Translate this page into:
Systolic Murmurs
M. Jyotsna, MD, DM, FACC, FESC, FICC Department of Cardiology, Nizam's Institute of Medical Sciences Punjagutta, Hyderabad, Telangana 500082 India janaswamyjyotsna@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Murmur is the vibration of heart components or great vessels. 1 Systolic murmurs are those murmurs that can be heard between S1 and S2.
Basics of Murmur
The turbulent flow generates murmurs, but the acoustic force generated by the turbulence is not sufficient to produce an audible sound on the chest wall.2 Brun proposed the concept of vortex shedding for the mechanism of generation of the murmurs. Vortices are produced from the diseased valves or great vessels. These vertices can be produced by increased flow with normal valves or great vessels. These vortices can produce sustained vibrations to generate audible murmur on the chest wall.
Another important factor for the generation of murmur along with turbulence is the velocity. In laminar flow, the velocity, as well as vortex shedding, is minimal. In increase flow conditions (e.g., increase cardiac output states), as velocity increases, the vortex shedding also increases. Even vortex shedding may increase with normal velocities if associated with additional areas of disruption of laminar flow. These vortices will determine the pitch of generated murmur. Vortices in downstream may coalesce and represent lower frequency than at the site of generation. It is always better to hear the sound at site of generation (e.g., at the site of stenosis), then in the downstream.
Technique of Auscultation
Auscultation should be done in a calm and quiet room with a stethoscope that is 25 to 30 cm long with the stiff diaphragm and shallow bell. Auscultation should be in lying, sitting, or standing, left lateral decubitus position, and after specific maneuvers. On chest, right second intercostal space (ICS) is called as aortic area, left third ICS is called as neoaortic area, left second ICS is called as pulmonary area, left fourth ICS is called as tricuspid area and at the cardiac apex as mitral area. Levine and Harvey recommended to do the auscultation from the mitral area and then move inch by inch to other areas.3 4 5
The areas to be auscultated other than above mentioned classical five areas are as follows:
-
The right parasternal region,
-
The right and left the base of the neck,
-
The right and left carotid arteries,
-
The left axilla,
-
The interscapular area.
Characteristics of the Systolic Murmur
-
Intensity (loudness)—Intensity of the systolic murmur is graded into six grades. Grade 1 refers to a murmur so faint that it can be heard only with special effort. A grade 2 murmur is faint but is immediately audible. Grade 3 refers to a moderately loud murmur and grade 4 to a murmur that is very loud and palpable. A grade 5 murmur is extremely loud and is audible with one edge of the stethoscope touching the chest wall. A grade 6 murmur is so loud that it is audible with the stethoscope just removed from contact with the chest wall.
-
Frequency (pitch)—Frequency of the murmurs mainly depends on the velocity of the blood flow. If velocity is high, then the pitch of the murmur increases. When blood flows from a high-pressure chamber (left ventricular, LV) to low-pressure chamber (left artery, LA) such as murmur due to mitral regurgitation (MR) will have high pitch due to high velocity. Murmur taking origin at the stenotic areas is of a low or medium pitched.
-
Quality—Quality depends upon the tone of the sound. The descriptions used to define quality are as follows:
-
Blowing—e.g., high-pitched murmur of MR,
-
Musical—e.g., functional or innocent murmurs; usually these are low or medium pitched murmurs,
-
Squeaking—e.g., aortic stenosis murmur. This is high pitched squeaking and whistling quality,
-
Whooping—e.g., late diastolic whoop in severe aortic regurgitation,
-
Honking—e.g., systolic murmur in ballooning mitral valve,
-
Harsh—e.g., these are usually high velocity murmur as in case atrial septal (AS) or pulmonary stenosis (PS) orventricular septal defect (VSD),
-
Rasping,
-
Grunting,
-
Rumbling—e.g., murmur of mitral stenosis.
Even though many descriptions are there to mention the quality of sound, none of them are characteristics of the particular disease. Many people may interchangeably use these words to describe the quality.
-
-
Duration—Systolic murmurs are classified depending upon a phase of systole, which is described detailed below.
-
Configuration—Shape of murmur is called a configuration of the murmur. It depends on the intensity and duration of the murmur. The descriptions used to describe the configuration of murmurs are as follows:
-
Crescendo,
-
Decrescendo,
-
Crescendo decrescendo,
-
Plateau,
-
-
Primary Location (point of maximum intensity)—The source of origin of murmur is determined by the site where the maximum murmur intensity is heard, even though the murmur may be heard throughout the chest.
-
Site(s) Of Radiation—Some murmurs radiate. The direction of the radiation may give information about the etiology of murmur.
Dynamic Auscultation
The physiologic maneuvers are as follows:
-
Respiration—Greater effect of the breathing is seen on the right side of the heart. Inspiration or Mueller's maneuver (forced inspiration on a closed glottis) causes increase in venous return right side of heart, so right side originated increase in murmurs with inspiration with good right ventricular function. Because of the pooling of blood in the low resistance pulmonary capacitance vessel during inspiration, the blood flow decreases to the left heart. The opposite occurs during expiration.
-
Standing—Standing causes decrease in venous return to the right side of heart first then to left side, whereas lying down increases venous return.
-
Sudden Squatting—Squatting causes decrease in the venous return to right heart and increase in the peripheral vascular resistance.
-
Isometric Hand Grip Exercise—The changes in the systemic circulation because of isometric handgrip exercise are as follows:
-
Increase in peripheral vascular resistance,
-
Increase in systemic blood pressure,
-
Increase in heart rate,
-
Increase in cardiac output,
-
Increase in LV volume,
-
Increase in LV filling pressure.
-
-
-
Valsalva Maneuver––Table 1 describes phases of the Valsalva, along with the physiological changes and their effects.
-
Passive Leg Rising—Venous return of the right side of the heart is increased by passive leg raising.
-
Post-Extrasystolic Pause—As there is an increase in the ventricular filling, a beat after an extrasystole myocardial contractility increases (according to Frank–Starling law).
-
Pharmacological Maneuvers—The pharmacological effects of below drugs are used to distinguish few of systolic murmurs etiology (Table 2).
|
Phase of Valsalva's maneuver |
Physiological changes |
Effect |
|---|---|---|
|
There is six to eight beats time delay for left-sided events than right-sided events. |
||
|
Phase 1 (initial phase) |
↑ Intrathoracic pressure |
↑ LV output |
|
Phase 2 (strain phase) |
↓Venous return |
↑ Heart rate ↓ Stroke volume ↓ Mean arterial pressure ↓ Pulse pressure |
|
Phase 3 (release phase) |
↑ Venous return |
– |
|
Phase 4 (over stood phase) |
– |
The normalization of features of phase 2 |
|
Drug |
Route of administration |
Dose |
Duration |
Pharmacological changes |
|---|---|---|---|---|
|
Amyl nitrite |
Inhalation |
– |
10–15 sec |
↓ Peripheral vascular resistance ↑ Stroke volume ↑Venous return |
|
Phenylephrine |
Intravenous |
0.5 mg |
– |
↑ Systolic blood pressure for 3–5 min Reflex bradycardia ↓ Myocardial contractility |
|
Methoxamine |
Intravenous |
3–5 mg |
– |
↑Systolic blood pressure by 20–40 mm Hg for 10–20 min Reflex bradycardia ↓ Myocardial contractility |
Systolic Murmurs—Source of Origin
Many involve stenosis of the semilunar valves or regurgitation of the atrioventricular valves. All systolic murmurs are more prominent in the presence of pregnancy, fever, anemia, or thyrotoxicosis.
Pictogram of the systolic murmurs is in Fig. 1.
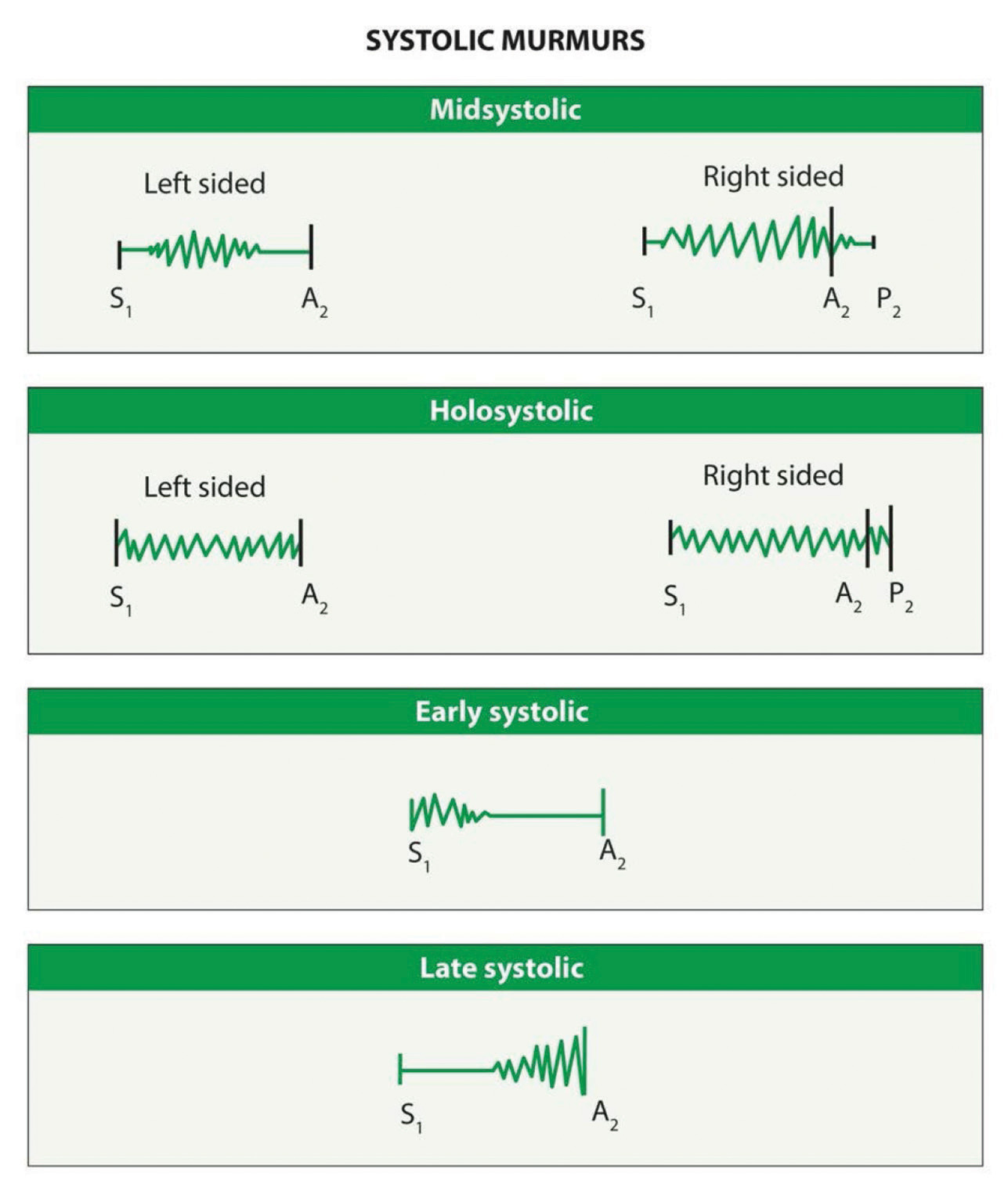
-
Fig. 1 Systolic murmurs.
Fig. 1 Systolic murmurs.
Classification of Systolic Murmurs
I) Already mentioned previously that systolic murmurs can be classified depending on the phase of systole.
-
Early Systolic Murmur—Starts with S1, peaks in early systole. Causes of early systolic murmurs are as follows:
-
Small VSD,
-
VSD with high pulmonary vascular resistance,
-
An innocent murmur of childhood,
-
Acute MR,
-
Normal-pressure TR,
-
Organic TR,
-
-
MidSystolic Murmur—Midsystolic ejection murmurs are generated across the semilunar valves. This murmur starts at the time of ejection, which is after S1 and ends with the cessation of blood flow means before S2. As this murmur is because of ejection of the blood from ventricles to corresponding great arteries, this murmur takes crescendo–decrescendo shape. So, the sequences of events are S1, isovolumetric contraction period, then ejection systolic murmurs, hangout interval, and lastly S2. The short crescendo about midsystole is an invariable feature of all ejection murmurs.3
Causes of midsystolic ejection murmurs include:
-
Outflow obstruction (aortic stenosis, pulmonic stenosis, hypertrophic obstructive cardiomyopathy [HOCM]),
-
Increased flow through normal semilunar valves (atrial septal defects),
-
Dilation of the aortic root or pulmonary trunk,
-
Diseased semilunar valves without obstruction.
-
-
Late Systolic Murmur—Late systolic murmurs (LSM) are crescendo in nature and start after S1 and, if left sided, extend up to S2.
Causes of LSM are as follows:
-
Mitral valve prolapse (MVP),
-
Tricuspid valve prolapse,
-
Papillary muscle dysfunction.
-
-
Holo Or Pansystolic Murmur—This murmur starts with S1 and ends at S2, so both heart sounds may be difficult to hear. Thought out systole the intensity of the murmur is constant or may increase in late systole.
-
MR,
-
Tricuspid regurgitation (TR),
-
VSD,
-
-
II) Another classification depends on the quality of murmur.
-
Ejection Murmurs—Ejection murmurs emanate from the semilunar valves or surrounding structures (i.e., the aortic or pulmonic root).
-
Regurgitant Murmurs—Regurgitant murmurs are created when blood flows from a high-pressure “donor” chamber to a low-pressure “recipient” chamber.
-
Extracardiac Sounds—Extracardiac sounds simulate systolic heart murmurs.
-
III) Another classification is functional or organic.
Always regurgitation murmurs are organic. Ejection systolic murmurs may be organic or functional.
1. Functional Systolic—These murmurs occur without underlying heart diseases. Functional systolic murmurs are heard in healthy individuals, especially in children or in high cardiac output states or during pregnancy. These murmurs may vary in intensity and duration at different periods. They usually get exaggerated during exercise and fear. Most of these innocent murmurs may disappear as a child grows, but it may persist in a few patients.6
These murmurs are of shorter duration with a frequency of 120 to 250Hz. They are best heard in left second ICS and increases with inspiration, and can be heard either with bell or diaphragm of the stethoscope (Fig. 2).
-
Fig. 2 Innocent murmur phonocardiogram.
Fig. 2 Innocent murmur phonocardiogram.
The causes of innocent murmurs are (details are mentioned in extracardiac sounds mimicking systolic murmurs) as follows:3
-
Still's murmur: The most common innocent murmur is the still's murmur which is characterized by medium pitched, nonradiating mid systolic short ejection murmur due to vibration of the pulmonary valve. This murmur is best heard along the left upper sternal border.
-
Pulmonary mid systolic murmur: This functional systolic murmur takes origin from the route of the pulmonary artery and may be heard in normal individuals. This differs from the still’s murmur by high pitch blowing quality.
-
Peripheral pulmonary systolic murmur
-
Supraclavicular or brachiocephalic systolic murmur
-
Systolic mammary souffle
-
Functional systolic murmur due to semilunar valve regurgitation: Aortic regurgitation (AR) or pulmonary regurgitation (PR) can produce functional systolic murmurs as forward flow increases. These murmurs start in early systole and peaks in mid systole with variable intensity, and are heard at aortic and pulmonary areas, respectively, without any radiation of the murmur. Usually, functional systolic murmurs grade is 1 to 3, occasionally, as in case of severe AR, systolic thrill (grade 4 murmurs) may be felt at the aortic area without associated aortic stenosis. Especially the thrill is more frequent in severe AR cases when it associated with an aneurysm.3
-
Aortic sclerosis—This is a common cause of midsystolic murmur in the elderly.
It is a type of functional murmur due to turbulent flow across the sclerotic aortic valve without abstraction; typically, it is a midsystolic murmur with musical or cooing quality.
2. Organic—Organic systolic murmurs evolve from structural abnormalities in the heart or great vessels.
-
Ejection Murmurs—Organic systolic ejection murmurs are due to:
-
Valvular aortic stenosis,
-
Aortic sclerosis,
-
Supravalvular aortic stenosis,
-
Subvalvular aortic stenosis,
-
HOCM,
-
Valvular pulmonic stenosis,
-
Pulmonary infundibular stenosis,
-
Atrial septal defect,
-
Tetralogy of Fallot (TOF).
-
Aortic Stenosis
a. Valvular Aortic Stenosis—The valvular AS causes are rheumatic, congenital—bicuspid or unicuspid, myxoid dysplasia, calcific degenerative, hyperlipidemia, Fabry's disease, infective endocarditis, and ochronosis. The murmur of AS is usually diamond shape with a low or medium pitch with harsh quality. It is best heard at the aortic/neoaortic area but heard throughout the chest and even radiate to the carotids. The murmur intensity increases with:
-
Sudden squatting,
-
Post-extrasystolic pass,
-
Release phase of Valsalva,
-
Passive leg rising,
-
After amyl nitrate administration.
The murmur intensity decreases with:
-
Phase 2 Valsalva,
-
Isometric handgrip,
-
The IV administration ofα-adrenergic agonists.
Characters of A2 in aortic stenosis3:
-
As the severity of the aortic stenosis increases, decrease in the intensity of the A2 occurs along with delay.
-
Always murmur of AS ends before the first component of the second heart sound (A2).
-
Even in left bundle branch block (LBBB) even though the reversal of second heart sound occurs (P2 earlier than A2), the murmur ends before A2.
-
In some cases of severe AS, A2 may completely become soft or absent and then there is difficulty in recognition of the pattern of the murmur.
-
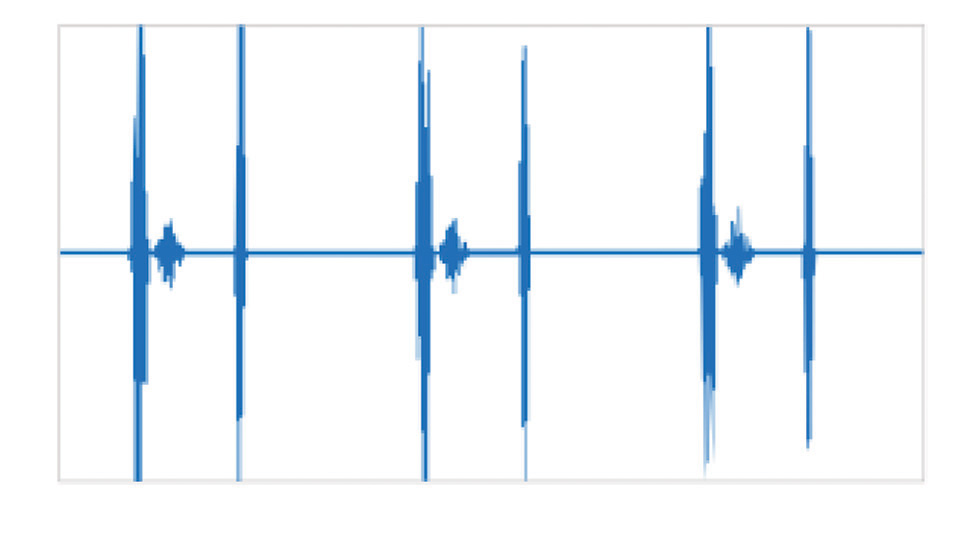
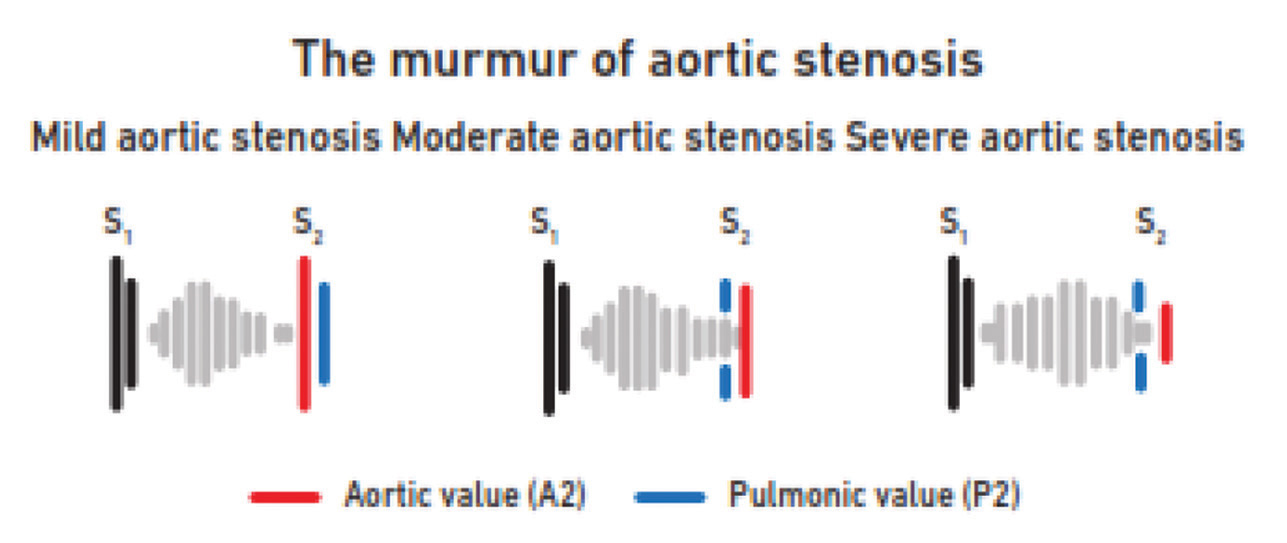
Mild aortic stenosis—In mild AS, the murmur is of mid-frequency, and the A2 may be louder than normal (Fig. 3).
-
Fig. 3 Mild aortic sclerosis.
Fig. 3 Mild aortic sclerosis.
In calcific AS, even though the source of origin of the murmur is from the flow across the aortic valve, it may be heard as two different murmurs. At base it is heard as low frequency But heard as a systolic murmur with musical quality at apex. Hearing two different qualities of the same murmur at different sites is called “Gallavardin phenomenon.”
The points to distinguish systolic murmur at apex due to MR vs. due to AS in case of Gallavardin phenomenon are as follows:
-
In AS, the murmur ends before the S2, whereas in MR it extends up to S2.
-
The AS murmur at apex may be as loud as or louder than the aortic area with ejection quality.
-
Dynamic auscultation distinguishes AS from MR as mentioned above.
Hourglass conduction—Hourglass conduction represents change in the intensity of the murmur. Softer murmur is heard at base, but intensity of murmur increases from aortic to mitral area.
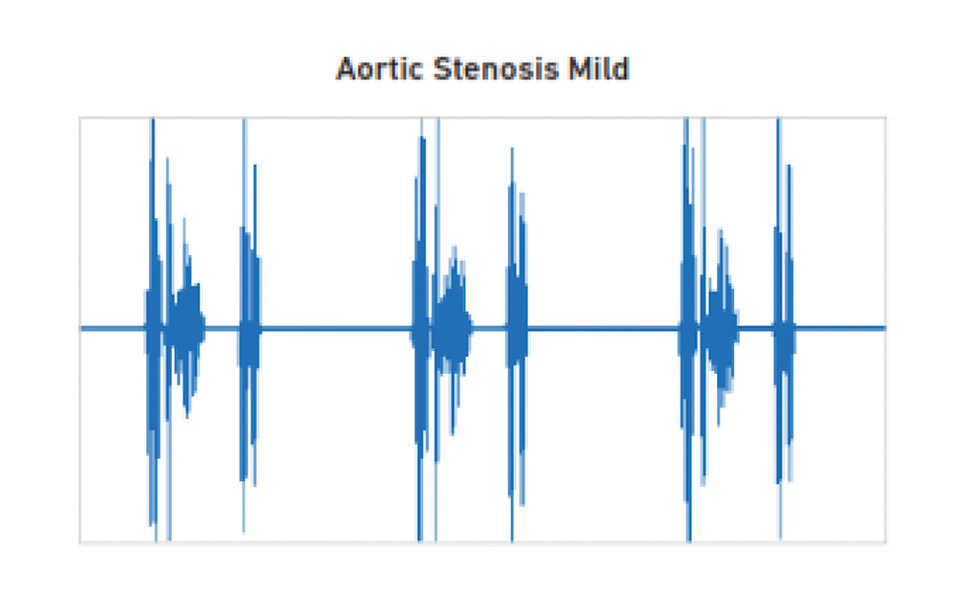
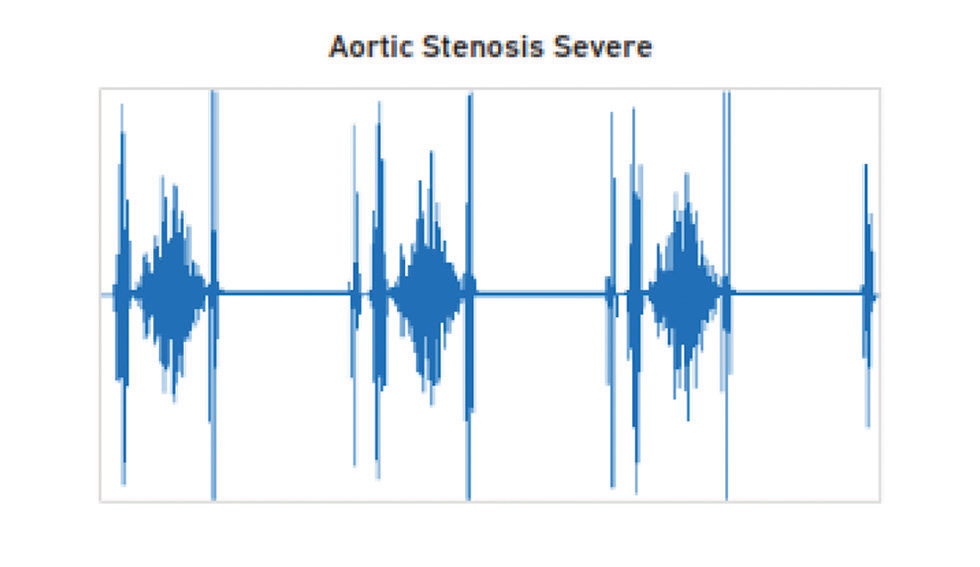
The severity of AS is known by (Fig. 4 5):
-
Fig. 4 Severe aortic stenosis phonocardiogram.
Fig. 4 Severe aortic stenosis phonocardiogram.
-
Fig. 5 The murmur of aortic stenosis.
Fig. 5 The murmur of aortic stenosis.
-
The shape (peaking) of the murmur—Early peaking of the ejection systolic murmur is the feature of mild AS and late peaking in severe AS.
-
Delayed aortic valve closure or paradoxically split S2 also indicated the severe AS. In calcific AS, A2 becomes soft.
-
The intensity of the murmur does not always reflect the severity of AS. When there is a significant decrease in the flow either due to LV dysfunction due to severe AS or associated severe MR, then the intensity of murmur decreases. When the patient has associated emphysema as conduction through the chest wall is decreased, murmur intensity may not be picked up.
-
Delayed carotid upstroke—The best clinical sign to detect the severity of AS.
Importance of the ejection click:
-
Presence of the ejection click localizes the level of obstruction to the valve as in bicuspid aortic valve.
-
Presence of click says that valve is mobile.
-
Presence of click mitigates against severe stenosis.
The time of onset of murmur: It depends on the3:
-
The time of onset of ejection—When diastolic pressure of the aorta is low as in the case of severe AR, then ejection starts quite early and murmur of associated AS starts early. When the diastolic pressure of aorta is high as in the case of LV dysfunction, then ejection will be delayed, and the murmur of the AS starts late.
-
Rate of ejection—With hyperdynamic ventricle ejection starts early, so murmur starts early.
Functional ejection systolic murmur due to severe AR is already described in functional murmurs.
Ejection midsystolic murmurs of a soft nature may be heard in the acute rheumatic fever due to valvulitis, but caution should be taken to diagnose valvulitis in the acute phase of a rheumatic fever unless the patient has associated AR murmur.
b. Subaortic Stenosis—Subaortic stenosis may be dynamic as in HOCM, discrete membranous type or tunnel aortic stenosis. Clinically the murmur of subaortic stenosis is similar to vulvar aortic stenosis. Mainly the destination between the two murmurs is the other associated features like an absence of the click and absence of dilation of ascending aorta of chest X-ray.
c. Supravalvular Aortic Stenosis
Causes of supravalvular aortic stenosis are:
-
Congenital aortic abnormalities (Hourglass type, diffuse or membranous type).
-
Aortic dissection.
-
Homozygous type 2 hyperlipidemia.
-
Healing aortotomy site.
-
Rubella.
-
Features to distinguish systolic murmur of supravalvular stenosis from the ejection systolic murmur of aortic stenosis are:
-
Best heard only in the primary aortic area with radiation to both the carotids.
-
No Gallavardin phenomena.
-
The amplitude of brachial and carotid pulses is more on the right side than on the left. This difference is due to the direction of the jet of the blood towards right bracho cephalic artery.
-
Ejection click is absent.
-
Williams syndrome features like elfin faces.
Hypertrophic Cardiomyopathy (Table 3)
|
Effect on the loudness of the murmur |
Maneuver |
||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Phase of Valsalva’s |
Standing |
Post-extrasystole |
Amyl nitrate inhalation |
Recumbency |
Passive leg rising |
Squatting |
Isometric handgrip |
IV α-adrenergic drug |
|
|
Abbreviations: HOCM, hypertrophic obstructive cardiomyopathy; MR, mitral regurgitation; MVP, mitral valve prolapse; PS, pulmonary stenosis; TR, tricuspid regurgitation; VSD, ventricular septal defect. aIn this case, not only the murmur increases the intensity but also starts earlier systole, and midsystolic click moves closer to the S1. |
|||||||||
|
HOCM |
Phase 2 ↑ |
↑ |
↑ |
↑ |
↓ |
↓ |
↓ |
↓ |
↓ |
|
PS valvular |
Phase 3 ↑ |
↑ |
↑ |
↑ |
|||||
|
MR |
↓ |
↑ |
↑ |
↑ |
|||||
|
MVP |
Phase 2 ↑a |
↑ a |
↓ |
↑ a |
↓ |
↓ |
↓ |
↓ |
↓ |
|
TR |
↓ |
↑ |
↑ |
↑ |
|||||
|
Small VSD |
↓ |
→ or ↑ |
|||||||
The murmur of HOCM is similar to the aortic stenosis murmur in its diamond shape (crescendo and decrescendo). Other associated features of HOCM murmur are as follows:
-
Presence of S4,
-
Bisferiens pulse,
-
Double or triple apical impulse,
-
Occasional thrill along the left sternal border.
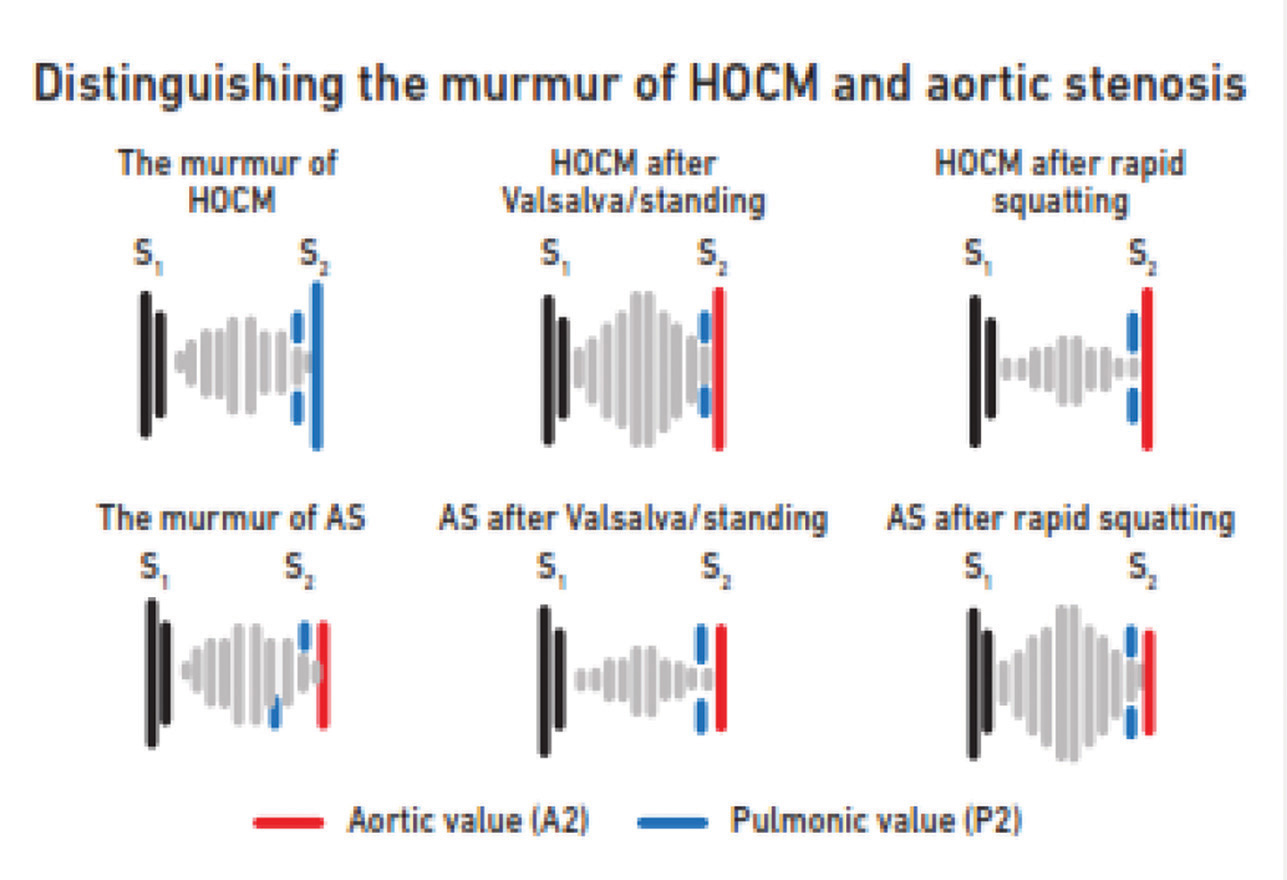
The murmur of HOCM differs from the aortic valve stenosis by:
-
Best heard along the left sternal border.
-
Less harsh.
-
Even though it is medium pitched, it is higher-pitched than the aortic stenosis murmur.
-
There is no radiation of this murmur to carotids.
-
Dynamic auscultation is useful (Fig. 6).
-
Fig. 6 Distinguishing the murmur of hypertrophic obstructive cardiomyopathy (HOCM) and aortic stenosis (AS).
Fig. 6 Distinguishing the murmur of hypertrophic obstructive cardiomyopathy (HOCM) and aortic stenosis (AS).
Site of Best Audibility of the Murmur and Its Significance in Aortic Stenosis
-
Best audible at right second space, conducted in right carotid—Valvular noncalcific AS.
-
Best audible in the left sternal border, no carotid conduction—Subvalvular AS, calcific AS, mistaken VSD, mistaken MR.
-
Carotid murmur with or without right second space murmur—Supravalvular AS, carotid stenosis.
-
Audible only at the apex—calcific AS in elderly with emphysema, mistaken for MR.
Pulmonary Stenosis (Table 3)
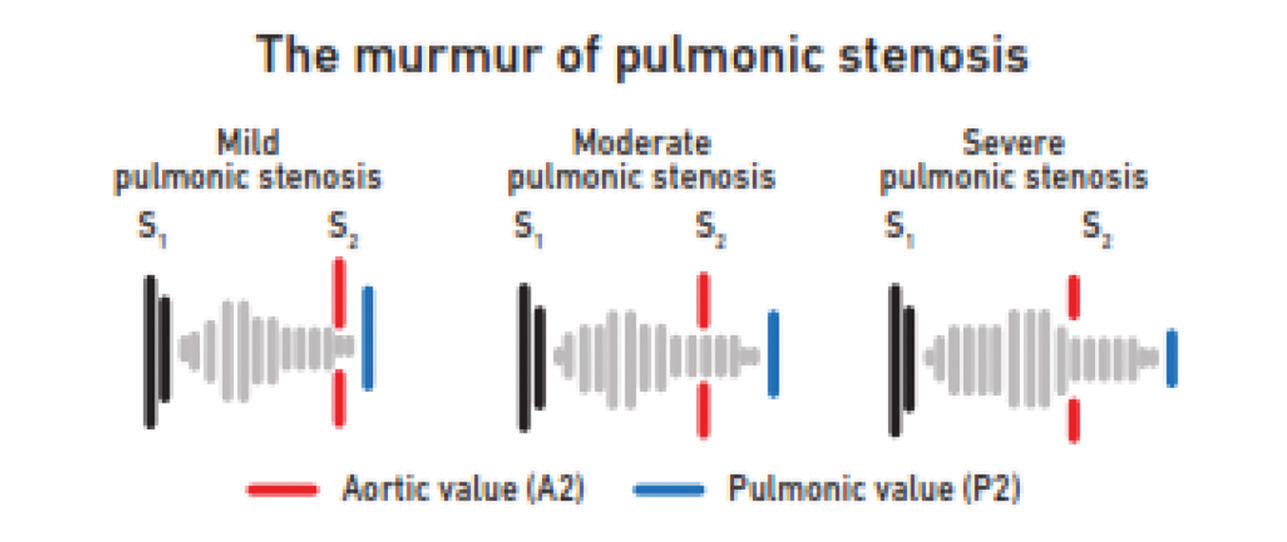
PS murmur is a harsh murmur, best heard in the pulmonary area with thrill and radiation to the supraclavicular area and left neck. It starts with S1 and ends before P2 can overlap A2. Because of the harsh quality, it may mimic VSD murmur, but S2 is normal in VSD, whereas it is wide split in PS. With severe PS, P2 becomes soft due to decreased mobility of valve leaflets (Fig. 7). These patients may have syndromic associations.
-
Fig. 7 The murmur of pulmonary stenosis.
Fig. 7 The murmur of pulmonary stenosis.
Pulmonary valvular stenosis murmur stimulates that of aortic stenosis in:
-
Diamond shape,
-
Late systolic peaking as severity increasing,
-
Quality.
The murmur of PS simulates that of AS. Distinguishing features are as follows:
-
PS murmur does not radiate as widely as AS murmur.
-
PS increases with inspiration with good RV function.
-
AS murmur extends up to A2, PS murmur overlaps A2 and extends up to P2.
Infundibular Pulmonary Stenosis
The causes of subvalvular stenosis are congenital (infundibular stenosis, double-chambered RV, neoplasm, and thrombus). Infundibular stenosis constitutes 10% cases of right ventricular outflow tract (RVOT) obstruction, either it could be an isolated anomaly or associated with VSD. It differs from valvular PS murmur as it is heard best in the third left ICS and absent pulmonary valvular click.
SupraValvular PS—Causes of supravalvular PS are congenital, tumor compression, thrombus, rubella.
Site of the Murmur Best Audibility and Its Significance
-
Left second space—valvular PS,
-
Infraclavicular and away from midline—supravalvular PS,
-
Left third or fourth space—infundibular PS or double chambered RV,
-
Right second or third space—PS with transposition of the great arteries (TGA),
-
Conduction to the left side of neck—valvular PS,
-
Failure to conduction to the left side—valvular PS is less likely, VSD, or infundibular PS is likely.
Atrial Septal Defect
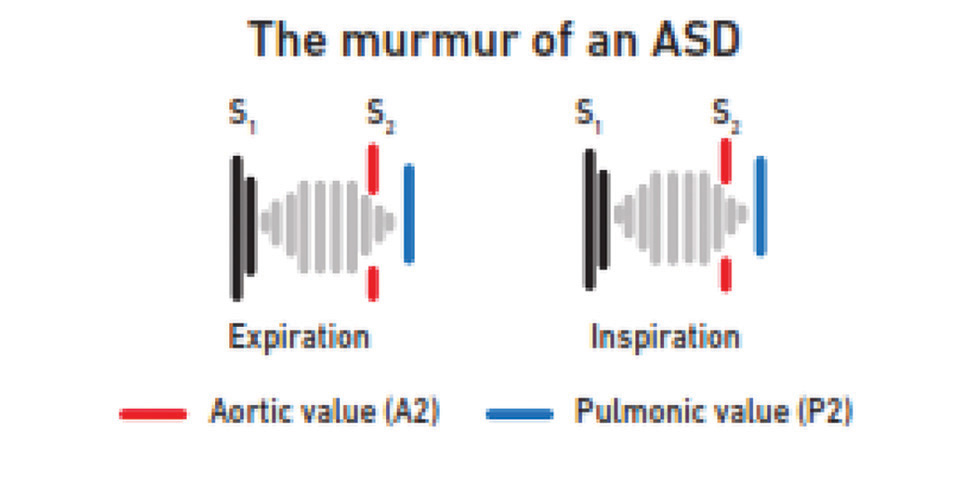
The systolic murmur in ASD is due to increase in blood flow across the RVOT. So, it has similar characters as functional pulmonary flow murmur as described above. Associated wide fixed split S2 in ASD differentiates from the functional murmur. Fixity of widened S2 split with accentuated P2 with pulmonary hypertension distinguishes from PS, wherein S2 is wide, but not fixed, and P2 become soft (Fig. 8).
-
Fig. 8 The murmur of atrial septal defect (ASD).
Fig. 8 The murmur of atrial septal defect (ASD).
Tetrology of Fallot
The source of origin of systolic murmur in TOF is:
-
From RVOT if RVOT stenosis is moderate to severe.
-
From VSD when RVOT obstruction is mild.
TOF with mild PS:
-
Grade 4, harsh, mid systolic murmur,
-
Diamond-shaped,
-
Heard all over the precordium,
-
Peaks in late systole,
-
Delayed and diminished P2.
TOF with severe PS:
-
Progressively peaks in early systole,
-
Single S2.
B. Regugitant Murmurs
-
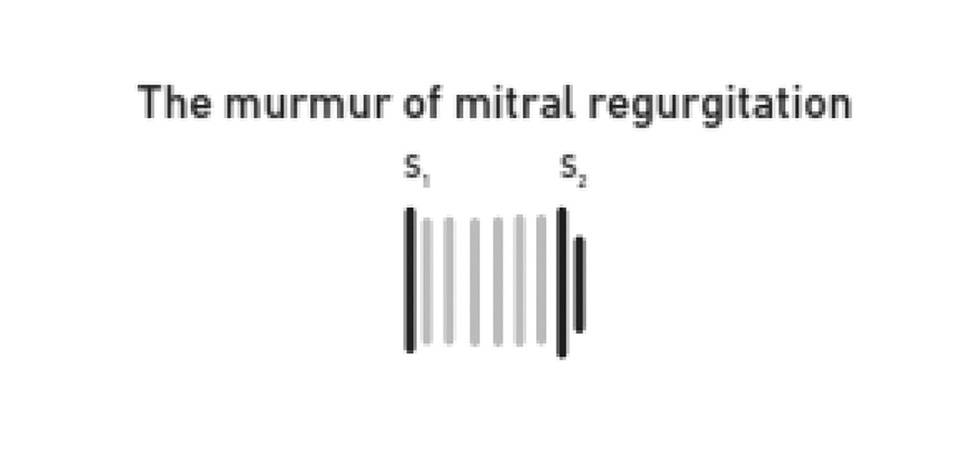
MR (Table 3)—MR may be due to rheumatic, papillary muscle dysfunction, acute MR, and MVP. The murmur of rheumatic mitral valve regurgitation is high pitched, blowing, and best heard at the cardiac apex with the diaphragm in left lateral position with radiation to the axilla. Usually, MR murmur radiates to the axilla, but it radiates to the base of the heart (upper left sternal boarder) in an anteriorly directed MR jet. It is holosystolic murmur that does not vary with inspiration. MR murmur starts with S1, at the onset of isovolumetric contraction itself (which corresponds with S1); the LV pressures are more than LA pressures. As the pressure difference between LV and LA persists though out the systole and even after aortic valve closure, the murmur can draw S2.
The murmur has a uniform intensity throughout systole giving the plateau feature to the murmur, but occasionally late systolic accentuation may occur. S3 is commonly heard (Fig. 9).
-
Fig. 9 The murmur of mitral regurgitation.
Fig. 9 The murmur of mitral regurgitation.
Castex murmur—Castex murmur of MR shows the associated LV dysfunction due to severe MR. In severe MR, the LV function is known by the type of LV apex (hyperdynamic with good LV function vs. sustained with LV dysfunction).7
MR murmurs may vary depending on the etiology. MR due to papillary dysfunction differs from that of rheumatic etiology. It may have cooing quality, high pitched, diamond shape, nonradiating murmur, best heard along the left sternal border, instead at apex. Usually the intensity of this murmur is < grade 4. Sometimes even MR due to dilated cardiomyopathy may also be simulated like this murmur.
Acute mitral valve regurgitation—Acute MR may be due to:
-
Chordae tendineae rupture,
-
Papillary muscle rupture,
-
Infective endocarditis,
-
Trauma.
Description of the murmur of acute MR:
-
Decrescendo,
-
Variable intensity (> grade 3),
-
May terminate before the A2,
-
Lower pitch than rheumatic MR,
-
May have harsh quality mimicking AS murmur,
-
Other qualities are similar to that of rheumatic MR, like best heard at the cardiac apex, which radiates to the axilla
It differs from TR murmur by:
-
Best site of audibility,
-
Effect of inspiration.
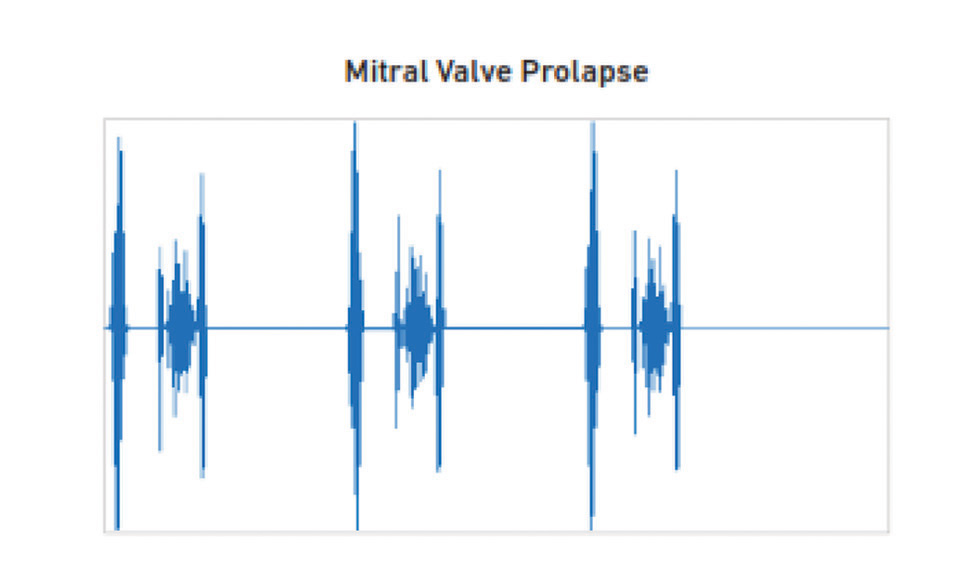
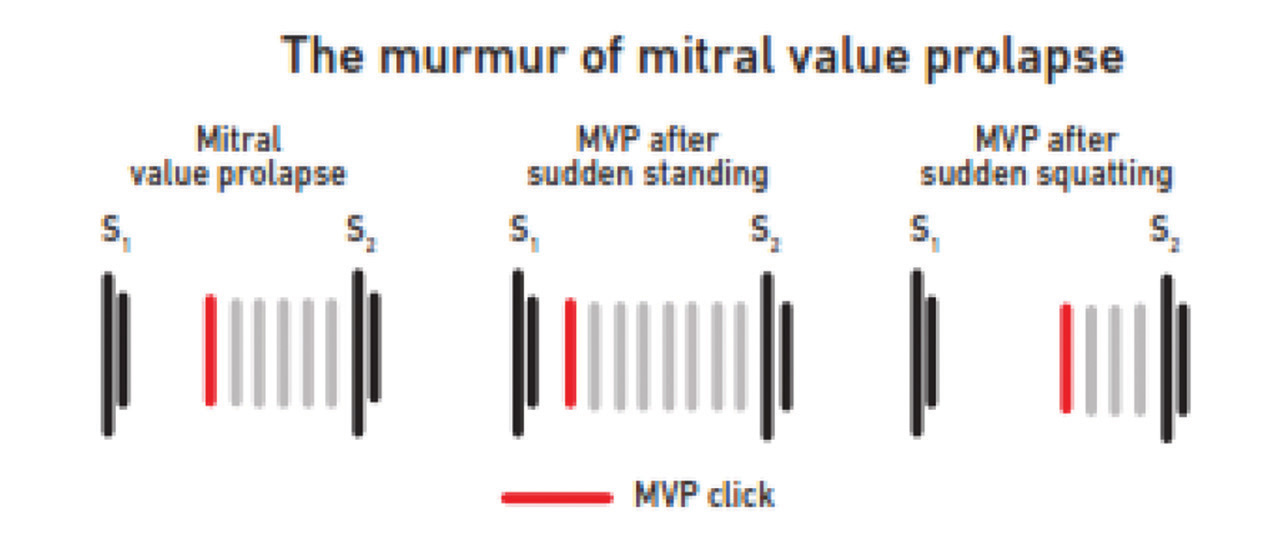
Mitral Valve Prolapse (Table 3)
Medium pitched crescendo LSM with mid systolic click exemplifies the classical MVP murmur. It best heard at the apex and no radiation (Fig. 10).
-
Fig. 10 Mitral valve prolapse phonocardiogram.
Fig. 10 Mitral valve prolapse phonocardiogram.
Variation in the murmur of MVP
-
May be holosystolic (either spontaneously or following maneuvers to decrease LV volume) (Fig. 11).
-
Even though the murmur duration becomes holosystolic, the medium pitch quality persists. When the intensity of the murmur increases to grade 5 or 6, then whooping or honking quality may impart.
-
It may radiate to the axilla.
-
Fig. 11 The murmur of mitral valve prolapse (MVP).
Fig. 11 The murmur of mitral valve prolapse (MVP).
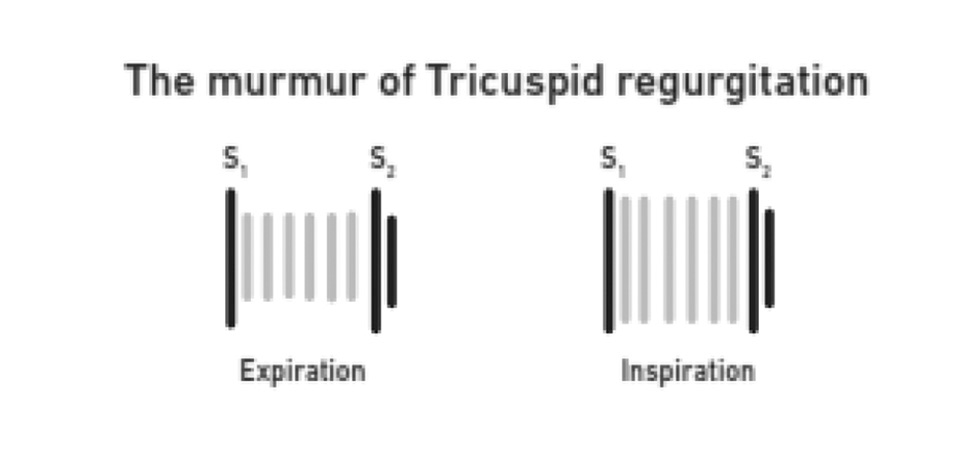
Tricuspid Regurgitation (Table 3)
Causes of TR are congenital (domed, tricuspid, bicuspid, unicommissural, hypoplastic annulus, dysplastic), carcinoid, and rheumatic. It is high pitched, blowing, pan systolic plateau, nonradiating murmur. It is best heard in the lower left sternal boarder; sometimes radiation may occur to the right sternal boarder. Inspiratory increase in the intensity of murmur is called Carvallo's sign.
The severe TR is characterized by:
-
Intensity of murmur,
-
RV S3,
-
cv wave in jugular venous pressure
-
Systolic pulsatile liver.
Variation from the routine features of TR:
-
RV failure—no respiratory variation.
-
TR due to pulmonary arterial hypertension (PAH)—pulmonary ejection click is present.
-
In RV enlargement, murmur may be heard leftward.
The murmur of tricuspid valve regurgitation is typically a high-pitched, blowing, holosystolic, plateau, nonradiating murmur best heard at the lower left sternal border. It may radiate to the right lower sternal border (Fig. 12).
-
Fig 12 The murmur of tricuspid regurgitation.
Fig 12 The murmur of tricuspid regurgitation.
The murmur of acute TR may be due to infective endocarditis or trauma. It is a decrescendo murmur and ends before S2.
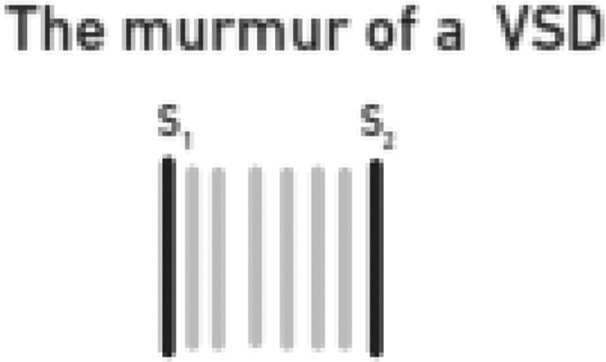
Ventricular Septal Defect (Table 3 Fig. 13)
-
Fig. 13 The murmur of ventricular septal defect (VSD).
Fig. 13 The murmur of ventricular septal defect (VSD).
The murmur of small VSD (Roger's type):
-
Low to medium pitched,
-
Holosystolic,
-
Midsystolic accentuation,
-
Best heard in the left third and fourth ICS along the left sternal border,
-
≥ Grade 3.
Large VSD with severe PAH (Eisenmenger complex):
-
Systolic murmur disappears,
-
May have medium pitched mid systolic murmur due to dilated aorta,
-
Signs of PAH (loud P2, pulmonary ejection click, pulmonary reregistration—Graham steel murmur, right side Austin Flint murmur).
Small, slit-like VSDs typically produce an early systolic murmur that ends during the early portion of mid systole. The pressure gradient between LV and RV is present throughout the systole, creating turbulent blood flow and a holosystolic murmur heard best at “Erb's point in small VSD.” The loudness of the murmur is dependent on the size of the VSD. Smaller the VSD, louder the murmur.
Extracardiac Sounds
Some extracardiac sounds mimic like systolic murmurs. These are as follows:
-
Innocent subclavian murmur—commonly heard in children. This murmur has crescendo–decrescendo shape, medium or high pitch, for short duration, either in early or midsystole. As the source of origin of the murmur is from the brachiocephalic artery, it is best heard in the same region and may hear at aortic and pulmonary area also. Also, disappears by pressure on the artery or hyperextension of the ipsilateral shoulder.
-
Carotid murmurs—best heard on the carotids, diminutively may be heard at the aortic or pulmonary area.
-
Internal mammary souffle—In a pregnant lady, along the sternal borders soft, high pitched, early to midsystolic murmur is due to an increase in the flow of internal mammary artery.
-
Coarctation of the aorta—Increase in flow across the stenotic segment of aorta produces medium to high pitched, late peaking systolic murmur, best heard in the interscapular area. This murmur may be heard faintly at aortic area also.
-
Murmurs associated with a dilated aortic or pulmonic trunk.
-
Patent ductus arteriosus (PDA) associated with pulmonary hypertension—Normal continuous murmur of PDA briefs first in diastole than even systole as the severity of pulmonary hypertension increases. In Eisenmenger PDA, there may systolic flow murmur due to a dilated pulmonary artery.
Conflict of Interest
None.
References
- Systolic murmurs.Clinical Methods: The History, Physical, and Laboratory Examinations. (3rd edition.). 1990. 1990. In: eds. Chapter 26. ISBN-10: 0–409–90077- X. Available from: Copyright © 1990, Butterworth Publishers, a division of Reed Publishing
- [Publisher] [Google Scholar]
- A general theory of the causes of murmurs in the cardiovascular system. Am J Med. 1959;27:360-374.
- [Google Scholar]
- Auscultation of the heart.The Heart, Arteries, and Veins. (6th edition.). New York: McGraw-Hill; 1986. In: eds.
- [Google Scholar]
- “Techniques - Heart Sounds & Murmurs Exam - Physical Diagnosis Skills - University of Washington School of Medicine.” Retrieved 2009–03–06. LINK:
- [Publisher]






