Translate this page into:
Physiological Significance of Myocardial Bridging by Fractional Flow Reserve—An Observational Study
Ashwin Kumar Panda, DNB Department of Cardiology, Nizam's Institute of Medical Sciences Punjagutta, Hyderabad 500082 India ashwin.blossom@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract

Background Myocardial bridge (MB) is a portion of an epicardial coronary artery that takes an intramuscular course. The systolic compression of MB often gets carried over to early and mid-diastole, compromising coronary blood flow. In clinical practice, we encounter patients with angina, non-invasive evidence of ischemia, and a MB as the only relevant finding on angiography. In view of studies in support of decreased coronary flow reserve in MB, we assessed the physiological significance of MB by fractional flow reserve (FFR).
Methods and Results We enrolled eight patients with chronic stable angina and positive noninvasive stress test, who had no significant CAD, and with evidence of MB in the left anterior descending artery. Mean age of population was 57.14 ± 6.25 years. Two (25%) were females and six (75%) were males. Four (50%) were smokers, five (62.5%) were diabetics, and two (25%) were hypertensives. Mean length of MB is 19.4 ± 5.04 mm. All underwent physiological assessment by FFR and the baseline, post nitroglycerin (NTG), and post adenosine readings were noted. Mean pre-NTG value, post-NTG, and post-adenosine were 0.974 ± 0.022, 0.96 ± 0.03, and 0.88 ± 0.042 (≤0.80 hemodynamically significant) respectively. Paired t-test showed significant reduction in FFR after NTG (p = 0.0452) and post-adenosine (p = 0.011) but all eight patients did not get significant FFR.
Conclusion MB was found to be physiologically insignificant in our group of patients. But a statistical significant reduction of FFR in MB, post NTG and post adenosine, does impress on the fact that, an extensive study over a longer period of course, could throw light on this unsettled area of physiological significance and optimal therapeutic approach.
Keywords
myocardial bridging
fractional flow reserve
treadmill test
non invasive stress imaging
Introduction
The usual anatomical position of the coronary arteries is between the pericardium and epicardium. Reyman in the year 1732, first described an incidental autopsy finding in which a portion of an epicardial coronary artery gets “tunneled” either partially or completely within the myocardial fibers and takes an intramuscular course for a varying length,1 called myocardial bridging (MB). At the time of its discovery, it was thought to be a benign cardiovascular anomaly.
The prevalence rate of MB is unknown, and rate of detection varies with the imaging modality of choice. The reported prevalence of MB is between 2 and 6% by coronary angiography and 19 and 22% by coronary computed tomography angiography.2 3 The current gold standard in identification of MB are autopsy studies, with a prevalence approaching 33 to 42%.2 4 5 Around 67 to 98% of MBs were found in the LAD, more particularly in the proximal and mid-LAD segments. Less commonly affected are the left circumflex and right coronary artery.6
Various factors have been linked to the significant variation in prevalence of MB across imaging modalities; these include the varying length and depth of myocardial tissue encompassing the tunneled artery, the axial orientation of the coronary artery in relation to the myocardial fibers, the presence of a fixed stenosis proximal to the MB, the presence of connective or adipose tissue opposing the tunneled segment, a concomitant aortic outflow obstruction, intrinsic tone of the coronary artery wall, significant hypotension, vasopressor use at the time of imaging, and intraobserver variability.7
Around 85% of coronary blood flow occurs during diastole, while MB is characterized by systolic coronary compression, thereby pointing toward its benign nature. However, the reality is much more complex and set into play by the interaction of anatomical and physiological factors that influence each other dynamically. The fact that the dynamic stenosis of MB differs significantly from the fixed type of atherosclerotic epicardial stenosis8 has been displayed by bioengineering models and invasive coronary testing. It has been observed that significant compromise of the coronary blood flow occurs due to the systolic compression of the tunneled segment in MB which often gets carried over to early and mid-diastole.9 This presents a diagnostic and therapeutic challenge in symptomatic patients despite its benign nature.
MB in many cases may be responsible for adverse complications including angina, myocardial ischemia,10 acute coronary syndromes,11 left ventricular dysfunction and stunning,12 arrhythmias,13 and even sudden cardiac death.
An association was found between MB and atherosclerosis. The proposed pathogenesis includes the role of perivascular adipose tissue and modified biomechanical forces. A frictional force acting tangential to the flow called wall shear stress (WSS), might contribute to the development of endothelial dysfunction and atherosclerosis and is thought to be possible by induction of changes in inflammatory pathways. An area of low WSS is created due to the sudden stop of the propagating ante grade systolic wave, leading to the development of an atherosclerotic plaque proximal to the MB.
The MB or the tunneled segment of the artery, is relatively free from plaque and this has been attributed to the absence of perivascular adipose tissue in the epicardium surrounding it, leading to proinflammatory signaling pathways elsewhere.14 Absence of adventitial vasa vasorum has been identified in this area by OCT imaging,15 which might act as a channel for propagation of inflammatory cells and cytokines from perivascular adipose tissue at the tunneled segment. Compression of MB also leads to better lymphatic clearance of inflammatory cells.16
In routine clinical practice, among patients with angina, frequent coronary angiography findings are noninvasive evidence of myocardial ischemia and an MB.
In view of studies in support of decreased coronary flow reserve in MBs, a more thorough identification of the hemodynamic significance of MBs is important to guide therapeutic approach. In this study, we contemplated to study the physiological significance of MB in patients positive for a non-invasive stress test.
Materials and Methods
This was an observational prospective study done over a span of 3 months in Nizam's Institute of Medical Sciences, Hyderabad. Patients who were more than 18 years with symptoms of angina or shortness of breath and have undergone a non-invasive stress test; and found to have normal coronaries or an otherwise insignificant disease but with MB as the only finding were included in the study. Patients with contraindications to adenosine like severe asthma, chronic obstructive pulmonary disease, advanced heart degree block, and patients with significant coronary artery disease were excluded from the study.
The non-invasive stress tests employed are treadmill test (TMT), dobutamine stress test with Thallium-single photon emission computer tomography (DST-SPECT). Selected patients underwent physiological assessment by fractional flow reserve (FFR) (Pressure wire Aeris Agile Tip by St. Jude's Medical). The baseline, Post NTG, and post adenosine readings were noted after intracoronary bolus doses of 40 to 80 µg NTG and 100 to 200 µg of single or two intracoronary adenosine doses. The baseline, post NTG, and post adenosine readings were noted.
Statistical Analysis
The data available so far on MB is mainly from case reports. In view of paucity of studies from Indian subcontinent, we have taken data from an unpublished study on MB at our institute, as a reference. In their study, out of 526 angiographies done over a span of 1 year, 25 patients were found to have MB and out of them nine patients were found to have positive stress test, amounting to 1.8%. So, taking this into consideration, and substituting in Cochrane's equation for sample size, and adjusting it to the study duration of 3 months, we anticipated a study size of 15 patients. However, as a part of series study, we have taken all patients who satisfied our inclusion and exclusion criteria over a span of 3 months and we could include only eight patients in the study.
The formula used for calculating sample size is Cochrane's equation:
n = Z 2 pq/e 2
n = sample size, Z-value for 95% confidence interval is 1.96, p = prevalence (proportion) of the attribute in question (here, it is 0.018), q = 1 − p (here, it is 0.782).
Data was collected, compiled using Microsoft Excel and statistical analysis was done using SSPS v20. Results on continuous variables were presented as mean and standard deviation. Results on categorical variables were presented as percentages. Paired “t” test was applied to the data to establish the significance of administration of NTG and adenosine. All p-values are two-tailed, and p <0.05 was considered statistically significant.
Results
We prospectively enrolled eight patients over a span of 3 months with angina and/or positive non-invasive stress test. These patients were only enrolled into the study if they had no significant coronary artery stenosis, and with angiographic evidence of MB. All the eight patients had MB in the left anterior descending artery only. The baseline echocardiography was not suggestive of any specific ST-T changes in all eight patients, except for T inversions in three and avF in one patient which were of no significance. The non-invasive stress tests employed are TMT and DST-SPECT. TMT was positive in seven out of eight patients and DST was positive in one patient.
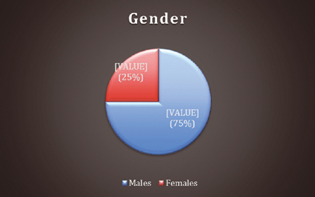
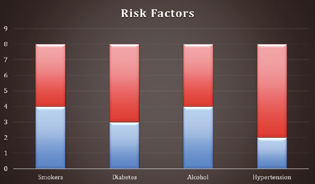
Mean age of population was 57.14 ± 6.25. 2 (25%) were females and six (75%) were males (Fig. 1). The distribution of risk factors (Fig. 2) was as follows: four (50%) were smokers, three (37.5%) were diabetics and two (25%) were hypertensives. Mean length of MB 19.4 ± 5.04 mm. Only two patients had one septal artery each originating from LAD in the MB segment. Only two patients were given nitrates prior to the study and none of the patients were on non-dihydropyridine calcium channel blockers.
-
Fig. 1 Distribution of males and females in the study population.
Fig. 1 Distribution of males and females in the study population.
-
Fig. 2 Distribution of risk factors in the study population.
Fig. 2 Distribution of risk factors in the study population.
All participants underwent physiological assessment by FFR or FFR (Pressure wire Aeris Agile Tip by St. Jude's Medical). The baseline, post NTG, and post adenosine readings were noted after intracoronary bolus doses of 40 to 80 µg NTG and 100 to 200 µg of single or two intracoronary adenosine doses. NTG was given to elicit hyperemic response and to augment the systolic compression of MB and severity of the same.
Mean pre-NTG value was 0.974 ± 0.022. Mean pre-adenosine/post-NTG value was 0.96 ± 0.03. Mean post-adenosine value was 0.88 ± 0.042. Paired t-test was employed to know the significant difference in the selected population before and after NTG boluses and before and after adenosine boluses.
Effect of NTG on MB was reflected by its reduction in FFR significantly, followed by p-value of 0.0452 by paired t-test (Table 1). Effect of adenosine was reflected by its reduction in FFR significantly followed by p-value of 0.011 (Table 2). However, FFR values ≤0.80 were considered indicative of hemodynamic significance of MB.
|
Pre NTG |
Post NTG |
p-Value (two-tailed) |
|
|---|---|---|---|
|
Mean ± SD |
0.974 ± 0.22 |
0.96 ± 0.03 |
0.045 |
|
Pre adenosine |
Post adenosine |
p-Value (two-tailed) |
|
|---|---|---|---|
|
Mean ± SD |
0.96 ± 0.03 |
0.88 ± 0.042 |
0.011 |
Discussion
In our study, done among patients with positive non-invasive stress test and presence of MB as an only finding on coronary angiogram, probably responsible for the positive stress test, FFR did not find any conclusive hemodynamic significance in all eight of the patients.
Among our study participants, only 50% patients were smokers, 37.5% were diabetics, and 25% were hypertensives—this did not seem to have any individual association with MB per se; however, in a study of 298,558 patients undergoing coronary angiography, patients with MB had higher rates of smoking, lower rates of cardiovascular risk factors like diabetes, chronic kidney disease, and prior MI.17
Coronary angiography as a diagnostic modality for MB is not without drawbacks, as presence of non-circular lumen morphology gets poorly delineated on two-dimensional angiography and nitroglycerin administration immediately prior to angiography does augment the severity of compression related to MB. Noninvasive modalities like dynamic CT myocardial perfusion imaging (CT-MPI) and machine learning-based CT-FFR18 were studied to assess the MB-related ischemia. While CT-MPI19 is considered the gold standard for noninvasive assessment, CT-FFRsystolic reliably excluded MB-related ischemia with high sensitivity and negative predictive value, but with poor specificity and positive predictive value.
IVUS has been used in a wide range of studies to assess MB using coronary angiography, but a lack of functional information of coronary blood flow and poor resolution limits its usage.20 Information about vulnerable plaque if any and varying degrees of fibrous intimal hyperplasia can be provided by OCT.21 However, rapid pullback and image acquisition, limit its use and fall behind IVUS for the assessment of MB.
In contrast to the above, both physiological and functional assessment of MB can be performed by pressure wire techniques. FFR is generally accepted as a gold standard for the functional assessment of obstructive atherosclerotic plaque. Schwartz et al22 who gave a classification for MBs, have suggested for intracoronary invasive hemodynamic assessment with FFR or diastolic FFR and a cut off value of 0.75 for significance.
In our study, a value of 0.80 was taken as a cut off and still all eight patients did not have significant hemodynamic compromise. However, the effect of NTG, as a provocative test, is justified by significant reduction in FFR, though not hemodynamically or physiologically, by a p-value of 0.042 by paired “t” test. The effect of adenosine as a stress challenge to MB is reflected by a significant reduction in FFR, by a p-value of 0.011 by paired “t” test, however, the reduction was not significant enough to cause physiological compromise of coronary circulation (mean FFR: 0.88 ± 0.042) in any of the eight cases.
While FFR measures mean pressure, a diastolic FFR or iFR (instantaneous free wave ratio) would be a better marker for physiological assessment of MB, as suggested by Escaned et al,23 who confirmed that MB predominantly affects diastolic hemodynamics. A recent study by Aleksandric et al,24 in which a head-to-head comparison was done between conventional FFR and diastolic FFR and that to with vasodilator and inotropic provocation, stated that d-FFR with inotropic stimulation, in comparison to vasodilation with adenosine, provided a more reliable physiological assessment of MB. However, conventional FFR did not find any significant difference in evaluation of MB with either of the provocative measures. The explanation provided was that, during inotropic stimulation, MB produces an increase of diastolic pressure difference Pa − Pd, but artificially negative systolic pressure difference (Pa − Pd) leading to artificial increase in conventional FFR values. An earlier study by Tarantini et al25 suggested that the use of diastole-specific indices like iFR would overcome the systolic decrease of pressure difference across the MB which might give rise to artificially high conventional FFR values.
There are certain limitations to labeling all the patients in the study as having benign MBs. First, it is difficult to apply the results of the study to the general population owing to a small sample size due to short duration of the study. Second, seven out of eight patients underwent TMT before undergoing CAG; more imaging-based stress scans would have helped us in identifying the exact area of ischemia and a better objective evidence of ischemia. Third, role of adenosine in assessment of hemodynamic evaluation of MBs was questioned in a study of limitations of FFR in MB,23 who suggested dobutamine as a better provocative test.
Conclusion
MB was found to be physiologically insignificant in our group of patients and be considered a benign entity. However, in view of small group of patients, we were unable to apply this to a larger group of population. But a statistically significant reduction of FFR in MB, post NTG and post adenosine, does impress on the fact that, an extensive study over a longer period of course, could perhaps throw light on this unsettled area of physiological significance and optimal therapeutic approach, for MB. However, in view of objective evidence of ischemia in the presence of MB, we strongly recommend the use of intracoronary hemodynamic evaluation of MB by FFR with or without dobutamine challenge.
Acknowledgment
I wish to extend my special thanks to Dr. Jyotsna Maddury, Professor and Head of the Department of Cardiology, NIMS, for her constant support and guidance throughout this project.
Conflict of Interest
None declared.
References
- Myocardial bridging: a meta-analysis of prevalence. J Forensic Sci. 2018;63(04):1176-1185.
- [Google Scholar]
- The prevalence and anatomical patterns of intramuscular coronary arteries: a coronary computed tomography angiographic study. J Am Coll Cardiol. 2007;49(05):587-593.
- [Google Scholar]
- The prevalence of myocardial bridging on multidetector computed tomography and its relation to coronary plaques. Pol J Radiol. 2019;84:e478-e483.
- [Google Scholar]
- Disturbed intracoronary hemodynamics in myocardial bridging: early normalization by intracoronary stent placement. Circulation. 1997;96(09):2905-2913.
- [Google Scholar]
- Transient integral boundary layer method to calculate the translesional pressure drop and the fractional flow reserve in myocardial bridges. Biomed Eng Online. 2006;5:42.
- [Google Scholar]
- New signs characteristic of myocardial bridging demonstrated by intracoronary ultrasound and Doppler. Eur Heart J. 1999;20(23):1707-1716.
- [Google Scholar]
- Myocardial bridging of the LAD in acute inferior wall myocardial infarction. Clin Cardiol. 2001;24:202-208.
- [Google Scholar]
- Myocardial stunning associated with a myocardial bridge. Int J Cardiol. 2002;82(01):65-67.
- [Google Scholar]
- Exercise-induced ventricular tachycardia in association with a myocardial bridge. Chest. 1991;99(05):1295-1296.
- [Google Scholar]
- Relationship between myocardial bridges and reduced coronary atherosclerosis in patients with angina pectoris. Int J Cardiol. 2013;167(03):883-888.
- [Google Scholar]
- Absence of adventitial vasa vasorum formation at the coronary segment with myocardial bridge—an optical coherence tomography study. Int J Cardiol. 2018;250:275-277.
- [Google Scholar]
- Augmentation of vessel squeezing at coronary-myocardial bridge by nitroglycerin: study by quantitative coronary angiography and intravascular ultrasound. Am Heart J. 1999;138:345-350. (2 Pt 1):
- [Google Scholar]
- CT fractional flow reserve for the diagnosis of myocardial bridging-related ischemia: a study using dynamic CT myocardial perfusion imaging as a reference standard. Korean J Radiol. 2021;22(12):1964-1973.
- [Google Scholar]
- Dynamic myocardial CT perfusion imaging for evaluation of myocardial ischemia as determined by MR imaging. JACC Cardiovasc Imaging. 2014;7(03):267-277.
- [Google Scholar]
- Functional versus anatomic assessment of myocardial bridging by intravascular ultrasound: impact of arterial compression on proximal atherosclerotic plaque. J Am Heart Assoc. 2016;5(04):e001735.
- [Google Scholar]
- Optical coherence tomography and intravascular ultrasound assessment of the anatomic size and wall thickness of a muscle bridge segment. Catheter Cardiovasc Interv. 2019;93:772-778. (S1):
- [Google Scholar]
- Myocardial bridging in absence of coronary artery disease: proposal of a new classification based on clinical-angiographic data and long-term follow-up. Cardiology. 2009;112(01):13-21.
- [Google Scholar]
- Importance of diastolic fractional flow reserve and dobutamine challenge in physiologic assessment of myocardial bridging. J Am Coll Cardiol. 2003;42(02):226-233.
- [Google Scholar]
- Functional assessment of myocardial bridging with conventional and diastolic fractional flow reserve: vasodilator versus inotropic provocation. J Am Heart Assoc. 2021;10(13):e020597.
- [Google Scholar]
- Unmasking myocardial bridge-related ischemia by intracoronary functional evaluation. Circ Cardiovasc Interv. 2018;11(06):e006247.
- [Google Scholar]








