Translate this page into:
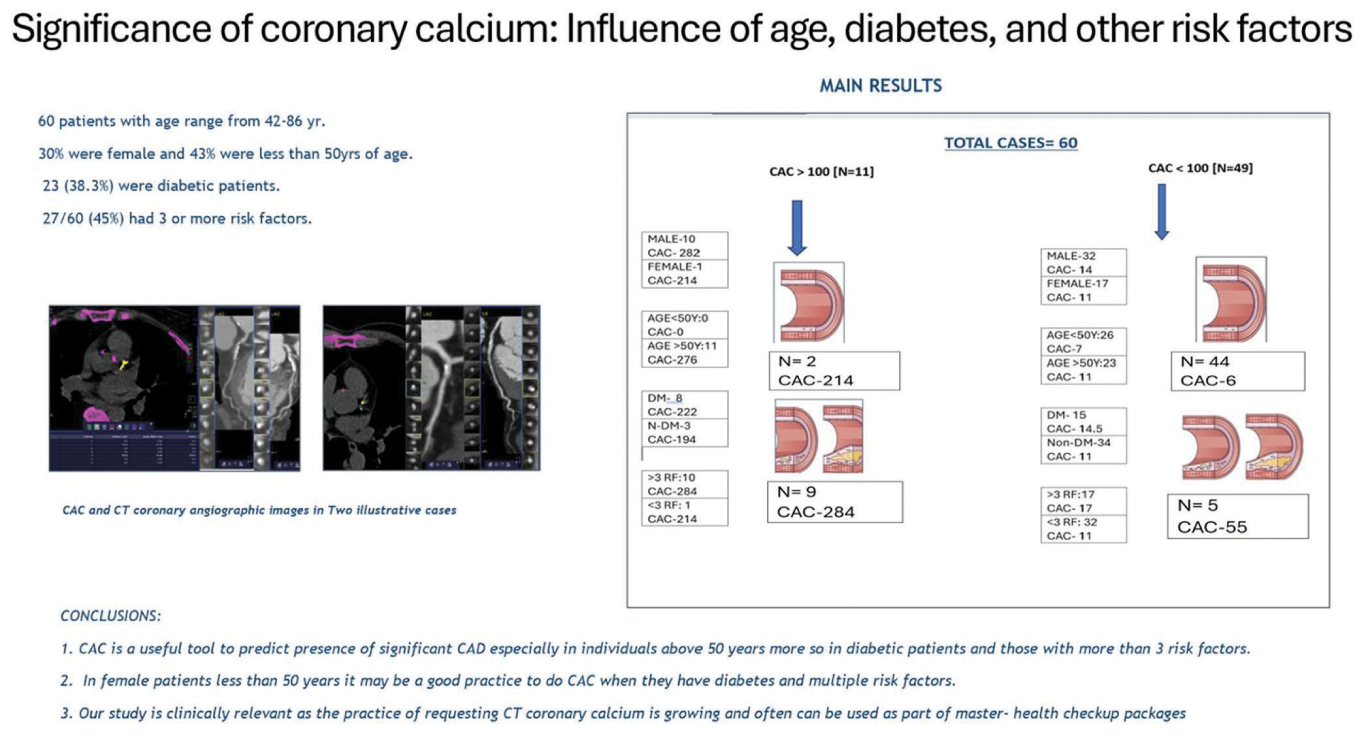
Significance of Coronary Calcium: Influence of Age, Diabetes, and Other Risk Factors
*Corresponding author: Sujata Patnaik, Department of Radiology, Nizam’s Institute Of Medical Sciences, Hyderabad, Telangana, India. sujata_patnaik222@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Chandran A, Patnaik S, Yarlagadda J. Significance of Coronary Calcium: Influence of Age, Diabetes, and Other Risk Factors. Indian J Cardiovasc Dis Women. doi: 10.25259/IJCDW_74_2024
Abstract
Objectives:
To evaluate the predictive value of Computed Tomography coronary artery calcium (CAC) in assessing the atherosclerotic coronary artery disease; also analyze the influence of age, diabetics and other risk factors on its predictive accuracy
Material and Methods:
Total 60 patients were studied over 18 months who were categorized based on CAC scores and with reference to age, diabetes and presence of more than three risk factors. The corresponding angiographic severity of the coronary lesions was noted. The patients were divided into Group-I: non-obstructive coronary artery disease-(CAD ) and Group-II: Obstructive CAD. The diameter stenosis was used as per standard practice to quantify CAD.
Results:
The subjects were in the age range: 42-86 years; 43% being less than 50 years. Eighteen of the 60 patients were females. 23 (38.3%) were diabetic patients. 27 of the 60, had 3 or more risk factors. Eleven had CAC > 100 and ten of them had significant CAD. In contrast only 5 out of 49 patients (10%) with CAC < 100 showed significant CAD. Higher the CAC score is more the degree of CAD particularly in patients aged > 50 years, diabetes and those with > 3 risk factors. The mean score was 206 in those with significant CAD compared to 14.5 in those with insignificant CAD.
Conclusions:
CAC is a reliable tool for predicting significant CAD, especially in patients aged > 50 years, diabetes and those with multiple risk factors. Even in patients < 50 years, CAC may be recommended when obstructive disease is suspected, particularly in women with diabetes or multiple risk factors. Further larger trials are suggested to substantiate our conclusion.
Keywords
Agatston score
Calcium score
Predictor of CV disease
Stable plaque
Sub-clinical atherosclerosis
ABSTRACT IMAGE
INTRODUCTION
The detection of coronary calcium was recognized as a marker for atherosclerosis as early as 1940. But only by, 1990, its measurement was standardized on computed tomography (CT) scan and was named as Agatston score. The original Agatston score was designed for electron beam CT estimation of calcium over the coronaries but subsequently was adapted to the new generation multi-detector computerized tomography (MDCT) scanners.[1] Over the next few years the Agatston score was validated as a reliable maker to detect the presence of atherosclerosis and elevated scores correlated with future cardiac events.[2] At present, the CT coronary artery calcium (CAC) is an accepted parameter to predict the likelihood of obstructive coronary disease in asymptomatic patients.[2] There are a few studies suggesting that the higher scores correlated with more aggressive coronary artery disease. It is a utility to monitor plaque progression while statin therapy is also recognized.[3] Our study is aimed to find out if Agatston score can predict the extent of the coronary artery disease (CAD) and if its predictive value is influenced by age, diabetes, or other risk factors.
MATERIALS AND METHODS
All willing patients with symptoms suspecting coronary artery disease, those needing computerized tomography based coronary artery angiography (CT-CAG) for pre-operative evaluation and those needing screening of coronary artery disease referred for coronary CT angiography were included in the study. The study period was 18 months. Informed consent was obtained before examination. Patients were asked to fast 4 h and were not allowed to have caffeine for 12 h before examination. Metformin was suspended on the day of examination and at least 48 h after contrast administration. Patients were asked to continue other regular medications. History of allergy was obtained and appropriate precautions were taken. 18G catheter was put in the antecubital vein. Oral metoprolol 50–100 mg was given 1 h before scan if the heart rate was high. Heart rate was maintained at <65 b/min. Intravenous metoprolol was given immediately before examination if required to control HR. 400–800 mcg of nitroglycerine sublingual tablet 5 min before coronary angiogram (CAG) was routinely used. The patient was asked to hold breath for 5–10 s. Electro cardiogram (ECG)-gated prospective scanning was done from below arch to base of heart. Voltage of 120 kV and 560 mA was used. Scan was done on 128 slice CT Somatom Definition AS+. At a rate of 5–7 cc/per second of 350–370 mg/mL, 80–100 mL of non-ionic iodinated contrast was injected. Bolus tracking was done with attenuation of 100 HU in ascending aorta.
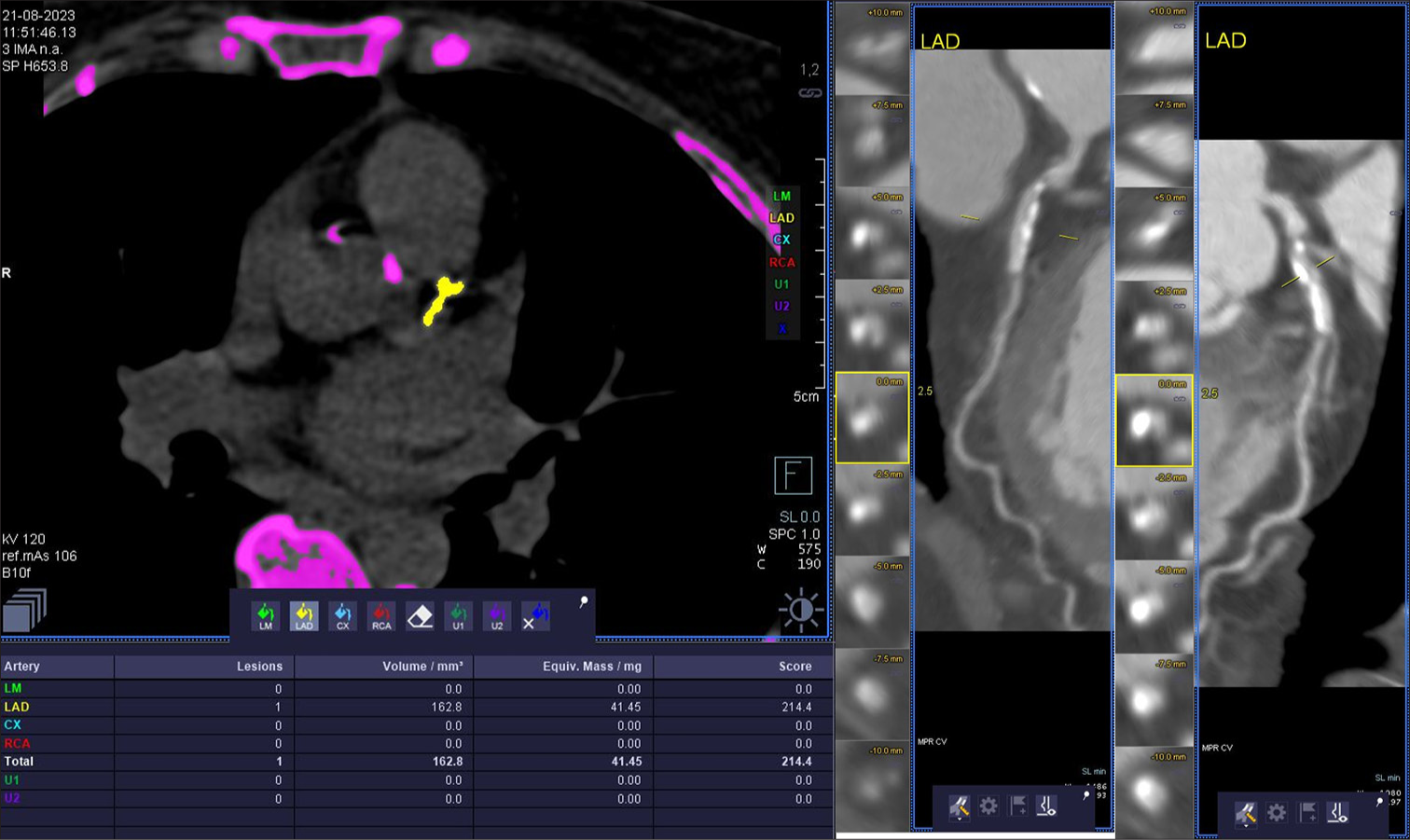
Calcium scoring (CAC) was obtained with software provided by Siemens. CAC of each coronary artery is summated to get the final score. Based on density, factor scores were given. multiplanar reconstruction (MPR), curved MPR, maximum intensity projection (MIP), and volume-rendered tomography (VRT) images were reconstructed. Overall, the extent of CAC was categorized as 0 – Absent CAC; 1–100; moderate – 101–300; Severe – 301–999, and extensive – >1000. Quantitative stenosis estimation was done on analysis of curved MRP images, followed by cross-sectional and longitudinal sections to measure the diameter and quantitate the stenosis. Those with more than 400 scores were excluded from the analysis.
Patients are divided into two groups based on the degree of stenosis – Group I: No atherosclerosis/non-obstructive lumen/narrowing <50% diameter stenosis and Group II: Obstructive lumen (>50% diameter stenosis). Patient are said to have significant CAD if any one or more than one epicardial vessel shows >75% diameter stenosis and the left main has >50% diameter stenosis.
RESULTS
There were 60 patients with 18 females (30%). The age ranged from 42 to 86 years. 26 (43%) were aged <50 years. 23 (38.3%) were diabetic patients. 27/60 (45%) had 3 or more risk factors. CAC values obtained in our study are detailed in Table 1. Eleven of the 60 (18.3%) had CAC > 100. Fifteen patients (25%) showed significant obstructive CAD. 10 of the 11 (91%) who had CAC > 100 showed significant CAD. Of the rest 49 with CAC < 100, only 5 (10%) showed significant CAD. The relationship between age and diabetic status was analyzed in Table 2. Among those >50 years, those with diabetes 12/18 (66%) showed significant CAC compared to 6/16 (37%) among the non-diabetics.
| CAC | CAC>100 | CAC<100 | ALL | |||
|---|---|---|---|---|---|---|
| Number | Mean CAC | Number | Mean CAC | Number | Mean CAC | |
| Male | 10 | 282 | 32 | 14 | 42 | 77 |
| Female | 1 | 214 | 17 | 11 | 18 | 22 |
| <50 years | 0 | 0 | 26 | 7 | 26 | 7 |
| >50 years | 11 | 276 | 23 | 11 | 34 | 94 |
| DM | 8 | 222 | 15 | 14.5 | 23 | 86 |
| Non-DM | 3 | 194 | 34 | 11 | 37 | 26 |
| Risk factors >3 | 10 | 284 | 17 | 17 | 27 | 115 |
| Risk factors <2 | 01 | 214 | 32 | 11 | 33 | 17 |
| Significant CAD | 10 | 284 | 05 | 55 | 15 | 207 |
| Insignificant/No CAD | 1 | 214 | 44 | 6 | 45 | 11 |
DM: Diabetes mellitus, CAD: Coronary artery disease
| Groups | Males number (mean CAC) | Females number-(mean CAC) | Remarks |
|---|---|---|---|
| In those with CAC >100 | 10 (284) | 1 (214) | Men are 10 times predominant and the mean score was higher |
| In those with CAC <100 | 32 (14) | 17 (11) | |
| Those <50 years | 21 (21) | 5 (11) | Irrespective of age, men showed higher scores than women |
| Those >50 years | 25 (109) | 9 (44) |
CAC: Coronary artery calcium
Among those <50 years of age, in those with CAC >100, 2/22 (9%) had CAD [Tables 1 and 3]. One is a diabetic with 2 other risk factors (RFs). His CAC was 52. Another male patient was non-diabetes but had 3 RF and CAC was 71. He showed significant CAD. In the group with significant CAD, the mean CAC was 206 as against 14.5 in those with insignificant CAD. Higher age, diabetes, and presence of >3 risk factors seem to be associated with higher CAC and significant CAD. The presence of significant CAD was directly correlated with the CAC value [Tables 4 and 5]. CT scan images of two illustrative cases from our study are illustrated below [Figures 1 and 2].
| Category | Aged <50 years | Aged >50 years | ||
|---|---|---|---|---|
| Number | Mean CAC | Number | Mean CAC | |
| All patients-Mean CAC | 26 | 20 | 34 | 101 |
| Male (No and mean CAC) | 21 | 21 | 25 | 109 |
| Female (No and mean CAC) | 5 | 11 | 9 | 44 |
| DM (No and mean CAC) | 5 | 19 | 18 | 124 |
| Non-DM (No and mean CAC) | 21 | 20 | 16 | 75 |
| Significant CAD | 2 | 42 | 12 | 255 |
| Insignificant CAD | 24 | 12 | 22 | 34 |
CAD: Coronary artery disease, CAC: Coronary artery calcium
| CAC groups | Number of RF | Significant CAD | Insignificant CAD | Total |
|---|---|---|---|---|
| CAC<100 (n=49) | >3 RF | 3 (17.6%) | 14 | 17 |
| 1 or 2 RF | 2 | 30 | 32 | |
| CAC>100 (n=11) | >3 RF | 9 (90%) | 1 | 10 |
| 1 or 2 RF | 0 | 1 | 1 |
CAD: Coronary artery disease, CAC: Coronary artery calcium, RF: Risk factors
| CAC - Range; Number | Significant CAD | Insignificant CAD | Remarks |
|---|---|---|---|
| <50 (41) | 1 | 40 | Higher CAC is associated with more incidence of significant CAD |
| 50–100 (5) | 3 (60%) | 2 | |
| 100–200 (5) | 3 (60%) | 2 | |
| 200–300 (5) | 4 (80%) | 1 | |
| 300–400 (4) | 4 (100%) | 0 | |
| Total | 15 | 45 |
CAD: Coronary artery disease, CAC: Coronary artery calcium
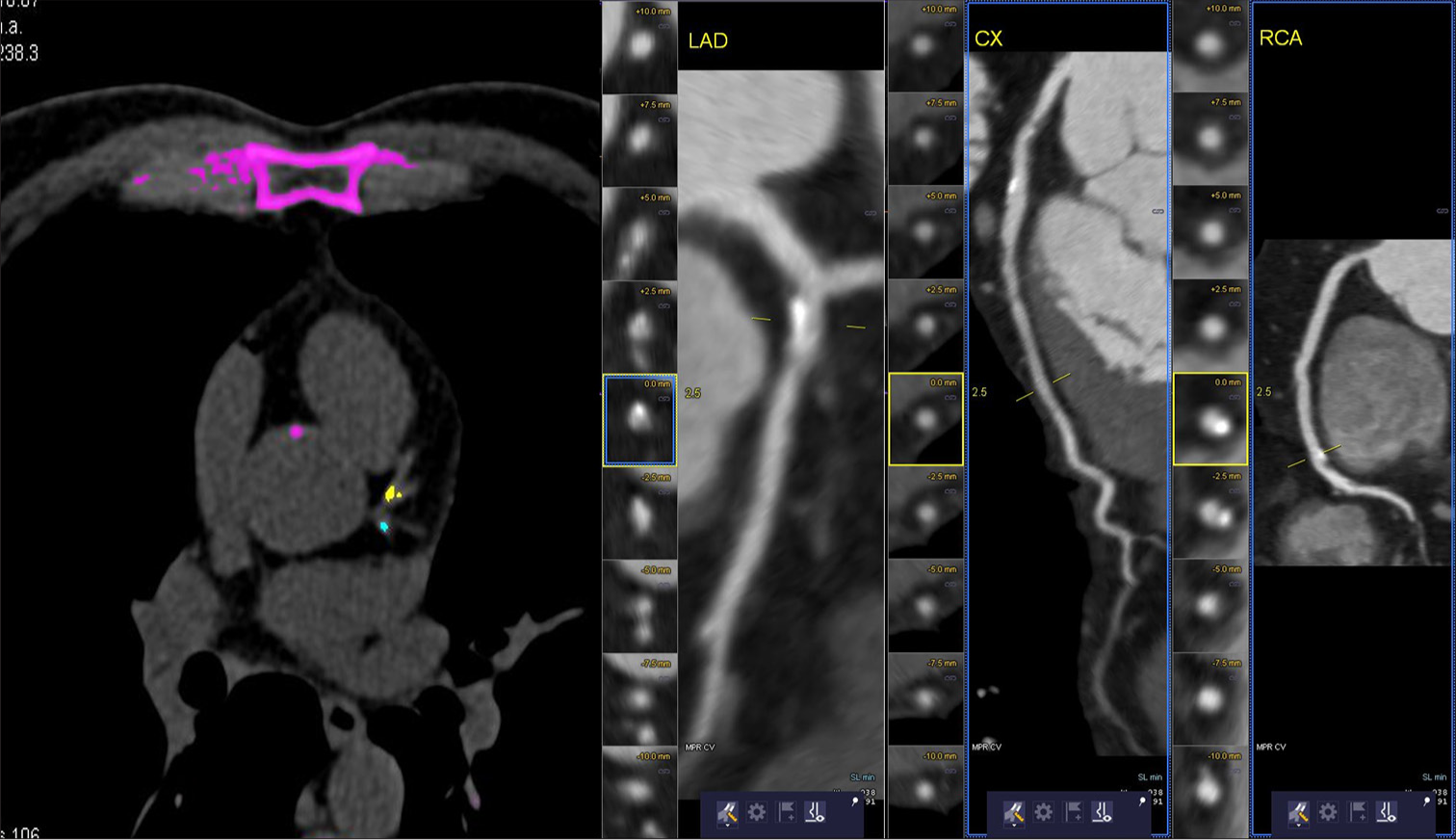
- 65 year old female patient with computed tomography coronary calcium score of 214. There is eccentric calcified plaque in the proximal left anterior descending artery causing a 50% block. She had 3 risk factors.
- 61 year-old male patient with calcium score of 131. There is no significant block on CT-coronary angiogram. He had 4 risk factors.
DISCUSSION
Despite the introduction of several modifications, the traditional Agatston score remained simple and time-tested CAC to assess atherosclerotic burden. Expert committees continue to endorse its use for risk prediction of asymptomatic individuals, to decide on the need to start statins, and to decide on the need for depiction of coronary arteries and lesions.[4] Age, diabetes, and other coronary risk factors influence the genesis and progression of atheromatous plaque. Hence, it is important to interpret the calcium score with respect to the age and presence of diabetes and other coronary risk factors when used to predict atherosclerosis in asymptomatic patients. Latest American Heart Association (AHA) guidelines recommended measuring CAC if the decision is uncertain in the age group of 40–75 years based on atherosclerotic cardiovascular disease (ASCVD) risk estimation to start statin therapy as primary prevention. Among those with intermediate risk, when the calcium score is zero, if there is no.
Diabetes, family history, or smoking statins are not recommended. With scores of 1–99 in persons above 55 years, statins are favored. When score is >100, statins are recommended.[5]
In South-Asians, the atherosclerosis manifests at an earlier age, even in the absence of traditional risk factors.[6] It is a common practice not to advise CAC as a screening test in individuals <50 years. In our study, we excluded those with symptoms or those with CAC >400. Eight out of 11 (72.7%) having high calcium scores have significant CAD, while 7 out of 49 (14.3%) have significant CAD with scores <100. Patients <50 years were 26 and rest were >50 years. In Coronary Artery Risk Development in Young Adults (2017), a prospective community-based study, it was observed that CAC of 100 or above is linked with high risk of mortality. Adults under the age of 50 years, who have any CAC found on CT scan, are at an increased risk of clinical coronary heart disease (CHD), CVD, and mortality even with low score.[7] This correlates with our observation. We had four cases of significant CAD with CAC of 3–50 agaston units (AU). Four out of 60 patients are non-diabetic and had scores of 0–64 AU having significant CAD. Three of them have multiple risk factors. It suggests that even those below 50 years can have higher CAC if they have diabetes or multiple risk factors.
There are some limitations to the traditional CAC score. There are efforts to further enhance its validity by looking at its distribution pattern (diffuse or concentrated), total CAC lesions, mean density, and quantification of extra coronary calcification. Efforts are also focusing on the radiation involved without compromising the quality of reports. CAC is found to be a better prediction tool than high-sensitivity C-reactive protein (hs-CRP) or carotid–intima media thickness (CMT) for cardiovascular events.
The Multi-Ethnic Study of Atherosclerosis (MESA) had designed a coronary heart disease (CHD) score, by taking factors such as age, gender, CAC, race, diabetes, current smoking, family history of CHD, total cholesterol, high-density lipoprotein, systolic blood pressure, and use of hypertension/lipid-lowering medications. This predicts 10-year CHD risk and was found very useful for age ranges 45–85 years.[7] We found that traditional CAC is simple to use and when correlated with age, presence of diabetes, or more than 3 risk factors, it can predict possible CAD in asymptomatic adult patients irrespective of their age. Our study is clinically relevant as the practice of requesting CT coronary calcium is growing. The cost of the test is about INR 1.5–2K and is often a part of master health check-up packages.
At present, newer trials are being conducted to fill the gaps in evidence for CAC-based primary prevention strategies.[8] The DISCHARGE trial published in 2024 included 3561 patients with stable chest pain and randomized to either invasive coronary angiogram or CT angiogram. Those who had CAC score of 0 had very low incidence of major adverse cardiac events (MACE) (hazard ratio −0.08) compared to those with 400 or more score (hazard ratio −1). This study highlights the predictive role for MACE in patients with stable angina.[9]
Our small observational study involving Indians suggested that the cut-off for initiating statins in those with CAC < 100 needs to be further lowered in diabetic patients or in presence of multiple other risk factors. Our study suggests a larger trial on this aspect. We also propose that whenever obstructive CAD is suspected in women <50 years in presence of diabetes or multiple risk factors CAC should be advocated, though it is not a common current practice.
CONCLUSION
CAC is a useful tool to predict presence of significant CAD, especially in individuals above 50 years more so in diabetic patients and those with more than 3 risk factors. In female patients <50 years, it may be a good practice to do CAC when they have diabetes and multiple risk factors.
Ethical approval:
The research/study was approved by the Institutional Review Board at Nizam’s Institute of Medical Sciences, number 1426/2022, dated March 01, 2023.
Declaration of patient consent:
The authors certify that they have taken appropriate patient consent.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Quantification of Coronary Artery Calcium Using Ultrafast Computed Tomography. J Am Coll Cardiol. 1990;15:827-32.
- [CrossRef] [PubMed] [Google Scholar]
- Prediction of Coronary Events with Electron Beam Computed Tomography. J Am Coll Cardiol. 2000;36:1253-60.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical Indications for Coronary Artery Calcium Scoring in Asymptomatic Patients: Expert Consensus Statement from the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr. 2017;11:157-68.
- [CrossRef] [PubMed] [Google Scholar]
- 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140:e563-95.
- [CrossRef] [Google Scholar]
- Cardiovascular Disease Risk and Pathophysiology in South Asians: Can Longitudinal Multi-omics Shed Light? Wellcome Open Res. 2021;5:255.
- [CrossRef] [PubMed] [Google Scholar]
- Application of a Lifestyle-Based Tool to Estimate Premature Cardiovascular Disease Events in Young Adults: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. JAMA Intern Med. 2017;177:1354-60.
- [CrossRef] [PubMed] [Google Scholar]
- Role of Coronary Artery Calcium Score of Zero and Other Negative Risk Markers for Cardiovascular Disease: The Multi-Ethnic Study of Atherosclerosis (MESA) Circulation. 2016;133:849-58.
- [CrossRef] [PubMed] [Google Scholar]
- Filling the Evidence Gaps Toward a Coronary Artery Calcium-Guided Primary Prevention Strategy. JAMA Cardiol. 2025;10:411-3.
- [CrossRef] [PubMed] [Google Scholar]
- Coronary Artery Calcium Score Predicts Major Adverse Cardiovascular Events in Stable Chest Pain. Radiology. 2024;310:e231557.
- [Google Scholar]







