Translate this page into:
Radiation Safety for Women in Cardiology: Myths and Important Messages
*Corresponding author: Sonya N. Burgess, Department of Cardiology, Nepean Hospital, Sydney, Australia. sonyatowns@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Burgess SN, Alasnag M, Haan LI, Takahashi S, Lukito AA, Cader A, et al. Radiation Safety for Women in Cardiology: Myths and Important Messages. Indian J Cardiovasc Dis Women. 2024;9:102-8. doi: 10.25259/IJCDW_10_2024
Abstract
Accurate fertility-based radiation safety data, education and knowledge is important for all staff exposed to occupational radiation. Women are under-represented in all medical fields with increased exposure to occupational radiation, to achieve better equity in our medical workforces evidence-based radiation safety knowledge is essential to overcoming perceived career barriers. This review of radiation safety policy and data focuses on providing health professions working in cardiology with accurate contemporary information about potential radiation exposure with respect to fetal risk for pregnant health professionals. The data summarized within this review shows when women continue to work in cardiac catheterization laboratories through pregnancy their expected occupational radiation exposure with appropriate shielding, will not meaningfully change pregnancy outcomes, nor will it significantly increase risk to the fetus. The review also summarizes international workplace policy for radiation exposure and monitoring and provides recommendations for ongoing safe practice.
Keywords
Radiation safety
pregnancy
Women in cardiology
equity
INTRODUCTION
W orkplace safety is important for health-care professionals working with occupational radiation. Understanding and quantifying radiation risk is essential. For women in cardiology, exposure to occupational radiation occurs during early career and during training when pregnancy is also likely.[1-4] Access to accurate, contemporary, and appropriate information is essential but can be challenging to find.[4]
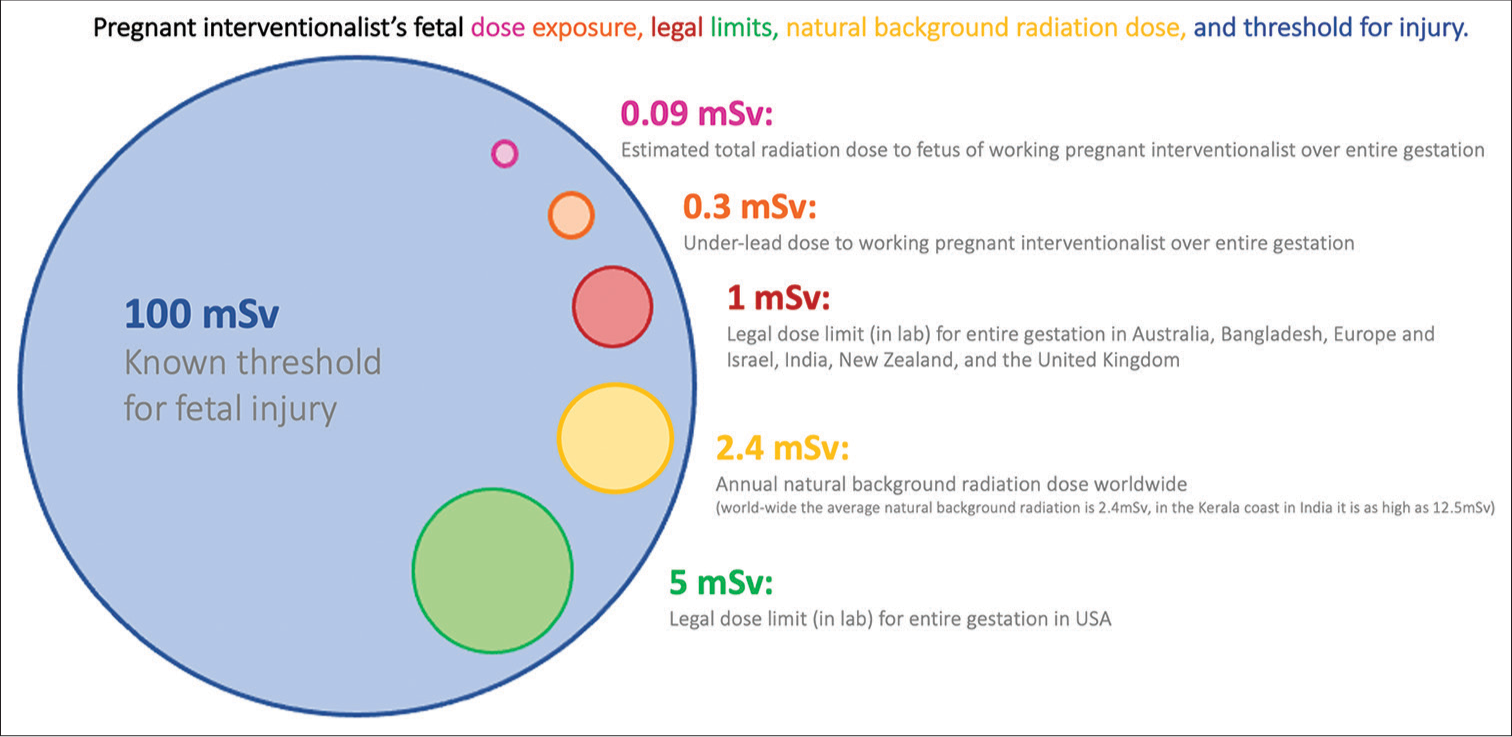
This editorial addresses occupational radiation safety issues for women in Cardiology. The objective is to provide simple balanced safety messages and to address and debunk any misinformation. Data demonstrate clearly that pregnant women can safely work in cardiac catheterization laboratories (with appropriate monitoring and shielding) with negligible risk to the developing fetus when well-maintained protective equipment is used[3,4] [Figure 1]. It is for this reason that international recommendations from Australasia, Canada, Europe, India, Israel, Japan, the United States, and the United Kingdom all state that pregnant women can continue to work in an ionizing radiation environment with appropriate monitoring[3,4] Table 1 data and thresholds sourced from Vu and Elder.
- Data and image adapted from Ghatan and Kothary and from Sahni et al.
| Radiation effect | Gestation (weeks) | Threshold dose (mSv) |
|---|---|---|
| Death | 3–4 | 100–200 |
| Malformations (major) | 4–8 | 250–500 |
| Significant growth limitation | 4–8 | 200–500 |
| Irreversible growth restriction | 8–15 | 250–500 |
| Severe intellectual disability | 8–15 >16 |
60–500 >1,500 |
| Microcephaly | 8–15 | >20,000 |
| Decreased IQ | >16 | >100 |
IQ: Intelligence quotient
These messages are important because radiation exposure is commonly identified as a major barrier for women considering a career in interventional cardiology, electrophysiology, and other specialties employing occupational radiation.[2-8] At present, disproportionate concerns regarding occupational radiation exposure during pregnancy may unnecessarily affect specialty selection or result in missed career development opportunities.[2-6,8] Accurate and balanced safety message should be readily available to all staff working cardiology catheterization laboratories.
DEBUNKING THE MYTHS: WHY DO WE NEED TO BE BETTER INFORMED ABOUT RADIATION SAFETY?
Internationally, interventional cardiology is the medical specialty with the most substantial under-representation of women.[2,4,6,9] Cardiology, orthopedics, gastroenterology, and interventional radiology are all specialties which require exposure to occupational radiation. These specialties have some of the worst representation of women amongst all medical specialties.[2,6,10] Women are under-represented in all procedural specialty fields associated with occupational radiation exposure, interventional cardiology, structural interventions, structural interventional imaging, electrophysiology, and interventional radiology, urology gastroenterology, and orthopedics.[2,11-14]
A large international survey of cardiologists investigating specialty choice found 20% of women identified concerns about radiation as a major factor in specialty selection, this was in the top 3 most commonly identified reasons for not selecting a career in interventional cardiology.[5] Current research suggests that trainees without readily accessible clear information may overestimate risk.[2,3,5] Training and interventional practice in cardiology and interventional cardiology requires radiation exposure, this is unlikely to change in the near future; therefore, data quantifying risk must be readily available to limit barriers to inclusion.
There is evidence that the lack of workforce gender diversity in these specialties may have an impact on patient outcomes.[2,5-20] Female under-representation in these specialties also limits patient choice and healthcare access.[17] To produce a more diverse and representative workforce within these specialties, successful strategies are needed.
To inform our trainees and colleagues about radiation safety when pregnant the questions, we must be able to answer are relatively simple: (1) Is it safe to continue to work in the coronary catheterization laboratories while pregnant? (2) Is it legal to continue to work in the coronary catheterization laboratories while pregnant? (3) How can we monitor and limit any risk?
Is it safe to continue to work in the coronary catheterization laboratory while pregnant?
The simple answer to this question is Yes, it is safe to continue to work in the coronary catheterization laboratory while pregnant. However, we need to acknowledge that evaluating the true risk to healthcare workers when pregnant can be challenging and is important. The amount of extra radiation exposure to the fetus of a pregnant interventional cardiologist or trainee is often overestimated, and background radiation exposure is often underestimated[2,4,8,21] [Figure 1] (Data and image adapted from Gahan et al.[8] and from Sahni et al.[21]). The average total occupational radiation dose to the fetus/uterus of a working pregnant interventional cardiologist is estimated to be 0.09mSv over her entire pregnancy.[8,22] The average background radiation exposure is 2.4mSv[21] worldwide, but varies geographically. Therefore, the incremental increase in radiation exposure from occupational radiation under leads is actually very small.
Legal radiation dose limits are intended to decrease or mitigate risk. There are no differences between the effects caused by natural radiation or radiation made by people which is artificially generated by industry or for medical use. The key to understanding radiation risk is understanding the amount of extra radiation (above the background daily exposure we all face) generated by working in occupational radiation.
While the developing fetus is highly sensitive to radiation, particularly in the first trimester, the scale of exposure from occupational exposure in the cardiac catheterization laboratory is a tiny fraction of documented thresholds for fetal injury.[4,8,21,23] If we keep the additional under lead dose to ≤1 milliSv, we change the background risk of childhood cancer or congenital malformation from 4.070% to 4.078%; if it is ≤0.5 mSv (which research reports suggest is most likely), we change background risk from 4.070% to 4.072%.[4,8,22,24] Radiation exposure effects [Table 1] require logarithmically higher doses of exposure and/or long durations of exposure than reported under-lead radiation doses to fellows or interventionalists, or to other healthcare workers in the catheterization laboratory[4] [Figure 1 and Table 1]. In terms of absolute risk, the probability of congenital malformation or cancer in a fetus of a pregnant interventional cardiologist or fellow increases a very small amount.
Is it legal to continue to work in the coronary catheterization laboratory while pregnant?
Internationally, legal radiation safety guidelines with statement regarding pregnancy are available, but vary country to country.[4] Table 2 summarizes their recommendation for pregnant workers. Most (but not all) countries allow pregnant workers to continue in cardiac catheterization laboratories with appropriate lead protection and monitoring.[25] In Europe, recent updated definitions of safe dose limits and standards for fetal exposure have been published from the European directive,[25] resulting in repeal or removal of previously more conservative policies or directives. Internationally recommended under-lead thresholds for the entire pregnancy are between 1 and 5 mSv.[4] These thresholds are very conservative values and are well below the 100 mSv threshold for fetal injury.[22]
| Threshold for total pregnancy | Guiding regulation/law | |
|---|---|---|
| Australia | <1 mSv | Australian Radiation Protection and Nuclear Safety Agency Radiation Protection Diagnostic and Interventional Cardiology, series 14.1. Australian Radiation Health Committee. 2008 |
| Austria | Not allowed | Law prohibits despite European directive 2013/59/Euratom directive supporting pregnancy in the catheterization laboratory |
| Belgium | <1 mSv | ARBIS July 20, 2001 |
| Canada | 4 mSv | The Canadian Radiation Protection Regulations (SOR/2000-203) |
| Cyprus | <1 mSv | 2018 |
| Denmark | <1 mSv | BEK nr 669 af July 07, 2019 (equivalent to EU directive) |
| France | <1 mSv | Articles D. 4152-5 et R, 4451-45 du code du travail |
| Germany | <1 mSv | Strahlenschutzgesetz: German Radiation Protection Law dated June 27, 2017 (amendment May 20, 2021, Strahlenschutzverordnung: German Radiation Protection Ordinance, 2018 (Federal Law Gazette Part I, p. 2034, 2036), (amendment May 20, 2021) |
| Hungary | Not allowed | Government Decree 487/2015 (XII. 30.) on the protection against ionizing radiation and the corresponding licensing |
| India | 1 mSv | Guidelines of Atomic energy Regulatory Board (Indian Government body) |
| Indonesia | <1 mSv | Regulations of the Nuclear Energy Regulatory Agency-BAPETEN Article 38.2020 |
| Ireland | <1 mSv | Radiological Protection Act 1991 (Ionizing Radiation) Regulations 2019 |
| Italy | Not allowed | DL 101 July 2020 |
| Israel | <1 mSv | 1992 Law by the Ministry of Labor, Social Affairs, and Social Services |
| Japan | ≤1 mSv effective dose ≤2 mSv dose to surface of abdomen |
Regulation on Prevention of Ionizing Radiation Hazard-Japanese Ministry of Health, Labor, and Welfare |
| Netherlands | <1 mSv | |
| New Zealand | <1 mSv | Radiation safety Act 2016 (New Zealand) |
| Portugal | Not allowed | 102/2009, 10 September |
| Romania | Not allowed | LAW 154/2015 |
| Singapore | Not allowed | |
| Slovenia | <1 mSv | ZVISJV-1, December 2017 |
| Spain | <1 mSv | Royal Decree 298/2009, of March 6, which modifies the Royal Decree 39/1997, of January 17 |
| Sweden | <1 mSv | SFS 2018:396 |
| UK | 1 mSv | The Ionizing Radiation Regulations 2017 (IRR 17) |
| USA | <5 mSv | Individual states have Pregnant Workers Fairness laws, NCRP guide practice |
Modified from Manzo-Silverman et al, with updates from the (Women in Interventional cardiology-Asia Pacific Society of Interventional Cardiology WIN-APSIC), NCRP: National Council on Radiation Protection and Measurements
The recently published European Association of Percutaneous Cardiovascular Interventions (EAPCI) statement on Radiation Exposure and Safety in Catheterization Laboratories for Health-care Professionals during Pregnancy reported global data from practice and found pregnant[25] interventional cardiologists monitoring their under-lead thresholds report measured under-lead doses well below these legal thresholds.[23,26-31]
How can we monitor and limit any risk? Safe practices that minimize radiation exposure
Occupational radiation management and risk mitigation are essential for all interventional cardiologists. All workers should aim to keep exposure as low as reasonably possible (ALARA). Research demonstrates 50–86% of female cardiologists and interventional cardiologists work in coronary catheterization laboratories with occupational radiation during pregnancy.[30,31] Critical organogenesis (weeks 2–8) is a particularly important time to limit radiation exposure and ensure good radiation safety practices, while timing of notification and confidentiality are also important issues to navigate in the first trimester.
Critical practices to minimize exposure should be adopted, including dosimeter use, monitoring, and well-maintained protective shielding. A separate under-lead fetal radiation counter or dosimeter badge with monthly monitoring is highly recommended and often mandated. Case by case dose monitoring can also be extremely reassuring and help to guide ALARA practices, and as documented in the EAPCI consensus statement, are often used. Safe fluoroscopy practices are essential, these include using fluoroscopy-store technology (last hold imaging) to minimize unnecessary cineangiography, minimizing radiation “on time,” choosing appropriate angle selection with lower radiation doses, scatter minimization with low image intensifier position, and minimization of magnification and frame rate.[8,28,29] Weightless lead and robotics percutaneous coronary intervention tools, where available, can provide alternative potential options for radiation protection. Mobile Perspex or lead shields should be available in all labs and careful positioning close to the operator should be used. Old equipment should be regularly updated as doses delivered by aging equipment increase dose and risk. Some countries such as Australia embed equipment update mandates into funding policy, to facilitate safe practice. There is an ethical imperative for institutions, managers, funding bodies and governments to take responsibility for equipment replacement, servicing, and updates to provide appropriate protection for all occupational radiation safety workers. All trainees should receive radiation safety training and part of advanced training and interventional fellowships, so they understand the importance of time, distance, and shielding to reduce radiation exposure.[4,8,20,22] Trainees should be directed to radiation safety courses and resources within hospitals which should include overt statements about pregnancy risk that are accurate and evidence based. Online resources such as the Women as One radiation safety initiative and tutorial,[20] society for cardiovascular angiography and interventions (SCAI) consensus document,[3] and EAPCI statement[4] ensure equitable access to accurate information regardless of worksite.
Evidence-based thresholds for radiation exposure are important; however, guidance from regulatory bodies vary worldwide, so do regulations and practices.[4] Safety equipment including well-maintained lead gowns and shields, radiation counters to quantify risk, and nationally endorsed guidelines for safe exposure to radiation are all essential tools to mitigate risk. When we use and are aware of ALARA techniques to minimize exposure, risks to the fetus remain extremely low in appropriately shielded and monitored workers.[3,4,21,24]
For healthcare workers, themselves the risk of malignancy from poorly shielded sites, including the head and in some cases the breast, must also be considered and avoided. Lead gowns with arm and breast shields should be provided to workers. Postpartum, there is guidance suggesting that lactation and breastfeeding are not unsafe during ionizing radiation exposure[4,31] and interventionalists are advised to wear appropriately-sized upper torso lead aprons, and ideally leads with a lead sleeve to shield breasts, to provide additional protection to upper outer quadrant of the breast. Lead gowns should also be regularly screened for damage and stored carefully to limit the risk of damage.
Great leaders lead with evidence-based practice, and a goal of giving all of their staff a sense of belonging, and a career they love, without giving up on the joy of having a family. National societies should also provide readily accessible links to accurate educational materials, relevant policies, and legal requirements.
This editorial is written collectively by interventional cardiologists, ethicists, and leaders from nine different countries, most of us are also mothers. We have navigated the demands of training, on-call duties, demanding emergency work, and academic medicine; and worked safely with occupational radiation, it can safely be done. We have also done it so the women that follow in our footsteps have the role models they need.
DISCUSSION
The data presented in this review clearly demonstrates that, pregnant women can safely work in cardiac catheterization laboratories (with appropriate monitoring and shielding) with negligible risk to the developing fetus when well-maintained protective equipment is used. This review also found that when evaluating international policy and legislation almost all countries support ongoing uninterrupted catheterisation laboratory work for pregnant women, with thresholds for exposure that are conservative but easy to remain below. Data from this review supports risk mitigation with clinical practices to reduce minimize exposure dose, this does not require two sets of lead to be worn, a single set of leads, crossing at the front of 0.5mm thickness attenuates 98-99.5% of scatter radiation dose[21]. This review prioritizes the use of evidence-based medicine to inform advice we give (others and ourselves) when considering working pregnant in the coronary catheterisation laboratory. It debunks the myth women should not work in a coronary catheterisation laboratory’ while pregnant, and in doing so removes one important barrier to more diverse cardiology workforces. This review from key leaders in interventional cardiology from the Asia Pacific Society of Interventional Cardiology including authors from Australia, Saudi Arabia, Singapore, Japan, Indonesia, Bangladesh, India, and America reenforces the substantial work already performed by SCAI[3], EAPCI[4], and Women as One[4]. All groups draw the same simple conclusions and give the same advice- that working in the coronary catheterisation laboratories should be something women can safely choose to do. Data presented in this review agrees with and further validates statements and recommendations from EAPCI collaborative statements[4] with the European heart rhythm association (EHRA)[4] the European Associations of cardiovascular imaging (EACVI) [4] and Women as one (WAO)[4] and in SCAI[3] consensus documents. All reports of working while pregnant are safe, feasible and legal in most countries, and should be supported by our colleagues, leaders, institutions, and countries to avoid inequity.
CONCLUSION
It is not necessary for women in cardiology to feel that they must choose between a career in interventional cardiology/electrophysiology and the safety of their families. It is safe, legal (in most countries), and feasible to continue to work with occupational radiation while pregnant. Radiation exposure can be managed safely where appropriate care is taken. Commonly reported myths and fallacies must be addressed with readily accessible data. We need leaders in interventional cardiology and electrophysiology, who understand radiation concerns do not need to be a barrier to women in cardiology. Internationally interventional cardiology is the medical specialty with the most substantial under-representation of women. We need to ensure we have access to accurate information regarding pregnancy safety, to address cardiology’s workforce diversity issues for our trainees, our colleagues, and patients.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Mirvat Alasnag, Dr. Takahashi Saeko, Dr. Aasyha Cader, Dr. Sarita Rao is on the editorial board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Becoming a Parent During Cardiovascular Training. J Am Coll Cardiol. 2022;79:2119-26.
- [CrossRef] [PubMed] [Google Scholar]
- Women in Medicine: Addressing the Gender Gap in Interventional Cardiology. J Am Coll Cardiol. 2018;72:2663-7.
- [CrossRef] [PubMed] [Google Scholar]
- SCAI Consensus Document on Occupational Radiation Exposure to the Pregnant Cardiologist and Technical Personnel. EuroIntervention. 2011;6:866-74.
- [CrossRef] [PubMed] [Google Scholar]
- Radiation Protection for Healthcare Professionals Working in Catheterisation Laboratories During Pregnancy: A Statement of the European Association of Percutaneous Cardiovascular Interventions (EAPCI) in Collaboration with the European Heart Rhythm Association (EHRA), the European Association of Cardiovascular Imaging (EACVI), the ESC Regulatory Affairs Committee and Women as One. EuroIntervention. 2023;19:53-62.
- [CrossRef] [PubMed] [Google Scholar]
- Motivations for and Barriers to Choosing an Interventional Cardiology Career Path: Results from the EAPCI Women Committee Worldwide Survey. EuroIntervention. 2016;12:53-9.
- [CrossRef] [PubMed] [Google Scholar]
- Representation of Women in Internal Medicine Specialties in North America, the United Kingdom, and Australasia: Cardiology's Outlier Status and the Importance of Diversity. Am J Cardiol. 2022;185:122-8.
- [CrossRef] [PubMed] [Google Scholar]
- Career Preferences and Perceptions of Cardiology among Us Internal Medicine Trainees Factors Influencing Cardiology Career Choice. JAMA Cardiol. 2018;3:682-91.
- [CrossRef] [PubMed] [Google Scholar]
- Radiation Safety Considerations for the Female Interventionist. Endovascular Today.
- [Google Scholar]
- Under-Representation of Women as Proceduralists and Patients in TAVR and TMVR Procedures: Data, Implications, and Proposed Solutions. Eur Cardiol Rev. 2022;17:e27.
- [CrossRef] [PubMed] [Google Scholar]
- Radiation Exposure in Pregnant and Nonpregnant Female Interventional Radiology Workers. Radiol Technol. 2016;87:574-8.
- [Google Scholar]
- Gender Equity within Medical Specialties of Australia and New Zealand: Cardiology's Outlier Status. Intern Med J. 2020;50:412-9.
- [CrossRef] [PubMed] [Google Scholar]
- Pregnancy and the Working Interventional Radiologist. Semin Intervent Radiol. 2013;30:403-7.
- [CrossRef] [PubMed] [Google Scholar]
- Radiation Exposure in Pregnant and Non-pregnant Female Interventional Radiology Workers. J Vasc Interv Radiol. 2014;25:S100.
- [CrossRef] [Google Scholar]
- Occupational Radiation Exposure to Interventional Radiologists: A Prospective Study. J Vasc Interv Radiol. 1992;3:597-606.
- [CrossRef] [PubMed] [Google Scholar]
- Differences in Management and Outcomes for Men and Women with ST-elevation Myocardial Infarction. Med J Aust. 2018;209:118-23.
- [CrossRef] [PubMed] [Google Scholar]
- Physician Characteristics Associated with Higher Adenoma Detection Rate. Gastrointest Endosc. 2018;87:778-86.e5.
- [CrossRef] [PubMed] [Google Scholar]
- Sex Preferences for Colonoscopists and GI Physicians among Patients and Health Care Professionals. Gastrointest Endosc. 2011;74:122-7.e2.
- [CrossRef] [PubMed] [Google Scholar]
- Influence of Gender of Physicians and Patients on Guideline-recommended Treatment of Chronic Heart Failure in a Cross-sectional Study. Eur J Heart Fail. 2009;11:299-303.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of Late Cardiac Death and Myocardial Infarction Rates in Women Vs Men With ST-Elevation Myocardial Infarction. Am J Cardiol. 2020;128:120-6.
- [CrossRef] [PubMed] [Google Scholar]
- Sex Disparities in Myocardial Infarction: Biology or Bias? Hear Lung Circ. 2020;30:18-26.
- [CrossRef] [PubMed] [Google Scholar]
- Radiation Safety in the Practice of Cardiology: What All Women Should Know (Women as One: Radiation Safety Toolkit) Available from: https://www.rad.womenasone.org [Last accessed on 2024 Mar 05]
- [Google Scholar]
- Human Exposure to High Natural Background Radiation: What Can It Teach Us About Radiation Risks? J Radiol Prot. 2009;29:A29-42.
- [CrossRef] [PubMed] [Google Scholar]
- Radiation Protection Measures and Sex Distribution in European Interventional Catheterisation Laboratories. EuroIntervention. 2020;16:80-2.
- [CrossRef] [PubMed] [Google Scholar]
- Mantel-Haenszel Analysis of Oxford Data. II. Independent Effects of Fetal Irradiation Subfactors23. JNCI J Natl Cancer Inst. 1976;57:1009-14.
- [CrossRef] [PubMed] [Google Scholar]
- Council Directive 2013/59/Euratom of 5 December 2013 Laying Down Basic Safety Standards for Protection against the Dangers Arising from Exposure to Ionising Radiation, and Repealing Directives 89/618/Euratom, 90/641/Euratom, 96/29/Eurat. Official Journal of the European Union, 17.1.2104, L 13/1
- [Google Scholar]
- Radiation Exposure to the Pregnant Interventional Cardiologist. Does It Really Pose a Risk to the Fetus? Rev Española Cardiol (English Ed). 2017;70:606-8.
- [CrossRef] [PubMed] [Google Scholar]
- on Behalf of Women in Interventional Cardiology of Australia and New Zealand (WIICAN) Unpublished Data on Pregancy in Female Interventional Cardiologists of Australia and New Zealand.
- [Google Scholar]
- Women in Interventional Cardiology: The French Experience. Ann Cardiol Angeiol (Paris). 2016;65:468-71.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiovascular Medicine and Society: The Pregnant Cardiologist. J Am Coll Cardiol. 2017;69:92-101.
- [CrossRef] [PubMed] [Google Scholar]
- Pregnancy During Cardiology Training. JACC Case Rep. 2019;1:221-4.
- [CrossRef] [PubMed] [Google Scholar]
- Committee Opinion No. 723: Guidelines for Diagnostic Imaging During Pregnancy and Lactation. Obstet Gynecol. 2017;130:e210-6.
- [CrossRef] [PubMed] [Google Scholar]








