Translate this page into:
Treatment of an Unyielding Central Vein Stenosis using Valvuloplasty Balloon in a Young Female Presenting with Ineffective Hemodialysis
Anupam Bhambhani, M.D., D.M., F.E.S.C. Associate Professor, Department of Cardiology, Vydehi Institute of Medical Sciences and Research Centre Whitefield, Bangalore, India 560066 anupam.bhambhani@yahoo.in
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Percutaneous balloon venoplasty is widely employed for the management of central vein stenosis (CVS), a condition frequently encountered in patients on maintenance hemodialysis (MHD). The hypertrophied and fibrotic venous stenotic lesions often pose a challenge for interventionists, due to resistance to dilatation and high-elastic recoil. We report here successful utilization of mitral valvuloplasty balloon for percutaneous treatment of an unyielding brachiocephalic vein stenosis. Repeated failure of conventionally used peripheral balloon dilatation catheter prompted the use of a mitral valvuloplasty balloon that could exert higher radial pressure while preventing melon-seeding and hence successfully achieve stenosis dilatation. The mitral valvuloplasty balloon can be effectively and safely used for lesions resistant to repeated dilatations by conventional peripheral balloons. Rheological stress on central veins from ipsilateral arteriovenous fistula (AVF) may result in development of stenotic lesions, even in the absence of prior venous catheterization of the affected vein; therefore, in the presence of relevant symptoms, this diagnosis should not be excluded on the basis of absence of prior direct trauma at the stenosis site.
Keywords
brachiocephalic vein stenosis
Central vein stenosis
Innominate vein stenosis
valvuloplasty balloon
venoplasty
Introduction
Central vein stenosis (CVS) is commonly encountered in patients on maintenance hemodialysis (MHD). It eventuates from chronic endothelial injury that occurs in response to the long indwelling vascular catheters as well as the rheological effects of hyperdynamic blood flow across surgically created arteriovenous fistula (AVF).
Percutaneous transluminal balloon venoplasty (PTBV) with or without stent implantation is the treatment of choice for CVS.1 Frequently, the CVS lesions are associated with severe hypertrophy and fibrosis, since the veins ipsilateral to the AVF are persistently exposed to arterial pressure. These factors result in resistance to dilatation and high-immediate recoil. We report here an unconventional use of valvuloplasty balloon for the effective treatment of a critical innominate vein stenosis, where the lesion was resistant to dilatation with conventional balloon.
Case Report
A 40-year-old hypertensive, nondiabetic lady, with end-stage renal disease (ESRD) and on MHD via AVF created between left brachial artery and cephalic vein, presented with progressive swelling of the left upper limb and face. Doppler interrogation of the left arm revealed left innominate vein stenosis and patent AVF. She was referred to us for further management. There was history of MHD through right internal jugular vein (IJV) access, that is, contralateral to the AVF, for six weeks during AVF maturation period.
Clinically, there was gross edema involving left arm and left half of the face, with tortuous and dilated neck veins. There was no history of temporary catheter insertion into the affected veins.
A superior venacavogram, done via right femoral vein access, revealed severe stenosis of the left innominate vein and extensive venous collaterals ( Fig. 1 A, Video 1).

-
Fig. 1 (A). Severe stenosis in left innominate vein with extensive collaterals; (B). Innominate vein after dilatation with valvuloplasty balloon (note the disappearance of venous collaterals).
Fig. 1 (A). Severe stenosis in left innominate vein with extensive collaterals; (B). Innominate vein after dilatation with valvuloplasty balloon (note the disappearance of venous collaterals).
We decided to treat the stenosis percutaneously. Written informed consent was obtained from the patient. The stenosis was crossed using a J-tipped 0.035-inch, 150-cm Glidewire (Terumo Interventional Systems, Japan) loaded into a 5F Multipurpose-A1 diagnostic catheter (Boston Scientific, USA). After exchanging the Glidewire for a stiffer 0.035-inch, 260 cm PTFE-coated guidewire, balloon dilatation was attempted several times using a small diameter (5 × 80 mm) peripheral balloon (Armada35 PTA catheter, Abbott, USA), so that space could be created for the passage of larger diameter balloons; however, the lesion recoiled immediately after each dilatation, leaving no effective lumen enlargement. It was challenging to advance a bulkier cutting balloon across the lesion, due to the resistance from tight stenosis and the acute angulation between superior vena cava (SVC) and innominate vein. After repeated unsuccessful attempts, we decided to switch to a balloon used for percutaneous transluminal mitral commissurotomy (PTMC).
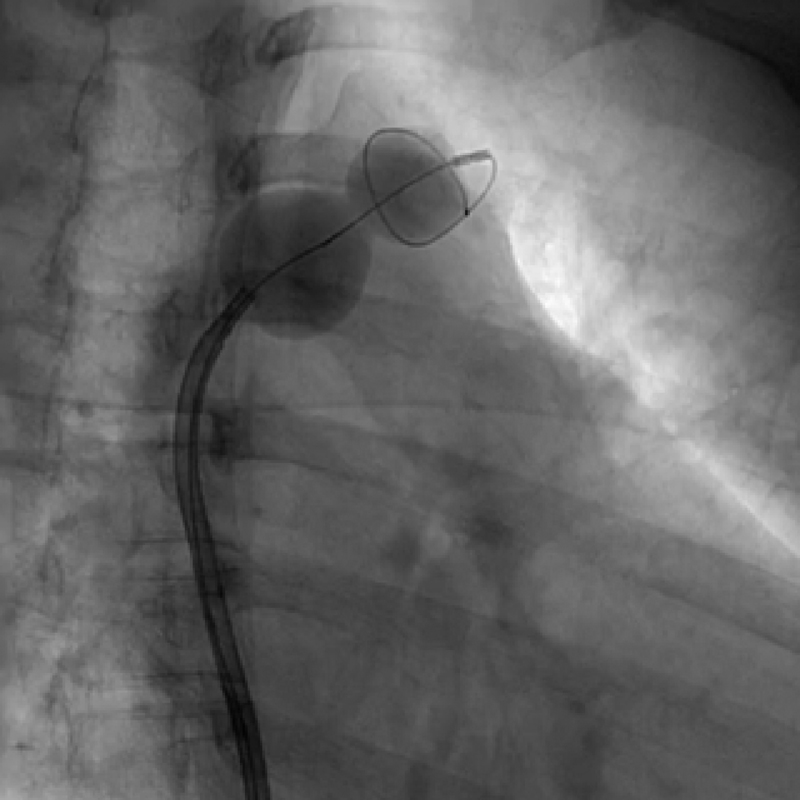
Since the affected innominate vein was grossly dilated, the balloon inflation diameter was decided, corresponding to the contralateral innominate vein diameter. After exchanging the 0.035-inch wire for pigtail-spring guidewire (Fig. 2) through MP-A1 catheter, the PTMC balloon, slenderized on its stretching tube, was advanced and positioned across the stenosis. Following three dilatations (Fig. 2), each lasting 10 minutes, the lesion yielded without recoil (Fig. 1 B). There was significant angiographic improvement with no residual gradient, and the collaterals regressed immediately (Fig. 1 B, Video 2). On the following day, facial and arm swelling were found reduced. The postprocedure period was uneventful.
-
Fig. 2 Innominate vein stenosis being dilated with the help of valvuloplasty balloon.
Fig. 2 Innominate vein stenosis being dilated with the help of valvuloplasty balloon.
Discussion
The PTMC balloon was originally conceptualized by the Japanese genius Kanji Inoue for mitral valvuloplasty. In the present case, where stenosis was recoiling despite repeatedly dilating with conventional balloon, PTMC balloon helped in achieving procedural success. The dilatation in this case could be attributed to some quintessential features of the PTMC balloon: a) unlike bulky cutting/scoring balloons, it could be slenderized on its stretching tube and smoothly advanced across the challengingly acute angle between superior vena cava and brachiocephalic vein (Fig. 1 A), despite the resistance imposed by critical stenosis; b) the pigtail-tip guidewire offered very good support, despite short stationing space available distal to the stenosis; c) due to its unique texture, the PTMC balloon could exert stronger force on the hypertrophied and fibrosed stenotic wall; and d) since the PTMC balloon acquires an hour-glass shape when it expands, it did not slip (melon-seed) while dilating the tight, fibrotic stenosis.
Another advantage offered by the PTMC balloon is that a single balloon provides a range of expansion diameters, allowing progressive and safe dilatations, while precluding the need for repeated balloon exchanges.
CVS often leads to inadequate hemodialysis due to fistula failure or increased venous back pressure. Various mechanisms proposed to explain the occurrence of CVS converge on to the endothelial denudation occurring secondary either to the rheological damage resulting from high velocity blood flow through AVF or to the chronic abrasion caused by venous catheters. This, in turn, results in thrombin generation, platelet activation, and initiation of an inflammatory response that culminates in intimal hyperplasia, fibrosis and, finally, stenosis at the site of venous injury.2
CVS is conventionally managed by balloon dilatation, followed by stenting in some cases. In a large study comparing venoplasty with or without stent implantation, the patency rates were not significantly different with either of the two strategies.1
To the best of our knowledge, use of this balloon has not been reported for treating CVS. The balloon dilatation was effective and safe, and postoperative recovery was uneventful with substantial improvement in symptoms.
Conclusion
Venoplasty remains the treatment of choice for CVS. In case of poor immediate response to PTV due to the acute recoil, use of PTMC balloon may be considered as a safe and effective alternative.
Conflict of Interest
The authors declare that there are no conflicts of interest concerning this case study.
References
- Percutaneous treatment of central venous stenosis in hemodialysis patients: long-term outcomes. Cardiovasc Intervent Radiol. 2009;32(02):271-278.
- [Google Scholar]
- Left Brachiocephalic vein stenosis due to the insertion of a temporal right subclavian hemodialysis catheter. Case Rep Vasc Med. 2017;2017:9524739.
- [Google Scholar]










