Translate this page into:
Student’s Corner–2
Maddury Jyotsna, MD DM FACC FESC FICC NIMS (Nizam institute of medical sciences) Punjagutta, Hyderabad, Telangana, 500082 India janaswamyjyostna@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Q1. Why DBP Does not Vary with AV Dissociation and Atrial Fibrillation
Answer by Prof. Dayasagar Rao
Systolic blood pressure (SBP) is mainly determined by stroke volume, while diastolic blood pressure (DBP) is determined by systemic vascular resistance (SVR), compliance of the arterial wall and duration of diastole.
When we say atrioventricular (AV) dissociation, we mean that the atria and the ventricles have independent rates and rhythms with a loss of synchrony, whereas in atrial fibrillation, the extremely high-heart rates make atrial contractions ineffective while reducing the diastolic filling time between two beats, leading to reduced ventricular filling. The variation in SBP in AV dissociation is due to variation in preload to ventricle proportional to atrial contribution to ventricle filling. No atrial contribution to ventricular filling occurs during simultaneous contraction of atria and ventricles, and maximum contribution by atria occurs when atrial contraction precedes ventricular contraction. Thus, in both these conditions, stroke volume is effectively reduced. Since DBP is not influenced by stroke volume, there are no changes seen.
Answer by Prof. Sampath
Arterial blood pressure is defined as lateral pressure exerted by contained column of blood on the walls of arteries.
Systolic blood pressure: It is the maximum pressure exerted in the arteries during systole of heart. It is calculated as a product of heart rate and stroke volume.
Diastolic blood pressure: It is the minimum pressure in the arteries during diastole of heart.
(It is multifactorial, depending on blood vessel diameter, vessel elasticity, blood viscosity, and total blood volume)
|
Determinants of systolic blood pressure: |
Determinants of diastolic BP: |
|
Volume of blood ejected |
Volume of blood remained |
|
Compliance of arterial wall |
Compliance of arterial wall |
|
Rate of runoff (resistance) |
Peripheral resistance |
In the above question, for the patient with AV dissociation and atrial fibrillation (preferably isolated), there is no change in peripheral resistance, which is the key determinant of DBP. Hence, no change in DBP.
For Students, a Few Important Formulae Relevant to the Question is Mentioned Below
Normally, diastole is longer than systole; hence, mean arterial pressure is not arithmetic mean of systolic and diastolic blood pressure.
Mean BP: DBP + 1/3rd of pulse pressure
Pulse pressure: SBP − DBP
Systolic pressure = diastolic pressure + pulse pressure
Pulse pressure = stroke volume/arterial capacitance
Mean arterial pressure = cardiac output × total peripheral resistance
Cardiac output =heart rate × stroke volume
Total peripheral resistance: blood viscosity × vascular resistance
Q2. Pulsus Paradoxus Mechanism in CCP and Tamponade
Answer by Prof. Dayasagar Rao
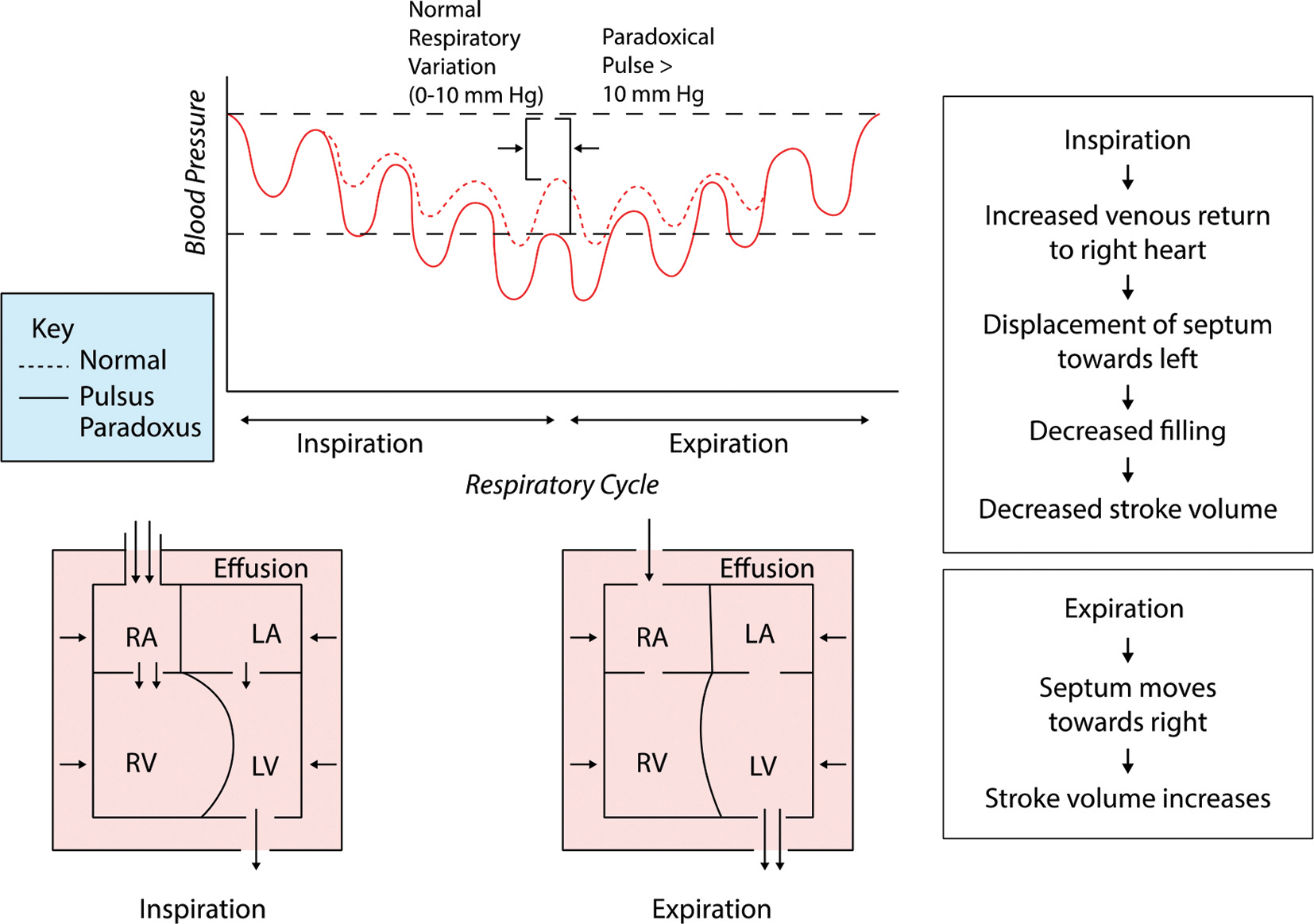
Pulsus paradoxus is a misnomer, meaning that it is not reversal of the normal but, in fact, exaggeration of the normal fall in systolic blood pressure (SBP) during inspiration (normally 4–5 mm Hg). This term was first introduced by Adolf Kussmaul (1983) to describe marked inspiratory fall in the SBP, which is associated with chronic constrictive pericarditis (CCP). Clinically, the term pulsus paradoxus applies to an exaggerated inspiratory fall in SBP > 10 mm Hg, which occurs due to left ventricular underfilling (Fig. 1).

-
Fig. 1 Inspiratory fall of systemic arterial pressure.
Fig. 1 Inspiratory fall of systemic arterial pressure.
Common to all pericardial diseases, the underlying mechanism is the smaller LV diastolic volumes that are produced during inspiration which, in turn, reduce the stroke volume and a subsequently increased fall in SBP.
It is important to appreciate that RA/RV/LV are intrapericardial but LA is extrapericardial. In CCP, there is dissociation of intrathoracic pressure from intrapericardial chambers, due to thickened and fibrosed pericardium; consequently, negative intrathoracic pressure is transmitted to extrapericardial structures–LA (fall in LA pressure) but not to intra pericardial structures like LV. Consequently, negative gradient results between LA and LV–LA pressure is lower than LV pressure, resulting in underfilling of LV; consequently, low-stroke volume and fall in SBP .
In contrast, among patients with cardiac tamponade, negative intrathoracic pressure is transmitted to intrapericardial chambers RA/RV/LV and better filling of RA/RV. Because of limited pericardial space in tamponade, RV fills at expense of LV filling, resulting in underfilling of LV–low-stroke volume and fall in SBP.
Thus, pulsus paradoxus in cardiac tamponade is due to exaggerated ventricular interaction, whereas in CCP, it is due to dissociation of intrathoracic pressure from intrapericardial chambers.
Answer by Prof. Sampath
Pulsus paradoxus (parodoxic pulse or paradoxical pulse) is an abnormally large decrease in stroke volume, systolic blood pressure (SBP), and pulse wave amplitude during inspiration.
Decrease in SBP by more than 10 mm hg on inspiration is diagnostic.
How to measure pulsus paradoxus: difference between two pressures on sphygmomanometer when
-
Onset of Korotkoff sounds (expiration only).
-
Korotkoff sounds are audible throughout the respiratory cycle.
Cardiac tamponade: Pulses paradoxus is commonly seen in cardiac tamponade, due to the intact cardiac transmission of respiratory variations of intrathoracic pressure.
Key underlying pathophysiology in cardiac tamponade: Cardiac transmission of respiratory variations of intrathoracic pressures are maintained (Fig. 2).
-
Fig. 2 Diagrammatic representation of mechanism of pulsus paradoxus in cardiac tamponade.
Fig. 2 Diagrammatic representation of mechanism of pulsus paradoxus in cardiac tamponade.
Causes of absent of pulsus paradoxus in cardiac tamponade are as follows:
Aortic regurgitation, atrial septal defect, severe LV dysfunction, LV hypertrophy, RV hypertrophy, severe hypotension, pericardial adhesions, and localized effusion.
Chronic constrictive pericarditis (CCP): Pulsus paradoxus is usually absent in CCP due to the absence of cardiac transmission of respiratory variation of intrathoracic pressure secondary to fibrous nonelastic pericardium.
It may be seen in effusive variant of CCP, which constitutes around 20% of total CCP.
Pulsus paradoxus in effusive CCP:
Visceral pericardium is fixed and fibrous, encasing heart in a contracted, nonelastic pericardium, which prevents transmission of negative intrathoracic pressure during inspiration to the heart, limiting ventricular filling during late diastole when pericardium has reached its elastic limit. When there is a concomitant effusion, ventricular filling is impeded during the entire diastolic cycle due to the tamponading effect of the effusion. Under a tense pericardium, an effusion, which may have otherwise been unnoticeable, mimics signs of tamponade in effusive CCP.
Due to tamponading effect of the overlying effusion, with underlying tense pericardium, there will be an exaggerated compression of the left ventricle by the deviated septum during right ventricular filling secondary to chamber interdependence in limited pericardial space, which leads to pulsus paradoxus.
Reverse pulsus paradoxus: Increase in SBP with inspiration.
Example: hypertrophic cardiomyopathy (HOCM), isorhythmic atrioventricular (AV) dissociation, and intermittent positive pressure ventilation.
Q3. JVP and its Variation in Constrictive Pericarditis and Restriction Cardiomyopathy–Hemodynamic Implications of Abnormal Waves
Answer by Prof. Dayasagar Rao
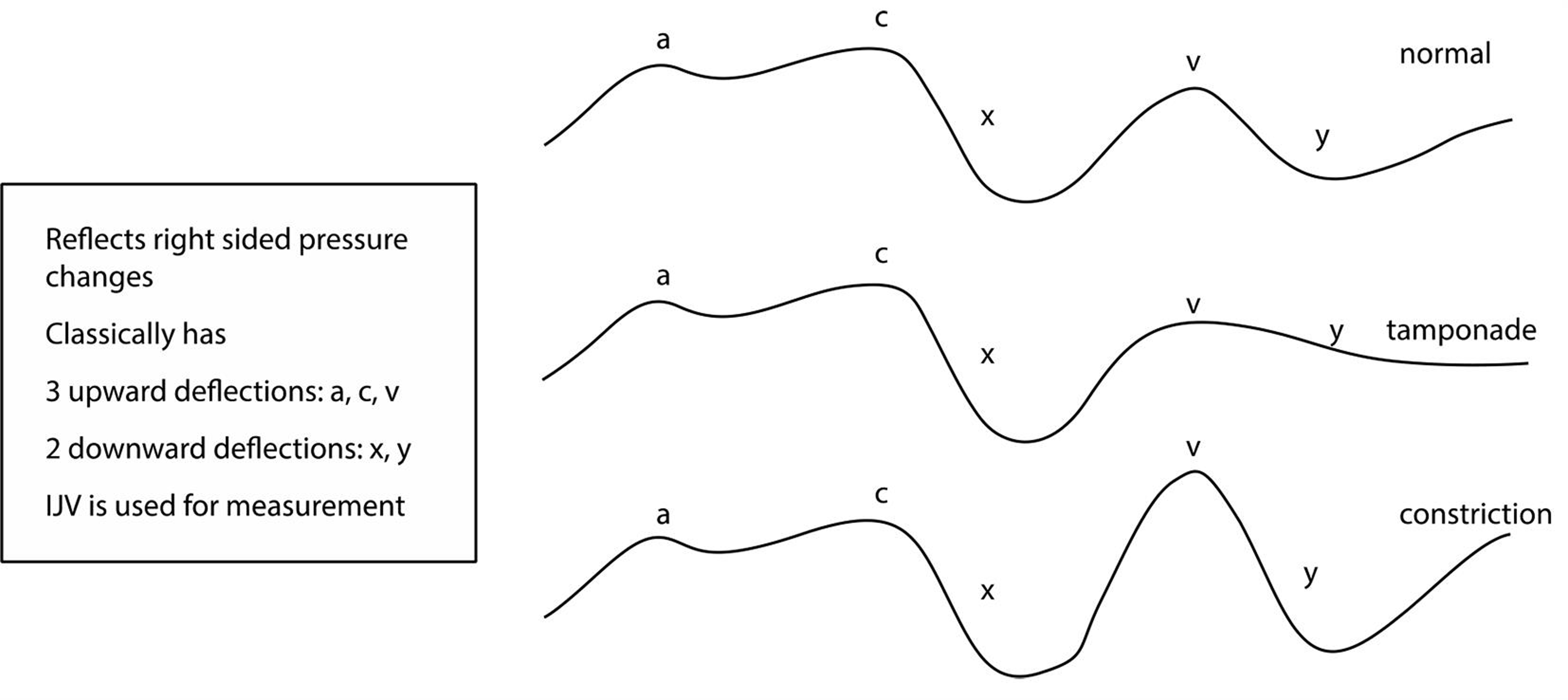
Jugular venous pressure (JVP) abnormalities reflect changes in right side of the heart.
Chronic constrictive pericarditis (CCP) is a pathological condition with encasement of the heart by a thickened pericardium, leading to secondary abnormalities in chamber filling and resultant lower cardiac output. On the other hand, restrictive cardiomyopathy is the primary disease of cardiac myocardium, characterized by increased myocardial stiffness and thus elevated intracardiac pressures. Shared among these disorders is diastolic dysfunction of ventricles, with preserved systolic function in pure constrictive pericarditis, whereas in restrictive cardiomyopathy, systolic dysfunction is also present in majority.
Two hemodynamic features are seen in CCP:
-
Dissociation of intrathoracic pressure from intrapericardial chambers.
-
Exaggerated ventricular interactions are present in CCP only and form the basis of marked respiratory variation in constriction.
Audible arteriovenous (AV) valve regurgitation may be present in restrictive cardiomyopathy but unusual in CCP.
Thus, JVP reflects the restrictive ventricular diastolic dysfunction–elevated JVP, which either fails to fall or increases on inspiration. Kussmaul’s sign is classical of CCP, but can also occur in patients with severe RV dysfunction in restrictive cardiomyopathy.
Exaggerated “X” and “Y” descent is a rule in constriction (Fig. 3) but blunted (even obliteration of ‘X’) in restrictive cardiomyopathy, consequent to RV systolic dysfunction or significant tricuspid regurgitation. The “A” & “V” waves are insignificant.
-
Fig. 3 JVP tracing in normal and constrictive pericarditis.
Fig. 3 JVP tracing in normal and constrictive pericarditis.
Answer by Prof. Sampath
Jugular venous pressure (JVP) indicates right atrial pressure waveform.
Chronic Constrictive Pericarditis (CCP)
Key underlying pathophysiology in CCP: Rigid tough pericardium limits filling of heart chambers. Table 1 mentioned the JVP in normal condition and in constrictive pericarditis with its hemodynamic explanations.
|
Parameter of JVP |
Normal JVP–hemodynamics |
Constriction–JVP findings |
Constriction–hemodynamic implication |
Secondary to |
|---|---|---|---|---|
|
Abbreviations: CCP, chronic constrictive pericarditis; JVP, jugular venous pressure. |
||||
|
JVP |
< 3 cm above sternal angle |
Elevated |
Limited filling of heart chambers |
Rigid pericardium |
|
A waves |
Atrial contraction |
Normal/may be prominent |
Normal or increased atrial contraction |
Diastolic dysfunction |
|
X descent |
Active ventricular filling |
Prominent |
Enhanced active ventricular filling |
Impaired passive ventricular filling |
|
V wave |
Atrial filling |
Usually equal to a wave |
Enhanced atrial filling |
Increased pulmonary pooling, increased pulmonary vein to left atrium gradient |
|
Y descent |
Passive ventricular filling |
Rapid descent |
Diastolic filling restricted to early diastole |
Restricted ventricular filling in mid and late diastole due to underlying rigid pericardium |
Restrictive Cardiomyopathy
Key underlying pathophysiology: Rigid myocardium limits filling of ventricular chamber which leads to the following:
-
Increased diastolic pressure.
-
Decreased ventricular filling.
JVP is elevated in later stages of restrictive cardiomyopathy secondary to limited filling of heart chambers. A wave is prominent secondary to enhanced atrial contraction with diastolic dysfunction with normal V wave, X descent, and Y descent. Normally,central venous pressure decreases with inspiration. Kussmaul’s sign–Increase or absence of increase in central venous pressure during inspiration. In Table 2, the JVP comparison with CCP, restrictive cardiomyopathy and cardiac tamponade is mentioned.
|
JVP |
Constrictive cardiomyopathy |
Restrictive cardiomyopathy |
Cardiac tamponade |
|---|---|---|---|
|
Abbreviation: JVP, jugular venous pressure. |
|||
|
Jugular venous pressure |
Elevated |
May be Elevated |
Elevated |
|
A waves |
Normal/may be prominent |
Prominent |
Never prominent |
|
V waves |
Usually equal to a wave |
Normal |
Normal |
|
X descent |
Prominent |
Normal |
Normal |
|
Y descent |
Rapid |
Normal |
Decreased or absent |
|
Kussmaul’s sign |
Usually positive |
May be positive |
Negative, may be positive |
When there is uncertainty of diagnosis, constriction or restriction, then cardiac catheterization may be helpful in constriction (Fig. 4). Sometimes, even after cardiac catheterization, to differentiate between these two conditions becomes difficult.

-
Fig. 4 Right and left ventricular curves on cardiac catheterization in constriction.
Fig. 4 Right and left ventricular curves on cardiac catheterization in constriction.
Conflicts of Interest
None declared.






