Translate this page into:
Thrombosed Abdominal Aortic Aneurysm in a Young Female
Sheshidhar Madaka Nizam's Institute of Medical Sciences, Hyderabad Telangana, 500082 India sheshidharmadaka@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
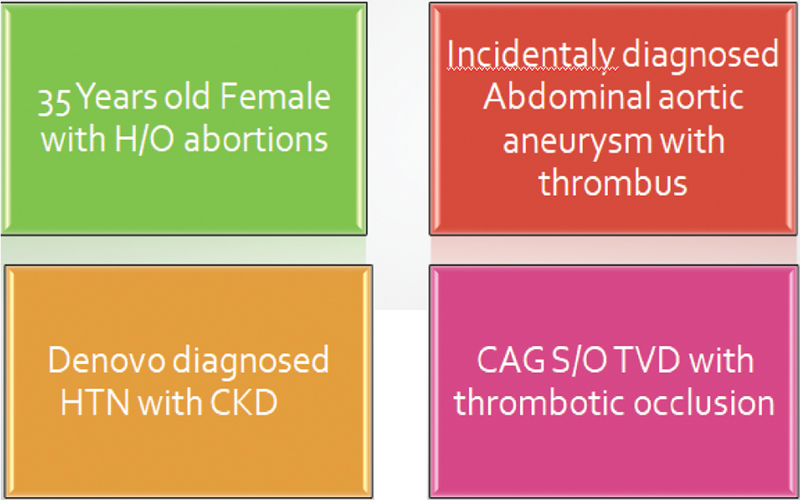
Presenter: A 35-year-old female, with the following chief complaints:
-
Shortness of breath (SOB) since 7 days and chest pain since 4 days.
-
Patient was apparently asymptomatic 7 days back; thereafter, she developed SOB, which was sudden onset, and New York Heart Association functional class (NYHA FC) III, which progressed to FC IV over the next 2 days and was also associated with orthopnea. Patient had no history of paroxysmal nocturnal dyspnea (PND) episodes.
-
Chest pain—one episode 4 days back, sudden onset, retrosternal, squeezing type, associated with sweating, continued for 30 minutes, and was relieved with medication.
-
Patient did not have any history of palpitations, syncope, bilateral swelling of legs, reduced urine output, facial puffiness, fever, cough, abdominal pain or distension, vomiting, diarrhea, back pain, skin rash, weight loss, easy fatigability, joint pain, ulcerations in the body, and history suggestive of rheumatic disease in past.
-
Obstetric history: She had a past history of four spontaneous abortions as well as a history of surgery for ovarian cyst (8 years back). She conceived with in vitro fertilization (IVF) but spontaneously aborted.
-
Patient had no similar complaints in the past. She is a homemaker. Patient takes mixed diet. She is not a known smoker, alcoholic, or tobacco chewer. Patient is not using any other medication. Family history was not suggestive of any cardiac disease or other medical illnesses in her family.
Discussant: To summarize the clinical details, a 35-year-old female presented with sudden onset of dyspnea since 7 days, progressed from class III to IV in 2 days, one episode of chest pain 4 days back, and past history of abortions. Based on clinical presentation, the differential diagnoses included the following:
-
Antiphospholipid antibodies (APLA) syndrome: These patients presented with vascular thrombotic events in the form of deep vein thrombosis (DVT), acute pulmonary thromboembolism, acute coronary syndrome (ACS) due to thrombotic occlusion of coronaries, and recurrent abortions; hence, the possibility of APLA syndrome can be considered as first possible diagnosis.1
-
Systemic lupus erythematosus (SLE): SLE patients presented with fever, joint pains, myalgias, skin rashes, cardiac involvement in the form of pericarditis and myocarditis. So, these patients can present as SOB and chest pain; however, no prodromal symptoms were seen in the patient.
-
ACS: Patients diagnosed with ACS manifest with chest pain and dyspnea if the patient developed left ventricular (LV) dysfunction, and they were also predisposed to develop arrhythmias. In our patient, coronary artery disease (CAD) can be considered.2
-
Dilated cardiomyopathy (DCMP): Patients diagnosed with DCMP usually manifest with SOB, which is usually insidious in onset and gradually progressive, and atypical chest pain. Patients diagnosed with DCMP will usually have long duration of symptoms; however present patient had breathlessness of only 7 days duration.
-
Viral myocarditis: Patients diagnosed with viral myocarditis usually have SOB, which is sudden in onset and includes chest pain. Hence, in this patient, there is high possibility of viral myocarditis. However, this patient did not elicit any inciting event.
-
Hypertrophic cardiomyopathy (HCM): Patients diagnosed with HCM usually develop symptoms by the 3rd and 4th decade.3 HCM patients present with chest pain, syncope, palpitations, and SOB.4 HCM patients present as dilated cardiomyopathy in the late burnt-out stages. About 60% patients usually have a positive family history of cardiomyopathy.5 In the present case, family history was absent, and patient had sudden onset of symptoms.
-
Infiltrative cardiomyopathy: Patients diagnosed with infiltrative cardiomyopathy usually present with SOB and chest pain after 6th decade. Infiltrative cardiomyopathy usually manifest as a component of multisystem disorder.6 In our present patient, there were no clinical manifestations related to other systems.
-
Calcific degeneration of bicuspid aortic valve: Patients with significant aortic stenosis (AS) due to calcific degeneration of bicuspid aortic valve present with angina, syncope, and SOB.7 These patients have a slightly longer history of symptoms. Our patient had sudden onset of SOB and chest pain and no history of syncope and palpitations.
Presenter: On general physical examination, patient was conscious, coherent, and oriented. Her body mass index (BMI) was 23 kg/m2 and temperature 98.4 °F. Pulse rate was 120 beats/min, and regular blood pressure was 190/100 mm Hg in right arm supine position and 200/100 in right lower limb. Respiratory rate was 34 cycles per minute and oxygen saturation was 99% on room air. Pallor was present, and there were no signs of icterus, cyanosis, clubbing, edema feet or lymphadenopathy. On cardiovascular (CVS) examination, jugular venous pressure (JVP) had normal mean column height and normal wave pattern. Apex beat was localized in left 5th intercostal space half inch medial to midclavicular line, LV type. First heart sound was normal in intensity. Second heart sound was normal in intensity and split. No added sounds were present. On auscultation of lungs, fine crackles were found. There was no evidence of organomegaly. No epigastric pulsations were noted on per abdomen examination. Central nervous system (CNS) examination was normal.
Discussant: Summary of the examination findings are blood pressure of 190/100 mm Hg in right arm supine position, pallor, and respiratory rate was 34 cycles per minute.
Keeping in mind history as well as examination findings, the probable differential diagnosis is:
-
Hypertensive heart failure: Presented with hypertension and cardiac involvement in the form of ischemic symptoms like chest pain and failure symptoms like SOB. Hypertensive heart disease can manifest as either systolic heart failure or diastolic failure or both. Hypertensive heart disease patients are more prone to develop acute events like decompensated heart failure, acute coronary events, or sudden cardiac death.8 Hypertension (HTN) disrupts the endothelial system, which increases the risk of CAD and peripheral arterial disease (PAD) and thus represents a significant risk factor for the development of atherosclerotic disease.
-
APLA syndrome: is an autoimmune disorder present as recurrent abortions and thromboembolic events like DVT, acute pulmonary thromboembolism and ACS. This patient has history of abortions, and acute coronary symptoms can be considered as initial differential diagnosis.
-
Autoimmune overlap syndromes: About 25 to 45 percent cases of APLA are associated with SLE. This can manifest as hypertension due to lupus nephritis, recurrent abortions and thrombotic events such as ACS, pallor due to hemolytic anemia, but other manifestations like skin involvement are absent in this case.
-
Early atherosclerosis: Early atherosclerosis can manifest as hypertension and acute coronary events. High blood pressure on its own increases atherosclerosis risk by 60 percent. Early atherosclerosis of renal and coronary vessels present as HTN and HTN-induced chronic kidney disease which manifests as anemia, renal failure and acute coronary events. Early atherosclerosis can be considered as initial diagnosis, but the female sex and age of presentation are against the atherosclerosis.9 10
-
Infiltrative cardiomyopathy: Infiltrative cardiomyopathy patients usually present with diastolic heart failure, concentric hypertrophy in initial stages, and in advanced stage, present as DCMP11 Occurrence of complete heart block and supraventricular tachyarrhythmia is high due to infiltration of conduction system and atrial dilatation. The typical features are absent in the present case.
-
Hypertensive HCM: Hypertension of mild-to-moderate degree sometimes occurs in patients with HCM, but it is predominant among the elderly. Early age of presentation in our case and anemia usually rules out this condition.12
Investigations
-
Chest X-ray
-
ECG
-
2D ECHO
-
Laboratory investigations (Table 1)
-
Others
|
Parameters |
Patient values |
|---|---|
|
Hb |
7.3 |
|
TLC |
7300 |
|
Platelets |
2.8 |
|
ESR |
140 |
|
Na/K |
134/ 4.4 |
|
Crt/BUL |
6/168 |
|
Bil T/D |
0.2/0.1 |
|
SGOT/PT |
13/11 |
|
T prot/alb |
7.1/3.9 |
|
LDH/CPK |
789/534 |
|
NTproBNP |
17878 |
|
TC/TG/HDL/LDL |
120/185/40/73 |
|
hsCRP |
24 |
|
Ca/Mg/PO4 |
8.5/0.78/4.9 |
|
Uric acid |
9.2 |
|
Vit D/PTH |
26.48/440 |
|
CUE |
Prot 1+ |
|
Urine PCR |
1.8 |
Abbreviations: ESR, erythrocyte sedimentation rate; HDL, high-density lipoprotein; hsCRP, high-sensitivity C-reactive protein; LDH, lactate dehydrogenase; LDL, low-density lipoprotein; PCR, protein to creatinine ratio; PTH, parathyroid; TC, total cholesterol; TG, triglyceride; TLC, total leucocyte count.
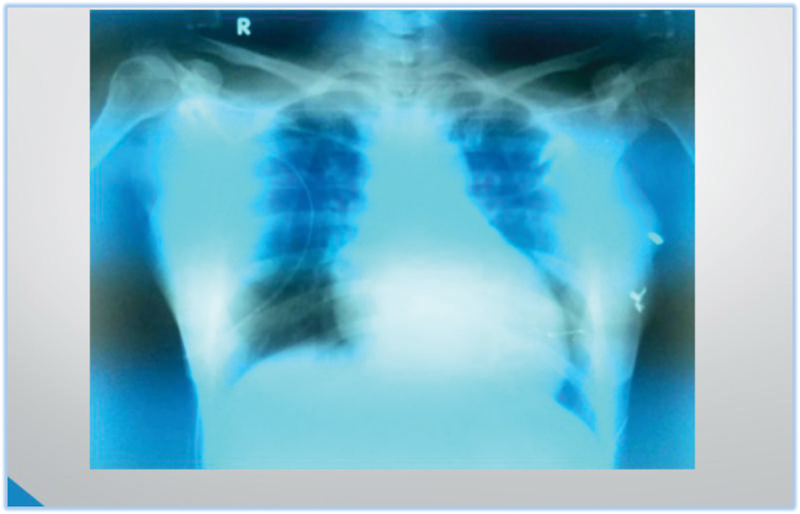
According to radiologist's opinion, in Fig. 1, chest X-ray shows normal cardiac size with normal pulmonary vascular markings. Aorta and pulmonary bay are normal. No signs of pulmonary venous hypertension.
-
Fig. 1 Chest X-ray PA view.
Fig. 1 Chest X-ray PA view.
ECG
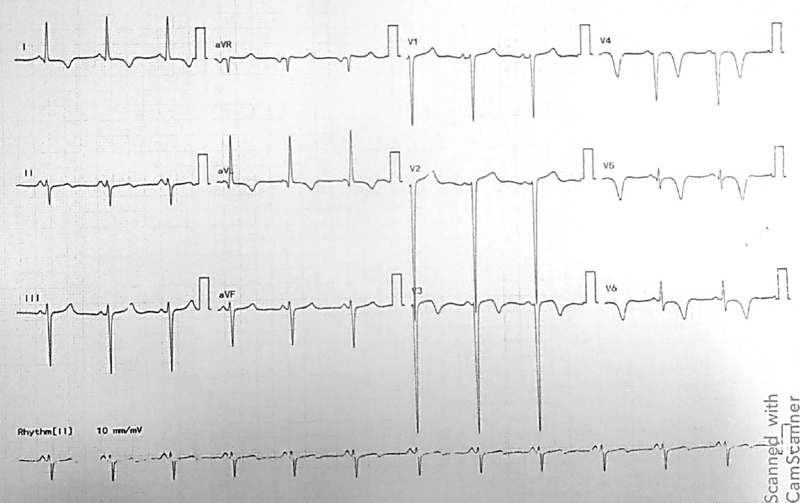
In Fig. 2, ECG on the day of hospital admission was suggestive of normal sinus rhythm (NSR) rate of 96, left axis deviation, and T-wave inversions in lead 1 aVL v3 to v6

-
Fig. 2 ECG on hospital admission.
Fig. 2 ECG on hospital admission.
In Fig. 3, ECG after 1 hour suggestive of NSR with deepening of T inversions in lead 1 aVL V3 to V6
-
Fig. 3 ECG after 1 hour on hospital admission.
Fig. 3 ECG after 1 hour on hospital admission.
ECG features suggestive of dynamic ECG changes. These features are in favor of ACS.
Discussant: In view of dynamic ECG changes, ACS is suspected, and patient is evaluated with troponin test and echocardiography.
Troponin Test: Positive
Echocardiography: normal-sized cardiac chambers, regional wall motion abnormalities (RWMA) + in distal interventricular septum (IVS), apex, mild LV dysfunction (ejection fraction [EF]: 45%), grade I diastolic dysfunction (A > E), mild mitral regurgitation (MR) (MRJA 2.1SQCM) mild tricuspid regurgitation (TR), mild pulmonary arterial hypertension (PAH) (RVSP 36), good right ventricular (RV) function (TAPSE 2.1), no clot/vegetation/pulmonary embolism (PE).
Discussant: Based on above ECG, echo changes patient had ACS non-ST-segment myocardial infarction (NSTEMI) with distal IVS and apex hypokinesia along with mild LV dysfunction.
Presenter: Patient was further evaluated with laboratory investigations (shown in Table 1)
Presenter: Above laboratory parameters (Table 1) suggest anemia with raised blood urea nitrogen (BUN) and creatinine values and increased NTproBNP and high-sensitivity C-reactive protein (hsCRP) values.
Discussant: Presence of normocytic normochromic anemia with raised renal parameters is more in favor of chronic kidney disease (CKD).
Patient was initially managed with diuretics and vasodilators. No significant improvement was found. Nephrology opinion was obtained, and hemodialysis done with blood transfusion. After stabilization, USG abdomen was done.
USG Abdomen
Radiologist opinion: showing bilateral (B/L) small kidneys, echogenicity, and loss of corticomedullary differentiation (CMD).
Right kidney: 43 × 14 mm.
Left kidney: 78 × 33 mm.
Abdominal aortic aneurysm extending from celiac axis till bifurcation. Maximum dimension is 54 × 42 mm.
There is concentric thrombus involving distal aorta with maximum thickness of 13 mm along with central lumen patent, extending into right common iliac artery (CIA).
-
High-resolution (HRCT chest): mild cardiomegaly with pulmonary edema.
No significant lung parenchymal abnormality seen.
-
COVID-19 RT-PCR: negative.
-
Presenter:
-
Patient was subjected to one more session of hemodialysis with 1 unit packed red blood cell (PRBC) transfusion and coronary angiogram (CAG) done.
-
CAG: suggestive of triple-vessel disease with thrombotic occlusion (Fig. 4)
-
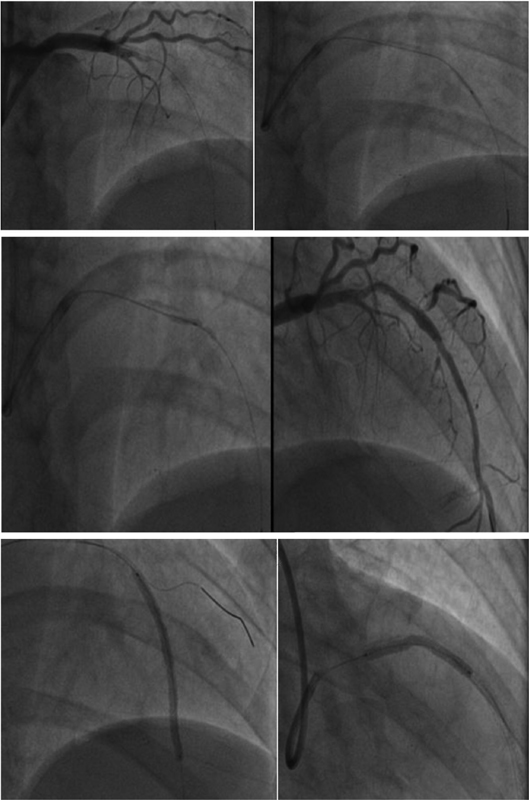
Patient managed with percutaneous coronary intervention (PCI) to left anterior descending (LAD) artery (Fig. 5).
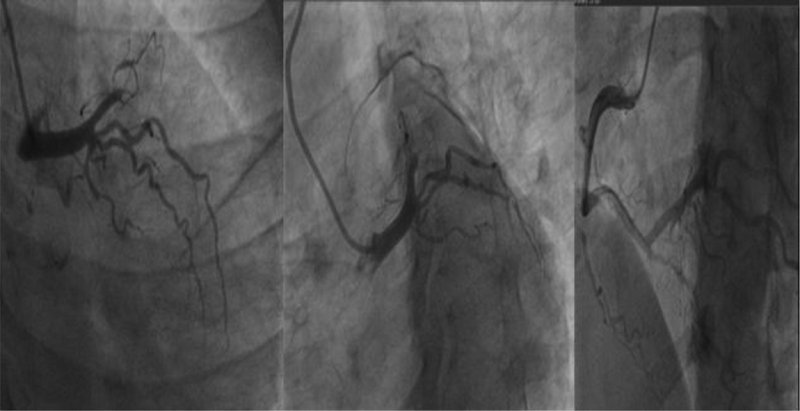
-
Fig. 4 Coronary angiogram (CAG) suggestive of triple-vessel disease.
Fig. 4 Coronary angiogram (CAG) suggestive of triple-vessel disease.
-
Fig. 5 Suggestive of percutaneous coronary intervention (PCI) to left anterior descending (LAD) artery.
Fig. 5 Suggestive of percutaneous coronary intervention (PCI) to left anterior descending (LAD) artery.
Presenter: A 35-year-old female with history of recurrent abortions, de novo HTN with CKD, triple-vessel disease with thrombotic occlusion, and abdominal aortic aneurysm with thrombus.
Discussant: Based on the above presentation, the differential diagnosis is as follows:
-
APLA.
-
Autoimmune overlap disorders.
-
Large vessel vasculitis (Takayasu arteritis).
-
Other vasculitic disorders.
-
Behcet's disease.
-
HTN-induced degenerative changes.
-
Early atherosclerosis.
Presenter: APLA and autoimmune overlap disorders are considered as first possible diagnosis to confirm the diagnosis; patient is further investigated with autoimmune profile as shown in Table 2.
|
Test |
Result |
|---|---|
|
Anticardiolipin antibodies (IgG + IgM) |
Negative |
|
β2 glycoprotein |
Negative |
|
LA |
Negative |
|
ANA |
Negative |
|
Anti dsDNA |
Negative |
|
RA factor |
Negative |
|
Anti-CCP |
Negative |
|
C3 |
Normal |
|
C4 |
Normal |
|
Test |
RESULT |
|
Nucleosomes |
Negative |
|
Histones |
Negative |
|
SmD1 |
Negative |
|
PCNA |
Negative |
|
U1-snRNP |
Negative |
|
SS-A/Ro52 |
Negative |
|
SS-A/Ro60 |
Negative |
|
SS-B/La |
Negative |
|
Scl-70 |
Negative |
|
AMA-M2 |
Negative |
|
Jo-1 |
Negative |
|
PM-Scl |
Negative |
|
Mi-2 |
Negative |
|
Ku |
Negative |
|
CENP-B |
Negative |
Abbreviations: ANA, antinuclear antibody; CL, cardiolipin, LA, lupus anticoagulant; RA, rheumatoid arthritis.
Discussant: Patient has negative rheumatoid arthritis (RA) factor, lupus antibodies, β2 glycoprotein, antinuclear antibody (ANA), ds DNA, complement factors, antihistone antibodies, U1RNP, SS-A, SS-B, Scl-70, Jo-1, Mi-2, Ku, and CENP-B antibodies.
APLA syndrome: is a disease with a myriad of clinical manifestations ranging from recurrent vascular thrombosis and pregnancy complications to valvular lesions, transverse myelitis, thrombocytopenia and hemolytic anemia. It may be primary or secondary, that is, associated with other autoimmune diseases. The latest classification criteria (Sydney 2006) recognize just three tests to define this syndrome—lupus anticoagulant (LA), anticardiolipin antibodies and anti gp 1 antibodies. In our patient, these antibodies are negative.
Autoimmune overlap syndromes: APLA, which occurs secondary to SLE or other autoimmune diseases, is called secondary antiphospholipid antibody syndrome (APS) and is characterized by arterial and venous thrombosis, recurrent miscarriages in pregnancy, and neurologic manifestations along with the presence of APLA. APLA are more prevalent in patients with SLE (∼ 50%) with LA constituting 15 to 34% and cardiolipin (CL) constituting 12 to 30%.13 In a study by Unikiene and Misiuniene, the incidence of APLA positivity was found to be 30.2% in the SLE group and 29% in the systemic sclerosis group. In our case, APLA antibodies, ds DNA, RA factor, ANA antibodies, SCL-70, SS-A, SS-B antibodies are negative.
Mixed Connective Tissue Disorder
It is a rare connective tissue disorder that is characterized by features commonly seen in three different connective tissue disorders: SLE, scleroderma, and polymyositis. Some affected people may also have symptoms of RA.14 Although mixed connective tissue disorder (MCTD) can affect people of all ages, it appears to be most common in women under age 30. Signs and symptoms vary but may include Raynaud's phenomenon, arthritis, heart, lung and skin abnormalities, kidney disease, muscle weakness, and dysfunction of the esophagus. In our case, classical manifestations are absent, and U1RNP antibodies are negative.
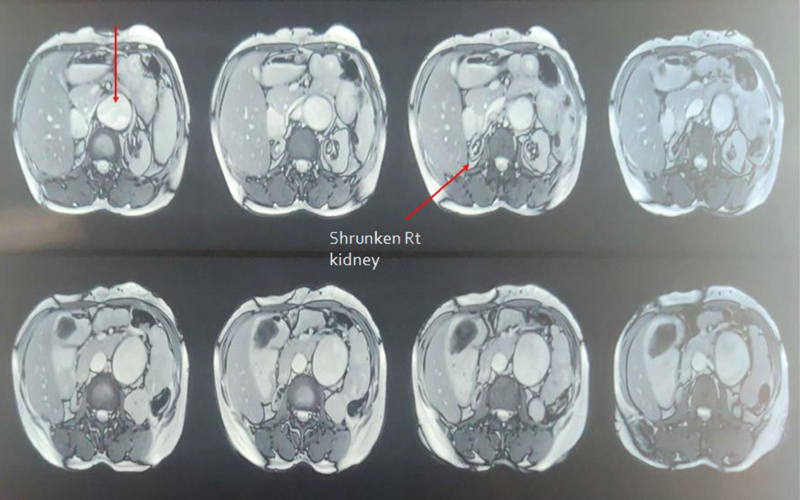
Presenter: After ruling out APLA and autoimmune overlap disorders, patient was further investigated with MR aortogram, as shown in Fig. 6.

-
Fig. 6 MR aortogram showing fusiform aneurysmal dilatation of suprarenal, renal and infr-renal (4.7 cm) segments of abdominal aorta (AA).
Fig. 6 MR aortogram showing fusiform aneurysmal dilatation of suprarenal, renal and infr-renal (4.7 cm) segments of abdominal aorta (AA).
MR AORTOGRAM
Radiologist Opinion
-
Ascending aorta, arch, and descending aorta are normal in course, caliber, and signal intensity
-
Fusiform aneurismal dilatation of suprarenal, renal and infrarenal (4.7 cm) segments of abdominal aorta (AA) extending from D12-L1 vertebrae till bifurcation, and eccentric thrombus involving right proximal CIA measuring 14 mm till periphery
-
Dilatation of right CIA with peripheral thrombus.
-
Superior mesenteric artery (SMA) arising from aneurysmal segment of AA.
-
Right RA arising from aneurysmal segment of AA, with narrowed distal portion and shrunken right kidney, as shown in Fig. 7.
-
Left RA is normal in caliber.
-
Fig. 7 MR aortogram showing shrunken right kidney.
Fig. 7 MR aortogram showing shrunken right kidney.
Presenter: Based on MRA findings, differential diagnoses considered in this case are as follows:
-
Large vessel vasculitis (Takayasu arteritis).
-
Behcet's disease.
-
HTN-induced degenerative changes.
Early Atherosclerosis
Large vessel vasculitis (Takayasu arteritis): is a rare systemic inflammatory vasculitis of large vessels with unknown etiology. It presents as granulomatous inflammation of aorta and its major branches and mainly involves carotid arteries and manifest as pulseless disease. In the acute phase of Takayasu arteritis, it results in thickening of vessel wall, mural edema and enhancement. The pulseless/occlusive phase, which results from vascular stenosis or occlusion and signs and symptoms, is dependent upon which vessels are involved. Stenosis is the most common complication of the aorta and most commonly involves the descending thoracic aorta and AA, although aortic occlusion or dilation may also occur.15 Most commonly involved vessels are subclavian arteries. Our case is not having classical features of Takayasu arteritis.
Behcet's disease: chronic relapsing remitting vasculitis affecting multiple organs present as recurrent oral ulcerations, genital ulcerations, uveitis, erythema nodosum vasculitis features like aneurysm, and positive pathergy test.16 In our case, classical manifestations are absent.
Presenter: After ruling out Takayasu arteritis and Behcet's disease, to differentiate HTN-induced degenerative changes and early atherosclerosis, patient was further probed with the following investigations, as shown in Table 3.
|
Test |
Result (normal range) |
|---|---|
|
Lp (a) |
72 (< 30) |
|
Homocysteine |
53.52 (< 15) |
|
Fibrinogen |
720 (200–400) |
|
hsCRP |
24 |
Abbreviation: hsCRP, high-sensitivity C-reactive protein.
Discussant: Patient has increased values of lipoprotein a, homocysteine, fibrinogen, and hsCRP.
HTM-induced degenerative changes: Abdominal aortic aneurysms (AAA) are fatal in 80% of the cases when ruptured. AAA in hypertensive versus nonhypertensive adult patients showed, overall, a 66% increased risk of developing the disease in hypertensive patients.17 HTN has been considered a potential risk factor for AAA; furthermore, a 20 mm Hg increase in systolic blood pressure (SBP) and a 10 mm Hg increase in diastolic blood pressure (DBP) were associated with a 14% and 28% increase in the risk of developing AAA, respectively. In our case, patient had increased values of atherosclerotic markers.
Early atherosclerosis: Atherosclerosis in young women, although a relatively rare occurrence, needs close attention and vigorous treatment.
The risk factors for accelerated atherosclerosis in young women are HTN, smoking, oral contraceptive (OC) pills intake, hyperlipidemia, premature menopause, underlying inflammatory disease (e.g., SLE, RA), diabetes mellitus, and family history. Other possible risk factors have included prolonged steroid use, homocystinemia, thrombocytosis, blood clotting disorders, previous viral infections, hyperinsulinemia and, of course, genetic factors.
Discussion: AAA is a disease predominantly seen in men > 50 years, and it is more common in smokers. The incidence in women increases with age, with a prevalence of only 0.4 to 1.3% in women > 65 years. The most common etiology seen is atherosclerosis, HTN, tobacco use, hypercholesterolemia, and associated CAD. The incidence in young women < 40 years is reported to be < 0.1%. The most common etiology seen is vasculitis, autoimmune disorders, early atherosclerosis associated with obesity, and dyslipidemia. In this case, patient presented with first episode of hypertensive emergency with de novo CKD, ACS (NSTEMI) and incidentally diagnosed AAA on imaging. The right renal artery is originating from the aneurysmal part of aorta with shrunken right kidney. So, renal failure in this case is due to AAA or AAA is due to renal failure and associated HTN, leading to degenerative changes which are not clear.
Also, the patient had high thrombus burden in coronaries as well as in AAA; CAD in young is usually seen in males with strong association with smoking. CAD in young females is again rarely seen and factors associated with this early atherosclerosis include CKD, HTN, dyslipidemia, South Asian race, homocysteinemia, Lp (a), metabolic syndrome, and other vasculitic or autoimmune causes.
In this case, renal failure with HTN can be considered as the factor triggering early atherosclerosis and CAD. All the inflammatory markers having strong association with early atherosclerosis were positive in this patient.
Clinical diagnosis: early atherosclerosis with ACS NSTEMI with AAA.
Discussion of management: Patient treated with diuretics, vasodilators, antiplatelets, statins, hemodialysis, blood transfusion, and PCI to LAD.
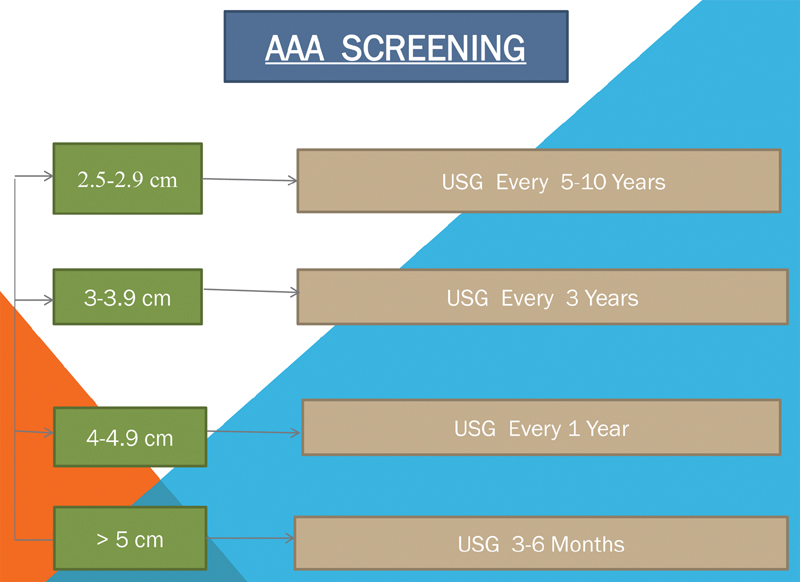
Abdominal Aorta Screening
AAA screening guidelines as shown in Fig. 8.
-
Fig. 8 Abdominal aortic aneurysm (AAA) screening guidelines.
Fig. 8 Abdominal aortic aneurysm (AAA) screening guidelines.
Presenter: Patient is advised to follow-up with USG abdomen and pelvis every year, based on screening guidelines.
Conflict of interest
None declared.
References
- Antiphospholipid antibodies (APLA) in immune thrombocytopenic purpura (ITP) and antiphospholipid syndrome (APS) Am J Hematol. 2006;81(06):391-396.
- [Google Scholar]
- Risk factors and comorbidities associated to cardiovascular disease in Qatar: a machine learning based case-control study. IEEE Access. 2021;9:29929-29941.
- [Google Scholar]
- New perspectives on the prevalence of hypertrophic cardiomyopathy. J Am Coll Cardiol. 2015;65(12):1249-1254.
- [Google Scholar]
- Impact of atrial fibrillation on the clinical course of hypertrophic cardiomyopathy. Circulation. 2001;104(21):2517-2524.
- [Google Scholar]
- Hypertrophic cardiomyopathy: genetics, pathogenesis, clinical manifestations, diagnosis, and therapy. Circ Res. 2017;121(07):749-770.
- [Google Scholar]
- Clinical profile and outcome of idiopathic restrictive cardiomyopathy. Circulation. 2000;101(21):2490-2496.
- [Google Scholar]
- Premature cardiovascular disease is common in relatives of patients with premature peripheral atherosclerosis. Arch Intern Med. 2000;160(09):1343-1348.
- [Google Scholar]
- Right ventricular sarcoidosis: is it time for updated diagnostic criteria? Tex Heart Inst J. 2014;41(02):203-207.
- [Google Scholar]
- Hypertensive hypertrophic cardiomyopathy of the elderly. N Engl J Med. 1985;312(05):277-283.
- [Google Scholar]
- Association of anti-phospholipid antibodies with connective tissue diseases. Indian Dermatol Online J. 2015;6(02):89-91.
- [Google Scholar]
- Mixed connective tissue disease. Best Pract Res Clin Rheumatol. 2016;30(01):95-111.
- [Google Scholar]
- Clinical diagnosis and management of large vessel vasculitis: Takayasu arteritis. Curr Cardiol Rep. 2014;16(07):499.
- [Google Scholar]
- Behçet's disease: new insights into pathophysiology, clinical features and treatment options. Autoimmun Rev. 2018;17(06):567-575.
- [Google Scholar]
- Blood pressure, hypertension and the risk of abdominal aortic aneurysms: a systematic review and meta-analysis of cohort studies. Eur J Epidemiol. 2019;34(06):547-555.
- [Google Scholar]






