Translate this page into:
The Interplay of Anemia and Cardiovascular Disease in Pregnant Women and APGAR Scores of their Newborn: A Retrospective Study in Pregnant Women
*Corresponding author: Ravi Kumar, Department of Community Medicine, Shri Ram Murti Smarak Institute of Medical Sciences, Bareilly, Uttar Pradesh, India. srmsimsravi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kumar R, Goyal P, Khan H. The Interplay of Anemia and Cardiovascular Disease in Pregnant Women and APGAR Scores of their Newborn: A Retrospective Study in Pregnant Women. Indian J Cardiovasc Dis Women. 2024;9:128-35. doi: 10.25259/IJCDW_58_2023
Abstract
Objectives:
The implications of maternal anemia extend beyond the immediate physiological consequences; moreover, the consequences of maternal anemia are not limited to the mother alone. It may lead to low Appearance, Pulse, Grimace, Activity, and Respiration (APGAR) scores. It, further, adds up to higher incidence of morbidity rates in neonates. The objective of the study is to assess the prevalence and severity of anemia during pregnancy, to establish a correlation between maternal hemoglobin (Hb) levels and APGAR scores in newborns, and determine the association between cardiovascular disease and severity of anemia.
Materials and Methods:
A retrospective study was conducted at a private medical college in Bareilly from March 2022 to March 2023. The study focused on pregnant females aged 15–49 years who were admitted and delivered within the facilities of the private medical college during this period. Pregnant females with pre-existing chronic conditions affecting Hb levels were excluded from the study. A total of 130 subjects were included in the study, and their Hb levels and APGAR scores at 1 min were considered for analysis.
Results:
The results show a spearmen rank correlation coefficient (r) = 0.575 between maternal Hb levels and APGAR scores at 1 min, indicating a significant positive relationship (P < 0.05). Infants born to mothers with moderate anemia exhibited the highest prevalence of low APGAR scores (<4), highlighting the potential impact of maternal anemia on immediate neonatal well-being. No significant association was found between cardiovascular diseases in pregnancy and severity of anemia.
Conclusion:
The findings indicate that the optimization of maternal Hb levels is a critical intervention to ensure a healthier start for the neonate. This study provides a crucial foundation for evidence-based practices in maternal healthcare and neonatal well-being. Focus on improving maternal Hb provides multifaceted benefits both in mothers and neonates.
Keywords
Anemia
APGAR score
Newborn
Hemoglobin
Correlation
ABSTRACT IMAGE
INTRODUCTION
Maternal health is a paramount concern in the realm of obstetrics, influencing both the well-being of the expectant mother and the optimal growth and development of the unborn child. Pregnancy increases considerably the iron needs in a mother and her fetus. During pregnancy, the fetal demand for iron increases maternal iron requirements by about 1 g.[1]Anemia during pregnancy, characterized by a decreased concentration of hemoglobin (Hb) in the blood, is a global public health challenge with far-reaching implications for both maternal and fetal outcomes. Anemia during pregnancy is defined as the Hb criteria is <11 g/dL.[2] A decline in Hb levels can compromise the blood’s oxygen-carrying capacity, potentially leading to detrimental effects on both maternal health and fetal development.
According to the recent data from the National Family Health Survey–5, the prevalence of anemia among pregnant women (15– 49 years) is a staggering 52.2%.[3] This underscores the pervasive nature of this public health challenge. This underscores the pervasive nature of this public health challenge, revealing that more than half of the expectant mothers in the surveyed population face the adverse effects of anemia during pregnancy. Anemia’s high prevalence among pregnant women necessitates urgent attention and comprehensive strategies to mitigate its impact on both maternal and fetal health. The profound implications of anemia during pregnancy are manifold, potentially leading to increased maternal morbidity, mortality, and adverse birth outcomes.
The implications of maternal anemia extend beyond the immediate physiological consequences. For the expectant mother, anemia can manifest as fatigue, weakness, shortness of breath, and diminished work capacity, which can significantly impact daily activities and overall quality of life. Severe anemia can lead to circulatory decompensation, increased cardiac output, an increased risk of hemorrhage, and decreased ability to tolerate blood loss, leading to circulatory shock and death.[4] However, the consequences of maternal anemia are not limited to the mother alone. The developing fetus relies entirely on the mother’s bloodstream for essential nutrients, including oxygen. Maternal anemia compromises the oxygen supply to the fetus, potentially impairing fetal growth and development. It may lead to preterm delivery, neonatal mortality, low birth weight, placental abruption, compromised head circumference and crown heel length, low APGAR scores, duration of hospital stay, etc.[5] This, further, adds up to higher incidence of morbidity rates.
Given the significant health implications associated with maternal anemia, understanding its intricate relationship with neonatal outcomes, as assessed by the APGAR score, is imperative. The Apgar score, developed by Virginia APGAR in 1952, offers a rapid assessment of the infant’s physical condition at birth.[6] This scoring system provides valuable insights into the newborn’s cardiovascular, respiratory, neuromuscular, and adaptive capacities, offering a snapshot of their transition from the intrauterine environment to extrauterine life.
Exploring the connection between maternal anemia and Apgar scores is a critical step toward elucidating the potential impact of maternal health on neonatal well-being. This research seeks to uncover correlations and patterns that could aid in the early identification of infants at risk due to maternal anemia. Ultimately, our goal is to contribute to evidence-based practices in maternal healthcare, optimize antenatal care strategies, and improve both short-term and long-term outcomes for both mother and child.
Aim
The aim of this study was to investigate the relationship between anemia and cardiovascular diseases during pregnancy and the impact of anemia on APGAR scores in newborns.
Objectives
The objectives of this study were as follows:
To assess the prevalence and severity of anemia during pregnancy in study population
To determine the relationship between cardiovascular diseases and severity of anemia in pregnant women
To correlate maternal Hb levels with APGAR scores.
MATERIALS AND METHODS
A retrospective study was conducted at SRMS Institute of Medical Sciences in Bareilly from March 2022 to March 2023. The study focused on pregnant females who were admitted and delivered within the facilities of the private medical college during this period. Pregnant females aged between 15 and 49 years who were admitted and subsequently delivered within the specified study duration were included in the study. Pregnant females with pre-existing chronic conditions affecting Hb levels, such as chronic kidney disease or hematological disorders, were excluded from the study.
Our initial study plan called for a comprehensive enumeration analysis spanning 2018–2022. However, we faced a significant challenge during the planning phase because the hospital’s records were only available from 2021 onwards. To maintain the integrity and representativeness of our sample, we had to make a strategic adjustment due to the limited availability of data. In response, we adopted a simple random sampling method, extracting ten samples per month from the available data during the reference period. This approach aimed to reduce the impact of the data availability issue while still ensuring a representative sample of the population under study. As a result, our final sample size consisted of 130 samples collected throughout the study period.
Hb levels of pregnant women along with details of cardiovascular diseases including hypertension, and APGAR scores of newborn at 1 min along with sociodemographic details were recorded in a case sheet.
Ethical clearance was obtained from the Institutional Ethical Committee to ensure adherence to ethical guidelines and the protection of participants’ rights and privacy throughout the study.
Statistical analysis was performed using Microsoft Excel 2019 and Minitab 19.1 statistical software. Frequencies and percentages were calculated for categorical data, and descriptive statistics were used to depict continuous data. Furthermore, correlation analysis was employed to assess the relationship between maternal anemia and APGAR scores in newborns, depending on the fact of normality. P < 0.05 was considered statistically significant. Chi-square test was done to determine the association between hypertension and severity of anemia.
RESULTS
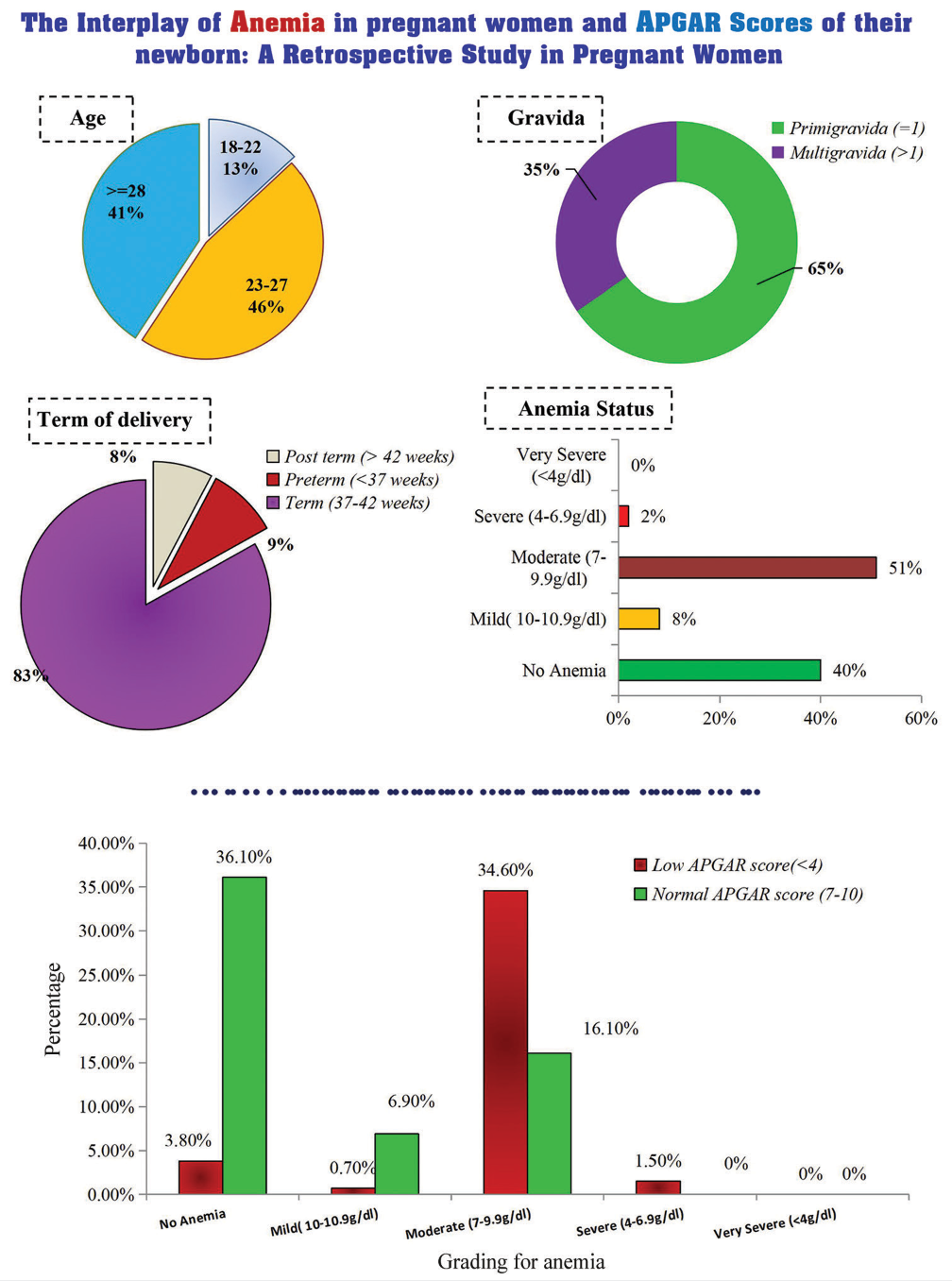
In this study, Table 1 presents a comprehensive snapshot of the study participants, offering insights into key dimensions. Age distribution indicates 13.1% of individuals in the 18–22 age group, 46.2% in the 23–27 category, and 40.8% aged 28 or older. Religious affiliation shows 51.5% identifying as Hindu and 48.5% as Muslim. Term of delivery data displays 7.7% post-term (>42 weeks), 9.2% preterm (<37 weeks), and 83.1% within the term range (37–42 weeks). Table 2 provides insightful data on maternal health parameter, showcasing the distribution of maternal anemia as per classification of anemia in pregnant women based on ICMR classification with an average Hb level of approximately 9.86 ± 1.9619 grams per deciliter (g/dL) among the mothers. Approximately 41% of the study population do not have anemia and 55% of the study population have moderate anemia. In the absence of cardiovascular disease, moderate anemia was present in 48.9% of expectant women, mild anemia in 9.8%, and absence of anemia in 41.3%. On the contrary, moderate anemia was present in 55.3% of expectant women diagnosed with cardiovascular disease, mild anemia in 2.6%, and absence of anemia in 36.8%. It was determined that P-value (0.0731) was not statistically significant in Table 3.
| Variable | Levels | Frequency | Percentage |
|---|---|---|---|
| Age | 18–22 | 17 | 13.1 |
| 23–27 | 60 | 46.2 | |
| ≥28 | 53 | 40.8 | |
| Religion | Hindu | 67 | 51.5 |
| Muslim | 63 | 48.5 | |
| Gravida | Primigravida (=1) | 85 | 65.4 |
| Multigravida (>1) | 45 | 34.6 | |
| Term of delivery | Preterm (<37 weeks) | 12 | 9.2 |
| Term (37–42 weeks) | 108 | 83.1 | |
| Post term (> 42 weeks) | 10 | 7.7 |
n: Total study participants
| Grading for anemia | Frequency | Percentage |
|---|---|---|
| No anemia | 52 | 40 |
| Mild (10–10.9 g/dL) | 10 | 8 |
| Moderate (7–9.9 g/dL) | 66 | 51 |
| Severe (4–6.9 g/dL) | 2 | 2 |
| Very severe (<4 g/dL) | 0 | 0 |
n: Total study participants
| Grading for anemia | Frequency | Percentage |
|---|---|---|
| No anemia | 14 | 37 |
| Mild (10–10.9 g/dL) | 1 | 3 |
| Moderate (7–9.9 g/dL) | 21 | 55 |
| Severe (4-6.9 g/dL) | 2 | 5 |
| Very severe (<4 g/dL) | 0 | 0 |
n: Total study participants
Table 4 provides a valuable comparison between the severity of maternal anemia, categorized by Hb levels, and the resulting APGAR scores of newborns at 1 min after birth. The severity of anemia is classified into five categories: No anemia, mild, moderate, severe, and very severe. Strikingly, infants born to mothers with moderate anemia (7–9.9 g/dL) exhibited the highest percentage of low APGAR scores (<4), constituting 45% of cases in this category. On the other hand, infants of mothers with mild anemia (10–10.9 g/dL) had a lower occurrence of low APGAR scores, with only 1% of cases. Importantly, no cases of severe or very severe anemia in mothers were associated with low APGAR scores at 1 min. These findings shed light on the potential correlation between maternal anemia severity and immediate neonatal well-being, emphasizing the need for targeted interventions to enhance both maternal and neonatal health outcomes.
| Grading for anemia | Cardiovascular diseases | Total (n=130) (%) | Test statistic | P-value | |
|---|---|---|---|---|---|
| Present (n=38) (%) | Absent (n=92) (%) | ||||
| Severe (4–6.9 g/dL) | 2.0 (5.3) | 0.0 (0.0) | 2.0 (1.5) | 6.98* | 0.0731 |
| Moderate (7–9.9 g/dL) | 21.0 (55.3) | 45.0 (48.9) | 66.0 (50.8) | ||
| Mild (10–10.9 g/dL) | 1.0 (2.6) | 9.0 (9.8) | 10.0 (7.7) | ||
| No anemia | 14.0 (36.8) | 38.0 (41.3) | 52.0 (40.0) | ||
Table 5 depicts two critical variables, that is, Hb levels measured in g/dL, indicative of maternal well-being, and the APGAR score at 1 min, reflecting the immediate neonatal health status post-birth. The average Hb level among the 130 subjects was approximately 9.863 g/dL, with a standard deviation of 1.962, suggesting a moderate degree of variability in maternal Hb levels. The minimum observed Hb level was 6.000 g/dl, while the maximum was 14.600 g/dL. At the first quartile (Q1), 25% of the subjects had a Hb level of 8.000 g/dL or lower, whereas at the third quartile (Q3), 75% of the subjects exhibited a Hb level of 11.325 g/dL or lower.
| Parameters | Hemoglobin (g/dL) | APGAR Score at 1 min |
|---|---|---|
| Mean | 9.86 | 7.24 |
| SD | 1.96 | 1.94 |
| Minimum | 6.00 | 0.00 |
| Q1 (25th Percentile) | 8.00 | 5.00 |
| Median (50th Percentile) | 9.65 | 8.00 |
| Q3 (75th Percentile) | 11.33 | 9.00 |
| Maximum | 14.60 | 9.00 |
APGAR: Appearance, pulse, grimace, activity, and respiration, Q1: First Quartile, Q3: Third Quartile, n: Total study participants, SD: Standard deviation
On the other hand, the APGAR score at 1 min, which evaluates neonatal well-being, had an average of 7.238 with a standard deviation of 1.936. At the first quartile (Q1), 25% of the newborns had an APGAR score of 5.000 or lower, while at the third quartile (Q3), 75% of the newborns exhibited an APGAR score of 9.000.
The histogram presented in Figure 1 portrays the distribution of Hb levels among all subjects. The histogram clearly illustrates a non-normal distribution, emphasizing the variability and diversity within the data. The shape of the histogram deviates from the typical bell curve associated with a normal distribution and showcases a skewed distribution. The histogram presented in Figure 2 offers a visual representation of the distribution of APGAR scores among all subjects. This histogram particularly highlights a distribution that deviates from the normal pattern, demonstrating a noticeable right skew. The skewness toward the higher APGAR scores indicates that a significant proportion of newborns exhibited robust health immediately after birth, as reflected by higher APGAR scores.

- Distribution of hemoglobin levels in pregnant women. (N: Sample size.)
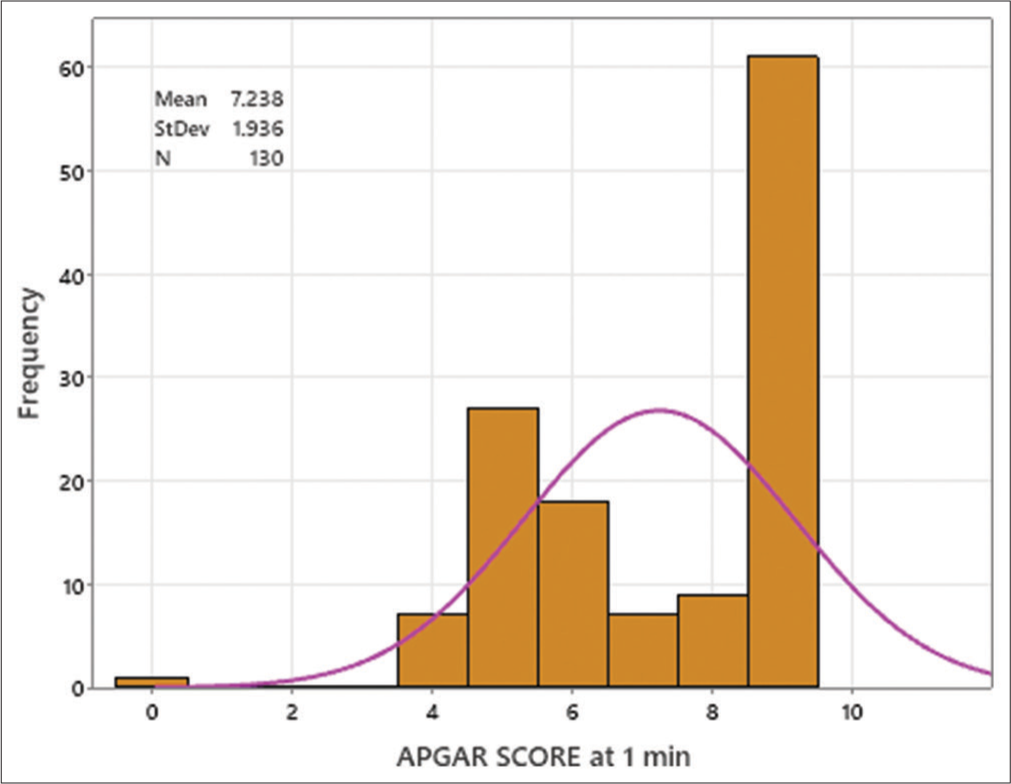
- Distribution of APGAR scores at 1 min in newborn. (APGAR: Appearance, pulse, grimace, activity, and respiration, N: Sample size.)
Understanding the distribution of Hb levels is fundamental in comprehending the health status of the subjects, and this histogram effectively visualizes the distribution pattern, setting the stage for further statistical analyses and insights into maternal well-being within the study. Further, [Figure 3] portrays a matrix plot illustrating the Spearman correlation analysis conducted between Hb levels and APGAR scores at 1 min for the study cohort. The Spearman correlation was employed due to the non-normal distribution of the data. The plot demonstrates a significant positive correlation between Hb levels and APGAR scores, with a correlation coefficient (r) of 0.546 (P< 0.001) indicates a high level of statistical significance observed between Hb levels and APGAR scores.
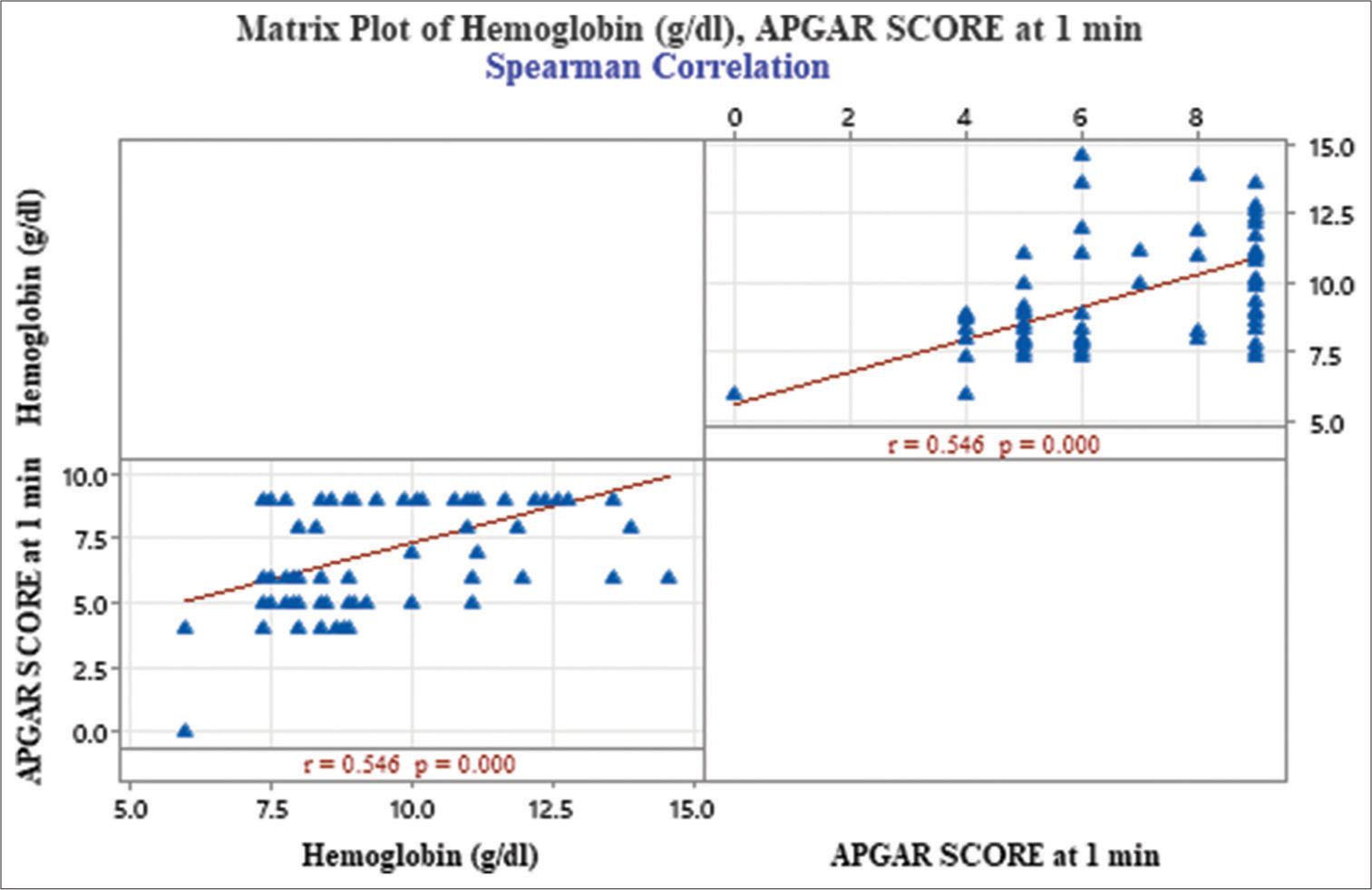
- Matrix plot illustrating spearman correlation between hemoglobin levels and APGAR scores at 1 min. (APGAR: Appearance, pulse, grimace, activity, and respiration, p=probability value, r=correlation coefficient.)
DISCUSSION
The correlation between a mother’s health during pregnancy and the immediate well-being of her newborn holds immense significance in the realm of obstetrics. This study delves into the intricate interplay between maternal anemia, a prevalent condition, and the initial neonatal health assessed through the APGAR score. It resembles a synchronized ballet – how the maternal health choreographs the baby’s inaugural moments. The study included 130 pregnant women out of which 52 were anemic (Hb < 11 g/dL) and 78 were non-anemic (Hb > 11 g/dL). The average APGAR score among the 130 newborns was approximately 7.238, indicating a satisfactory initial health status for most of the neonates. The findings highlight a substantial prevalence of maternal anemia (40%) in the study population, with moderate anemia being the most common severity. Despite this prevalence, no cases of very severe anemia were observed. Regarding immediate neonatal well-being, the majority of newborns demonstrated satisfactory APGAR scores at 1 min, implying a relatively healthy start in the extrauterine environment.
Maternal anemia is a major risk factor for adverse pregnancy outcomes. Comparing the groups of anemic and nonanemic mothers in our study revealed a compelling insight into the immediate well-being of their neonates. At the crucial 1-min mark, a striking 36.9% of neonates born to anemic mothers exhibited lower APGAR scores, signifying potential challenges in their early adaptation. This study results are similar to the findings of Preethi et al.[6] who concluded that at the critical 1-min mark, a notable 32% of infants born to anemic mothers showed lower APGAR scores, indicating potential hurdles in their initial adjustment to the outside world.
In this study, we observed a moderate positive correlation between maternal Hb levels and APGAR scores at 1 min, implying that higher maternal Hb levels are linked to improved immediate neonatal outcomes. Our study echoes the outcomes found in the research by Bano et al., which revealed a notable correlation between maternal anemia and significantly lower APGAR scores in neonates born to anemic mothers when compared to those born to non-anemic mothers.[7] This trend is reaffirmed by several other studies. For example, a study conducted by Ghimire et al., in Nepal emphasized anemia as a significant risk element for unfavorable outcomes in both mothers and neonates.[8] Particularly, neonates born to anemic mothers showed an increased likelihood of having low birth weight, a low APGAR score, being categorized as small for gestational age, experiencing intrauterine death, and encountering perinatal death. Despite variations in the anemia threshold (Hb <7 g/dL) in their study compared to ours (<11 g/dL) and a smaller sample size, their findings align with our observations regarding APGAR scores.
Likewise, Akhter et al., in Bangladesh, Batar et al., and Kaul et al., in their respective studies in Jummu city and New Delhi showcased similar connections between maternal anemia and birth weight, placental weight, and APGAR scores of neonates.[9-11] This body of evidence collectively emphasizes the consistent and pivotal impact of maternal anemia on neonatal health metrics across various populations and contexts. However, this finding contrasts with the study conducted by Lumbanraja et al., which reported no significant correlation between Hb concentration during pregnancy and low APGAR scores.[2]
The study found a higher prevalence of moderate anemia in pregnant women with cardiovascular disease, with a higher presence of mild anemia and lower absence of anemia. However, the difference was not statistically significant, highlighting the complexity of managing both conditions. In addition, the bidirectional relation of anemia and cardiovascular study had been established in a study done by Gan et al.,[12] which underscores the complexity of management of both conditions simultaneously.
The prevalence of anemia among pregnant women within our study population reveals a significant health concern. Our findings demonstrate a clear correlation between maternal Hb levels and immediate neonatal outcomes, emphasizing that higher maternal Hb levels are associated with better APGAR scores at 1 min. These insights underscore the critical importance of addressing maternal anemia and optimizing Hb levels during pregnancy to positively influence neonatal health and improve immediate postnatal outcomes.
Limitations
This study has limitations, including its retrospective design, which may introduce biases due to reliance on existing medical records, and its small sample size of 130 subjects. The study’s generalizability to broader populations is limited, and data availability constraints may overlook relevant variables or time periods. Confounding factors may still exist, and generalizing findings to other populations should be done cautiously considering demographic, cultural, and healthcare contexts. In addition, potential bias in Hb measurement across different settings may affect the observed associations between maternal anemia and neonatal outcomes.
CONCLUSION
Optimizing maternal Hb levels emerges as a crucial intervention point for ensuring a healthier start for the neonate. By addressing maternal anemia comprehensively through antenatal care and targeted interventions, we can strive to enhance both maternal and neonatal well-being, forging a path toward a healthier future for generations to come. It emphasizes the importance of routine antenatal screening for anemia and interventions to improve maternal Hb levels during pregnancy. These interventions may include nutritional supplementation, iron-fortified foods, and prenatal iron supplementation. Health-care providers can use this information to prioritize high-risk pregnancies and allocate resources effectively. Future research should focus on longitudinal studies and randomized controlled trials to evaluate the long-term impact of maternal anemia on neonatal health and development. Investigating the underlying mechanisms linking maternal Hb levels to neonatal outcomes can provide further insights into maternal-fetal health interactions. Integrating these findings into clinical practice guidelines and public health policies can help reduce maternal anemia burden and improve global neonatal health outcomes.
Acknowledgment
This paper has emerged out of the project entitled “Comparing the pregnancy outcomes in women with or without congenital or other heart diseases: A record based study” sponsored by Women in Cardiology and Related Sciences (WINCARS) under the scheme Prajwalika Scholarship Program.
Ethical approval
The research/study was approved by the Institutional Review Board at Shri Ram Murti Smarak Institute of Medical Sciences, Bareilly, Uttar Pradesh, India, number SRMS IMS/ECC/2023/07, dated 03-02-2023.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Audio summary available at
Financial support and sponsorship
Prajwalika Scholarship Program.
References
- Relationship between Maternal Hemoglobin Concentration and Neonatal Birth Weight. Hematology. 2011;16:373-6.
- [CrossRef] [PubMed] [Google Scholar]
- The Correlation between Hemoglobin Concentration during Pregnancy with the Maternal and Neonatal Outcome. Maced J Med Sci. 2019;7:594-8.
- [CrossRef] [PubMed] [Google Scholar]
- Anaemia Mukt Bharat. Available from: https://pib.gov.in/PressReleasePage.aspx?PRID=1795421 [Last accessed on 2023 Sep 27]
- [Google Scholar]
- Maternal Anaemia and Risk of Mortality: A Call for Action. Lancet Glob Health. 2018;6:e479-80.
- [CrossRef] [PubMed] [Google Scholar]
- Study on Relationship between Maternal Haemoglobin and the Early Neonatal Outcome in Term Babies. Int J Contemp Pediatr. 2019;6:1938.
- [CrossRef] [Google Scholar]
- A study of Maternal Anemia and Its Association between APGAR Score of Newborns with Anemic and Non-anemic Mothers at a Medical College Hospital. Res J Med Allied Health Sci. 2021;4:23-6.
- [Google Scholar]
- APGAR Score of Neonates Born to Anemic Mothers Versus Non-anemic Mothers. J Islamabad Med Dent Coll. 2018;7:246-9.
- [CrossRef] [Google Scholar]
- Maternal and Fetal Outcome Following Severe Anaemia in Pregnancy: Results from Nobel Medical College Teaching Hospital, Biratnagar, Nepal. J Nobel Med Coll. 2013;2:22-6.
- [CrossRef] [Google Scholar]
- Maternal Anemia and its Correlation with Iron status of Newborn. Birdem Med J. 2014;4:27-32.
- [CrossRef] [Google Scholar]
- Maternal and Perinatal Outcome of Pregnancy with Severe Anemia. Int J Biomed Adv Res. 2015;6:611-6.
- [Google Scholar]
- Maternal Haemoglobin and Perinatal Outcome in a Tertiary Care Hospital in Jammu City, India. Int J Reprod Contracept Obstet Gynecol. 2017;6:5060-6.
- [CrossRef] [Google Scholar]
- Causal Association between Anemia and Cardiovascular Disease: A 2-Sample Bidirectional Mendelian Randomization Study. J Am Heart Assoc. 2023;10:e029689.
- [CrossRef] [PubMed] [Google Scholar]








