Translate this page into:
Salt Perception Threshold and Vascular Risk in Prehypertensive Women Compared to Normotensive and Hypertensive Women
*Corresponding author: Vidya Ganji, Department of Physiology, All India Institute of Medical Sciences, Hyderabad, Telangana, India. docvidyaganji@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ganji V, Taranikanti M, Umesh M, Kalpana M, Vamshidhar IS, John NA, et al. Salt Perception Threshold and Vascular Risk in Prehypertensive Women Compared to Normotensive and Hypertensive Women. Indian J Cardiovasc Dis Women. 2024;9:59-65. doi: 10.25259/IJCDW_68_2023
Abstract
Objectives:
To evaluate and compare the Salt perception threshold and vascular stiffness in pre-hypertensive women with that of normotensive and hypertensive women.
Materials and Methods:
Study design – This was a cross-sectional study. A total of 440 adult females in the age group of 25–60 years from urban and rural areas were included in the study. After initial screening, the subjects were divided into three groups. Group I: Prehypertensive females; Group II: Hypertensive females; and Group III: Normotensive females. Salt perception threshold was determined by salt impregnated taste strips with sodium chloride at different concentrations. Vascular stiffness of the subjects was measured and compared using an oscillometric non-invasive arteriography.
Results:
The salt intake was higher by 2.1 g/day in Group I females and 5.6 g/day in Group II females when compared to Group III females. The salt detection threshold and SPT were higher significantly in pre-hypertensive females and much higher in hypertensive females compared to normotensive females. The mean values of brachial ankle pulse wave velocity (BaPWV) and carotid femoral pulse wave velocity (CFPWV) were found to be significantly higher in Group I females compared to normotensives.
Conclusion:
High SPT in prehypertensive females will lead to high consumption of salt to achieve taste satisfaction. A progressive reduction of salt in food is recommended in these females would significantly decrease the percent progression of pre-HTN to HTN decreasing the risk for cardiovascular morbidity.
Keywords
Salt perception threshold
Vascular stiffness
Pulse wave velocity
Prehypertensive women
Hypertension
Cardiovascular risk
ABSTRACT IMAGE
INTRODUCTION
Cardiovascular diseases (CVDs) represent the main cause of population morbidity and mortality worldwide. Although the incidence of CVD is lower in women than men, women have a higher mortality and worse prognosis after acute cardiovascular events. The risk of CVD in women is often underestimated due to misperception that women are more protected than men against CVD. These gender differences have caused concerns for prevention of CVD in women. Hypertension (HTN) and unhealthy diet are among the major risk factors for CVD. The development of HTN depends on complex interaction between genes and environmental factors.[1] Numerous studies have demonstrated a causal relationship between excessive salt intake and essential HTN leading to increased cardiovascular morbidity.[2,3] Prehypertension (pre-HTN) defined as systolic blood pressure (SBP) 120–139 mmHg and diastolic blood pressure (DBP) 80–89 mmHg is an early condition that precedes HTN. The risk of cardiovascular morbidity and mortality is 1.6–2 times greater in pre-hypertensives than normotensives even without progression to HTN.[4,5] The global mean sodium intake in 2010 was about 4 g/d (salt ≈ 10 g/d) in adults and is especially higher in India where the consumption of salt intake is approximately 10 g/day.[6] The World Health Organization recommends a sodium reduction of <2 g/day in adults and the current HTN guidelines recommend reducing the sodium intake as an important and simple strategy to reduce HTN and a way of a lifestyle modification.[7] Eventual progression of pre-HTN to HTN and development of stroke and left ventricular hypertrophy has been projected in several studies with high incidence of stroke in India.[8]
Evidence from clinical studies suggested an association between regular dietary salt intake and arterial vascular stiffness. Pulse wave velocity (PWV) is the gold standard for arterial stiffness which correlates well with Framingham risk score and is considered a good predictor of cardiovascular events.[9] Vascular stiffness is a pathological process of change in structure and function of arterial wall that changes mainly with age but high salt consumption is also linked to increased arterial stiffness. These changes in arterial wall are believed to be induced by both reduced bioavailability of nitric oxide and a deficient response of local renin-angiotensinaldosterone system to high sodium consumption. Several studies have shown occurrence of increased carotid artery intimal-thickness and coronary atherosclerosis in prehypertensive stage itself.[10,11] In addition, massive salt restrictions experiments and clinical research have found that the reduction of salt intake not only reduces blood pressure but also alleviates arterial stiffness which is independent of anti-hypertensive effect suggesting that salt load may directly affect vascular stiffness.[12] However, most of the studies done in this subject were on white population and very few studies were done in the Asian population and fewer in the Indian population.
Since high salt intake has such a large impact on global health, it is important to figure out the factors contributing to high salt intake. Evidence suggests that increased salt intake dulls the taste of salt.[13] Hence, measuring the salt taste perception threshold is helpful to detect individuals with increased salt intake. Salt perception threshold (SPT) means how sensitively an individual perceives salt taste and it is a factor influencing salt intake. Few studies have shown that lower salt taste perception and high SPT was associated with higher salt intake and higher prevalence of HTN.[14,15]
The prevalence of pre-HTN and HTN is very high in Indian women and there is little data available about the salt-taste sensitivity, amount of salt intake, and its association with arterial stiffness in pre-HTN and HTN females in the Indian population. Even though pre-HTN is not yet considered as a disease, its early detection can prevent the risk of development of HTN and cardiovascular risk[16,17] using effective screening strategies. The adoption of lifestyle interventions is limited in the Indian population and there is little data available on SPT, amount of salt intake, and arterial stiffness in pre-HTN. A moderate reduction in dietary salt intake might be cardioprotective and prevent progression of pre-HTN to HTN. Thus, in the present study, we tried to address the knowledge gap and to determine the relationship of SPT with arterial stiffness in prehypertensive women and compare those with hypertensive and normotensive women.
Objectives
The objective of this study was to evaluate and compare the Salt perception threshold (SPT) and vascular stiffness in pre-hypertensive women with that of normotensive and hypertensive women.
MATERIALS AND METHODS
Study design
This was a cross-sectional study.
A total of 430 adult females in the age group of 25–60 years from urban and rural areas of Bibinagar were included in the study.
Exclusion criteria
Women below 25 years and above 60 years, women with history of diabetes mellitus, obesity (body mass index [BMI] >30), dyslipidemia, pregnancy, breast feeding, on oral contraceptive pills, impaired renal function tests, and clinical evidence of cardiovascular disease which may alter the vascular endothelial function were excluded from the study. Women with history of smoking, history of active drug or chronic alcohol use, consumption of coffee or juice within 2 h before the test, those having blocked nose, and other conditions that might alter taste perception were excluded from the study.
Data collection procedure and tools used
The study was conducted after approval of the Institutional Ethics Committee (AIIMS/BBN/IEC/JUNE/2023/279-R). An informed consent was obtained from the participants after explaining the purpose of the study and a questionnaire was given to all the participants to acquire knowledge on dietary behaviors, frequency of salt consumption, demography, physical activity, and other eating practices.
Individuals coming to the medicine outpatient department were screened for pre-HTN and HTN. The blood pressure was measured as per eighth joint national committee (JNC 8) guidelines using standard mercury sphygmomanometers as per standard protocol. An average of two or more readings at each of two or more visits after initial screening was considered and the subjects were divided into three groups:
Group I: Prehypertensive females (As per American heart association (AHA), Individuals with SBP 120–139 mmHg and diastolic blood pressure (DBP) 80–89 mm Hg); Group II: Hypertensive females (including newly diagnosed Hypertensives) (defined as SBP >140 mmHg and DBP >90 mmHg); and Group III: Normotensive females (systolic blood pressure (SBP) <120 mmHg and DBP <80 mmHg). The SPT consists of an individual’s ability to recognize the salt taste. Taste perception for salt was determined by salt impregnated taste strips with sodium chloride at concentrations of 0, 0.016 g/mL (labeled as L), 0.04 g/mL (labeled as K), 0.1 g/mL (labeled as J), and 0.25 g/mL (labeled as I). The subjects were instructed not to have tea/coffee 2 h before test. The subject’s mouth was washed with distilled water before doing the test. The salt impregnated strip was held in the subject’s mouth for 3 s and the subject was asked whether he or she experienced no taste/any taste. When the subjects replied “some taste,” once, it was defined as salt detection threshold (SDT) – Lowest concentration at which the subject recognized change from no-Na strip to a Na – impregnated test strip. The mouth was washed with distilled water again and the procedure was repeated using the salt strips of higher concentrations of sodium chloride until the subjects replied “salty taste” for two consecutive concentrations. The lower concentration at which the subjects properly reported as “salty taste” in two consecutive strips were defined as values of SPT.
Vascular stiffness of the subjects was measured and compared using an oscillometric non-invasive arteriography. This device used two upper arm cuffs and two lower limb cuffs as a sensor with the cuff pressurized to at-least 35 mmhg over actual systolic pressure. The device determines the brachial ankle pulse wave velocity (BaPWV), carotid femoral pulse wave velocity (CFPWV), arterial stiffness index (ASI), and ankle brachial index (ABI): To assess the stiffness of large arteries. The arteriography also recorded the SBP and DBP, pulse pressure, and heart rate.
Plot of analysis or statistical tools
Characteristics of the study subjects were presented as mean values and standard deviations. Thresholds of salt perception were analyzed using the median detection and recognition categories in each category. The continuous data were analyzed by Mann– Whitney U-test and analysis of variance test for comparison among the three groups. Pearson correlation analysis was done to determine probable correlation relationships among continuous variables. The data were analyzed using SPSS software version 23 and all the probability values for statistical tests with P < 0.05 were regarded as statistically significant.
RESULTS
A total of 430 females in the age group of 20–60 years were included in the study, who were divided into three groups. Group I (n = 130): Pre-hypertensives; Group II (n = 170): Hypertensives; and Group III (n = 130): Normotensives/control. The mean age of the participants in the study for prehypertensives was 38.5 ± 8.6 years, hypertensives was 47.3 ± 9.6 years, and normotensives was 24.9 ± 7.6 years. Most of the women included in Group III were postmenopausal women.
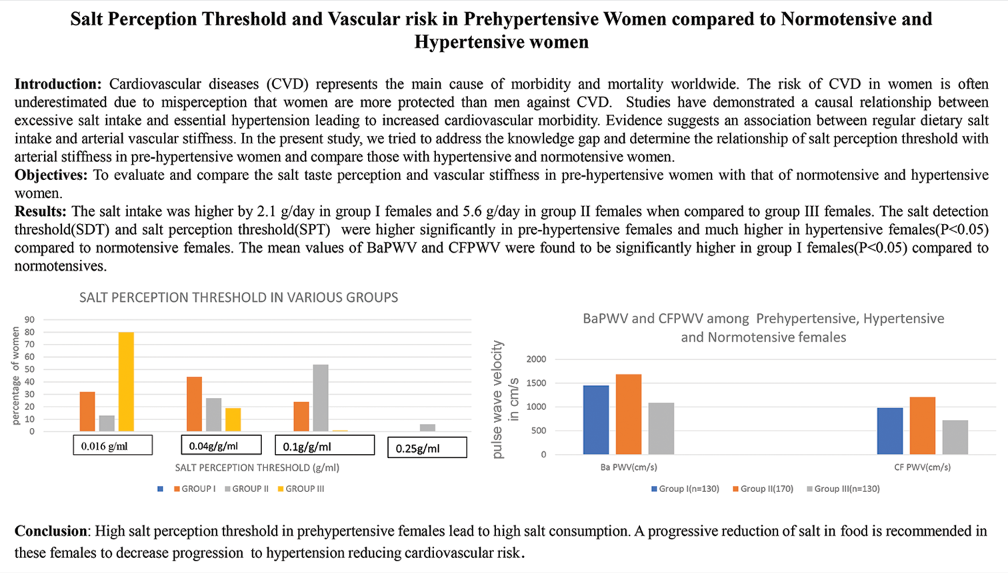
The mean BMI was high but not significant in Group I (preHTN) and higher in Group II (HTN) females compared to controls (Group III), as described in Table 1. The mean values of blood pressure among the three groups are given in Table 1. There was significant increase in pulse pressure in Groups I and II (P < 0.01). The salt intake was higher by 2.1 g/day in Group I females and 5.6 g/day in Group II females than Group III females [Table 2]. It was observed among pre-HTN females (Group I), the proportion of SPT was L (0.016 g/mL) (lowest concentration of NaCl) in 32% of women, K (0.04 g/mL) in 44% and SPT is J (0.01 g/mL) in 24%, whereas among HTN females, SPT was L in 13%, K in 27%, J in 54%, and I in 6% (highest concentration of NaCl) [Table 2]. The SPT among Group III females was L in 80%, K in 19%, and J in 1%. This shows that the SDT and SPT were higher significantly in pre-hypertensive females and much higher in hypertensive females compared to normotensive females suggesting that an association existed between salt taste perception and blood pressure levels [Figure 1]. However, there was no correlation between the salt detection and recognition threshold. It was observed that the frequency of adding salt to food while eating was higher in hypertensive females.
| Variable | Group I (Pre-HTN) (n=130) Mean±SD |
Group II (HTN) (n=170) Mean±SD |
Group III (controls) (n=130) Mean±SD | P-value |
|---|---|---|---|---|
| Age in years | 38.5±8.6 | 47.3±9.6 | 24.9±7.6 | 0.05 |
| BMI kg/m2 | 26.2±2.17 | 27.5±3.01 | 24.7±2.14 | 0.452 |
| SBP (mm Hg) | 127.4±9.54 | 143.8±10.12 | 118±9.32 | <0.001 |
| DBP (mmHg) | 84.7±7.36 | 92.2±8.90 | 78.5±6.12 | <0.001 |
| MABP (mmHg) | 94.8±13.9 | 105.4±14.3 | 86.2±13.6 | 0.001 |
| PP (mmHg) | 44.8±8.62 | 54.2±19 | 40.2±7.11 | 0.01 |
Normally distributed data expressed as Mean±SD. SD: Standard deviation, BMI: Body mass index, SBP: Systolic blood pressure, DBP: Diastolic blood pressure, MABP: Mean arterial blood pressure, PP: Pulse pressure, HTN: Hypertension
| Group | Salt intake (g/day) | SDT (Conc. of NaCl) (g/mL) | SPT (Conc. Of NaCl) (g/mL) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean±SD | 0.016 (L) (%) |
0.04 (K) (%) |
0.1 (J) (%) |
0.25 (I) (%) |
0.016 (L) (%) |
0.04 (K) (%) |
0.01 (J) (%) |
0.25 (I) (%) |
|
| GROUP I Pre-HTN (n=130) |
8.2±1.4 | 37 | 44 | 19 | - | 32 | 44 | 24 | - |
| GROUP II HTN (n=170) |
11.7±2.1 | 12 | 26 | 56 | 6 | 13 | 27 | 54 | 6 |
| GROUP III Controls (n=130) |
6.1±1.2 | 82 | 17 | 1 | - | 80 | 19 | 1 | - |
Normally distributed data is expressed as Mean±SD. SD: Standard deviation, HTN: Hypertension, SDT: Salt detection threshold, SPT: Salt perception threshold; L: 0.016 g/mL of NaCl (lowest concentration of NaCl); K: 0.04 g/mL of NaCL; J: 0.1 g/mL of NaCl; I: 0.25 g/mL of NaCl, Group I indicates Prehypertensive women (Pre-HTN), Group II indicates hypertensive (HTN) women and group III indicates normotensive women

- Comparison of salt perception threshold among women with Pre-hypertension (Group I), Hypertension( Group II) and Normotension ( Group III).
The mean values of BaPWV and CFPWV were found to be significantly high (P < 0.001) in pre-hypertensives (Group I females) and higher in hypertensives compared to normotensives [Table 3]. Figure 2 shows the comparison of brachial ankle pulse velocity (BaPWV) and carotid femoral pulse wave velocity (CFPWV) among the 3 groups. However, there was no significant difference in arterial stiffness index (ASI) and Ankle brachial index (ABI) among the 3 groups (P > 0.05).
| Variable | Group I (n=130) Pre-HTN Mean±SD |
Group II (170) HTN Mean±SD |
Group III (n=130) controls Mean±SD |
P-value |
|---|---|---|---|---|
| BaPWV (cm/s) | 1451.85±192.03 | 1683.99±336.06 | 1087.30±164.2 | 0.001 |
| CFPWV (cm/s) | 980.99±204.21 | 1207.10±231.11 | 721.57±66.4 | 0.001 |
| ASI (ratio) | 30.46±11.6 | 52.39±12.2 | 27.8±10.8 | 0.31 |
| ABI | 1.05±0.05 | 1.07±1.01 | 1.007±0.23 | 0.46 |
Normally distributed data expressed as Mean±SD. SD: Standard deviation, HTN: Hypertension, BaPWV: Brachial ankle pulse wave velocity, CFPWV: Carotid femoral pulse velocity, ASI: Arterial stiffness index, ABI: Ankle brachial index, HTN: Hypertension
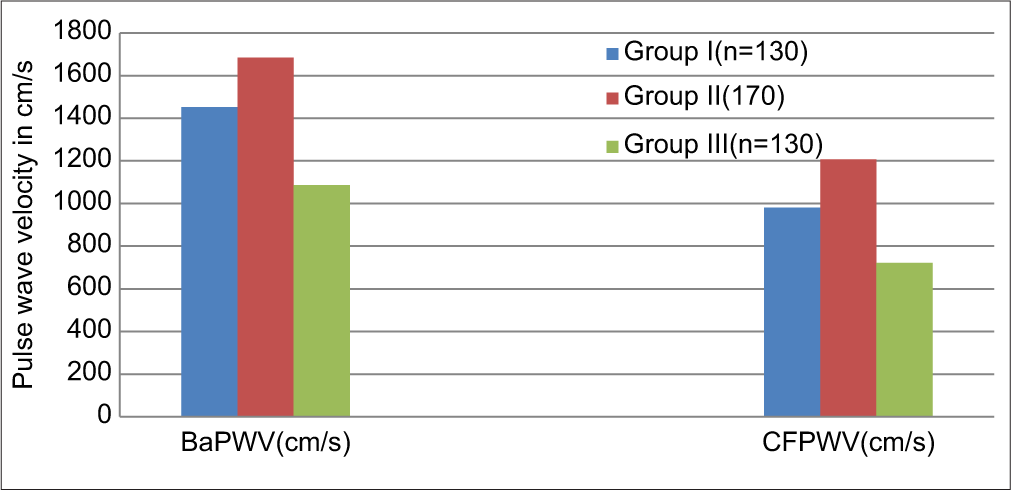
- Comparison of means of brachial ankle pulse wave velocity (BaPWV), carotid femoral pulse wave velocity (CFPWV) among women with Pre-hypertension: Group I, Hypertension: Group II and Normotension: Group III.
DISCUSSION
In the Indian population, to the best of our knowledge, there are limited studies on this subject. In this study, we assessed the different levels of dietary salt intake and in different groups. The salt intake was higher by 2.1 g/day in pre-hypertensive females and 5.6 g/day in hypertensive females when compared to controls and the salt taste perception threshold (SPT) was significantly higher in these females which led to higher salt intake. These results are supported by Moinuddin et al. who reported that the daily salt intake of pre-hypertensives was significantly greater than normotensives (P < 0.001).[17] High salt intake plays a crucial role in the transition between pre-HTN and HTN. Another study by Kudo et al.[11] examined the association of salt perception with salt intake and blood pressure levels in the general population in two communities – Akita and Osaka where salt intake was different. They found that Akita men detection threshold tended to be associated positively with SBP and DBP and concluded that high salt thresholds of salt perception were inversely associated with salt int ake. A study done by Chung[10] also examined the relationship between taste perception for salt and blood pressure in Korean adults and found that the recognition threshold for NaCl was significantly higher in hypertensive females concluding that taste acuity for salt is altered in hypertensive females which may influence dietary behavior associated with sodium intake. A study by Kim et al. have found no significant difference in salt detection threshold and salt perception threshold between controls and hypertensive groups and Lee et al[18,19] found salt perception threshold did not show any relationship with actual salt intake and salt eating habits but those eating salty food showed higher blood pressures. On the other hand, few studies[20-22] concluded that salt taste preferences are not related to sodium consumption and found no association between salt taste perception threshold and blood pressure and there was no significant difference in SPT between control and hypertensive groups. An Indian study by Inamdar et al.[13] assessed consumption of sodium among hypertensives and normal patients and found that habitual sodium consumption was higher in young adults, but they did not relate the high consumption with blood pressure. Individuals who consume a diet higher in salt are at a greater risk of HTN.[23] Intersalt cooperative research group found that a reduction in sodium intake of 100 mmol/d reduced SBP by 3–6 mmHg.[4]
Our results revealed that females with pre-HTN and HTN who eat a diet high in salt had higher BMI >25 kg/m2 than controls who eat a normal salt diet. These results were supported by a study done by Moinuddin et al.[17] where BMI is higher in pre-hypertensives as compared to hypertensives but this difference was not significant. However, the pulse rate, SBP, and DBP were significantly higher in prehypertensives as compared to normotensives (P < 0.001). Pre-hypertensives had a higher prevalence of risk factors and higher BMI.
The mean values of BaPWV and CFPWV which are indicators of vascular stiffness were found to be significantly high in prehypertensives and higher in hypertensive females compared to controls in our study. These results are in line with a study done by Jang et al.[22] showed brachial ankle pulse wave velocity (BaPWV) and carotid femoral pulse wave velocity (CFPWV) increased with blood pressure. In another study,[23] arterial stiffness measured by CF PWV and BaPWV in elderly subjects with pre-HTN was significantly higher than in normotensive elderly normal individuals. Vasan et al. reported that pre-HTN individuals exhibit higher rates of progression to HTN and higher risk for atherosclerotic disease than do normotensive individuals.[24,25] A longitudinal study by Framingham offspring found that arterial stiffness measured by PWV predicts future hypertensive status.[26] There is complexity in the relationship between arterial stiffness and blood pressure.[27] A study was done using a hypothetical model to analyze the association between salt intake and PWV through direct and mediating pathways that aimed to investigate whether the association between salt intake and arterial stiffness has a sex-specific pattern demonstrated that high salt intake has a direct and independent effect increasing arterial stiffness regardless of sex.[28]
A study done by Amen[12] from Iraq compared the salt taste threshold in hypertensive patients taking certain types of anti-hypertensive medication with that of healthy individuals and concluded that the salty taste threshold was decreased in hypertensive patients compared with healthy subjects.
A meta-analysis of 11 randomized controlled trials based on salt restriction in different populations revealed that an average intake reduction of sodium intake of 89.3 mmol/day was associated with a 2.84% reduction in PWV.[29] They also showed a significant reduction in SBP and DBP with a reduction in salt intake.
Study limitations
The study is a cross-sectional study and, therefore, lacked information on the association between low salt intake and CVD. An individual’s daily sodium intake varies day by day. 24 h urinary sodium estimations which are gold standard to evaluate 24 h urinary sodium excretion are needed. The sample size of 430 was relatively small and it is possible that more significant results could have been obtained from a larger sample size.
CONCLUSION
The present study suggests that high SPT in prehypertensive females contributes to high salt intake and is associated with high blood pressure. Advice on lifestyle modification and salt restriction in the diet could prevent the progression of preHTN to HTN and prevent cardiovascular events in females with pre-HTN.
Ethical approval
The research/study was approved by the Institutional Ethics Committee, number AIIMS/BBN/IEC/JUNE/2023/279-R, dated June 22, 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Audio summary available at
Financial support and sponsorship
The present study is funded under PSS-2023 by WINARS.
References
- Prevalence and Predictors of Prehypertension and Hypertension in Adult Population of Rural Southern India-An Epidemiological Study. J Family Med Prim Care. 2021;10:2558-65.
- [CrossRef] [PubMed] [Google Scholar]
- What Has Made the Population of Japan Healthy? Lancet. 2011;378:1094-105.
- [CrossRef] [PubMed] [Google Scholar]
- Blood Pressure and Dietary Salt in Human Populations. Ecol Food Nutr. 1973;2:143-56.
- [CrossRef] [Google Scholar]
- Intersalt: An International Study of Electrolyte Excretion and Blood Pressure, Results for 24 hour Urinary Sodium and Potassium Excretion. BMJ. 1988;297:319-28.
- [CrossRef] [PubMed] [Google Scholar]
- Dietary Salt Intake and Coronary Atherosclerosis in Patients with Prehypertension. J Clin Hypertens. 2014;16:575-80.
- [CrossRef] [PubMed] [Google Scholar]
- Role of Prehypertension in the Development of Coronary Atherosclerosis in Japan. J Epidemiol. 2004;14:57-62.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of Prehypertension on Common Carotid Artery Intima-media Thickness and Left Ventricular Mass. Stroke. 2009;40:1515-8.
- [CrossRef] [PubMed] [Google Scholar]
- Factors Associated with the Severity of Hypertension among Malaysian Adults. PLoS One. 2019;14:e0207472.
- [CrossRef] [PubMed] [Google Scholar]
- The Taste of Salt Measured by a Simple Test and Blood Pressure in Japanese Women and Men. Hypertens Res. 2009;32:399-403.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between Taste Perception for Salt and Blood Pressure in Normotensives and Hypertensive Korean Adults (P12-027-19) Curr Dev Nutr. 2019;3:P12-027-19.
- [CrossRef] [Google Scholar]
- Salt Taste Perception and Blood Pressures Levels in Population Based Samples: The Circulatory Risk in Community Study (CIRCS) Br J Nutr. 2021;125:203-11.
- [CrossRef] [PubMed] [Google Scholar]
- Salty Taste Threshold in Hypertensive Patients Taking Certain Types of Anti-hypertensive Medication Compared to Healthy Individuals. J Interdiscipl Med Dent Sci. 2015;3:184.
- [CrossRef] [Google Scholar]
- The Habitual Additional Sodium Intake among Hypertensive Patients Visiting a Tertiary Health Care Center, Indore, Madhya Pradesh. Indian J Community Med. 2020;45:435-9.
- [CrossRef] [PubMed] [Google Scholar]
- Normotension, Prehypertension and Hypertension in Urban Middle-class Subjects in India: Prevalence, Awareness, Treatment, and Control. Am J Hypertens. 2013;26:83-94.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of Hypertension among Indian Adults: Results from the Great India Blood Pressure Survey. Indian Heart J. 2019;71:309-13.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of Anthropometric Indices, Salt Intake and Physical Activity in the Aetiology of Prehypertension. J Clin Diagn Res. 2016;10:CC11-4.
- [CrossRef] [PubMed] [Google Scholar]
- The Salt Taste Threshold in Untreated Hypertensive Patients. Clin Hypertens. 2017;23:22.
- [CrossRef] [PubMed] [Google Scholar]
- Not Salt Taste Perception but Self-reported Salt Eating Habit Predicts Actual Salt Intake. J Korean Med Sci. 2014;29:91-6.
- [CrossRef] [PubMed] [Google Scholar]
- Salt Taste Perceptions and Preferences are Unrelated to Sodium Consumption in Healthy Older Adults. J Am Diet Assoc. 1996;96:471-4.
- [CrossRef] [PubMed] [Google Scholar]
- Meta-analysis of the effect of dietary sodium restriction with or without concomitant Renin-Angiotensin-aldosterone inhibiting treatment on albuminuria. Clin J Am Soc Nephrol. 2015;10:1542-52.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants of Brachial Ankle Pulse Wave Velocity and Carotid Femoral Pulse Wave Velocity in Healthy Koreans. J Korean Med Sci. 2014;29:798-804.
- [CrossRef] [PubMed] [Google Scholar]
- Arterial Stiffness in Early Phases of Prehypertension In: Pre-Hypertension and Cardiometabolic Syndrome. Germany: Springer; 2018. p. :101-3.
- [CrossRef] [Google Scholar]
- Impact of High-normal Blood Pressure on the Risk of Cardiovascular Disease. N Eng J Med. 2001;345:1291-7.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of Frequency of Progression of Hypertension in Non-hypertensive Participants in the Framingham Heart Study: A Cohort Study. Lancet. 2001;358:1682-6.
- [CrossRef] [PubMed] [Google Scholar]
- Effects on Blood Pressure of Reduced Dietary Sodium and the Dietary Approaches to Stop Hypertension (DASH) Diet. N Engl J Med. 2001;344:3-10.
- [CrossRef] [PubMed] [Google Scholar]
- Aortic Stiffness, Blood Pressure Progression and Incident Hypertension. JAMA. 2012;308:875-81.
- [CrossRef] [PubMed] [Google Scholar]
- Association between Salt Taste Sensitivity Threshold and Blood Pressure in Healthy Individuals: A Cross Sectional Study. Sao Paulo Med J. 2020;138:4-10.
- [CrossRef] [PubMed] [Google Scholar]
- Salt Intake, Stroke and Cardiovascular Disease: Meta-analysis of Prospective Studies. BMJ. 2009;339:b4567.
- [CrossRef] [PubMed] [Google Scholar]








