Translate this page into:
NT-proBNP Levels in Relation to Various Grades of Hypertension – An Observational Study
-
Received: ,
Accepted: ,
How to cite this article: Remala A, Karthikeya K. NT-proBNP levels in relation to various grades of hypertension – An observational study. Indian J Cardiovasc Dis Women 2023;8:5-10.
Abstract
Objectives:
The objectives of this study were to compare levels of NT-proBNP in various grades of hypertension, correlate with electrocardiographic criteria of LVH and with diastolic function on echocardiography.
Materials and Methods:
This study was conducted on 100 patients attending the cardiology outpatient department of Nizam’s Institute of Medical Sciences, patients satisfying the inclusion criteria were enrolled in this study after taking informed consent.
Results:
This study includes the patient population with a mean of 54.32 ± 6 years of age. ECG criteria of LVH are more common in patients with Grade 1 (60%) and Grade 2 (89%) hypertension.
Conclusion:
Patients with higher grades of hypertension have more LV mass which is corresponding to ECG criteria satisfying LVH and more diastolic dysfunction as well as higher NT pro-BNP values.
Keywords
Hypertension
Left ventricular hypertrophy
NT- pro BNP
ABSTRACT IMAGE

INTRODUCTION
Hypertension is one of the most frequent cause of hospital visit and chronic prescription of medications. Blood pressure is inadequately controlled in roughly one half of individuals with hypertension.
A major predictor of cardiovascular events in high blood pressure is an increase in the left ventricular thickness (LVH) and its detection is critical as an indirect marker of cardiac damage.[1] The LVH detection in clinical practice has various limitations. Most guidelines recommend the use of ECG but have poor sensitivity, though echocardiography is widely used, it is time consuming and costly. Cardiac biomarkers can be used for risk stratification.
An increase in blood volume and pressure overload and cardiac remodeling, such as left ventricular hypertrophy and systolic/diastolic dysfunction, leads to the secretion of natriuretic peptides by cardiomyocytes. The levels of N terminal pro-brain natriuretic peptide (NTproBNP) are related to LV geometry and mass.[2] In the late stages of cardiac diseases such as heart failure or coronary artery disease, the strong prognostic markers are BNP and NT-proBNP. Recently, it was proved that there is a good correlation between plasma levels of NT-proBNP for the diagnosis of LVH.[3] However, only limited data are available regarding natriuretic peptides as the prognostic marker of hypertension. The prompt wide use of NT-proBNP for risk stratification in hypertension is recommended due to its ease of measurement, low cost, and widespread availability of test kits.
These promising features prompted us to test the association between NT-proBNP levels in hypertensives with various grades of the left ventricular hypertrophy, consecutively referred to our center.
Olsen et al.,[4,5] in a substudy on Losartan Intervention for Endpoint reduction, proved that NT-proBNP had a significant prognostic value in high blood pressure that is subjects with severe hypertension with severe eccentric LVH had higher NT-proBNP levels. In a group of hypertensives from the common population, Pedersen et al.[6] confirmed this finding after adjustment for traditional risk factors.
The aim is to study the trends of NT-proBNP levels in different stages of hypertension.
Objectives
The objectives of this study were as follows:
To compare levels of NT-proBNP in various grades of hypertension.
To detect differences in levels of NT-proBNP across systolic, diastolic, and pulse pressure categories.
To compare levels of NT-proBNP with electrocardiographic criteria of LVH.
To compare levels of NT-proBNP with diastolic function on echocardiography.
MATERIALS AND METHODS
This study was conducted on 100 patients attending the cardiology outpatient department of Nizam’s Institute of Medical Sciences, patients satisfying the inclusion criteria of age >18 years, patients with essential hypertension with normal biventricular systolic function were enrolled in this study after taking informed consent, and patients with secondary hypertension, acute coronary syndrome, and significant coronary artery disease, patients with systolic dysfunction EF <50%, and patients with decompensated heart failure, established systolic, and diastolic heart failure. Conditions associated with elevated levels of NT-proBNP other than cardiac conditions such as acute and chronic renal failure, pulmonary diseases such as pulmonary hypertension, COPD, pneumonia, ARDS, and sepsis and conditions associated with low levels of NT-proBNP – obesity and pericardial constriction were excluded from this study.
METHODOLOGY
The patient’s vital data were noted and the study group was divided into three groups based on blood pressure values. Blood pressure was measured in the sitting position in the left upper limb. Subjects were stratified according to ACC/AHA 2017 guidelines as high normal blood pressure (SBP 120–129 and DBP <80 mmHg), Grade 1 hypertension (SBP 130–139 or DBP 80–89 mmHg), and Grade 2 hypertension (SBP 140 or >, DBP 90 or >) and was followed up for three months with no change in medications used. Along with NT pro-BNP, routine biochemical analysis was also done. A cardiac evaluation was done with electrocardiography and echocardiography.[2] Samples of NT-proBNP values taken 15 days apart were collected and compared among three groups of patients, along with their ECG and ECHO to diagnose the degree of the left ventricular hypertrophy and diastolic dysfunction.
ECG criteria, the Sokolow-Lyon index (SV1 + RV5 or V6) cutoff >35 mm, and Cornell voltage criteria [R-wave amplitude in lead aVL (RaVL) ≥11 mm] were considered as a criterion for diagnosing LVH.
Echocardiography was done in Philips iE33 machine to assess systolic LV function and grading of diastolic dysfunction of these patients was done based on mitral flow velocities and tissue Doppler velocity into GRADE I (mild diastolic dysfunction or impaired relaxation phase: E/A <0.8, DT >200 milliseconds, and E/e’ ≤8), Grade II (moderate diastolic dysfunction or pseudonormal phase: E/A 0.8–1.5, DT 160–200 milliseconds, and E/e’9–12), and Grade III (severe diastolic dysfunction or restrictive filling phase E/A ≥2, DT <160 milliseconds, and E/e’ ≥13).
Patients were stratified according to NT-proBNP levels into three groups, they are Group 1 (< 60 pg/ml), Group 2 (61–130 pg/ml), and Group 3 (> 130 pg/m) based on the average of 2 NT-proBNP values obtained.
Statistical data analysis
Data were collected and compiled using Microsoft Excel and statistical analysis was done using SSPS v28.0. Continuous variables are presented as mean and standard deviation whereas categorical variables as percentages. To find out the significance of study parameters on a categorical scale between three groups, Chi-square test was used. An independent t-test has been used for the analysis of continuous variables for normal distribution. All p values were two tailed and P < 0.05 will be considered statistically significant.
RESULTS
Three groups of NT-proBNP based on the following values: Group 1 <60 pg/mL; Group 2 - 61–130 pg/mL; and Group 3 >131 pg/ml were analyzed. This study includes the patient population with a mean of 54.32 ± 6 years of age among which 46% are female and 54% are male, as shown in [Figure 1].

- Sex * NT-proBNP groups.
Among patients in Group 1, 42.4% had high normal blood pressure, 54.5% had Grade 1, and 3% had Grade 2 hypertension. Among patients in Group 2, 17% had high normal BP, 37.7% had Grade 1, and 45.3% had Grade 2 hypertension. Among patients of Group 3, none had high normal BP, 14.3% had Grade 1 hypertension, and 85.7% had Grade 2 hypertension with P = 0.001, as shown in [Figures 2 and 3].
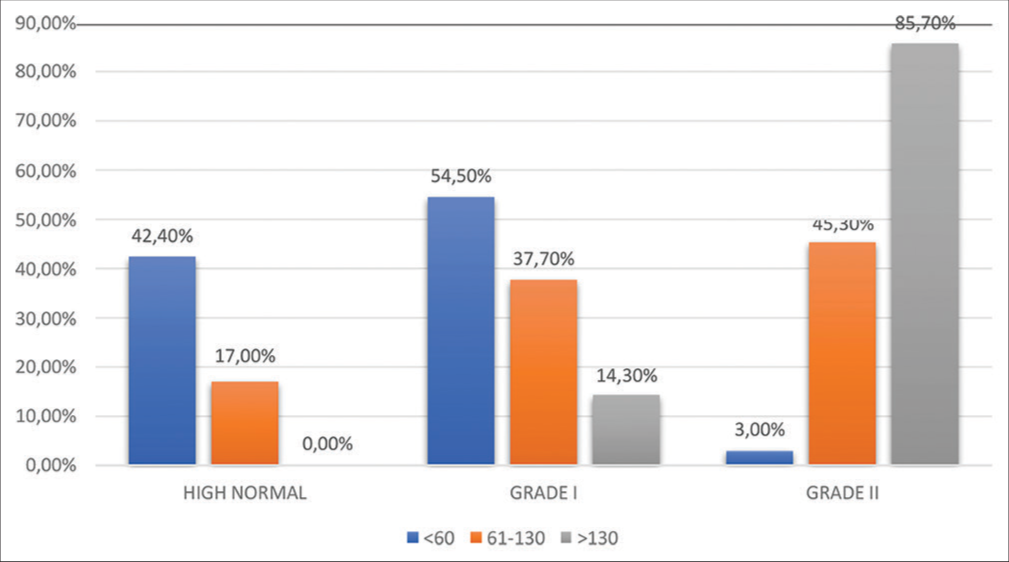
- SBP group * NT-proBNP groups. Chi-square = 33.850, P = 0.001 (s).
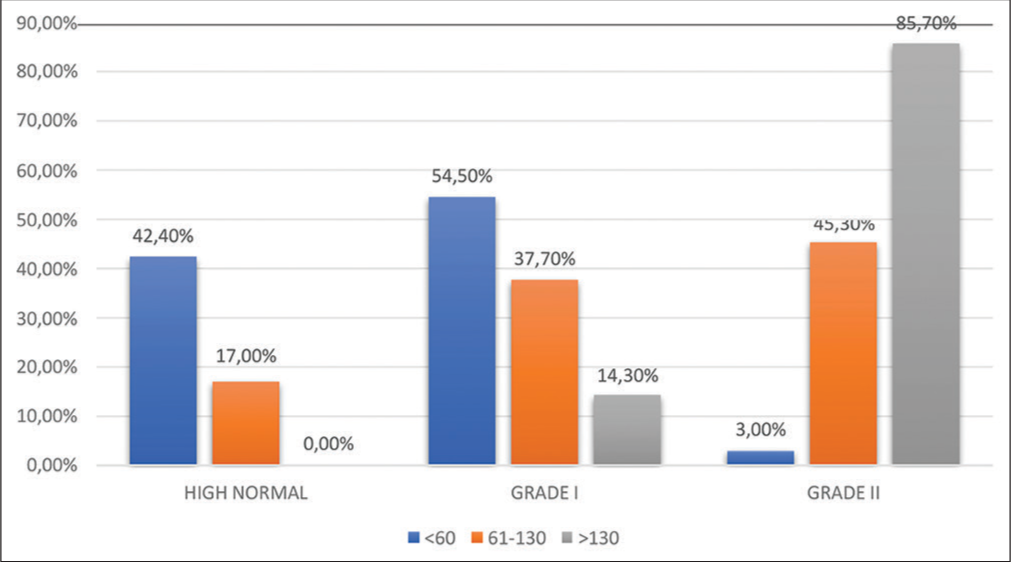
- DBP group * NT-proBNP groups. Chi-square = 33.850, P = 0.001 (s).
ECG criteria of LVH are present in 36.4% and absent in 63.6% of patients of Group 1; present in 81.1% and absent 18.9% of patients of Group 2; and present in 85.7% and absent in 14.3% of patients in Group 3 with P = 0.001, as shown in [Table 1]. ECG criteria of LVH are more common in patients with Grade 1 (60%) and Grade 2 (89%) hypertension, as shown in [Tables 2-4].
| NT-proBNP groups | Total | |||
|---|---|---|---|---|
| <60 | 61–130 | >130 | ||
| ECHO | ||||
| GI | ||||
| Count | 31 | 14 | 0 | 45 |
| % | 93.9% | 26.4% | 0.0% | 45.0% |
| GII | ||||
| Count | 2 | 39 | 7 | 48 |
| % | 6.1% | 73.6% | 50.0% | 48.0% |
| GIII | ||||
| Count | 0 | 0 | 7 | 7 |
| % | 0.0% | 0.0% | 50.0% | 7.0% |
| Total | ||||
| Count | 33 | 53 | 14 | 100 |
| % | 100.0% | 100.0% | 100.0% | 100.0% |
Chi-square=90.264, P=0.001 (S)
| NT-proBNP groups | Total | |||
|---|---|---|---|---|
| <60 | 61–130 | >130 | ||
| LVH ECG criteria | ||||
| Absent | ||||
| Count | 21 | 10 | 2 | 33 |
| % | 63.6% | 18.9% | 14.3% | 33.0% |
| Present | ||||
| Count | 12 | 43 | 12 | 67 |
| % | 36.4% | 81.1% | 85.7% | 67.0% |
| Total | ||||
| Count | 33 | 53 | 14 | 100 |
| % | 100.0% | 100.0% | 100.0% | 100.0% |
Chi-square=21.014, P=0.001 (S)
| SBP group | Total | |||
|---|---|---|---|---|
| High normal | Grade I | Grade II | ||
| LVH ECG criteria | ||||
| Absent | ||||
| Count | 13 | 16 | 4 | 33 |
| % | 56.5% | 40.0% | 10.8% | 33.0% |
| Present | ||||
| Count | 10 | 24 | 33 | 67 |
| % | 43.5% | 60.0% | 89.2% | 67.0% |
| Total | ||||
| Count | 23 | 40 | 37 | 100 |
| % | 100.0% | 100.0% | 100.0% | 100.0% |
Chi-square=14.881, P=0.001 (S)
| DBP group | Total | |||
|---|---|---|---|---|
| High normal | Grade I | Grade II | ||
| LVH ECG criteria | ||||
| Absent | ||||
| Count | 13 | 16 | 4 | 33 |
| % | 56.5% | 40.0% | 10.8% | 33.0% |
| Present | ||||
| Count | 10 | 24 | 33 | 67 |
| % | 43.5% | 60.0% | 89.2% | 67.0% |
| Total | ||||
| Count | 23 | 40 | 37 | 100 |
| % | 100.0% | 100.0% | 100.0% | 100.0% |
Chi-square=14.881, P=0.001 (S).
Among patients of Group 1, 93.9% had Grade I diastolic dysfunction, 6.1% had Grade II diastolic dysfunction, and none had Grade III hypertension. Among patients in Group II, 26.4% had Grade I hypertension, 73.6% had Grade II hypertension, and none had Grade III hypertension. Among Group 3, 50% had Grade II, 50% had Grade III hypertension, and none had grade I hypertension, as shown in [Table 1]. Grade 1 diastolic dysfunction is seen in most of the patients with high normal blood pressure (69.6%) and Grade 2 diastolic dysfunction is seen in most of the patients of Grade 2 (55%) and three hypertension groups (51.4%) with P = 0.008, as shown in [Tables 5 and 6].
| Diastolic dysfunction grades | SBP group | Total | ||
|---|---|---|---|---|
| High normal | Grade I | Grade II | ||
| ECHO | ||||
| GI | ||||
| Count | 16 | 17 | 12 | 45 |
| % | 69.6% | 42.5% | 32.4% | 45.0% |
| GII | ||||
| Count | 7 | 22 | 19 | 48 |
| % | 30.4% | 55.0% | 51.4% | 48.0% |
| GIII | ||||
| Count | 0 | 1 | 6 | 7 |
| % | 0.0% | 2.5% | 16.2% | 7.0% |
| Total | ||||
| Count | 23 | 40 | 37 | 100 |
| % | 100.0% | 100.0% | 100.0% | 100.0% |
Chi-square=13.669, P=0.008 (S)
| DBP group | Total | |||
|---|---|---|---|---|
| High normal | Grade I | Grade II | ||
| ECHO | ||||
| GI | ||||
| Count | 16 | 17 | 12 | 45 |
| % | 69.6% | 42.5% | 32.4% | 45.0% |
| GII | ||||
| Count | 7 | 22 | 19 | 48 |
| % | 30.4% | 55.0% | 51.4% | 48.0% |
| GIII | ||||
| Count | 0 | 1 | 6 | 7 |
| % | 0.0% | 2.5% | 16.2% | 7.0% |
| Total | ||||
| Count | 23 | 40 | 37 | 100 |
| % | 100.0% | 100.0% | 100.0% | 100.0% |
Chi-square=13.669, P=0.008 (S)
DISCUSSION
In our study, it was found that patients with higher grades of hypertension had more prevalence of ECG criteria satisfying for LVH, higher grades of diastolic dysfunction, and higher NT-proBNP values indicating left ventricular hypertrophy. According to the current guidelines, the LVH is useful for risk estimation, by several indexes the first-step relies on ECG, which allows for estimating the presence of this condition. Natriuretic peptides can spot LVH in hypertension and turn, the LVH is helpful for prognostication in patients with hypertension.
In consideration of age-matched normotensive control subjects, the mean plasma ANP and BNP levels were higher in all essential hypertensive patients. Plasma ANP levels were higher than in hypertensive patients with eccentric hypertrophy, and concentric hypertrophy when compared to normotensive control subjects. Normotensive subjects and hypertensive patients with normal geometry have the same ANP levels. Plasma BNP levels are higher in the high blood pressure group of patients with normal geometry, concentric remodeling, and eccentric hypertrophy than in normotensive control subjects although these differences were not significant; BNP levels and BNP/ANP ratio were high in concentric LV hypertrophy. ANP levels have a notable association with LV mass index, cardiac wall thickness, ventricular septal thickness, and mean arterial pressure. Plasma BNP levels has significant association with cardiac wall thickness, ventricular septal thickness, and left ventricular mass index but not with mean arterial pressure. Plasma ANP and BNP levels are elevated in the primary hypertensive patients with the left ventricular hypertrophy. In addition, BNP secretion is increased in concentric hypertrophy. Thus, plasma ANP and BNP levels quantification are practical for the discernment of concentric left ventricular hypertrophy in individuals with essential hypertension.[2]
Pedersen et al.[6] reported that NT-proBNP predicts the risk of a composite endpoint of death, stroke/transient ischemic attack, and myocardial infarction in individuals of hypertensives from an urban area of Copenhagen. However, the small group of the study has not given a correct conclusion.
A study on N-terminal pro-brain natriuretic peptide-A powerful predictor of mortality in hypertension[7] adds several keynotes of information: (1) This study substantiates that plasma NT-proBNP has the prognostic value in terms of all-cause mortality in a large sample of hypertensive patients; (2) it supports that plasma NT-proBNP has the prognostic value of in estimating death which is independent of a large series of traditional risk factors, such as ambulatory BP or kidney function; (3) it showed that this prognostic value is independent of and superior to, two ECG indexes of LVH; and (4) this study reveals that plasma NT-proBNP has its prognostic significance after excluding of population with LVH by ECG criteria, highlighting the role of this marker in the very complex task of improving risk stratification in patients with low risk (i.e., with “normal ECG”). Plasma NTproBNP and BNP levels are more in the high blood pressure group than in normotensive patients;[8,9] they are increased with LVH.[9,10] Due to longer t1/2, less intrapersonal variation, and potentiality to identify minor preclinical cardiac changes,[11] normally, NT-proBNP has prognostic value after excluding patients with LVH in ECG. Plasma NT-proBNP level of 133 pg/mL (the highest tertile) is correlated with a 3-fold rise in the risk of mortality in correlation with having levels of 50.8 pg/mL, even after modification for confounders. In fact, in people free of heart failure, McKie et al.[12] revealed that the threshold at 109 pg/mL was of prognostic value for mortality, a value similar to that described by Rutten et al.[13] in the Rotterdam study. More specifically, in hypertension, Olsen et al.[4] demonstrated in the Losartan Intervention for Endpoint reduction substudy, the prognostic value of a 170 pg/mL cutoff chosen as the median value of this high-risk population.
Natriuretic peptides estimate the frequency of atrial fibrillation as they are related to LV mass, LV dysfunction,[11] diastolic filling pressure,[14] and myocardial ischemia.[15] Blood pressure and degree of aortic stiffness[16] also dictate the level of natriuretic peptides. There indicates that natriuretic peptides have a good relationship with the risks of future heart failure,[16] ischemic events,[13] and stroke.[13] Natriuretic peptides have an emerging role in being able to predict outcomes beyond cardiac events.
CONCLUSION
Patients with higher grades of hypertension have more LV mass which is corresponding to have ECG criteria satisfying LVH and more diastolic dysfunction as well as have higher NT pro-BNP values.
Limitations
The major limitation of our study is the compact group of population and also the small duration of the study period. Lack of ambulatory blood pressure monitoring in the population included in our study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Audio summary available at
Financial support and sponsorship
Nil.
References
- Prognostic implications of echocardiographically determined left ventricular mass in the Framingham heart study. N Engl J Med. 1990;322:1561-6.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between left ventricular geometry and natriuretic peptide levels in essential hypertension. Hypertension. 1996;28:22-30.
- [CrossRef] [PubMed] [Google Scholar]
- N-terminal pro-brain natriuretic peptide: A promising biomarker for the diagnosis of left ventricular hypertrophy in hypertensive women. Arch Cardiovasc Dis. 2008;101:307-15.
- [CrossRef] [PubMed] [Google Scholar]
- N-terminal brain natriuretic peptide predicted cardiovascular events stronger than high sensitivity C-reactive protein in hypertension: A LIFE substudy. J Hypertens. 2006;24:1531-9.
- [CrossRef] [PubMed] [Google Scholar]
- N-terminal pro-brain natriuretic peptide predicts cardiovascular events in patients with hypertension and left ventricular hypertrophy: A LIFE study. J Hypertens. 2004;22:1597-604.
- [CrossRef] [PubMed] [Google Scholar]
- N-terminal pro-brain natriuretic peptide in arterial hypertension: A valuable prognostic marker of cardiovascular events. J Card Fail. 2005;11:S70-5.
- [CrossRef] [PubMed] [Google Scholar]
- N-terminal pro-brain natriuretic peptide: A powerful predictor of mortality in hypertension. Hypertension. 2021;57:702-9.
- [CrossRef] [PubMed] [Google Scholar]
- Brain natriuretic peptide as a cardiac hormone in essential hypertension. Am J Med. 1992;92:29-34.
- [CrossRef] [PubMed] [Google Scholar]
- Lack of activation of molecular forms of the BNP system in human grade 1 hypertension and relationship to cardiac hypertrophy. Am J Physiol Heart Circ Physiol. 2006;291:H1529-35.
- [CrossRef] [PubMed] [Google Scholar]
- Superiority of brain natriuretic peptide as a hormonal marker of ventricular systolic and diastolic dysfunction and ventricular hypertrophy. Hypertension. 1996;28:988-94.
- [CrossRef] [PubMed] [Google Scholar]
- Head-to-head comparison of the diagnostic utility of BNP and NTproBNP in symptomatic and asymptomatic structural heart disease. Clin Chim Acta. 2004;341:41-8.
- [CrossRef] [PubMed] [Google Scholar]
- Amino-terminal pro-B-Type natriuretic peptide and B-Type natriuretic peptide: Biomarkers for mortality in a large community-based cohort free of heart failure. Hypertension. 2006;47:874-80.
- [CrossRef] [PubMed] [Google Scholar]
- Amino-terminal proB-Type natriuretic peptide improves cardiovascular and cerebrovascular risk prediction in the population: The Rotterdam study. Hypertension. 2010;55:785-91.
- [CrossRef] [PubMed] [Google Scholar]
- The role of NT-proBNP in the diagnostics of isolated diastolic dysfunction: Correlation with echocardiographic and invasive measurements. Eur Heart J. 2005;26:2277-84.
- [CrossRef] [PubMed] [Google Scholar]
- B-Type natriuretic peptide and ischemia in patients with stable coronary disease: Data from the heart and soul study. Circulation. 2003;108:2987-92.
- [CrossRef] [PubMed] [Google Scholar]
- Plasma natriuretic peptide levels and the risk of cardiovascular events and death. N Engl J Med. 2004;350:655-63.
- [CrossRef] [PubMed] [Google Scholar]







