Translate this page into:
New Indices to Detect Acute Kidney Injury in Coronary Artery Disease Patients
*Corresponding author: Abdul Samad Shaik, MD, Department of Cardiology, Nizam Institute of Medical Sciences, Hyderabad, Telangana, India. aminaazeem99@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shaik AS, Lakshmi VS. New Indices to Detect Acute Kidney Injury in Coronary Artery Disease Patients. Indian J Cardiovasc Dis Women. 2024;9:10-4. doi: 10.25259/IJCDW_15_2023
Abstract
Objectives:
Pre-procedure liver impairment has been revealed as a poor prognostic factor post-percutaneous coronary intervention (PCI). Recent investigations discovered that the aspartate aminotransferase-to-alanine aminotransferase ratio (De-Ritis ratio) indicates the severity of liver impairment and was related to adverse outcomes. We aimed to evaluate the predictive value of the De-Ritis ratio for contrast-associated acute kidney injury (CA-AKI).
Materials and Methods:
We prospectively enrolled 150 patients undergoing elective PCI between June 2022 and August 2022. Contrast-induced AKI: It is defined as an acute decline in renal function, defined as an increase in creatinine of ≥0.5 mg/dL or ≥25% compared to baseline. It usually develops 24–72 h post administration of an IV contrast agent in the absence of other identifiable causes.
Results:
The incidence of CA-AKI was 8% (n = 12). The De-Ritis ratio >1.30 was identified as the best cutoff value for CA-AKI prediction.
Conclusion:
The De-Ritis ratio was an independent risk factor for CA-AKI in patients undergoing elective PCI.
Keywords
Coronary artery disease
Coronary angiography
Contrast-induced acute kidney injury
De-Ritis ratio
Aspartate transaminase/alanine aminotransferase ratio
ABSTRACT IMAGE

INTRODUCTION
Contrast-associated acute kidney injury (CA-AKI) is attributed to the contrast agents administrated at the time of diagnostic or therapeutic coronary interventions.[1] It is one of the leading causes of acute kidney injury. It contributes to prolonged duration of hospital stay, the requirement of hemodialysis, and increased in-hospital mortality and morbidity. Hence, early identification and development of predictive scores can aid in reducing post-procedure renal injury.[2,3] Patients with ischemic heart disease and liver insufficiency are at risk of perioperative complications.[4] Among themselves, patients undergoing percutaneous coronary intervention (PCI) are at risk of AKI and associated with a poor prognosis. Hence, pre-operative liver function assessment and risk stratification are important to prevent such procedural complications.[5,6]
MATERIALS AND METHODS
It is a prospective study conducted at Nizam’s Institute of Medical Sciences, Hyderabad. The study aimed to assess the prognostic capacity of the De-Ritis ratio in anticipating the development of CA-AKI who underwent PCI. One hundred and fifty cases were enrolled who underwent elective PCI between June 2022 and August 2022. The study included patients with coronary artery disease who underwent elective PCI and had aspartate transaminase (AST) and alanine aminotransferase (ALT) values below 200 mg/dL and patients unwilling to give consent were excluded from study. The following patients were excluded: Patients who had end-stage renal disease or dialysis-dependent, received contrast 1 week prior or 8 h post-procedure, had a history of concurrent administration of any nephrotoxic drug 1 week before or 48 h after the procedure, or those who succumbed within 24 h of admission.
Contrast-induced AKI: This is the acute reduction in renal function, described as an elevation in serum creatinine of ≥0.5 mg/dL or ≥25% compared to baseline. It usually develops 24–72 h post-administration of an IV contrast agent in the absence of other identifiable causes. Data were collected including demographic, clinical, laboratory, and angiographic details. Biochemical parameters such as lipid profile, fasting blood sugars, alanine aminotransferase, aspartate aminotransferase, bilirubin, international normalized ratio, uric acid, and the cue were collected on admission. Serum creatinine measurements were taken on admission and continued for 2 consecutive days. A team of expert interventional cardiologists conducted the procedures. The investigator played no part in determining the approach and technique used for revascularization. PCI was done using IOHEXOL which is a non-ionic contrast of osmolality 780 mOsm/kg. The X-ray contrast medium used is a monomeric tri-iodinated, water-soluble substance with a concentration of 350 mg iodine per milliliter (mL). Each injection typically has a volume ranging from 4 mL to 8 mL. Subsequently, patients received intravenous normal saline at a rate of 1 mL/kg/h for 12 h during the periprocedural period. However, in the case of heart failure patients, the rate was adjusted to 0.5 mL/kg/h.
Statistical analysis
Categorical factors such as sex and comorbidities are presented using frequencies and percentages. On the other hand, continuous parameters such as age, creatinine, hemoglobin, AST, ALT, AST/ALT ratio, total cholesterol, triglyceride (TG), low-density lipoprotein (LDL), high-density lipoprotein, and ejection fraction are presented using means and standard deviations. To compare the mean difference between AST/ALT ratios ≤1.3 and ratios >1.3, a t-test for independent samples was employed.
Qualitative factors and their association with AST/ALT were analyzed using the Chi-square test. Sensitivity analysis was performed using an AST/ALT ratio of 1.3 as a cutoff to predict CA-AKI. Data was entered into MS Excel and analyzed with SPSS 19.0. P < 0.05 was considered significant.
RESULTS
A total of 150 patients were enrolled in the study. Table 1 displays the baseline characteristics of the study population. The average age of the patients was 51.9 ± 9.2 years, with 105 (70%) being male and 45 (30%) being female. Based on the De-Ritis ratio, the patients were categorized into two groups: those with a ratio ≤1.30 (low) and those with a ratio >1.30 (high). Among the study population, 13 (8.6%) patients had a high ratio, while 137 (91.3%) had a low ratio.
| PARAMETERS | AST/ALT<1.3 | AST/ALT>1.3 |
|---|---|---|
| Age | 59±9.2 | 59.9±9.6 |
| Baseline creatinine | 0.99±0.30 | 1.02±0.28 |
| Hb | 12.1±1.7 | 12.6±1.98 |
| Total Cholesterol | 181.8±30.0 | 176.6±36.4 |
| HDL | 38.9±8.6 | 37.0±11.2 |
| LDL | 110±27.9 | 104.1±33.1 |
| TG | 161.28±36.01 | 177.7±39.1 |
| EF | 43.5±10.1 | 40.3±9.04 |
AST: Aspartate transaminase, ALT: Alanine aminotransferase, Hb: Hemoglobin, HDL: High density lipoprotein, LDL: Low density lipoprotein, TG: Triglycerides, EF: Ejection fraction
The high-ratio group exhibited elevated AST, TGs, and LDL-cholesterol in contrast to the low-ratio group.
Out of total 150 patients, 12 (8%) developed CA-AKI. Within this group, 10 (76.9%) patients were part of the high De-Ritis ratio group [Table 2], indicating a significantly associated among the De-Ritis ratio and the CA-AKI occurrence (P ≤ 0.001), which was significantly higher than the association observed with ALT (P = 0.164) and AST (P = 0.362) alone [Table 3]. The sensitivity and specificity are 83.33% and specificity 97.83%, respectively. The positive predictive value and negative predictive value are 76.92% and 98.54%, respectively. The accuracy of the test is 96.67%
| CA-AKI | AST/ALT | |
|---|---|---|
| ≤1.3 | >1.3 | |
| Yes | 2 (1.5%) | 10 (76.9%) |
| No | 135 (98.5%) | 3 (23.1%) |
De-Ritis ratio: AST/ALT, AST: Aspartate transaminase, ALT: Alanine aminotransferase, CA-AKI: Contrast associated acute kidney injury
| Crosstab | ||||
| Count | ||||
| AST/ALT | Total | |||
| <=1.3 | >1.3 | |||
| CA-AKI | ||||
| Yes | 2 | 10 | 12 | |
| No | 135 | 3 | 138 | |
| Total | 137 | 13 | 150 | |
| AST/ALT | ||||
| <=1.3 | >1.3 | |||
| 1.5% | 76.9% | |||
| 98.5% | 23.1% | |||
| P Value (Chi-Square test) | <0.001 | |||
| Sensitivity | 83.33% | |||
| Specificity | 97.83% | |||
| PPV | 76.92% | |||
| NPV | 98.54% | |||
| Accuracy | 96.67% | |||
AST: Aspartate transaminase, ALT: Alanine aminotransferase, CA- AKI: Contrast associated acute kidney injury, PPV: Positive predictive value, NPV: Negative predictive value
CA-AKI developed in 12 (8%) of the patients. The optimal cutoff value for the De-Ritis ratio in predicting CA-AKI was determined to be 1.3, demonstrating a sensitivity of 83.3% and a specificity of 97.83%.
DISCUSSION
In this research, we investigated the correlation between De-Ritis ratio, and CA-AKI in elective PCI patients [Figure 1 and Table 4]. Our findings revealed that patients who had more De-Ritis ratio had a significantly increased occurrence of CA-AKI. Patients with liver insufficiency who underwent PCI experienced a higher incidence of AKI and were frequently linked to unfavorable clinical outcomes.[7] In their study, Alqahtani et al. reported that patients who had liver cirrhosis and underwent PCI were at a high risk of developing AKI and had a higher in-hospital death rate compared to without cirrhosis.[8,9] Similarly, a larger countrywide database analysis demonstrated a greater incidence rate of intestinal bleeding, AKI, 90-day death rate, and 90-day readmission rate.[10] Hence, conducting a prior assessment of liver function plays a critical role in reducing procedural complications.
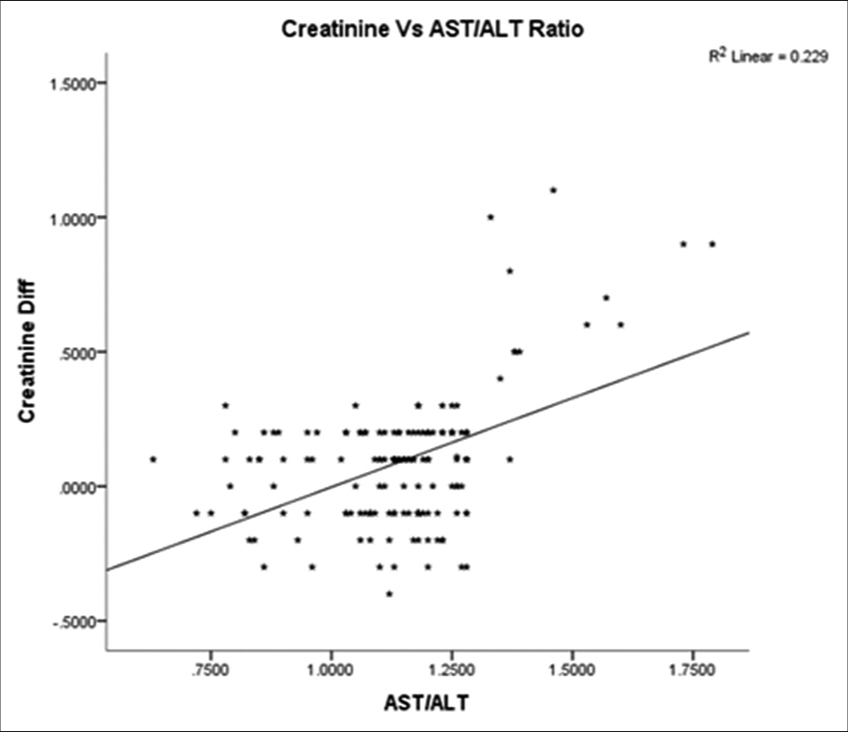
- Correlation between contrast-associated acute kidney injury and De-Ritis ratio. AST: Aspartate transaminase, ALT: Alanine aminotransferase.
| Correlations | |
|---|---|
| AST/ALT | |
| Creatinine Diff | |
| Pearson Correlation | 0.478 |
| Sig. (2-tailed) | 0.000 |
| N | 150 |
AST: Aspartate transaminase, ALT: Alanine aminotransferase, N: Number
AST and ALT are used as markers for liver injury. When combined as the De-Ritis ratio, these levels can indicate liver dysfunction.[11] In addition, the ratio has been confirmed to be associated with adverse outcomes in patients with myocardial infarction,[12] diabetes,[13] and cardiac arrest.[14,15]
In a retrospective study involving 422 patients who undergone hepatectomy, it was observed that a De-Ritis ratio is ≥1.29 served as a standalone risk element for AKI, even after accounting for other potential influencing factors.[16,17] In another longitudinal retrospective study, 6264 patients who undergone surgery related to cardiovascular demonstrated that a high De-Ritis ratio was associated with a significant correlation between mortality and AKI. Likewise, in a previous study, an elevated De-Ritis ratio was identified as a prognosticator for AKI requiring dialysis and early to mid-term mortality after the implantation of a left ventricular assist device.The ratio can be served as a convenient and quick surrogate marker for assessing pre-procedure liver function, and it proves to be valuable in predicting the occurrence of CA-AKI after elective PCI. In cases where the De-Ritis ratio exceeds 1.30, it is crucial to identify the underlying cause of liver dysfunction and initiate appropriate treatment.[18,19]
The exact reason behind the connection between an elevated ratio and CA-AKI remains unknown. As previously cited, elevated levels of the ratio are linked to impaired hepatic function.[11] Moreover, hepatic impairment can result in an imbalance between vasodilatory and vasoconstricting factors, leading to splanchnic and systemic vasodilation and renal vasoconstriction. Ultimately, these mechanisms contribute to renal dysfunction and the development of CA-AKI. Indeed, ALT is exclusively found in the cytoplasm of liver cells, whereas AST is present in both the mitochondria and cytoplasm. It has been postulated that a high ratio might be attributed to mitochondrial impairment, which, in turn, may be a result of oxidative stress.[13] Indeed, oxidative stress and inflammation has been shown to be associated with CA-AKI. Therefore, it is sensible to propose that an elevated De-Ritis ratio is correlated with a higher risk of developing CA-AKI.[20] Therefore, a high De-Ritis ratio could be indicative of impaired renal function, which, in turn, may be associated with an increased risk of CA-AKI.
Limitations
At the outset, we did not carry out dynamic assessments of the De-Ritis ratio during the patient’s hospitalization, and the measurement was performed solely on admission. This limitation may have introduced random errors in the analysis.
Second, our study did not incorporate data concerning other standard risk factors for CA-AKI, such as the prevalence of diabetic kidney disease, congestive cardiac failure, and dehydration.
To strengthen the generalizability and validity of our findings, a multi-center study involving a larger patient population is necessary.
CONCLUSION
The findings of this study demonstrate that the De-Ritis ratio acts as an independent risk factor for the development of CA-AKI in patients undergoing elective PCI. These results provide evidence supporting the potential utility of the DeRitis ratio as a convenient and quick liver function evaluation tool for risk classification. Implementing measures based on the De-Ritis ratio before the procedure could help clinicians mitigate the post-procedural risk of CA-AKI.
Ethical approval
The study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-Assisted technology for manuscript preparation
The authors confirm that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
Audio summary available at
Financial support and sponsorship
Nil.
References
- Predictive Value of Aspartate Aminotransferase-to-Alanine Aminotransferase Ratio for Contrast-Associated Acute Kidney Injury in Patients Undergoing Elective Percutaneous Coronary Intervention. J Cardiol. 2022;79:618-25.
- [CrossRef] [PubMed] [Google Scholar]
- Understanding and Preventing Contrast-Induced Acute Kidney Injury. Nat Rev Nephrol. 2017;13:169-80.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of Contrast-Induced Acute Kidney Injury with Transient or Persistent Renal Dysfunction on Long-Term Outcomes of Patients with Acute Myocardial Infarction Undergoing Percutaneous Coronary Intervention. Heart. 2011;97:1753-7.
- [CrossRef] [PubMed] [Google Scholar]
- Post-Contrast Acute Kidney Injury in a Hospitalized Population: Short- Mid- and Long-Term Out- Come and Risk Factors for Adverse Events. Eur Radiol. 2020;30:3516-27.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology and Prognostic Implications of Contrast-Induced Nephropathy. Am J Cardiol. 2006;98:5K-13K.
- [CrossRef] [PubMed] [Google Scholar]
- Morbidity and Mortality Following Coronary Artery Bypass Graft Surgery in Patients with Cirrhosis: A Population-Based Study. Liver Int. 2009;29:1141-51.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes and Characteristics of Myocardial Infarction in Patients with Cirrhosis. J Invasive Cardiol. 2019;31:E162-9.
- [Google Scholar]
- Nationwide Cohort Study of Outcomes of Acute Myocardial Infarction in Patients with Liver Cirrhosis: A Nationwide Cohort Study. Medicine (Baltimore). 2020;99:e19575.
- [CrossRef] [PubMed] [Google Scholar]
- Temporal Trends in the Utilization and Outcomes of Percutaneous Coronary Interventions in Patients with Liver Cirrhosis. Catheter Cardiovasc Interv. 2020;96:802-10.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of Cirrhosis on 90-Day Outcomes After Percutaneous Coronary Intervention (from A Nationwide Database) Am J Cardiol. 2020;125:1295-304.
- [CrossRef] [PubMed] [Google Scholar]
- Progressive Liver Functional Impairment is Associated with an Increase in AST/ALT Ratio. Dig Dis Sci. 1999;44:1249-53.
- [CrossRef] [PubMed] [Google Scholar]
- De-Ritis Ratio Improves Long-Term Risk Prediction After Acute Myocardial Infarction. J Clin Med. 2018;7:474.
- [CrossRef] [PubMed] [Google Scholar]
- The Aspartate Aminotransferase-to-Alanine Aminotransferase Ratio Predicts all-cause and Cardiovascular Mortality in Patients with Type 2 Diabetes. Medicine (Baltimore). 2016;95:e4821.
- [CrossRef] [PubMed] [Google Scholar]
- De-Ritis Ratio is Associated with Mortality after Cardiac Arrest. Dis Markers. 2020;2020:8826318.
- [CrossRef] [PubMed] [Google Scholar]
- Relation of Aspartate Aminotransferase to Alanine Aminotransferase Ratio to Nutritional Status and Prognosis in Patients with Acute Heart Failure. Am J Cardiol. 2021;139:64-70.
- [CrossRef] [PubMed] [Google Scholar]
- K/DOQI Clinical Practice Guidelines for Chronic Kidney Disease: Evaluation, Classification, and Stratification. Am J Kidney Dis. 2002;39:S1-266.
- [Google Scholar]
- Prognostic Significance of End-Stage Liver Diseases, Respiratory Tract Infection, and Chronic Kidney Diseases in Symptomatic Acute Hepatitis E. Front Cell Infect Microbiol. 2020;10:593674.
- [CrossRef] [PubMed] [Google Scholar]
- Hepatic Dysfunction in Ambulatory Patients with Heart Failure: Application of the MELD Scoring System for Outcome Prediction. J Am Coll Cardiol. 2013;61:2253-61.
- [Google Scholar]
- A Model to Predict Poor Survival in Patients Undergoing Transjugular Intrahepatic Portosystemic Shunts. Hepatology. 2000;31:864-71.
- [CrossRef] [PubMed] [Google Scholar]
- Model for End-Stage Liver Disease Score Predicts the Mortality of Patients with Coronary Heart Disease who Underwent Percutaneous Coronary Intervention. Cardiol Res Pract. 2021;2021:6401092.
- [CrossRef] [PubMed] [Google Scholar]







