seen that the stress perceived by the working women and various influences at work did have an increased risk of developing rhythm changes. A study conducted on Indian working women showed that working Indian women are more stressed than their counterparts, mainly due to the societal structure where still household chores, and taking care of the child are still “women’s jobs,” irrespective of their working status.[18] Limitations of the study include the smaller proportion, generalization of results cannot be done and there was no comparison group.
CONCLUSION
In spite of certain limitations, the present study depicts cardiac rhythm disorders in association with modifiable risk factors. Significant changes in ECG parameters such as heart rate, HRV, and QTc prolongation on a working day. Those with higher work stress scores had been reported with QTc prolongation implying that work-related stress contributes to physiological dysregulation of the autonomic nervous system, leading to an increased risk of cardiac rhythm disorders. These findings necessitate the need for screening tools with easy to wear and operate for continuous cardiac monitoring to ensure early diagnosis of cardiac rhythm disorders. Thereby, targets of intervention to modify the lifestyle in younger age group of 21–30 years are the utmost need. Following the healthy sleep pattern, an active lifestyle, avoidance of regular alcohol usage, reducing the work stress by regular practice of pranayama and yoga, and self-reflection to be practiced to organize the work schedule are the recommendations arising from the present study. Further, community-based studies on larger sample are required to establish the biological plausibility.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- The relationship of autonomic imbalance, heart rate variability and cardiovascular disease risk factors. Int J Cardiol. 2010;141:122-31.
- [CrossRef] [PubMed] [Google Scholar]
- Claude Bernard and the heart-brain connection: Further elaboration of a model of neurovisceral integration. Neurosci Biobehav Rev. 2009;33:81-8.
- [CrossRef] [PubMed] [Google Scholar]
- Prolonged job strain reduces time-domain heart rate variability on both working and resting days among cardiovascular-susceptible nurses. Int J Occup Med Environ Health. 2014;28:42-51.
- [CrossRef] [PubMed] [Google Scholar]
- Psychophysiological biomarkers of workplace stressors. Neurosci Biobehav Rev. 2010;35:51-7.
- [CrossRef] [PubMed] [Google Scholar]
- How to calculate sample size for observational and experimental nursing research studies? Natl J Physiol Pharm Pharmacol. 2020;10:1-8.
- [CrossRef] [Google Scholar]
- Remote multi vital monitoring of decentralized trial participants using artificial intelligence technology based solution In: Manohar K, Bheerappa N, Radhika M, eds. ISRPTCon 2022 Proceedings of 14th Annual Conference of Indian Society for Rational Pharmacotherapeutics. Hyderabad. Telangana, India: Hetero; 2022. p. :67.
- [Google Scholar]
- The Work Stress Questionnaire (WSQ)-reliability and face validity among male workers. BMC Public Health. 2019;19:1580.
- [CrossRef] [PubMed] [Google Scholar]
- Association between work-related stress and QT prolongation in male workers. Int J Environ Res Public Health. 2019;16:4781.
- [CrossRef] [PubMed] [Google Scholar]
- Association between clustering of unhealthy lifestyle factors and risk of new-onset atrial fibrillation: A nationwide population-based study. Sci Rep. 2020;10:19224.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and determinants of cardiac arrhythmias and conduction anomalies in adults aged = 40 years in Jimma Town, Southwest of Ethiopia: A cross-sectional study. Afr Health Sci. 2022;22:210-9.
- [CrossRef] [PubMed] [Google Scholar]
- Prospective arrhythmia surveillance after a COVID-19diagnosis. Open Heart. 2022;9:e001758.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence and impact of cardiac arrhythmias in coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis. Indian Pacing Electrophysiol J. 2020;20:193-8.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of mental stress on heart rate and heart rate variability In: Katholeika Universiteit Leuven, editors. Proceedings of 4th ECIFMBE. Berlin, Heidelberg: Springer-Verlag; 2009. p. :1366-9.
- [CrossRef] [Google Scholar]
- Electrocardiographic changes during acute mental stress. Int J Med Sci Public Health. 2016;5:835-8.
- [CrossRef] [Google Scholar]
- Behavioral cardiology: Recognizing and addressing the profound impact of psychosocial stress on cardiovascular health. Curr Atheroscler Rep. 2006;8:111-8.
- [CrossRef] [PubMed] [Google Scholar]
- A study on psychological stress of working women. Int J Multidiscip Res. 2012;2:434-45.
- [Google Scholar]








