Translate this page into:
Syncope
Lalita Nemani, MD, DM, FESC Department of Cardiology, Nizam's Institute of Medical Sciences (NIMS) Punjagutta 500082, Hyderabad India drlalita775@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Definition
Syncope refers to loss of consciousness (LOC) associated with loss of postural tone that is sudden in onset, transient, is followed by spontaneous recovery,1 2 and is with no residual neurologic deficit. Premonitory symptoms such as light-headedness, nausea, yawning, or sweating are common. Most causes of syncope are benign except in a small subset of a population where it presages a life-threatening event. The word pre-syncope is often used to describe the occurrence of premonitory symptoms of syncope but without LOC.
Epidemiology
Syncope is relatively common. It affects 3% of men and 3.5% of women at some point in life. Elderly are more commonly affected, especially aged > 75 years (6%). However, any age can be affected with syncope in the presence or absence of other medical problems. Young adults commonly have non-cardiac causes whereas cardiac syncope is more frequent with advancing age. Syncope in pediatric populations is rare and warrants prompt, detailed evaluation.
Pathophysiology
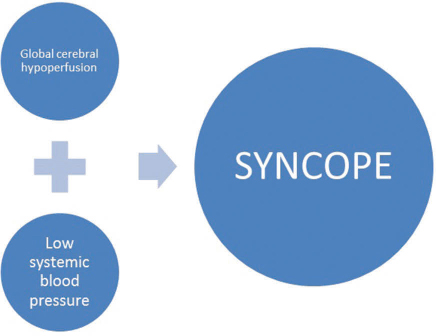
Normal blood flow to the brain is 50 to 65 mL/100 g of brain tissue with a total flow of 750 to 900 mL/min approximately, which is 15% of cardiac output and only 2% of body weight. Syncope results from global cerebral hypoperfusion and low systemic blood pressure (BP)3 4 (Fig. 1).
-
Fig. 1 Pathophysiology of syncope.
Fig. 1 Pathophysiology of syncope.
-
Cerebral hypoperfusion: Glucose is the primary metabolic substrate for the brain. The brain cannot store energy. It requires contrast blood flow for its supply of glucose. Cessation of cerebral hypoperfusion for just 6 to 8 seconds can result in syncope.5 6 Thus syncope can be due to cerebral hypoperfusion or reduction in energy substrates to the brain. Reduction in energy substrates is usually in the form of hypoxia (PO2 < 60 mm Hg) and hypoglycemia (mean plasma glucose < 40 mg/dL). When more than one factor is involved, an even lesser degree of abnormality can result in syncope.
-
Systemic BP is the product of cardiac out and total peripheral resistance. A drop in either can result in syncope. A systolic BP (SBP) of 50 to 60 mm Hg at heart level, or 30 to 45 mm Hg at brain level,5 6 especially in the upright position will cause LOC.

-
Fig. 2 Etiology of low cardiac output resulting in syncope. AS, ankylosing spondylitis; HOCM, hypertrophic obstructive cardiomyopathy; PH, pulmonary hypertension; PTE, pulmonary thromboendarterectomy.
Fig. 2 Etiology of low cardiac output resulting in syncope. AS, ankylosing spondylitis; HOCM, hypertrophic obstructive cardiomyopathy; PH, pulmonary hypertension; PTE, pulmonary thromboendarterectomy.
-
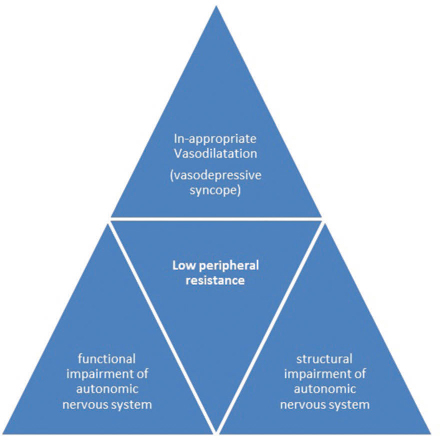
Fig. 3 Etiology of low peripheral resistance resulting in syncope.
Fig. 3 Etiology of low peripheral resistance resulting in syncope.
It is important to realize that more than one mechanism may be operational in the production of syncope. In a case of vasovagal syncope, both cardioinhibitory mechanism causing bradycardia and vasodepressor component causing inappropriate vasodilatation are seen resulting in a steep fall in central aortic pressure and global hypoperfusion of the brain culminating into syncope.
Etiology
Syncope is most commonly caused by conditions that do not directly involve the heart. The most significant single cause of syncope is “unknown causes” in 43% followed by reflex mediated (especially vasovagal) in 37%, cardiac in 13%, neurologic in 5%, and metabolic/drugs in 3% (Table 1).
|
1. Reflex syncope (neurally mediated) |
|
a. Vasovagal |
|
i. Orthostatic |
|
ii. Emotional |
|
b. Situational |
|
i. Coughing (cough syncope) |
|
ii. Micturition (micturition syncope) |
|
iii. Defecation |
|
iv. Postprandial |
|
v. Miscellaneous—sudden laughter, weight lifting, instrument playing |
|
c. Carotid sinus hypersensitivity |
|
d. Nonclassic forms |
|
2. Orthostatic hypotension a. Primary autonomic failure—Parkinson's disease, multi-system atrophy, Lewy's body dementia |
|
b. Secondary autonomic failure—diabetes, uremia, spinal cord injury, amyloidosis |
|
c. Drug-induced—antihypertensives, vasodilators, diuretics, sedatives |
|
d. Volume depletion—hemorrhage, vomiting, diarrhea |
|
3. Cardiac syncope |
|
a. Bradyarrhythmias—sinoatrial (SA) node dysfunction, atrioventricular (AV) node dysfunction, pacemaker dysfunction, drug-induced bradycardia |
|
b. Tachyarrhythmia—supraventricular tachycardia, ventricular tachycardia, ventricular fibrillation, channelopathies, structural, idiopathic and drug-induced |
|
c. Structural abnormality—aortic stenosis, mitral stenosis, pulmonary stenosis, hypertrophic cardiomyopathy |
|
d. Others vascular conditions—pulmonary thromboem-bolism, acute aortic dissection, pulmonary arterial hypertension1 |
Vagal Syncope
Vagal syncope is the most common form of neurocardiogenic syncope. Vasovagal is usually benign and self-limiting but could prove fatal in patients with limited cardiac reserve, severe obstructive coronary artery disease (CAD), and left ventricular outflow tract obstruction. Usually, vagal syncope occurs in two forms: vasodepressor and cardioinhibitory, both attributed to activation of Bezold-Jarisch reflex.3 4
-
Vasodepression refers to hypotension resulting from insufficient sympathetic vasoconstriction. It is characterized by a steady fall in arterial pressure with or without an increase in heart rate.
-
Cardioinhibition refers to parasympathetic predominance, resulting in bradycardia or asystole. It is characterized by a sudden fall in heart rate, resulting in a precipitous fall in arterial pressures. It is usually triggered by severe pain, unpleasant sight, fasting, prolonged standing, crowded, uncomfortable surrounding, postural hypotension, hyperventilation, and psychogenic factors.
Features of a Typical Vasovagal Episode
-
Usually, occurs in a standing or sitting position. May occur in the supine position as in cardiac catheterization due to access site pain.
-
Lasts for few seconds to < 1 minute, rarely 2 to 5 minutes.
-
Prodrome of weakness, light-headedness, nausea, yawning, sweating, pallor, a sensation of impending doom. An occasional urge to pass urine or motion.
-
LOC with fall to ground or slump to one side while sitting. Pulse is slow or low volume.
-
Wakes up with a feeling of dizziness, nausea, vomiting. Orients to surroundings within seconds.
-
The total duration of episode 5 to 10 minutes7 8 9 (Fig. 4).

-
Fig. 4 Pathophysiology of VVS (vasovagal syncope).
Fig. 4 Pathophysiology of VVS (vasovagal syncope).
Hysteric faint/fainting lark: Self-induced syncope due to gravitation hypotension, Valsalva's maneuver–induced raised intrathoracic pressure, and cerebral vasoconstriction due to hypocapnia as a result of hyperventilation.
Rock concert syncope: Mass fainting, common among rock concert audience. Precipitated by sleeplessness, fasting, prolonged standing, anxiety, and hyperventilation in the crowd.
The nonclassic form of reflex syncope is seen with uncertain or absent triggers and may have an atypical presentation.
Carotid sinus syncope results from an exaggerated response to carotid sinus stimulation (carotid sinus hypersensitivity). Diagnosed when carotid sinus pressure for 5 seconds results in pauses of > 3 seconds causing syncope. Carotid sinus reflex plays an essential role in autoregulation of BP. An abnormal reflex results in excessive BP and heart rate response. Carotid sinus stimulation causes cardiac vagal inhibition results in bradycardia/asystole—inhibition of sympathetic activity in the skeletal vasculature results in peripheral vasodilatation and hypotension.
It is common in the elderly men and occur suddenly with minimal prodrome. An episode is typically precipitated by using tight collars, shaving, head turning, looking up, and coughing.
Cardiac Syncope
Arrhythmias account for nearly 80% of cases of cardiac syncope, and the most frequent arrhythmia producing syncope is ventricular tachycardia (VT). Onset is often sudden with or without prodrome; palpitations may precede or follow the episode. Cardiac syncope typically occurs in a supine position, in bed, or during exertion or sexual activity. There may be no detectable pulse, and myoclonic jerks and incontinence may occur due to prolonged asystole.10 11
Tachyarrhythmias
-
Ventricular tachycardia accounts for 40% of cardiovascular syncope—the most common diagnosis in the elderly beyond 70 years. Most have underlying heart disease. The majority have no prodrome, though palpitations and light-headedness may be experienced by few. Diagnosis is established by 12-lead electrocardiogram (ECG).
-
Long QT syndrome: Prolongation of QT interval could be due to a variety of reasons and predispose to torsade de pointes. Commonly presents before the age of 20 years. Syncope or cardiac arrest occurs under emotional or physical stress. A correctly interpreted ECG gives a clue to diagnosis.
-
Supraventricular tachycardia (SVT): Syncope is less common in SVT, accounting for 8% of cardiac causes of syncope. Certain factors that predispose to syncope in SVT are underlying severe heart disease (aortic stenosis, hypertrophic cardiomyopathy, pulmonary stenosis, restrictive cardiomyopathy), advanced age, rates > 200/min, and underlying preexcitation. Paradoxically, younger patients with better atrioventricular (AV) conduction and faster rate are more prone to syncope than elderly with slow AV nodal conduction.
Bradyarrhythmias account for 31% of cardiac causes of syncope. It is seen most commonly with sick sinus syndrome (SSS) and complete heart block (CHB).
-
Sick sinus syndrome: The patient presents with a history of syncope following relief of sudden-onset palpitations. SSS should also be suspected in cases of SVT in which rates are < 200/min with a history of recurrent syncope. Syncope in SSS could be due to severe sinus bradycardia, CHB, or sinus arrest.
-
Complete heart block: Syncope is rare in congenital CHB. Syncope occurs in CHB with associated conduction defects. Prodromal symptoms are frequently absent, and unconsciousness supervenes with few seconds. Commonly mistaken for a seizure.
Nonarrhythmic Cardiovascular Causes of Syncope
-
Aortic stenosis: Exercise-induced syncope is one of the cardinal symptoms of severe aortic stenosis. Syncope occurs as a result of fall in systemic vascular resistance (vasodilatation in skeletal muscles), failure of forearm vasoconstriction (ventricular Bezold-Jarisch reflex), and failure of a rise in cardiac output in the presence of a fixed obstruction. In nonsevere aortic stenosis, syncope could result from associated CAD or arrhythmias.12
-
Hypertrophic cardiomyopathy: Syncope may occur irrespective of the severity of outflow obstruction and is due to arrhythmias or ventricular filling.13
-
Mitral stenosis (MS): Syncope is relatively rare in MS despite it being severe. Paroxysmal atrial arrhythmias, severe pulmonary hypertension, acute pulmonary embolism, associated ankylosing spondylitis (AS), or CAD, and ball valve thrombus may present with syncope in MS. Recurrent syncope in a suspected patient of MS should suggest left atrial myxoma.
-
Syncope is not uncommonly seen in severe pulmonary hypertension or acute massive pulmonary embolism as a result of severe obstruction to pulmonary circulation consequent to increase in pulmonary vascular resistance.
-
Syncope in systemic hypertension suggests postural hypo-tension, cerebrovascular accident, hypertensive encephalopathy, and, rarely, pheochromocytoma.
-
Coronary artery disease: This is the most frequent cause of syncope in middle-aged and elderly patients. Syncope in CAD suggests polymorphic VT or ventricular fibrillation or hypotension due to a large area of dysfunctional myocardium. Bradyarrhythmia secondary to myocardial infarction (MI) or acute mechanical complication can also present as syncope.
Approach to a Patient with Syncope
Symptoms and Signs
History and physical examination are the standards of care in evaluating syncope.1 2 Etiology of syncope is established in 50 to 85% of patients with a thorough history and physical examination. No single laboratory test is diagnostic for syncope. History, physical examination, and 12-lead ECG are the only recommendations (level A) by the 2007 American College of Emergency Physicians (ACEP) Clinical Policy on Syncope.14
Symptoms of syncope: Patient may describe the syncope episode as one of the following: blacking out, feeling lightheaded/dizzy/drowsy/unsteady and weak, fainting, or falling for no reason.
Premonitory symptoms are seen in 70% of patients in the form of light-headedness, nausea, diaphoresis, epigastric discomfort, and blurred vision. Chest pain, dyspnea, and palpitations are the red signs of cardiac etiology.
A detailed description of the episode including the circumstances surrounding it, precipitating factors, patient's activity, and position preceding the event must be obtained from the patient.
-
Precipitants such as sleep or food deprivation, pain, fear, apprehension, fatigue, alcohol consumption, and change in environment should be enquired.
-
Activity before syncope may suggest the etiology. Syncope may occur at rest; with a change of posture; on exertion; after exertion; or with specific situations such as shaving (carotid sinus hypersensitivity), coughing (cough syncope), voiding (micturition syncope), or prolonged standing. Syncope occurring within 2 minutes of standing suggests orthostatic hypotension.15
-
Syncope on standing, sitting, or lying. Syncope in sitting position on recumbent posture is more likely to be cardiac.16
-
The clinical background gives an essential clue to the etiology of syncope:
-
Diabetic: Hypoglycemia, cerebral vascular disease (CVA), CAD, or postural hypotension due to autonomic neuropathy
-
Hypertensive: Postural hypotension due to drugs, CVA/CAD
-
Coronary artery disease: Acute ischemia, arrhythmia, mechanical complication
-
Postoperative/immobilization: Pulmonary embolism
-
Deaf patient: Prolonged QT syndrome
-
Pain/unpleasant event/sight: Vasovagal
-
History of fall or head injury: Subdural hematoma
-
Signs of Syncope
A complete physical examination is mandatory and might give clues to etiology.
-
Vital signs: the presence of fever; tachycardia or bradycardia; postural change in BP could suggest the cause for syncope.
-
Detailed cardiac examination.
-
Detailed neurologic examination.
-
Signs of trauma: Trauma could be secondary to syncope. Tongue trauma is specific for seizures (Table 2).
|
Recommendation |
Class |
Level |
|---|---|---|
|
Abbreviations: AV, atrioventricular; BBB, bundle branch block; ECG, electrogram; ESC, European Society of Cardiology; ICD, implantable cardioverter-defibrillator; OH, orthostatic hypotension; SVT, supraventricular tachycardia; VT, ventricular tachycardia; VVS, vasovagal syncope. |
||
|
Reflex syncope and OH |
||
|
VVS is highly probable if syncope is precipitated by pain, fear, or standing, and is associated with typical prodrome (pallor, sweating, and nausea) |
I |
C |
|
Situational reflex syncope is highly probable if syncope occurs during or immediately after specific triggers |
I |
C |
|
Syncope due to OH is confirmed when syncope occurs while standing and there is concomitant significant OH |
I |
C |
|
In the absence of the above criteria, reflex syncope and OH should be considered likely when the features that suggest reflex syncope or OH is present, and the features that suggest cardiac syncope are absent |
IIa |
C |
|
Cardiac syncope |
||
|
Arrhythmic syncope is highly probable when ECG shows: |
I |
C |
|
• Persistent sinus bradycardia < 40 beats/min or sinus pauses > 3 s in awake state and in the absence of physical training |
||
|
• Mobitz II second- and third-degree AV block |
||
|
• Alternating left and right BBB |
||
|
• VT or rapid paroxysmal SVT |
||
|
• Nonsustained episodes of polymorphic VT and long or short QT interval |
||
|
• Pacemaker or ICD malfunction with cardiac pauses |
||
|
Cardiac ischemia-related syncope is confirmed when syncope presents with evidence of acute myocardial ischemia with/without myocardial infarction |
I |
C |
|
Syncope due to structural cardiopulmonary disorders is highly probable when syncope presents in patients with prolapsing atrial myxoma, left atrial ball thrombus, severe aortic stenosis, pulmonary embolus, or acute aortic dissection |
I |
C |
Investigations
-
ECG: Mandatory in all cases of syncope. Immediate ECG when suspicion of arrhythmia is strong.
-
Blood tests: Depending on the clinical scenario.
-
Hematocrit/hemoglobin: Hemorrhage.
-
Arterial blood gas analysis and O2 saturation: Hypoxia.
-
Troponin: Ischemia.
-
D-dimer: Pulmonary embolism.
-
-
Carotid sinus massage (CSM)17–19: CSM produces ventricular pauses > 3 seconds and a fall in SBP of > 50 mm Hg in carotid sinus hypersensitivity. The diagnosis of carotid sinus syndrome (CSS) requires demonstration of symptoms/syncope for diagnosis. In a multicentric study, CSM could diagnose CSS in 8.8% patients when performed after initial evaluation and is recommended according to the 2009 European Society of Cardiology (ESC) guidelines. CSM was indicated after an initial evaluation. However, the main complication is neurologic; with transient ischemic attack (TIA) or stroke observed in 21% from four different studies (Table 3).
-
Orthostatic challenge: A change in position from the supine to upright causes extrathoracic shift of blood. In decreased venous return and cardiac output. A fall in BP causing syncope may occur in the absence of compensatory mechanisms.
|
Recommendation |
Class |
Level |
|---|---|---|
|
Abbreviations: ESC, European Society of Cardiology; CSM, carotid sinus massage; CSS, carotid sinus syndrome. |
||
|
Indications |
||
|
CSM is indicated in patients > 40 years of age with syncope of unknown origin compatible with a reflex mechanism |
I |
B |
|
Diagnostic criteria |
||
|
CSS is confirmed if it causes bradycardia (asystole) and hypotension that reproduce spontaneous symptoms, and patients have clinical features compatible with a reflex mechanism of syncope |
I |
B |
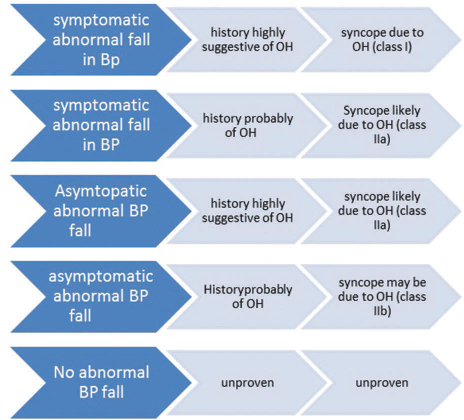
Diagnostic criteria 20: A fall in SBP of ≥ 20 mm Hg or diastolic BP (DBP) ≥ 10 mm Hg, or a decrease in SBP to < 90 mm Hg is considered as orthostatic hypotension. Occurrence of isolated diastolic drop in BP is rare and of little clinical relevance. A corresponding increase in heart rate is blunted or absent (usually not > 10 beats/min) in patients with neurogenic OH but exaggerated in anemia or hypovolemia (Fig. 5).
-
Fig. 5 ESC 2018 diagnostic criteria for orthostatic hypotension (OH) after orthostatic challenge. BP, blood pressure.
Fig. 5 ESC 2018 diagnostic criteria for orthostatic hypotension (OH) after orthostatic challenge. BP, blood pressure.
There are three methods for eliciting orthostatic challenge: (1) active standing, (2) head-up tilt test, and (3) 24-hour ambulatory BP monitoring (ABPM).
Active Standing
A sphygmomanometer for elicitation of OH on standing is adequate for routine clinical testing. When more frequent readings (> 4) or continuous beat-to-beat noninvasive BP measurement is required, automated devices are recommended (Table 4).
|
Recommendation |
Class |
Level |
|---|---|---|
|
Abbreviations: BP, blood pressure; ESC, European Society of Cardiology; HR, heart rate; OH, orthostatic hypotension. |
||
|
Indication |
||
|
Intermittent determination by sphygmomanometer of BP and HR while supine and during active standing for 3 min is indicated at initial syncope evaluation. |
I |
C |
|
Continuous beat-to-beat noninvasive BP and HR measurement may be preferred when short-lived BP variations are suspected, such as in initial OH. |
IIb |
C |
|
Diagnostic criteria as mentioned in Fig. 5 |
||
Tilt testing: First introduced in 1986. The trinitroglycerin (TNG) protocol and the isoproterenol protocol are the most commonly used ones presently21 (Fig. 6).

-
Fig. 6 Tilt testing protocols. HR, heart rate; TNG, trinitroglycerin.
Fig. 6 Tilt testing protocols. HR, heart rate; TNG, trinitroglycerin.
Tilt testing is useful for diagnosis but has limited value in assessing treatment efficacy. A negative tilt table response does not exclude a diagnosis of reflex syncope (Table 5).
|
Recommendation |
Class |
Level |
|---|---|---|
|
Abbreviations: ESC, European Society of Cardiology; OH, orthostatic hypotension; POTS, Postural orthostatic tachycardia syndrome; PPS, psychogenic pseudosyncope. |
||
|
Indications |
||
|
Tilt testing should be considered in patients with suspected reflex syncope, OH, POTS, or PPS. B |
IIa |
B |
|
Tilt testing may be considered to educate patients to recognize symptoms and learn physical maneuvers |
IIb |
B |
|
Diagnostic criteria |
||
|
Reflex syncope, OH, POTS, or PPS should be considered likely if tilt testing reproduces symptoms along with the characteristic circulatory pattern of these conditions |
IIa |
B |
A positive cardioinhibitory response to tilt testing predicts asystolic spontaneous syncope with high probability. However, a positive vasodepressor, a mixed response, or even a negative response does not exclude the presence of asystole during spontaneous syncope. In syncope of unknown origin, Tilt testing identifies patients at risk of orthostatic stress known as hypotensive susceptibility and has practical implication in therapy.
A 24-hour ABPM and home BP monitoring (HBPM) help detect OH in daily life better than single office BP measurements; however, evidence is limited regarding its utility in this aspect.
Autonomic function tests22 23 help detect an autonomic failure as the cause of syncope (Table 6).
|
Recommendation |
Class |
Level |
|---|---|---|
|
Abbreviations: ABPM, ambulatory blood pressure monitoring; BP, blood pressure; ESC, European Society of Cardiology; HBPM, home blood pressure monitoring; OH, orthostatic hypotension. |
||
|
Valsalva's maneuver |
||
|
Valsalva's maneuver should be considered for the assessment of autonomic function in patients with suspected neurogenic OH. B |
IIa |
B |
|
Valsalva's maneuver may be considered for confirming the hypotensive tendency induced by some forms of situational syncope, e.g., coughing, brass instrument playing, singing, and weightlifting. |
IIb |
C |
|
Deep-breathing test |
||
|
Deep-breathing tests should be considered for the assessment of autonomic function in patients with suspected neurogenic OH. |
IIa |
B |
|
Other autonomic function tests |
||
|
30:15 ratio, cold pressure test, sustained handgrip test, and a mental arithmetic test may be considered for the assessment of autonomic function in patients with suspected neurogenic OH. |
IIb |
C |
|
ABPM and HBPM |
||
|
ABPM is recommended to detect nocturnal hypertension in patients with autonomic failure |
I |
B |
|
ABPM should be considered to detect and monitor the degree of OH and supine hypertension in daily life in patients with autonomic failure. C |
IIa |
C |
|
ABPM and HBPM may be considered to detect whether BP is abnormally low during episodes suggestive of orthostatic intolerance. |
IIb |
C |
Electrocardiographic monitoring23 24 is recommended when arrhythmia as a cause of syncope is highly suspected. However, the yield to diagnosis is role varies from 1.9 to 17.6% depending on the mode of ECG monitoring. Implantable loop recorders (ILRs) are more cost-effective than conventional strategy.25 A patient should be observed for at least 4 years before a conclusion is drawn—no arrhythmia at the time of syncope rules out an arrhythmic syncope. The absence of simultaneous BP recording limits ECG monitoring devices (Table 7).
|
Recommendation |
Class |
Level |
|---|---|---|
|
Abbreviations: AV, atrioventricular; ECG, electrocardiogram; ESC, European Society of Cardiology; ILR, implantable loop recorder; SVT, supraventricular tachycardia; VT, ventricular tachycardia. |
||
|
Immediate in-hospital monitoring (in bed or by telemetry) is indicated in high-risk patients. C |
I |
C |
|
Holter monitoring should be considered in patients who have frequent syncope or pre-syncope (≥ 1 episode per week). B |
IIa |
B |
|
External loop recorders should be considered, early after the index event, in patients who have an inter-symptom interval ≤ 4 wk |
IIa |
B |
|
ILR is indicated in an early phase of evaluation in patients with recurrent syncope of uncertain origin in the absence of high-risk criteria. A |
I |
A |
|
ILR is indicated in patients with high-risk criteria in whom a comprehensive evaluation did not demonstrate a cause of syncope or lead to a specific treatment. |
I |
A |
|
ILR should be considered in patients with suspected or certain reflex syncope presenting with frequent or severe syncopal episodes. |
IIa |
B |
|
ILR may be considered in patients in whom epilepsy was suspected, but the treatment has proven ineffective. B |
IIb |
B |
|
ILR may be considered in patients with unexplained falls. |
IIb |
B |
|
Diagnostic criteria |
||
|
Arrhythmic syncope is confirmed when a correlation between syncope and an arrhythmia is detected. B |
I |
B |
|
In the absence of syncope, arrhythmic syncope should be considered likely when periods of Mobitz II second- or third-degree AV block or a ventricular pause > 3 s or rapid, prolonged paroxysmal SVT or VT are detected. |
IIa |
C |
Video recording of syncope event26 has led to new insight into the pathophysiology of syncope (Table 8).
|
Recommendation |
Class |
Level |
|---|---|---|
|
Abbreviations: ESC, European Society of Cardiology. |
||
|
Home video recordings of spontaneous events should be considered. Physicians should encourage patients and their relative to obtain home video recordings of spontaneous events. C |
IIa |
C |
|
Adding video recording to tilt testing may be considered to increase the reliability of clinical observation of induced events. C |
IIb |
C |
Electrophysiologic studies (EPS) have a limited role in the evaluation of syncope. In routine clinical practice < 3% patients undergo EPS for evaluation of unexplained syncope. Positive results are obtained predominantly in patients with structural heart disease. EPS has no role in syncope with normal ECG, no structural heart disease, and no palpitations. A negative study does not exclude arrhythmic cause of syncope (Table 9).
|
Recommendation |
Class |
Level |
|---|---|---|
|
Abbreviations: BBB, bundle branch block; ECG, electrocardiogram; EPS, electrophysiology study; ESC, European Society of Cardiology. |
||
|
Indications |
||
|
In patients with syncope and previous myocardial infarction, or other scar-related conditions, EPS is indicated when syncope remains unexplained after noninvasive evaluation. B |
I |
B |
|
In patients with syncope and bifascicular BBB, EPS should be considered when syncope remains unexplained after noninvasive evaluation. B |
IIa |
B |
|
In patients with syncope and asymptomatic sinus bradycardia, EPS may be considered in a few instances when noninvasive tests (e.g., ECG monitoring) have failed to show a correlation between syncope and bradycardia. B |
IIb |
B |
|
In patients with syncope preceded by sudden and brief palpitations, EPS may be considered when syncope remains unexplained after noninvasive evaluation. |
IIb |
C |
Adenosine triphosphate (ATP) provocation testing27 is useful in the evaluation of unexplained syncope without prodrome; 20 mg bolus of adenosine is injected rapidly (< 2 seconds). Ventricular asystole > 6 seconds or AV block lasting > 10 seconds is considered abnormal. Its low predictive value does not support its routine use.
Echocardiography: Syncope alone is not an indication for echocardiography. Aortic stenosis, hypertrophic obstructive cardiomyopathy, pulmonary embolism, cardiac masses, and aortic dissection when identified on echocardiography28 are responsible for syncope without further testing (class I C) (Table 10).
|
Recommendation |
Class |
Level |
|---|---|---|
|
Abbreviations: ESC, European Society of Cardiology; HCM, hypertrophic cardiomyopathy. |
||
|
Indications |
||
|
Echocardiography is indicated for diagnosis and risk stratification in patients with suspected structural heart disease. B |
I |
B |
|
Two-dimensional and Doppler echocardiography during exercise in the standing, sitting, or semisupine position to detect provocable left ventricular outflow tract obstruction that is indicated in patients with HCM, a history of syncope, and resting or provoked peak instantaneous left ventricular outflow tract gradient < 50 mm Hg. |
I |
B |
Exercise stress testing: There is no evidence for its use in a general population presenting with syncope (Table 11).
|
Recommendation |
Class |
Level |
|---|---|---|
|
Abbreviations: AV, atrioventricular; ESC, European Society of Cardiology. |
||
|
Indications |
||
|
Exercise testing is indicated in patients who experience syncope during or shortly after exertion. C |
I |
C |
|
Diagnostic criteria |
||
|
Syncope due to second- or third-degree AV block is confirmed when the AV block develops during exercise, even without syncope. C |
I |
C |
|
Reflex syncope is confirmed when syncope is reproduced immediately after exercise in the presence of severe hypotension. |
I |
C |
Coronary angiography: Indications to perform coronary angiography remains the same as in patients without syncope (class IIa C). In patients with significant obstructive CAD and syncope, percutaneous coronary intervention (PCI) does not reduce the incidence of syncope.
Mimics of syncope: Syncope may be confused with seizures, coma, shock, or other states of altered consciousness.
The following questions should be asked:
-
Was LOC complete?
-
Was LOC sudden in onset and short duration?
-
Was recovery spontaneous, complete, and without sequelae?
-
Was there a loss of postural tone?
Syncope is likely if all the answers are final. Other forms of transient LOC (TLOC) should be considered if one or more answers are negative29 (Table 12).
|
Condition |
Characteristic Feature |
|---|---|
|
Abbreviations: LOC, loss of consciousness; TLOC, transient loss of consciousness. |
|
|
Seizure |
Convulsive activity, automatism or focality, and aura favor seizure. Prior nausea and diaphoresis suggest syncope. Oral trauma, incontinence, and postictal confusion suggest a seizure. Post-event confusion can occur in syncope but lasts < 30 s. |
|
Pseudocoma |
Duration of apparent LOC is longer—many minutes to hours; repetition occurs many times in a day. |
|
Cataplexy |
Falls with flaccid paralysis and nonresponsive, no amnesia |
|
Metabolic disorders—hypoglycemia, hypoxia, hyperventilation with hypocapnia |
Duration of impaired consciousness is longer. |
|
Intoxication |
Duration of impaired consciousness is longer |
|
Cardiac arrest |
LOC yet no spontaneous recovery |
|
Coma |
Duration much longer than TLOC |
Risk Stratification and Prognosis
Prognosis is poor in cardiac syncope with 1-year mortality reported as high as 18 to 33%, especially those with New York Heart Association (NYHA) functional class III or IV. Some patients do well after definitive surgical treatment or pacemaker placement.
Noncardiac syncope does not affect overall mortality. Vasovagal syncope has an excellent prognosis with infrequent recurrences. Situational syncope and orthostatic syncope also have an excellent prognosis; however, recurrences occur and may result in significant morbidity regarding the quality of life and secondary injury.
Syncope of unknown etiology generally has a favorable prognosis, with 2% incidence of sudden death, 20% chance of recurrent syncope, and 78% remission rate within 1 year.
Management of a suspected case of syncope in the emergency department (ED) depends on the response to three questions30:
-
Is there a severe identifiable underlying cause?
-
What is the risk of a severe outcome?
-
Does the patient require admission?
About 10% of patients presenting with syncope in the ED have a severe outcome with 7 to 30 days. It is essential to identify these high-risk patients and ensure appropriate investigations.
The ROSE (Risk stratification Of Syncope in the Emergency department) ED questionnaire31 can predict 1-month serious outcomes and all cause. It has excellent sensitivity and negative predictive value (98.5%) in the identification of high-risk patients with syncope (Table 13).
|
Admit is any of the following are present at arrival in ED |
|---|
|
Abbreviations: BNP, brain natriuretic peptide; ECG, electrocardiogram; ED, emergency department; Hb, hemoglobin; ROSE, Risk stratification Of Syncope in the Emergency department. |
|
A. Bradycardia < 50/min |
|
B. BNP levels > 300 pg/mL |
|
C. Rectal examination action—feces, occult blood |
|
D. Anemia: Hb < 9 g/dL |
|
E. Chest pain with syncope |
|
F. ECG showing Q waves (other than lead III) |
|
G. Saturation of oxygen < 94% on room air |
|
Acrony: BRACES |
Patients with low-risk features can be safely discharged after properly educating the patient. High-risk patients would require admission and further evaluation (Table 14).
|
Low risk |
High risk |
|
|---|---|---|
|
Abbreviations: ECG, electrocardiogram; ESC, European Society of Cardiology; OH, orthostatic hypotension; VVS, vasovagal syncope. |
||
|
Syncopal event |
VVS or OH |
Cardiac syncope |
|
Past medical history |
Recurrent syncope, long history No structural heart disease |
Severe structural or coronary artery disease |
|
Clinical examination |
Normal |
Cardiac murmur Persistent bradycardia Persistent hypotension GI or rectal bleed |
|
ECG |
Normal |
Abnormal ECG - Arrhythmias - Ischemic changes |
ESC 2018 Recommendations for Management of Syncope in Emergency Department
-
Patients with low-risk features likely to have a reflex or situational syncope or syncope due to OH; can be discharged from the ED (class I. B).
-
Patients with high-risk features receive an early intensive and prompt evaluation in hospital (class I. B) B.
-
Patients who have neither high- nor low-risk features are observed in the ED (class I. B).
-
Risk stratification scores may be considered for risk stratification in the ED (class IIb. B) B.
Treatment and Management
Treatment depends on risk stratification and type of syncope. Counseling and patient education are an integral part of treatment and management of syncope. It has been observed and reported in the literature that the recurrence of syncope decreases spontaneous once medical attention is given irrespective of initiation of specific therapy, especially in cases of reflex and unexplained syncope. This implies that pharmacologic therapy and other interventions can be postponed in the case of low-risk conditions.
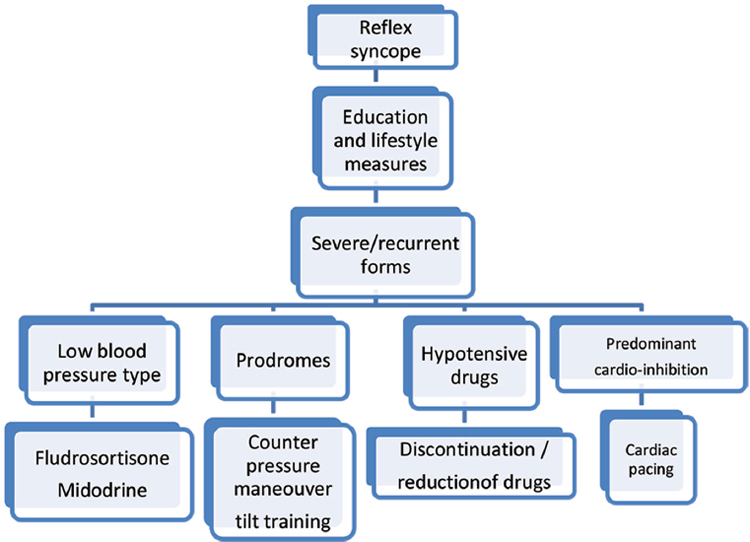
Reflex syncope: Repeated and disabling reflex syncope can be distressing and affect the quality of life. Patient education regarding the diagnosis and risk of recurrences, reassurance about its benign nature, and advice on how to avoid triggers and situations are the cornerstones of treatment. It has a high impact in reducing the recurrence of syncope. Specific therapy may be considered in severe cases (Fig. 7).

-
Fig. 7 Indications for specific therapy.
Fig. 7 Indications for specific therapy.
Specific therapy is required in only 14% of the patient population with syncope.
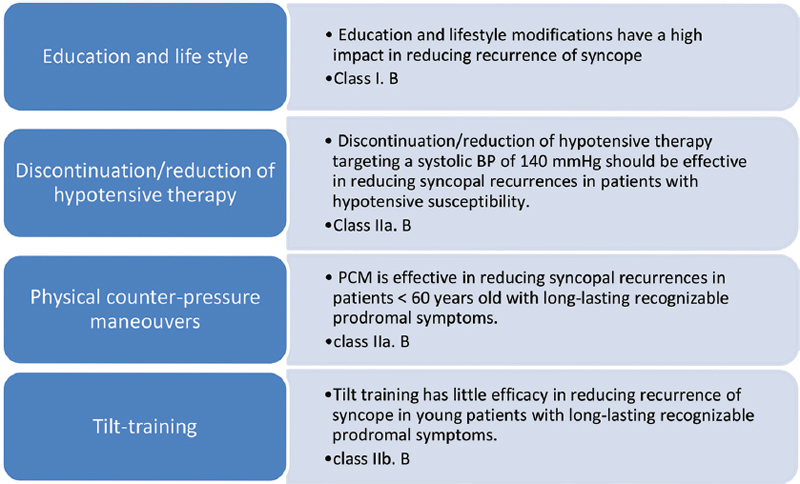
ESC 2018 recommendations for treatment and management of reflex syncope are summarized in Fig. 8:
-
Fig. 8 ESC 2018 recommendations for management of reflex syncope. BP, blood pressure; PCM, physical counter-pressure maneuver.
Fig. 8 ESC 2018 recommendations for management of reflex syncope. BP, blood pressure; PCM, physical counter-pressure maneuver.
Pharmacologic therapy: Effective in the specific subset of reflex syncope.
-
Fludrocortisone: Effective in reducing syncope recurrences in young patients with low BP in the absence of comorbidities (class IIb. B). The dose recommended is 0.05 to 0.2 mg tid. It acts by increasing renal sodium absorption and expanding plasma volume.
-
α-Agonists: Act by vasoconstriction: etilefrine 25 mg bd and midodrine 2.5 to 10 mg tid. There is conflicting evidence regarding the effectiveness of α-agonists in reducing syncopal recurrence (class IIb. B). Further research is warranted.
-
β-Blockers: There is sufficient evidence to say that β-blockers are not appropriate for reducing syncopal recurrence (class III. A).
-
Other drugs: Paroxetine, a selective serotonin reuptake inhibitor; benzodiazepine; somatostatin analog octreotide. Insufficient data are available on these. Further research is warranted.
-
Emerging therapies: Theophylline; norepinephrine transport inhibitors (reboxetine and sibutramine) and ganglionic plexus ablation have proved useful in reflex syncope and warrant further research.
Cardiac pacing: Indicated in elderly > 60 years with the severe form of syncope and preferably a DDDR (dual-chamber rate adaptive pacemaker), especially after a positive tilt test (Table 15).
|
Recommendation |
Class |
Level |
|---|---|---|
|
Abbreviations: AV, atrioventricular; ESC, European Society of Cardiology. |
||
|
Cardiac pacing should be considered to reduce syncopal recurrences in patients aged > 40 y, with spontaneous documented symptomatic asystolic pause(s) > 3 s or asymptomatic pause(s) > 6 s due to sinus arrest, AV block, or the combination of the two. B |
IIa |
B |
|
Cardiac pacing should be considered to reduce syncope recurrence in patients with cardio-inhibitory carotid sinus syndrome who are > 40 y with recurrent frequent, unpredictable syncope. B |
IIa |
B |
|
Cardiac pacing may be considered to reduce syncope recurrences in patients with tilt-induced asystolic response who are > 40 y with recurrent frequent, unpredictable syncope. B |
IIb |
B |
|
Cardiac pacing may be considered to reduce syncope recurrences in patients with the clinical features of adenosine-sensitive syncope. |
IIb |
B |
|
Cardiac pacing is not indicated in the absence of a documented cardioinhibitory reflex. |
III |
B |
The choice of specific therapy is decided according to the age, severity of syncope, and clinical forms. The algorithm for management according to ESC 2018 guidelines is mentioned in Fig. 9.
-
Fig. 9 Algorithm for management of reflex syncope—ESC 2018.
Fig. 9 Algorithm for management of reflex syncope—ESC 2018.
Orthostatic hypotension syncope: Education and lifestyle change are the cornerstones of treatment. Aggressive BP reduction should be avoided. Diuretics and β-blockers that are more prone for OH to be avoided (Fig. 10).

-
Fig. 10 ESC 2018 recommendations for management of OH. PCM, physical counter-pressure maneuver.
Fig. 10 ESC 2018 recommendations for management of OH. PCM, physical counter-pressure maneuver.
Cardiac arrhythmia as the primary cause of syncope: The significant factors predicting the efficacy of pacing in preventing syncope recurrence are a stable relationship between symptoms and bradycardia. An implantable cardioverter-defibrillator (ICD) can prevent sudden cardiac death (SCD) but does not prevent syncope due to VT. Thus, when syncope is due to VT, catheter ablation should always be attempted when feasible in addition to ICD implantation (Table 16).
|
Recommendation |
Class |
Level |
|---|---|---|
|
Abbreviations: AV, atrioventricular; BBB, bundle branch block; EPS, electrophysiologic study; ESC, European Society of Cardiology; ICD, implantable cardioverter-defibrillator; ILR, implantable loop recorder; SVT, supraventricular tachycardia; VT, ventricular tachycardia; VVS, vasovagal syncope. |
||
|
Bradycardia |
||
|
Cardiac pacing is indicated when there is an established relationship between syncope and symptomatic bradycardia due to either sick sinus syndrome or intrinsic AV block. |
I |
B |
|
Cardiac pacing is indicated in asymptomatic patients with paroxysmal intrinsic third- or second-degree AV block. C |
I |
C |
|
Cardiac pacing should be considered when the relationship between syncope and asymptomatic sinus node dysfunction is less established. C |
IIa |
C |
|
Cardiac pacing is not indicated in patients when there are reversible causes for bradycardia. |
III |
C |
|
Bifascicular BBB |
||
|
Cardiac pacing is indicated in patients with syncope, BBB, and a positive EPS or ILR-documented AV block. B |
I |
B |
|
Cardiac pacing may be considered in patients with unexplained syncope and bifascicular BBB. |
IIb |
B |
|
Tachycardia |
||
|
Catheter ablation is indicated in patients with syncope due to SVT or VT to prevent recurrence. B |
I |
B |
|
An ICD is indicated in patients with syncope due to VT and an ejection fraction ≤ 35%. A |
I |
A |
|
An ICD is indicated in patients with syncope and previous myocardial infarction who have VT induced during EPS. C |
I |
C |
|
An ICD should be considered in patients with an ejection fraction > 35% with recurrent syncope due to VT despite catheter ablation and pharmacologic therapy. C |
IIa |
C |
|
Antiarrhythmic drug therapy, including rate-control drugs, should be considered in patients with syncope due to SVT or VT. |
IIa |
C |
In syncope secondary to structural cardiac disease, the primary goal should be to treat the underlying disease and not only to prevent syncopal recurrence.
Unexplained syncope is defined as syncope that does not meet any class I diagnostic criteria. It is presumed to be to be a transient arrhythmia.
-
In a patient at high risk for SCD due to unexplained syncope, ICD implantation should be considered (class IIa. B).
-
In patients with unexplained syncope and long QT syndrome: ICD implantation should be considered in addition to β-blockers (class IIa. B).
-
In patients intolerant or resistant to β-blockers and ICD, left cardiac sympathetic denervation might be considered (class IIb. B).
-
In unexplained syncope and Brugada's syndrome: ICD implantation can be considered (class IIa. B).
-
An ILR may be considered instead of ICD in unexplained syncope and long QY/Brugada with low-risk features (class IIb. B).
Conclusion
Despite the existing guidelines, each patient with syncope needs to be individualized. The diagnostic process should be reevaluated, and alternative therapies should be considered if the recommendations fail or are not applicable to an individual patient. Presence of syncope adds to increased morbidity and mortality irrespective of the underlying cause. There is a wide gap between the clinical practice and existing guidelines in syncope. This calls for further large-scale clinical trials to assess the efficacy of existing therapies and the need for newer more useful recommendations. Development of dedicated syncopal units to ensure appropriate risk stratification, diagnosis, and treatment of patients disabled by syncope would be beneficial.
Conflict of Interest
None declared.
References
- ESC Scientific Document Group. 2018 ESC Guidelines for the diagnosis and management of syncopeEur Heart J. 2018;39(21):1883-1948.
- [Google Scholar]
- The elusive pathophysiology of neurally mediated syncope. Circulation. 2000;102(23):2898-2906.
- [Google Scholar]
- Vagal and sympathetic mechanisms in patients with orthostatic vasovagal syncope. Circulation. 1997;96(08):2509-2513.
- [Google Scholar]
- Symptoms and signs of syncope: a review of the link between physiology and clinical clues. Brain. 2009;132:2630-2642. (Pt 10)
- [Google Scholar]
- The semiology of tilt-induced reflex syncope in relation to electroencephalographic changes. Brain. 2014;137:576-585. (Pt 2)
- [Google Scholar]
- The origin of vasovagal syncope: to protect the heart or to escape predation? Clin Auton Res. 2008;18(04):170-178.
- [Google Scholar]
- Prevalence and triggers of syncope in medical students. Am J Cardiol. 2003;91(08):1006-1008. A8
- [Google Scholar]
- Vasovagal syncope in medical students and their first-degree relatives. Eur Heart J. 2006;27(16):1965-1970.
- [Google Scholar]
- American Heart Association; American College of Cardiology Foundation; Heart Rhythm Society. American Heart Association/American College of Cardiology Foundation/Heart Rhythm Society scientific statement on noninvasive risk stratification techniques for identifying patients at risk for sudden cardiac death: a scientific statement from the American Heart Association Council on Clinical Cardiology Committee on Electrocardiography and Arrhythmias and Council on Epidemiology and PreventionCirculation. 2008;118(14):1497-1518.
- [Google Scholar]
- Identifying cardiac syncope based on clinical history: a literature-based model tested in four independent datasets. PLoS One. 2013;8(09):e75255.
- [Google Scholar]
- Unexplained syncope in patients with structural heart disease and no documented ventricular arrhythmias: value of electrophysiologically guided implantable cardioverter defibrillator therapy. Europace. 2003;5(03):305-312.
- [Google Scholar]
- Differences in mechanisms and outcomes of syncope in patients with coronary disease or idiopathic left ventricular dysfunction as assessed by electrophysiologic testing. J Am Coll Cardiol. 2004;44(03):594-601.
- [Google Scholar]
- American College of Emergency Physicians. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with syncopeAnn Emerg Med. 2007;49(04):431-444.
- [Google Scholar]
- The value of the clinical history in the differentiation of syncope due to ventricular tachycardia, atrioventricular block, and neurocardiogenic syncope. Am J Med. 1995;98(04):365-373.
- [Google Scholar]
- Carotid sinus hypersensitivity in asymptomatic older persons: implications for diagnosis of syncope and falls. Arch Intern Med. 2006;166(05):515-520.
- [Google Scholar]
- Clinical context and outcome of carotid sinus syndrome diagnosed by means of the ‘method of symptoms’. Europace. 2014;16(06):928-934.
- [Google Scholar]
- Assessment of the vasodepressor reflex in carotid sinus syndrome. Circ Arrhythm Electrophysiol. 2014;7(03):505-510.
- [Google Scholar]
- Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clin Auton Res. 2011;21(02):69-72.
- [Google Scholar]
- The Newcastle protocols for head-up tilt table testing in the diagnosis of vasovagal syncope, carotid sinus hypersensitivity, and related disorders. Heart. 2000;83(05):564-569.
- [Google Scholar]
- Cardiovascular autonomic testing performed with a new integrated instrumental approach is useful in differentiating MSA-P from PD at an early stage. Parkinsonism Relat Disord. 2015;21(05):477-482.
- [Google Scholar]
- External prolonged electrocardiogram monitoring in unexplained syncope and palpitations: results of the SYNARR-Flash study. Europace. 2016;18(08):1265-1272.
- [Google Scholar]
- Effectiveness and safety of remote monitoring of patients with an implantable loop recorder. Rev Esp Cardiol (Engl Ed). 2013;66(12):943-948.
- [Google Scholar]
- The value of home video with ambulatory EEG: a prospective service review. Seizure. 2014;23(06):480-482.
- [Google Scholar]
- Adenosine and clinical forms of neurally-mediated syncope. J Am Coll Cardiol. 2015;66(02):204-205.
- [Google Scholar]
- Role of echocardiography in the evaluation of syncope: a prospective study. Heart. 2002;88(04):363-367.
- [Google Scholar]
- Task Force for the Diagnosis and Management of Syncope; European Society of Cardiology (ESC); European Heart Rhythm Association (EHRA); Heart Failure Association (HFA); Heart Rhythm Society (HRS) Guidelines for the diagnosis and management of syncope (version 2009)Eur Heart J. 2009;30(21):2631-2671.
- [Google Scholar]
- Management of transient loss of consciousness of suspected syncopal cause, after the initial evaluation in the emergency department. Emergency Care J. 2016;12:25-27.
- [Google Scholar]
- The ROSE (risk stratification of syncope in the emergency department) study. J Am Coll Cardiol. 2010;55(08):713-721.
- [Google Scholar]






