Translate this page into:
Pseudoaneurysm of Ascending Aorta with Sternal Erosion after Double Valve Replacement—A Case Report
Amaresh Rao Malempati, MS, MMch Additional Professor CT Surgery, Nizam's Institute of Medical Sciences Panjagutta, Hyderabad 500082, Telangana India raoamareshm@yahoo.co.in
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Pseudoaneurysm of ascending aorta is a rare complication after aortic surgery. Predisposing factors can be infection, chronic hypertension, connective tissue disorders, or dissection. Chest pain, sternal erosion, dysphagia, or stridor can be the modes of presentation. It can also present as a pulsatile mass. Redo sternotomy in a case of pseudoaneurysm of aorta can cause fatal hemorrhage or air embolism. In such a scenario, femorofemoral bypass and hypothermic circulatory arrest help to simplify the approach to the pseudoaneurysm. The authors present a case of a 23-year-old female with pseudoaneurysm of the ascending aorta causing sternal erosion. Ascending aortic repair was done using Dacron patch with femorofemoral bypass and hypothermic circulatory arrest. Sternum was repaired using pectoralis major muscle flap.
Keywords
pseudoaneurysm
cardiopulmonary bypass
deep hypothermic circulatory arrest
Introduction
Thoracic aortic pseudoaneurysm is an uncommon complication of cardiac or aortic surgery. Its incidence is < 0.5%.1 The cause is disruption of the intima and media of the aorta with the resultant swelling being contained by the adventitia and the surrounding mediastinal structures. Other factors can be either trauma or infection.2 The major risk factor for ascending aortic pseudoaneurysm is leak from aortic cannulation site.3
Pseudoaneurysms can also occur at previous venting, aortotomy, anastomotic site or proximal vein graft sites. The various mechanisms implicated are anastomotic technique, infection, and intrinsic aortic wall disease. The lesion can be detected initially by a chest X-ray (posteroanterior view), which will show widening of the mediastinum. The diagnostic test is computed tomographic aortogram (CT aortogram).4 Repair of such a fragile lesion is a surgical challenge.
Case Presentation
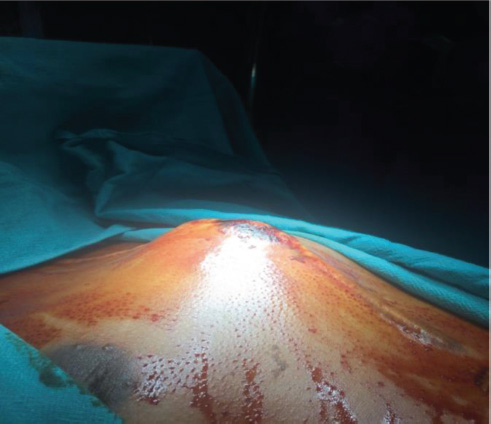
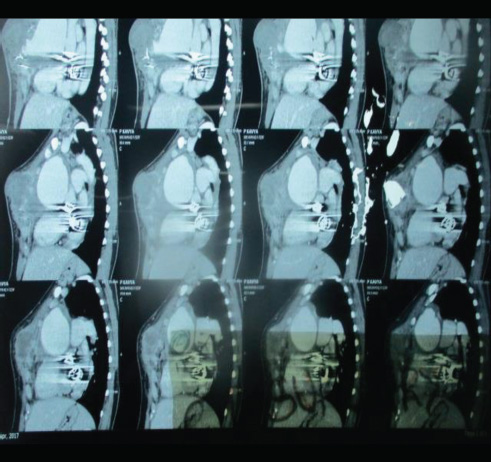
A 23-year-old female patient presented with complaints of fever on and off for 6 months and pulsatile swelling in front of the chest for 1 month. One year back, she was operated for rheumatic valvular heart disease of severe mitral and aortic stenosis with mitral valve replacement of 25 mm and aortic valve replacement of 19-mm Chitra valves. She was not a known hypertensive or diabetic. On examination, the patient was febrile with a temperature of 101°F. Pulsatile mass of 8 × 7 cm was noted in front of sternum (Fig. 1). On chest X-ray, mediastinal widening was present (Fig. 2). Two-dimensional (2D) echo showed that both prosthetic valve leaflets were moving well, no increased gradients across valves or paravalvular leak were noted, and biventricular function was good. On a CT aortogram, pseudoaneurysm of size 8 × 7 cm size was noted (Figs. 3 4).
-
Fig. 1 Pseudoaneurysm eroding the sternum with impending rupture.
Fig. 1 Pseudoaneurysm eroding the sternum with impending rupture.

-
Fig. 2 Mediastinal widening on chest X-ray.
Fig. 2 Mediastinal widening on chest X-ray.

-
Fig. 3 CT scan showing pseudoaneurysm eroding the sternum.
Fig. 3 CT scan showing pseudoaneurysm eroding the sternum.
-
Fig. 4 Sagittal section of CT scan showing sternal erosion.
Fig. 4 Sagittal section of CT scan showing sternal erosion.
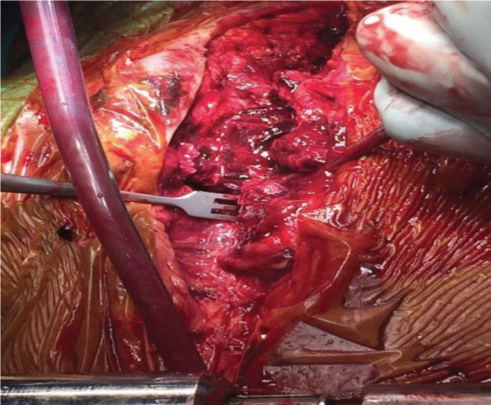
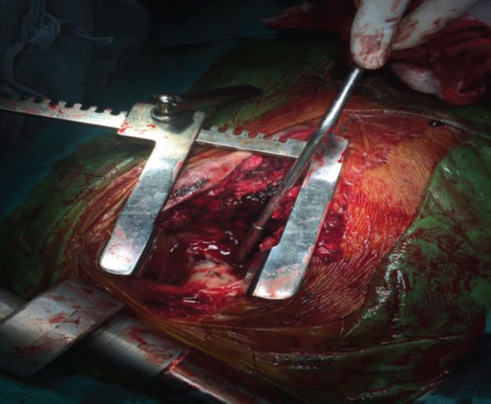
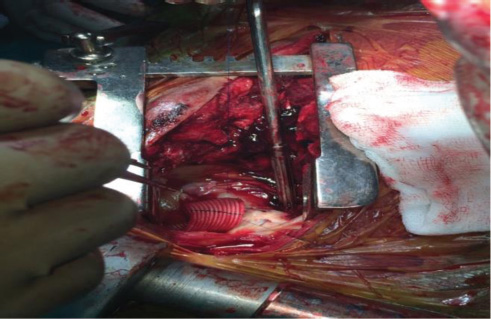
We operated on the patient with a femorofemoral bypass with deep hypothermic circulatory arrest for 20 minutes. After circulatory arrest was achieved on femorofemoral bypass, midline sternotomy was done. Intraoperatively, there were dense adhesions present in the mediastinum (Fig. 5). We removed all blood clots and released adhesions. After clearing the surgical field, we noted a defect of size 3 × 2 cm at the aortotomy site on the right side (Fig. 6), closed the defect with Dacron patch, and reinforced with pledgeted sutures (Fig. 7). After that cardiopulmonary bypass reinitiated, the patient was rewarmed to 36°C and came off bypass in normal sinus rhythm. We temporarily closed the skin, and after 24 hours, sternal reconstruction was done with pectoralis muscle flap (Fig. 8). Postoperatively, the patient was kept on broad-spectrum antibiotics and was discharged on 15th postoperative day. On follow-up, the patient was doing well till then.
-
Fig. 5 Intraoperative picture showing instrument at edge of eroded sternum after clot evacuation.
Fig. 5 Intraoperative picture showing instrument at edge of eroded sternum after clot evacuation.
-
Fig. 6 Instrument pointing to rent in ascending aorta.
Fig. 6 Instrument pointing to rent in ascending aorta.
-
Fig. 7 Closing of rent with Dacron patch.
Fig. 7 Closing of rent with Dacron patch.

-
Fig. 8 Sternal reconstruction with pectoralis major muscle flap.
Fig. 8 Sternal reconstruction with pectoralis major muscle flap.
Discussion
Morbidity and mortality of pseudoaneurysm of the ascending aorta is between 29 and 46%.5 This is due to the fatal hemorrhage from rupture of the lesion. Therefore, a pseudoaneurysm should be operated upon soon after diagnosis. When such a lesion is located anteriorly, is large and eroding into the sternum, risk of massive hemorrhage during sternotomy or surgery is very high.6 So it is important to be careful during redo sternotomy. Another important aspect is preservation of cerebral perfusion.6 Authors have described various methods of initiating cardiopulmonary bypass prior to redo sternotomy.1 6 7 The best approach depends on the site and the size of the pseudoaneurysm. Femoral or axillary artery cannulation has been suggested as the most feasible.
Mohammadi et al8 used bilateral carotid artery cannulation and femorofemoral bypass in nine patients. Bachet et al,7 in 2007, directly cannulated both carotids in five patients. They argued that it preserved cerebral blood flow and also maintained systemic flow. However, subjects in both these studies experienced neurological sequelae. Carotid artery cannulation has not been widely used due to the risk of stroke.
Alternative novel approaches such as use of atrial septal defect occluder device for closure of the pseudoaneurysm might be tried in selected patients.9
Hypothermic circulatory arrest decreases the intravascular volume and provides cerebral protection. Thereby, it gives the surgeon some time to dissect, define, and repair the lesion. It also prevents sudden, extreme blood loss.10
Conclusion
Repair of a large pseudoaneurysm of the ascending aorta via redo median sternotomy entails high risk of fatal hemorrhage. Femorofemoral bypass and moderate hypothermia with transient circulatory arrest help safe conduct of surgery.
Conflicts of Interest
None.
References
- Mediastinal false aneurysm after thoracic aortic surgery. Ann Thorac Surg. 2000;70(02):547-552.
- [Google Scholar]
- Tuberculous pseudoaneurysms of the aortic arch. J Thorac Cardiovasc Surg. 2003;125(02):411-412.
- [Google Scholar]
- Pseudoaneurysm of the ascending aorta following cardiac surgery. Chest. 1988;93(01):138-143.
- [Google Scholar]
- Computed tomography in the diagnosis of iatrogenic false aneurysms of the ascending aorta. AJR. 1984;142:117-118.
- [Google Scholar]
- Management of a pulsatile mass coming through the sternum. Pseudoaneurysm of ascending aorta 35 years after repair of tetralogy of Fallot. Interact Cardiovasc Thorac Surg. 2010;10(05):820-822.
- [Google Scholar]
- Surgical management of a giant ascending aortic pseudoaneurysm. Tex Heart Inst J. 2010;37(06):710-713.
- [Google Scholar]
- Reoperation for giant false aneurysm of the thoracic aorta: how to reenter the chest? Ann Thorac Surg. 2007;83(05):1610-1614.
- [Google Scholar]
- Reoperation for false aneurysm of the ascending aorta after its prosthetic replacement: surgical strategy. Ann Thorac Surg. 2005;79(01):147-152. , discussion 152
- [Google Scholar]
- Novel treatment approach to ascending aorta pseudoaneurysms: a case report. J Tehran Heart Cent. 2017;12(03):134-137.
- [Google Scholar]
- Pseudoaneurysm of the ascending thoracic aorta years after aortic valve replacement. Cardiovasc Revasc Med. 2018;19(02):196-98.
- [Google Scholar]







