Translate this page into:
Refractory Angina—An Overview and Recent Trends
Meenakshi Kadiyala, MD, DM Department of Cardiology Saveetha Medical College and Hospital, Tandalam, Chennai 602105, Tamil Nadu India drmeenaram@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Because of improvement in survival from coronary artery disease and increasing life expectancy of the population, chronicity and resistance to therapy have become growing problems confronting the cardiologist. Refractory angina pectoris is an entity based on clinical diagnosis, and it refers to recurrent and sustained chest pain more than 3 months duration caused by coronary insufficiency that is unamenable to conventional modalities of treatment, including drugs, percutaneous coronary interventions, or coronary bypass grafting. Individuals with this entity may have an impaired quality of life, with recurrent angina, poor general health and psychological distress impairing functional and productive sustenance. A multitude of therapeutic options exists for patients with refractory angina pectoris, and randomized trials have shown them to be reasonably effective in reducing symptoms, though further research is warranted.
Keywords
coronary artery disease
myocardial oxygen demand
refractory angina
Introduction
Chronic symptomatic coronary artery disease (CAD), otherwise called refractory angina (RFA), is, as the name implies, resistant to medical therapy and conventional revascularization techniques. Patients have recurrent chest pain, shortness of breath, and easy fatigability restricting and limiting day-to-day activities and impairing quality of life.
About 100,000 patients every year are diagnosed with RFA.1 To label a patient as RFA, there should be objective evidence of ischemia as evidenced by marked limitation of ordinary physical activity, a positive treadmill test, and abnormal stress imaging studies, and the usefulness of all known conventional therapies should have been exhausted. Many of these patients might have already undergone multiple percutaneous or surgical revascularizations, and thus they are not candidates for additional procedures. The several reasons why revascularization cannot be considered in them are diffuse coronary disease, poor target vessels, and contraindicating comorbidities.1 A second and sometimes third opinion regarding feasibility of revascularization should be sought before labeling as RFA.
Mental stress-induced myocardial ischemia (MSIMI) is described as objective signs of myocardial ischemia such as ST-segment depression in the electrocardiogram (ECG) during a mental stress. In the REMIT (Remission Evaluation of Metabolic Intervention in Type 2 diabetes) trial, most patients treated with the selective serotonin-reuptake inhibitor (SSRI) escitalopram (5 mg daily for 6 weeks) were free of MSIMI compared with patients treated with a placebo (17.5% vs. 34.2%, p = 0.04). Escitalopram had no effect on exercise-induced ischemia, but rather improved anxiety and emotional reactions to mental stress. Escitalopram should be used cautiously in the concomitant presence of major depression, as it has been associated with increased suicidal risk in such subsets of patients.2
There have been a few studies on the natural history and mortality predictors for patients with RFA. The older studies, such as the Cleveland Clinic series, showed that the 1-year mortality was as high as 17%.3 4 The Mediators of Social Support (MOSS) Study at Duke University indicated a mortality of 38% at 2.2-year in persons not eligible for revascularization.5 In contrast, 1-year mortality from the Options In Myocardial Ischemic Syndrome Therapy (OPTIMIST) study done 15 years later was 4%. This marked decline may occur due to a different patient population studied or due to improved and more potent drugs, optimal use of guideline-based therapies, and more advanced revascularization techniques, including frequent use of left internal mammary artery grafts.3 Based on these observations, the clinician should have a standardized protocol for the management of patients with RFA, ranging from lifestyle modification to novel therapies.4
Traditional Pharmacologic Therapy
Short- or long-acting oral nitrates are the commonly used antianginal agents. They reduce the preload by vasodilation, increase myocardial oxygen supply, and decrease myocardial oxygen demand. Tolerance to nitrates blunts their effectiveness, and daily nitrate-free interval to preserve their effectiveness is mandatory.5
β-Blockers. They, particularly selective agents, remain the first-line drug for the treatment of angina pectoris. They decrease heart rate, myocardial contractility, and blood pressure reducing myocardial oxygen demand. Slowing of heart rate also allows time for coronary filling.
Calcium channel blockers. They are arterial vasodilators, with variable effects on cardiac conduction and contractility. The nonhydropyridines such as verapamil and diltiazem have negative inotropic and chronotropic effects, and thus they decrease myocardial oxygen demand whereas dihydropyridines such as nifedipine increase myocardial oxygen supply by coronary vasodilation.6
Antiplatelet agents. Aspirin is recommended for all patients with CAD unless there is a contraindication. For patients allergic to aspirin, clopidogrel or ticlopidine can be used. The CAPRIE (Clopidogrel versus Aspirin in Patients at Risk of Ischemic Events) trial demonstrated that clopidogrel was more effective than aspirin in decreasing the combined risk of myocardial infarction, vascular death, or ischemic stroke. Presently dual-antiplatelet therapy is the order of the day.7 8
Lipid-lowering agents. Pooled data show that every 1% reduction in total cholesterol reduces coronary events by 2%. Statins by their pleiotropic effects are useful in the primary and secondary prevention of atherosclerotic cardiovascular disease.
Angiotensin-converting enzyme (ACE) inhibitors. The HOPE (Heart Outcomes Prevention Evaluation), PEACE (Prevention of Events with Angiotensin-Converting Enzyme Inhibition), EUROPA (EURopean trial On reduction of cardiac events with Perindopril in stable coronary Artery disease) trials, etc. have all evaluated the anti-ischemic effects of ACE inhibitors in patients with CAD and normal left ventricular function and have found a significant reduction in mortality and recurrent ischemic events.
Newer Pharmacologic Agents
Low-molecular-weight heparins (LMWHs) can be used as an outpatient therapy. Randomized trials evaluating the efficacy of LMWH showed a statistically significant decrease in fibrinogen levels and an improvement in the time to both 1-mm ST-segment depression and peak ST-segment depression. There was no increase in major bleeding events.
Intermittent low-dose thrombolytic therapy may enhance both the micro- and macrocirculatory coronary blood flow in RFA, and trials in its favor have been conducted. Because of the small number of patients studied and the lack of a control group, its role still remains uncertain.
Ranolazine hydrochloride acts by altering the sodium-dependent calcium channels during myocardial ischemia. It is also a metabolic modulator shifting cardiac lipid oxidation to glucose oxidation. Ranolazine trials, in which ranolazine either alone or with atenolol, diltiazem, or amlodipine in stable angina, showed a significant dose-related improvement in the exercise tolerance when compared with placebo. A similar finding was observed in the TIMI 36 trial.9
L-Arginine produces endothelium-dependent vasodilation and is supposed to increase coronary blood flow, exercise duration, and maximum workload during stress testing.10
Nicorandil activates the mitochondrial ATP-sensitive potassium channels and may offer ischemic preconditioning of the myocardium. The Nicorandil in Angina trial, in which nicorandil 20 mg twice daily, showed a 17% relative risk reduction in myocardial infarction (MI) and death when compared with placebo.11
Ivabradine reduces myocardial oxygen demand by its negative chronotropic effect without any effect on cardiac inotropy, and it has anti-ischemic and antianginal efficacy either as monotherapy or along with atenolol.12
Noninvasive Therapy
Enhanced external counterpulsation (EECP) therapy uses a mechanism similar to the intra-aortic balloon. The cuffs in EECP inflate during diastole, sequentially from the calves to the upper thighs, and deflate at the beginning of systole. EECP helps improve anginal symptoms by diastolic augmentation and increased coronary perfusion pressure, and augments the collateral circulation either by angiogenesis or opening of previously dormant vessels or both. The MUST-EECP (Multicenter Study of Enhanced External Counterpulsation) trial randomized end-stage CAD patients to either the active EECP group (300 mm Hg cuff inflation) or the inactive sham EECP group (75 mm Hg cuff inflation), and the results showed a significant increase in the time to 1-mm ST-segment depression, fewer anginal episodes, and decreased nitroglycerin use in the active EECP group. Exercise duration increased in both groups, but the intergroup difference was not significant. Only 10% of patients experienced adverse reactions necessitating withdrawal.13 International EECP Patient Registry showed an improvement of at least one angina class in 81% of the patients with Canadian Cardiovascular Society (CCS) class III or IVRA. The major limitation of this study is the lack of a control group. At this time, EECP is not applicable for all patients with RFA, and it is contraindicated in the presence of severe pulmonary vascular disease and congestive heart failure, moderate to severe aortic insufficiency, uncontrolled arrhythmias, etc. However, it remains a good treatment option for a few patients with severe, resistant ischemia.
Yoga and the heart-breathing exercise or pranayama can be suggested in RFA patients because they are easy. Studies have shown that patients that follow yoga, in addition to their cardiac medications for 30 days, show a greater improvement in the functional capacity than those who follow only medical therapy. Several pranayamas have been offered in heart diseases, such as Bhastrika, Kapalbhati, Bahya, Anulom Vilom, Nadi Shodhan, Bhramari, Udggeth, and Pranav pranayamas. Yoga postures suggested to prevent CAD include Uttanapadasana and Pavanamuktasana. Cardiac patients should perform yogasana and pranayama only under expert guidance. Yoga benefits CAD by reducing hypertension; ensuring better control of diabetes mellitus (DM) and dyslipidemia; and reducing stress, anxiety, and depression.
Invasive Therapies
Laser transmyocardial revascularization (TMR) involves using high-power carbon dioxide lasers to create10 to 50, 1-mm-diameter transmural channels 1 cm apart along the left ventricular free wall in the ischemic myocardium by a left lateral thoracotomy either alone or along with coronary artery bypass grafting (CABG). The channels were originally thought to provide direct blood flow to the myocardium; however, as they close within weeks after the procedure, the beneficial effect of TMR is probably by stimulating angiogenesis or causing myocardial denervation. Five prospective randomized trials on TMR in “no-option” patients with 1-year follow-up have revealed that it is associated with better angina relief, improved exercise tolerance, decreased hospitalization, and longer event-free survival compared with maximal medical therapy. A minimally invasive robot-assisted TMR can also be performed endoscopically (PTMLR), and it is a less morbid procedure with quicker recovery in patients with medical comorbidities. Although anginal class scores significantly decreased in the TMLR and PTMLR groups, overall survival at 12 months was not significantly different and the procedure is now almost obsolete14 15 (Table 1).
|
Study (Ref) |
Year |
n |
Follow-up (mo) |
Laser type |
Two class improvement in angina (laser vs. placebo) |
One-y survival (laser vs. placebo) |
|---|---|---|---|---|---|---|
|
Cooley et al26 |
1999 |
192 |
12 |
CO2 |
72% vs. 13% (p < 0.01) |
85% vs. 79% |
|
Allen et al15 |
1999 |
275 |
12 |
H-YAG |
76% vs. 32% (p < 0.01) |
84% vs. 89% |
|
Burkhoff et al27 |
1999 |
182 |
12 |
H-YAG |
48% vs. 14% (p < 0.01) |
95% vs. 90% |
|
Schofield et al28 |
1999 |
188 |
12 |
CO2 |
24% vs. 4% (p < 0.01) |
89% vs. 96% |
|
Oesterle et al29 |
2000 |
221 |
12 |
H-YAG |
34% vs. 14% (p < 0.01) |
93% vs. 97% |
|
Leon et al30 |
2000 |
298 |
6 |
H-YAG |
34% vs. 42% |
98% vs. 97% |
|
Whitlow et al31 |
2001 |
330 |
12 |
H-YAG |
32% vs. 10% (p < 0.01) |
92% vs. 93% |
Angiogenesis. Treatment of chronic ischemic heart disease (IHD) using bone marrow cells (BMC) is under intense investigation. A meta-analysis of three trials wherein RFA patients who received an intramyocardial injection of CD34+ stem cells improved their total exercise time and reduced their angina frequency with a reduction in mortality and major adverse events when compared with placebo. Although the early results of cell-based therapies are promising, the long-term effects on the myocardium and other issues such as the type of cell to be used, the optimal dose, and the ideal and effec tive route of delivery are still unresolved. Data from Mann et al suggest a need for repeated administrations to maintain efficacy.16 Autologous mesenchymal stromal cells (MSCs) have been tested in patients with advanced CAD and RFA. When injected directly into the ischemic myocardium, they significantly improved total exercise duration and angina class, up to 3 years after implantation.17 18
Coronary sinus reducer. Regional wall motion abnormalities and increased left ventricular end-diastolic pressure due to ischemia compress the subendocardial capillaries, reducing perfusion. Insertion of a balloon-inflatable coronary sinus reducer device, implanted via a simple transjugular approach, increases coronary sinus pressure and venous resistance and increases subendocardial flow. This approach also stimulates neovascularisation.19 The COSIRA (Coronary Sinus Reducer for Treatment of Refractory Angina) study demonstrated significant improvements in angina symptoms and quality of life with this device in 35% patients showing a reduction of ≥2 CCS classes compared with 15% in the control group (p = 0.020). However, it is only suitable for patients with left-sided coronary ischemia. This treatment is currently not approved in the United States or Canada but is available in some European countries.20
Extracorporeal shockwave myocardial revascularization therapy (ESMR) involves delivering low-energy shockwaves to the border of ischemic myocardium over 4 to 9 weeks. It is thought to reduce ischemia and improve left ventricular function by local vasodilation and neovascularization. Case-control studies, randomized controlled trials (RCTs), and multicenter studies have shown improvements in angina in patients with RFA. Prior ESMR therapy has been suggested to enhance the beneficial effects of BMCs delivered by intracoronary injection. Further studies are needed to determine the exact role of ESMR in RFA.21
Neuromodulation by interruption or modification of the aff erent signals through which pain is perceived is an emerging therapeutic option for patients with RFA. Symptoms appear to improve with both transcutaneous electric nerve stimulation (TENS) or spinal cord stimulation (SCS), although the data for SCS are more convincing. There is objective evidence that both modalities may reduce ischemia. Concerns are that SCS is invasive and TENS produces cutaneous side effects.22 Furthermore, a strong placebo component may be present. Currently, interest in neurostimulation is centered mainly in Europe.
Gene therapy is a potential therapy for RFA. Animal research has shown promising results, although convincing data of its efficacy in humans have not been established. Preliminary results are promising, but use of plasmids has been questioned. Recent studies have used adenoviral vectors for gene transport that can deliver a higher titer of the gene product, but the possibility of vector-induced cytotoxicity remains. Future studies are needed to assess the true efficacy of gene therapy, ideal vector, and best mode of delivery.23
Percutaneous in situ coronary venous arterialization (PICVA) is a percutaneous approach to CABG that redirects arterial blood flow from the occluded artery into an adjacent coronary vein, arterializing it and providing retroperfusion to ischemic myocardium. Percutaneous in situ coronary artery bypass (PICAB) is also a recent technology for RFA patients in whom arterial blood flow is redirected from a diseased artery to an adjacent coronary vein and then rerouted back to the artery after the lesion. Thus, the coronary vein acts as a bypass conduit.24 Although PICVA and PICAB can be considered in patients with coronary anatomy unamenable for traditional revascularization, they are still experimental and further trials are needed before they can be applied to patients with RFA.
Chelation therapy is based on the hypothesis that ethylenediamine-tetraacetic acid (EDTA) could extract calcium from the atherosclerotic plaque after it was noted in 1950 that patients treated with EDTA for lead poisoning experienced relief of angina. The PATCH trial revealed the ineffectiveness of chelation therapy and the potential for serious side effects, including lethal hypocalcemia and severe kidney dysfunction.25 The American Heart Association, the American College of Cardiology, the Food and Drug Administration, and the National Institutes of Health have published an official conclusion that there was no validated scientific evidence to demonstrate any benefit from this therapy.
Heart Transplantation
Whether heart transplantation should be considered as the last option for patients with disabling angina in whom all conventional modalities have failed is still under debate. In fact, some patients may live longer with their angina, as compared with the survival expectancy after transplantation.
Pragmatic rehabilitation promotes patients to manage their own symptoms and thereby to improve quality of life and mental well-being. It consists of two main components. The first is education to avoid needless fear and wrong conceptions about angina; angina is not always life threatening, that recurrent angina can help formation of collaterals, that the severity of the symptoms can also be effected by the mental state, and that not all the pain perceived needs to be of cardiac origin. The second component deals with lifestyle modifications to reduce cardiovascular risk (e.g., smoking cessation, weight loss, and exercise). Pragmatic rehabilitation is typically delivered by a dedicated nurse and a clinical psychologist through group-based education programs. Meta-analysis and the Seattle Angina Questionnaire revealed that this technique resulted in significantly less angina and improved quality of life.
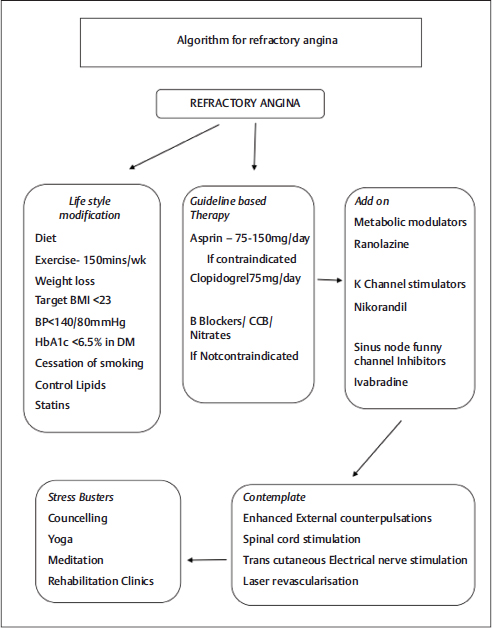
The authors proposed algorithm to follow for the RFA in Fig. 1.
-
Fig. 1 Algorithm for refractory angina. BMI, body mass index; BP, blood pressure; CCB, calcium channel blocker; DM, diabetes mellitus; HbA1C, hemoglobin A1C.
Fig. 1 Algorithm for refractory angina. BMI, body mass index; BP, blood pressure; CCB, calcium channel blocker; DM, diabetes mellitus; HbA1C, hemoglobin A1C.
Conclusion
Angina pectoris refractory to conventional medical therapy and not amenable to either CABG or PCI poses a difficult situation for both the patient and physician. A second and third opinion is needed before being labeled as “refractory angina pectoris.” For these “no-option” patients, a new emerging armamentarium of drugs and innovative revascularization techniques should be considered. Neurostimulation and EECP may benefit a few, and angiogenic gene therapy is a promising option. Ultimately, the physician and the patient must determine which alternative treatment may be the best for them. Novel therapeutic approaches are welcome after a thorough evaluation of their efficacy and cost-effectiveness, and development of clinical guidelines specific to RFA should also be encouraged.
References
- The problem of chronic refractory angina; report from the ESC Joint Study Group on the Treatment of Refractory Angina. Eur Heart J. 2002;23(05):355-370.
- [Google Scholar]
- Prevalence and clinical characteristics of mental stress-induced myocardial ischemia in patients with coronary heart disease. J Am Coll Cardiol. 2013;61(07):714-722.
- [Google Scholar]
- Long-term survival in patients with refractory angina. Eur Heart J. 2013;34(34):2683-2688.
- [Google Scholar]
- Current and future treatment strategies for refractory angina. Mayo Clin Proc. 2004;79(10):1284-1292.
- [Google Scholar]
- Improvements in long-term mortality after myocardial infarction and increased use of cardiovascular drugs after discharge: a 10-year trend analysis. J Am Coll Cardiol. 2008;51(13):1247-1254.
- [Google Scholar]
- Comparison of the antianginal efficacy of isosorbide dinitrate (ISDN) 40 mg and verapamil 120 mg three times daily in the acute trial and following two-week treatment. Eur Heart J. 1988;9(02):149-158.
- [Google Scholar]
- Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. [published correction appears in BMJ. 2002;324 (7330):141] BMJ. 2002;324:71-86. 7329
- [Google Scholar]
- A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE) Lancet. 1996;348:1329-1339. 9038
- [Google Scholar]
- MARISA Investigators. Anti-ischemic effects and long-term survival during ranolazine monotherapy in patients with chronic severe anginaJ Am Coll Cardiol. 2004;43(08):1375-1382.
- [Google Scholar]
- Effect of supplemental oral L-arginine on exercise capacity in patients with stable angina pectoris. Am J Cardiol. 1997;80(03):331-333.
- [Google Scholar]
- Effects of nicorandil patients with refractory angina and advanced coronary artery disease. Can J Cardiol.
- [Google Scholar]
- Ivabradine use in refractory unstable angina: a case report. Int J Immunopathol Pharmacol. 2009;22(03):849-852.
- [Google Scholar]
- Enhanced external counterpulsation and future directions: step beyond medical management for patients with angina and heart failure. [Published correction appears in J Am Coll Cardiol 2007;50(25):2441.] J Am Coll Cardiol. 2007;50(16):1523-1531.
- [Google Scholar]
- Percutaneous myocardial laser revascularization in patients with refractory angina pectoris. Am J Cardiol. 2003;91(06):661-666.
- [Google Scholar]
- Comparison of transmyocardial revascularization with medical therapy in patients with refractory angina. N Engl J Med. 1999;341(14):1029-1036.
- [Google Scholar]
- Safety and feasibility of transendocardial autologous bone marrow cell transplantation in patients with advanced heart disease. Am J Cardiol. 2006;97(06):823-829.
- [Google Scholar]
- Angiogenesis in ischaemic myocardium by intramyocardial autologous bone marrow mononuclear cell implantation. Lancet. 2003;361:47-49. 9351
- [Google Scholar]
- Working Group Members. Clinical and research issues regarding chronic advanced coronary artery disease: part I: contemporary and emerging therapiesAm Heart J. 2008;155(03):418-434.
- [Google Scholar]
- Coronary Sinus Reducer system™: a new therapeutic option in refractory angina patients unsuitable for revascularization. Int J Cardiol. 2016;209:122-130.
- [Google Scholar]
- Coronary sinus reducer stent for the treatment of chronic refractory angina pectoris: a prospective, open-label, multicenter, safety feasibility first-in-man study. J Am Coll Cardiol. 2007;49(17):1783-1789.
- [Google Scholar]
- Safety and efficacy of extracorporeal shock wave myocardial revascularization therapy for refractory angina pectoris. Mayo Clin Proc. 2014;89(03):346-354.
- [Google Scholar]
- Electrical neuromodulation for patients with cardiac diseases. Neth Heart J. 2013;21(02):91-94.
- [Google Scholar]
- Angiogenic gene therapy for refractory angina. Expert Opin Biol Ther. 2016;16(03):303-315.
- [Google Scholar]
- [Emergent strategies in interventional cardiology] Rev Esp Cardiol. 2005;58(08):962-973.
- [Google Scholar]
- Treatment of refractory angina in patients not suitable for revascularization. Nat Rev Cardiol. 2014;11(02):78-95.
- [Google Scholar]
- Transmyocardial laser revascularization: clinical experience with twelvemonth follow-up. J Thorac Cardiovasc Surg. 1996;111:791-799.
- [Google Scholar]
- Histologic appearance of transmyocardial laser channels after 4 1/2 weeks. Ann Thorac Surg. 1996;61:1532-1535.
- [Google Scholar]
- Transmyocardial laser revascularisation in patients with refractory angina: a randomised controlled trial. Lancet. 1999;353:519-524.
- [Google Scholar]
- Percutaneous transmyocardial laser revascularisation for severe angina: the PACIFIC randomised trial. Lancet. 2000;356:1705-1710.
- [Google Scholar]
- A blinded, randomized, placebo-controlled trial of percutaneous laser myocardial revascularization to improve angina symptoms in patients with severe coronary disease. J Am Coll Cardiol. 2005;46(10):1812-1819.
- [Google Scholar]
- One-year results of percutaneous myocardial revascularization for refractory angina pectoris. Am J Cardiol. 2003;91(11):1342-1346.
- [Google Scholar]







