Translate this page into:
Vicious Rhythm of a Toxic Lady’s Glove
*Corresponding author: Praveen Nagula, Department of Cardiology, Osmania General Hospital, Hyderabad, Telangana, India. drpraveennagula@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Chintala V, Parvathareddy K, Motkar A, Nagula P. Vicious Rhythm of a Toxic Lady’s Glove. Indian J Cardiovasc Dis Women. doi: 10.25259/IJCDW_45_2024
Abstract
Digitalis glycosides are among the oldest drugs used in cardiology. Despite the reduction in digoxin use and improved therapeutic monitoring, digoxin toxicity remains a significant cause of morbidity and mortality due to its use in specific cardiac diseases. Suspicion of digoxin toxicity should involve supportive care, discontinuation of the drug and administration of digoxin-specific antibody fragments. We present a case of a 62-year-old female with heart failure, who was administered intravenous digoxin for her presentation with atrial fibrillation having a fast ventricular rate. Subsequently, the patient had a junctional rhythm which was mistaken for controlled ventricular rate. This led to bidirectional tachycardia, the sine qua non of digitoxicity. The renal parameters were deranged. The patient was managed with antiarrhythmics and dialysis.
Keywords
Atrial fibrillation
Bidirectional tachycardia
Digoxin antibody
Digoxin toxicity
Paroxysmal Junctional tachycardia
INTRODUCTION
The recommended medications to control the ventricular in a patient with atrial fibrillation and left ventricular dysfunction are digoxin and amiodarone. It is important to mention that digoxin toxicity (digitoxicity) is often missed due to its narrow therapeutic index. Life-threatening arrhythmias (both Brady and tachyarrhythmias) can manifest in toxicity, due to the digoxin action to slow the sodium-potassium ATPase (Na-K-ATPase) pump and stimulate the backup pacemakers of the heart. Of the arrhythmias, bidirectional tachycardia is the diagnostic arrhythmia of digtoxicity.
CASE REPORT
A 62-year-old female presented to the emergency room with shortness of breath and palpitations. She is being medically managed for her heart failure with reduced ejection fraction. On examination, she had a heart rate of 200 per min with a blood pressure of 130/90 mm Hg. An electrocardiogram revealed atrial fibrillation with a fast ventricular rate. In view of her heart failure, she was given intravenous digoxin, which brought her heart rate to 110 bpm [Figure 1]. Intravenous furosemide was given leading to symptomatic improvement. A repeat ECG showed a ventricular rate of 80 bpm with a regularized rhythm. Four hours later, the patient complained of chest pain, and a repeated ECG showed bidirectional tachycardia (right bundle branch block alternating with the left anterior hemiblock) [Figure 2]. The serum creatinine was 5.6 mg/dL. Digoxin toxicity was suspected due to the varying arrhythmias and she was given intravenous lidocaine as digoxin antibodies were not available. She underwent hemodialysis for her deranged renal function tests. Unfortunately, serum digoxin levels could not be assessed due to unavailability of testing at our center. However, the diagnosis of digoxin toxicity was made based on strong clinical indicators, namely, the temporal sequence of digoxin administration, emergence of junctional and bidirectional tachyarrhythmias, and renal dysfunction.
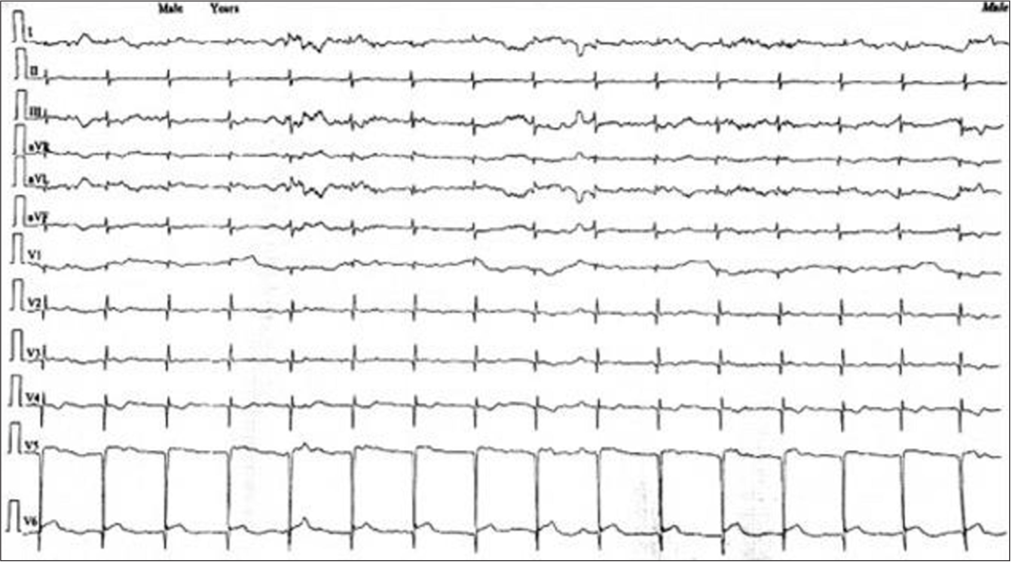
- Electrocardiography taken after intravenous digoxin showing regular narrow complex tachycardia. No visible p waves were seen suggesting the tachycardia to be originating from the atrioventricular node.
![Electrocardiography after the onset of chest pain, showing narrow complex regular tachycardia. There are no p waves seen. The QRS morphology varies in the strip recorded (right bundle branch morphology [in circle] and left anterior hemiblock [in square box]) suggesting bidirectional ventricular tachycardia.](/content/148/2025/0/1/img/IJCDW-45-2024-g002.png)
- Electrocardiography after the onset of chest pain, showing narrow complex regular tachycardia. There are no p waves seen. The QRS morphology varies in the strip recorded (right bundle branch morphology [in circle] and left anterior hemiblock [in square box]) suggesting bidirectional ventricular tachycardia.
DISCUSSION
Digoxin is a cardiac glycoside derived from digitalis purpurea (foxglove) and digitalis lanata (woolly foxglove). The term “Digitalis” was coined by the German scholar Fuchsius. Its primary mechanism of action is to inhibit Na-K ATP ase, which increases intracellular calcium, leading to an increase in the force of contraction (inotropy).[1] It also has parasympathetic action on the sinoatrial node, slows the discharge rate, shortens the refractory period of the atria, and prolongs the Atrioventricular nodal refractoriness. Electrophysiologic effects on the His-Purkinje system and ventricular muscle are minimal, except with toxic concentrations. The PR interval, QRS, and QT intervals are generally unaffected, except in patients with underlying AV node disease. PR interval is prolonged. The characteristic ST and T wave abnormalities seen with the use of digoxin (digoxin effect) do not represent toxicity.[1]
The therapeutic effects of digoxin are observed when the serum digoxin concentration (SDC) is between 0.5 and 0.9 ng/dL. Mortality increases when SDC exceeds 1 ng/dL. Most patients experiencing digoxin toxicity are elderly, have other cardiac and non-cardiac comorbidities, and are on multiple medications, some of which are known to potentially interfere with SDC. The most common presentation of digoxin toxicity is due to unintentional overdose or decreased drug clearance caused by hepatic or renal dysfunction.[2] Patients with acute toxicity present with symptoms such as anorexia, nausea, vomiting, and fatigue. Chronic toxicity usually presents with an insidious onset over days to weeks, with neurological symptoms including confusion, disorientation, and fatigue. Visual changes such as halos, scotomas, flashing lights, and xanthopsia have also been reported.
At toxic levels, digoxin-mediated increased myocyte excitability due to decreased resting membrane potential combined with increased vagal tone can cause almost any type of cardiac arrhythmias. The most common electrocardiographic manifestations of toxicity include atrioventricular block, escape rhythms, and premature ventricular contractions. These common arrhythmias are non-specific, with many etiologies, but junctional tachycardia and bi-ventricular tachycardia are strongly suggestive of digoxin toxicity.[3] In addition to renal dysfunction, polypharmacy and underlying dyselectrolytemia – common in heart failure patients, significantly increase the risk of digoxin toxicity. Medications such as diuretics, Angiotensin-Converting Enzyme inhibitors, and spironolactone can predispose to hypokalemia and hyperkalemia, both of which alter digoxin’s electrophysiological effects and toxicity threshold.
The drug can cause disturbances by creating an A-V nodal block and stimulating subsidiary pacemakers. When a regular rhythm develops in a patient with chronic atrial fibrillation, it may indicate digitalis intoxication.[4] The regular rhythm can be caused by the development of paroxysmal junctional tachycardia. In this case, the regularized rhythm was mistakenly interpreted as rate control when the patient received intravenous digoxin. This arrhythmia is increasingly recognized as a common manifestation of digitalis intoxication, more common than the well-known arrhythmia atrial tachycardia with block.[5]
When digitalis intoxication goes unnoticed and progresses to accelerated junctional rhythms, with or without an exit block, the final arrhythmia may be bidirectional tachycardia.[6,7] This serious abnormality is thought to be caused by the toxic effects of digitalis on ventricular conduction. The right bundle branch block is often present, and conduction in the left ventricle is believed to occur alternately over the anterior and posterior divisions of the left bundle. While serum digoxin levels can aid in diagnosis, clinical judgment remains paramount, especially when the classical ECG manifestations, such as bidirectional tachycardia, are observed.[6,7] In practice, levels may not always be promptly available, and therapy should not be delayed in cases with high clinical suspicion. Farkas (2025) emphasizes that clinical indicators, such as bidirectional tachycardia occurring in the context of heart failure and renal impairment, should prompt presumptive treatment before laboratory confirmation.[8]
All patients with suspected digoxin toxicity should receive supportive care and digoxin should be discontinued. Patients experiencing chronic digoxin toxicity and exhibiting elevated drug levels are typically dehydrated and may have acute renal failure. Proper hydration and management of renal failure may have a more significant impact on clinical outcomes than the administration of digoxin-specific antibodies.
In cases of renal failure and hyperkalemia, emergent hemodialysis may be considered. However, it is not effective in treating digoxin toxicity due to the drug’s extensive fat distribution. Indications for treatment with digoxin-specific antibodies in the setting of chronic toxicity include life-threatening arrhythmias (ventricular tachycardia or fibrillation), severe bradycardia unresponsive to atropine, impaired renal function with increased digoxin concentration, and hyperkalemia resistant to standard potassium-lowering therapy.[9] In 2025, expert consensus strongly advocates for the prompt use of digoxin-specific antibodies in suspected cases of life-threatening digoxin toxicity, even before confirming serum levels. This recommendation comes in light of the significant mortality risk linked to ventricular arrhythmias (Hack et al., 2025).[10]
Learning points
Suspicion of digitalis toxicity is of paramount importance in the presence of predisposing factors such as renal dysfunction, hypokalemia in heart failure patients.
The occurrence of junctional tachycardia in patients with atrial fibrillation with pharmacological cardioversion should provoke the suspicion of digitoxicity.
Bidirectional tachycardia is the sine qua non of digitoxicity.
Digoxin levels may not be available allover; the clinical assessment forms the primary role in diagnosing digitoxicity.
CONCLUSION
Careful patient selection, individual risk factor consideration, clinical manifestation evaluation, serum monitoring, and recognition of digoxin-mediated arrhythmias are essential for effective treatment and reduction of morbidity and mortality in this patient population.
Ethical approval:
Institutional Review Board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine. (12th ed). Netherlands: Elsevier Saunders; 2022. p. :761-774.
- [Google Scholar]
- Cardiac Glycoside Toxicity: More than 200 Years and Counting. Crit Care Clin. 2012;28:527-35.
- [CrossRef] [PubMed] [Google Scholar]
- Digoxin-Associated Mortality: A Systematic Review and Meta-Analysis of the Literature. Eur Heart J. 2015;36:1831-8.
- [CrossRef] [PubMed] [Google Scholar]
- Digitalis Intoxication in Patients with Atrial Fibrillation. Circulation. 1973;47:888-96.
- [CrossRef] [PubMed] [Google Scholar]
- Too Much of a Good Thing: Digitalis Toxicity. Am J Med. 2015;128:257-9.
- [CrossRef] [PubMed] [Google Scholar]
- Digitalis Intoxication. A Prospective Clinical Study with Serum Level Correlations. N Engl J Med. 1971;284:989-97.
- [CrossRef] [PubMed] [Google Scholar]
- Digoxin & Cardiac Glycosides: Toxicity & Therapeutic Use. 2025. EMCrit Project. Available from: https://emcrit.org/ibcc/dig [Last accessed on 2024 Jul 29]
- [Google Scholar]
- Clinical Outcomes from Early use of Digoxin-Specific Antibodies Versus Observation in Chronic Digoxin Poisoning (ATOM-4) Clin Toxicol (Phila). 2019;57:638-43.
- [CrossRef] [PubMed] [Google Scholar]
- Expert Consensus on the Diagnosis and Management of Digoxin Toxicity. Am J Med. 2025;138:25-33.e14.
- [CrossRef] [PubMed] [Google Scholar]








