Translate this page into:
Prevalence of Metabolic Syndrome in Female Patients with Psoriasis
*Corresponding author: Deepthi Konda, Department of Dermatology, All India Institute of Medical Sciences, Bibinagar, Telangana, India. knddeepthi@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Konda D, Mathurthi G, Taranikanti M. Prevalence of Metabolic Syndrome in Female Patients with Psoriasis. Indian J Cardiovasc Dis Women. 2024;9:221-4. doi: 10.25259/IJCDW_65_2023
Abstract
Introduction:
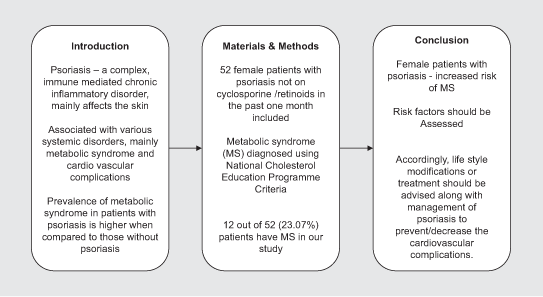
Psoriasis is a complex, immune mediated chronic inflammatory disorder that mainly affects the skin, joints, scalp and nails and also various systems of the body. Of the various systems involved, cardiovascular diseases and metabolic syndrome are of major concern due to their increased risk of morbidity and mortality.
Objectives:
To estimate the prevalence of Metabolic syndrome in female patients with psoriasis.
Materials and methods:
52 female psoriatic patients were recruited in the study and various components of metabolic syndrome i.e waist circumference, blood pressure. Serum triglycerides, high density lipoproteins, glucose levels were assessed.
Results:
In our study on 52 female psoriatic patients, 12 patients (23.07%) had metabolic syndrome.
Conclusion:
Psoriatic patients are at an increased risk of cardiovascular diseases which should be taken into account while treating psoriasis
Keywords
Psoriasis
Metabolic syndrome
Female
ABSTRACT IMAGE
INTRODUCTION
Psoriasis is a complex, immune-mediated, and inflammatory disorder that mainly affects the skin, scalp, joints, and nails.[1] The previous studies have showed the relationship between psoriasis and systemic disorders such as anxiety, depression, increased risk of cardiovascular diseases, inflammatory bowel disease, and metabolic syndrome (MS).[2,3] These associations led to the concept of psoriasis being considered as a systemic disease rather than a cutaneous disease. MS is a tetrad of hypertension, glucose intolerance, hyperlipidemia, and obesity. Psoriasis, irrespective of its body surface area involvement, severity, nails, or joints involvement is known to be associated with MS. Moreover, the presence of MS increases the risk of developing cardiovascular disorders. Thus, psoriasis may be an indirect but important risk for cardiovascular morbidity and mortality, especially in middle aged and young patients.[4] Various factors such as anxiety, depression, cigarette smoking, alcohol consumption, homocysteneimia, social withdrawal, and obesity are relatively more common in psoriatic patients which, further, add to the cardiovascular risk profile in them. Furthermore, the commonly used oral drugs for management of psoriasis such as cyclosporine and retinoids can also aid in worsening the MS components such as hypertension and hyperlipidemia. Certain studies have showed the estimated prevalence of MS to be 30-50% among psoriasis patients when compared to 15–24% in the non-psoriatic general population.[3-5] This increased prevalence has to be taken into consideration while treating psoriasis patients and risk factors have to be properly assessed and treated accordingly along with psoriasis management. However, there are no studies on only female psoriatic patients and MS. Hence, this project was taken up to study about the prevalence of MS in female psoriatic patients.
Aims and objectives
The aim of this study was as follows:
To estimate the prevalence of MS in female patients with psoriasis.
MATERIALS AND METHODS
This was a hospital-based cross-sectional study, and it was done in our Department of Dermatology in a tertiary care hospital in Bibinagar, Telangana. Approval was obtained from the Institution Ethics Committee before starting the study. Written informed consent was then obtained from all the participants before enrolling them in the study. All the consecutive 52 female patients with psoriasis attending the dermatology out-patient department and fulfilling the following criteria were recruited as participants.
Inclusion criteria
Female patients with clinically and/or biopsy proven psoriasis of at least 3 months duration and not on oral cyclosporine and retinoids in the past 1 month were included in the study.
Exclusion criteria
Age of the patients <18 years and patients who are pregnant at the time of the study:
After enrolling, sociodemographic data such as age, occupation, and comorbidities like hypertension and diabetes mellitus were documented. Details of psoriasis such as age of onset of psoriasis, number of exacerbations, duration of psoriasis, treatment (topical/oral/native) history, and family history of psoriasis were documented. Then, body surface area (BSA) involved by psoriasis, scalp scaling, nail changes, joint pain, and swelling were entered in the pro forma. Various components of MS were assessed as follows. Circumference of the waist was measured at the level of the uppermost part of the pelvic bone. For serum triglycerides, high-density lipoproteins, and glucose levels, around 5 mL of venous blood sample was collected from the patients under strict aseptic conditions, after overnight fast. Blood pressure was recorded with the cuff on the right arm of the patient in a sitting position. Two readings were taken with an interval of 15 min and blood pressure was the average of two readings. The patient was said to have MS if she had three or more of the following criteria.[6] High-density lipoprotein <50 mg/dL, waist circumference >35 inches, triglycerides >150 mg/dL, blood pressure >130/85 mmHg, and fasting glucose >l00 mg/dL.
The collected data were then analyzed using the Statistical Package for the Social Sciences (version 13, Illinois, USA).
RESULTS
A total of 52 female patients with psoriasis were included in the study. Various study parameters in the study population are shown in Table 1.
| Parameter | Study population (52 patients) |
|---|---|
| Mean age | 45.55±8.35 years |
| Age of onset of psoriasis | 28.36±6.32 years |
| Mean body surface area (%) | 16.20±3.89% |
| Scalp involvement | 15/52 (28.8%) |
| Nail involvement | 6/52 (11.53%) |
| Joint involvement | 10/52 (19.23%) |
| Metabolic syndrome | 12/52 (23.07%) |
Sociodemographic
The age of the patients was ranging from 20 to 62 years with mean age being 45.55 years (±8.35). Of the 52 patients, housewives constituted 90%, and professions such as manual labor, farmer, student, and house help contributed to remaining 10%.
Comorbidities
Twelve out of 52 patients (23%) had hypertension and 21 out of 52 patients (40%) had diabetes mellitus.
Clinical details of psoriasis
Mean age at the onset of psoriasis was 28.36 (±6.32) years. The mean duration of psoriasis was 1.1 (±4.52) years. Out of 52 patients, scalp was affected in 15 patients, nail changes in the form of nail pitting were seen in six patients, and joint involvement in the form of joint pain and swelling was seen in ten patients. The mean BSA involved by psoriasis was 16.20 (±3.89)%.
MS
MS was diagnosed in 12 out of 52 (23.07%) female patients with psoriasis in our study.
DISCUSSION
Studies by Nijsten and Wakkee,[2] Gottlieb et al.,[3] and few other studies showed that MS is relatively more common in psoriatic patients when compared to those without psoriasis. Various theories have been considered to explore the relation between psoriasis and MS. The important pathogenetic feature of psoriasis is persistent inflammation. T helper 17 cells produce several cytokines, of which interleukin (IL)-17, tumor necrosis factor-α, and IL-22 are important and they result in differentiation and hyperproliferation of keratinocytes, thus increasing the risk of psoriasis. These cytokines are also known to be implicated in the pathogenesis of obesity, diabetes mellitus, hypertension, and hyperlipidemia. Thus, the common cytokine milieu is likely to increase the risk of MS in psoriasis.[7]
Proinflammatory cytokines released in psoriasis are known to increase oxidative stress and endoplasmic reticulum stress which lead to increased insulin resistance, diabetes mellitus, and obesity which are major components of MS. Adiponectin, a cytokine released from adipose tissue decreases the triglyceride levels, increases high-density lipoprotein levels and is thus a protective agent against obesity. However, in psoriasis patients, it is seen that adiponectin levels are decreased which, in turn, can lead to obesity, thus increasing the risk of development of MS.[7]
Zindancı et al.[8] conducted a study that showed a 53% prevalence of MS as 53% in psoriatic patients in comparison to those without psoriasis. Similarly, the prevalence of MS was 30.1% in psoriasis patients.[1] The prevalence of MS in female patients with psoriasis in our study was 23.07%. Furthermore, our study was only on female patients and that can explain the relatively low prevalence of MS in our study. Nisa and Qazi[9] showed prevalence of MS as 28% in 150 psoriasis patients. Mebazaa et al.[10] conducted a study comparing the prevalence of MS in psoriatic patients (35.5%) and controls (30.8%). It was relatively more in psoriatic patients. However, this difference of MS in psoriatic patients and controls was not found in a study conducted by Kim et al. (P = 0.2).[11] The difference in the ethnicity, genetic makeup, occupation with immobile nature, physical activity, and food habits can explain the variation in prevalence of MS in various studies.[12]
CONCLUSION
Patients with psoriasis including female patients are at increased risk of MS when compared to the general population. This should be taken into consideration and risk factors have to be properly assessed, and accordingly, lifestyle modifications or treatment should be advised along with management of psoriasis to prevent or decrease the cardiovascular complications.
Ethical approval
The research/study was approved by the Institutional Review Board at All India Institute of Medical Sciences, number AIIMS/BBN/IEC/SEPT/2023/311-R, dated 28 October 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Audio summary available at
Financial support and sponsorship
Nil.
References
- Prevalence of Metabolic Syndrome in Patients with Psoriasis: A Hospital-Based Case-Control Study. Br J Dermatol. 2007;157:68-73.
- [CrossRef] [PubMed] [Google Scholar]
- Complexity of the Association between Psoriasis and Comorbidities. J Invest Dermatol. 2009;129:1601-3.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term Prognosis in Patients with Psoriasis. Br J Dermatol. 2008;159(Suppl 2):2-9.
- [CrossRef] [PubMed] [Google Scholar]
- Scoring Systems in Dermatology. Indian J Dermatol Venereol Leprol. 2006;72:315-21.
- [CrossRef] [PubMed] [Google Scholar]
- Third Report of the National Cholesterol Education Program Export Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) 2002. Washington, DC: National Cholesterol Education Program, National Heart, Lung, and Blood Institute; National Institutes of Health; NIH Publication No. 2-5215. Available from: https://www.nhlbi.nih.gov/guidelines/cholesterol/atp3xsum.pdf [Last accessed on 2023 Nov 23]
- [Google Scholar]
- Metabolic Syndrome and Psoriasis: Mechanisms and Future Directions. Front Immunol. 2021;12:711060.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of Metabolic Syndrome in Patients with Psoriasis. ScientificWorldJournal. 2012;2012:312463.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of Metabolic Syndrome in Patients with Psoriasis. Indian J Dermatol Venereol Leprol. 2010;76:662-5.
- [CrossRef] [PubMed] [Google Scholar]
- Metabolic Syndrome in Tunisian Psoriatic Patients: Prevalence and Determinants. J Eur Acad Dermatol Venereol. 2011;25:705-9.
- [CrossRef] [PubMed] [Google Scholar]
- Analysis of Cardiovascular Risk Factors and Metabolic Syndrome in Korean Patients with Psoriasis. Ann Dermatol. 2012;24:11-5.
- [CrossRef] [PubMed] [Google Scholar]
- The Metabolic Syndrome in South Asians: Epidemiology, Determinants, and Prevention. Metab Syndr Relat Disord. 2009;7:497-514.
- [CrossRef] [PubMed] [Google Scholar]







