Translate this page into:
Need of the Hour— COVID-19 for Cardiologists
Jyotsna Maddury., MD, DM, FACC, FESC, FICC Department of Cardiology, Nizam’s Institute of Medical Sciences Hyderabad, Telangana India janaswamyjyotsna@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
The most distressing pandemic at present is coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).1 Even though COVID-19 predominantly affects the lungs by causing acute respiratory distress syndrome, the heart is not completely spared. People with underlying heart disease are at risk. The main aim of this article is to summarize the available evidence of cardiac involvement in COVID-19 patients and outlay precautions to patients with underlying cardiovascular disease (CVD).
People with the cardiopulmonary disease are at higher risk. As the virus survives in low temperatures, nose and sinuses are the main sources of infection. This virus could affect the heart, especially a diseased heart. Although information about COVID-19 is changing on an hourly basis, information of the previous severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS)–producing coronaviruses offers insight.2 They were linked to cardiac disease as they produced inflammation of the heart muscle, myocardial infarction, and rapid-onset heart failure.
Most of the published information on COVID-19 is from China. Three important publications in New England Journal of Medicine, Lancet, and Allergy are based on the cases from China.3 4 5 Even though the initial study published in Lancet showed male preponderance (70% males), in a short duration another publication in Allergy showed a 1:1 ratio of male (50.7%) and female involvement. Initial studies showed low association of chronic cardiac diseases (10%) in COVID-19 patients along with the acute cardiac injury accounting to 23%. Acute cardiac injury was diagnosed when hypersensitive cardiac troponin I was > 28 pg/mL. Recent studies have showed increased association of CVD, up to 40%, in COVID-19 patients. But more recent studies have showed increased association of CVD, up to 40%, in COVID-19 patients. Fifty percent of COVID-19 patients had comorbidities, most common was hypertension (in 30%), diabetes (in 19%), and coronary artery disease (in 8%). This high proportion of CVD was the cause for high mortality in patients with COVID-19. COVID-19 in patients with compensated heart failure may precipitate heart failure.6 In COVID-19 patients cardiovascular disorders including arrythmias may occur due to drug therapy for the diseases, especially the antiviral drugs or drug interactions. So, these patients also require close monitoring.
Even though the comorbid conditions association with COVID-19 was high, acute myocardial infarction was reported only in one young female who had normal coronaries on angiogram. These reports with new information urge cardiologists to warn patients about the potential risk and encourage them to practice “additional, reasonable precautions” for those with underlying heart disease.
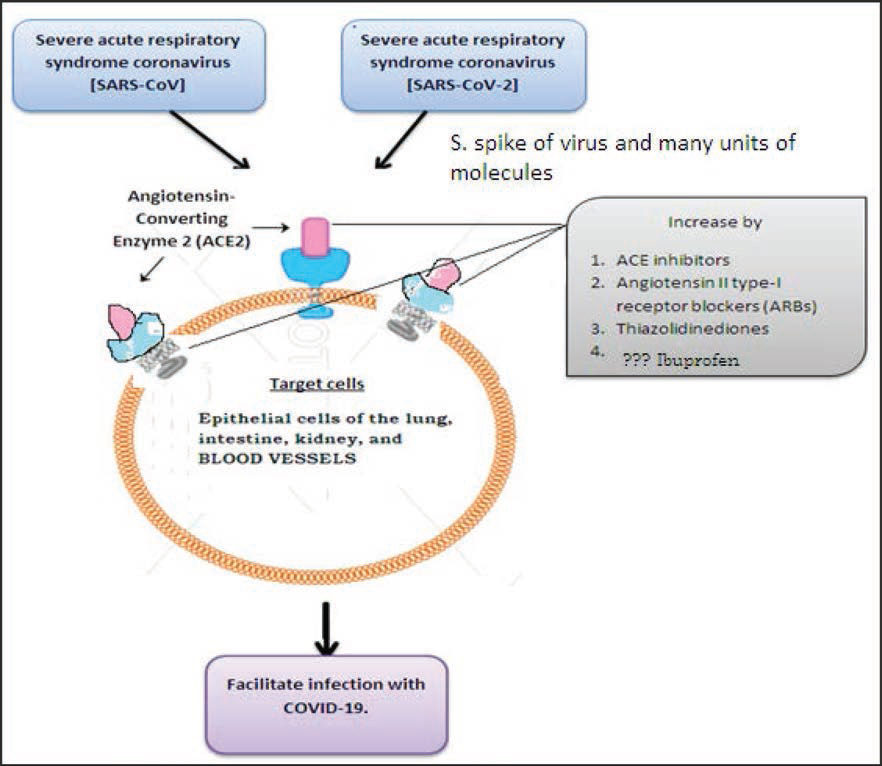
The mechanism of increased risk for cardiovascular disease patients to COVID-19 is not clear.7 The virus penetrates the cell though the angiotensin-converting enzyme 2 (ACE2) receptor and then multiplies to produce the disease. These receptors are present on epithelial cells of the lung, intestine, kidney, and blood vessels.8 Patients with hypertension and diabetes, who receive angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin receptor blockers (ARBs) have more expression of these ACE2 receptors on the target cells, which may facilitate the entry of the virus (Fig. 1). But a similar effect is not seen with calcium channel blockers.
-
Fig. 1 Role of ACE2 receptors in COVID-19.
Fig. 1 Role of ACE2 receptors in COVID-19.
Previously, acute myocarditis and heart failure was reported with MERS-CoV. As SARS-CoV-2 and MERS-CoV have similar pathogenicity, myocardial injury caused due to SARS-CoV-2 infection may be immune mediated through the ACE2 receptor or cytokine storm and/or hypoxia due to acute respiratory distress syndrome (ARDS).9 Added myocardial damage along with ARDS makes the patient’s prognosis worse and treatment becomes difficult and complex. During the course of progression of COVID-19 disease, due to intense systemic inflammatory response more frequent cardiac involvement occurs.
Deaths from COVID-19 are due to cytokine storm syndrome and fulminant myocarditis. Cytokine storm syndrome culminates as ARDS. Fulminant myocarditis is primarily caused by infection with viruses, with mortality rates as high as 50 to 70%.
Concern about the continuation of ACEIs and ARBs for patients who are already taking them was discussed by different hypertensive societies.10 11 12 13 The European Society of Hypertension and the European Society of Cardiology council on hypertension encourage the use of ACEIs/ARBs due to lack of evidence supporting their role in COVID-19. Even other societies like Hypertension Canada12; Canadian Cardiovascular Society 13; The Renal Association, United Kingdom14; International Society of Hypertension15; American College of Physicians16; Spanish Society of Hypertension17; American Heart Association18; Heart Failure Society of America19; American college of Cardiology20; European Renal Association–European Dialysis and Transplant Association21; American Society of Pediatricnephrology22; and High Blood Pressure Research Council of Australia23 recommend the continued use of ACEs/ARBs. The three United States medical societies16 18 20 advise patients on ACEI or ARB to not stop the current treatment unless advised by their doctors if they contract COVID-19. In addition, European Society of Hypertension and Spanish Society of Hypertension recommend case-by-case changes of the drugs in seriously ill patient.
Other drugs that are used in CAD patients like statins, antiplatelets, and β-blockers were discussed in the webinar jointly released by the American College of Cardiology (ACC) and Chinese cardiology association. They recommend to continue statin but with close monitoring. Antiplaletes and β-blockers are also to be continued. If steroids are required for fulminant myocarditis, the dose should be low to moderate. If a COVID-19 patient comes with ST elevation myocardial infaction (STMI), then thrombolysis should to be considered. If primary percuaneous coronary intervention (PCI) is required then it is better to do it in isolated cath laboratories. If they are not available and mandatory to do then minimum central air circulation in the cath laboratory.
At present we know only about the acute course of the disease. We need to follow these patients for long-term effects. SARS-CoV–infected patients on long-term follow-up of 12 years showed hyperlipidemia (68%), cardiovascular system abnormalities (44%), and glucose metabolism disorders (60%).24 As SARS-CoV 2 also has similar pathogenicity as SARS-CoV, follow-up of these COVID-19 patients for cardiac events and altered metabolic status is required.
With this increasing need for awareness of cardiac diseases in COVID-19, ACC released a clinical bulletin for the cardiac care team.20 Cardiac complications in COVID-19 simulates that of SARS, MERS, and influenza. The cardiologist has to assist other clinical specialties to manage the cases of COVID-19 with cardiac complications. Echocardiography (ECG) should be done in patients with ECG changes and those demonstrating heart failure, arrhythmia, or cardiomegaly. Patients with CVD are at risk of contracting COVID-19 and have a worse prognosis. As there is an increased risk of secondary infections with COVID-19, patients are advised to remain current with vaccinations, including the pneumococcal vaccine and influenza vaccine in accordance with current ACC/ American Heart Association (AHA) guidelines. In patients with heart failure or volume overload conditions, fluid administration should be carefully monitored.
Strategies should include identifying cardiovascular patients with COVID-19 symptoms from other patients, including the outpatients, substituting telephonic or telehealth consultations for in-person reviews of stable CAD patients in order to prevent possible nosocomial COVID-19 infections.21
Care should be taken to avoid underdiagnosis of AMI in the COVID–19 setting.
Based on a small study of 26 patients in France and 16 nonrandomised trials, it is believed that the time taken to resolve viral shedding from COVID-19 patients is decreased by treatment with hydroxychloroquine alone or in combination with Azithromycin.25 With raised concerns about the increased risk of arrhythmic death caused by QT prolongation associated with use of chloroquine, hydroxychloroquine, or azithromycine (alone or in combination), hydroxychloroquine or chloroquine therapy should occur in the context of a clinical trial or registry, until sufficient evidence is available for use in clinical practice.26
Regarding the management of patients with ACS in the setting of COVID-19, SCAI consensus is to preferably take true STEMI patients for primary angioplasty and to avoid diagnostic or therapeutic interventions in NSTEMI ACS patients with low risk features. It is also recommended to avoid endotracheal intubation in the cath lab as much as possible, but if it must be done, it is advised to remove all nonessential personnel from the lab to avoid potential exposure to aerosolized virus. For patients in respiratory distress, intubation before transfer to the cath lab is advised to avoid aerosolization.27
In conclusion, the exact mechanism through which SARS-CoV-2 causes COVID-19 is not known; it may be through the ACE2 receptors and immune mechanism. SARS-CoV-2 infection in patients with underlying CVD have worse prognosis. Cardiovascular protection should be given attention during the treatment for COVID-19.
Conflict of Interest
None declared
References
- Emerging threats from zoonotic coronaviruses—from SARS and MERS to 2019-nCoV. J Microbiol Immunol Infect (20):30011-6. pii; S1684-1182
- [CrossRef] [Google Scholar]
- Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55(03):105924.
- [Google Scholar]
- Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020 (e-pub ahead of print)
- [CrossRef] [Google Scholar]
- Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;S2213-2600(20):30079-5.
- [Google Scholar]
- Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020;00:1-12.
- [Google Scholar]
- Comparison of heart failure and 2019 novel coronavirus pneumonia in chest CT features and clinical characteristics [in Chinese] Zhonghua Xin Xue Guan Bing Za Zhi. 2020;48(00):E007.
- [Google Scholar]
- SARS-CoV-2: a potential novel etiology of fulminant myocarditis. Herz 2020 (e-pub ahead of print)
- [CrossRef] [Google Scholar]
- Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J Virol. 2020;94(07):e00127-e20.
- [Google Scholar]
- A tug-of-war between severe acute respiratory syndrome coronavirus 2 and host antiviral defence: lessons from other pathogenic viruses. Emerg Microbes Infect. 2020;9(01):558-570.
- [Google Scholar]
- Statement by the ESC https://www.escardio.org/Councils/Council-on-Hypertension-(CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-ang. Accessed March 17, 2020
- Bozkurt B, Kovacs R, Harrington B. Position statement of the ESC Council on Hypertension on ACE-Inhibitors and Angiotensin Receptor Blockers. https://www.escardio.org/Councils/Council-on-Hypertension-(CHT)/News/position-statement-of-the-esc-council-on-hypertension-on-ace-inhibitors-and-ang. Accessed March 13, 2020
- Hypertension Canada’s Statement on. Hypertension, ACE-Inhibitors and Angiotensin Receptor Blockers and COVID-19. https://hypertension.ca/wp-content/uploads/2020/03/2020-30-15-Hypertension-Canada-Statement-on-COVID-19-ACEi-ARB.pdf. Accessed March 13, 2020
- Canadian Cardiovascular Society. Important information related to COVID-19. https://www.ccs.ca/en. Accessed March 13, 2020
- The Renal Association. United Kingdom. COVID-19: information and guidance for renal professionals. https://renal.org/covid-19. Accessed March 15, 2020
- International Society of Hypertension. A statement from the International Society of Hypertension on COVID-19. https://ish-world.com/news/a/A-statement-from-the-International-Society-of-Hypertension-on-COVID-19. Accessed March 17, 2020
- American College of Physicians. Coronavirus Disease 2019 (COVID-19): Information for internists. https://www.acponline.org/clinical-information/clinical-resources-products/coronavirus-disease-2019-covid-19-information-for-internists. Accessed April 2, 2020
- Urgent communique of the seh-lelha (Spanish society of hypertension-Spanish league for the fight against arterial hypertension) on the management of the hypertensive patient in treatment with drugs that block the renina-angiotensin-aldos-aldos system. https://www.seh-lelha.org/covid-19. Accessed March 17, 2020
- Bozkurt B, Kovacs R, Harrington B. HFSA/ACC/AHA statement addresses concerns re: using RAAS antagonists in COVID-19. Available at: https://www.acc.org/latest-in-cardiology/articles/2020/03/17/08/59/hfsa-acc-aha-statement-addresses-concerns-re-using-raas-antagonists-in-covid-19. Accessed March 17, 2020
- Heart Failure Society of America. Patients taking ACE-i and ARBs who contract COVID-19 should continue treatment, unless otherwise advised by their physician. https://www.hfsa.org/patients-taking-ace-i-and-arbs-who-contract-covid-19-should-continue-treatment-unless-otherwise-advised-by-their-physician. Accessed March 17, 2020
- COVID -19 Clinical Guidance for the Cardiovascular Team (American College of Cardiology). https://www.acc.org//~/media/Non-Clinical/Files-PDFs-Excel-MS-Word-etc/2020/02/S20028-ACC-Clinical-Bulletin-Coronavirus.pdf. Accessed March 11, 2020
- European Renal Association- European Dialysis and Transplant Associationhttps://www.era-edta.org/en/covid-19-news-and-information. Accessed March 25, 2020
- American Society of Paediatric nephrology. https://www.healio.com/nephrology/infection-control/news/online/%7Bfc4f7dd1-4fe7-49f1-bf6a-01c68ff5f8ac%7D/american-society-of-nephrology-cdc-offer-updated-coronavirus-guidelines. Accessed March 12, 2020
- High Blood Pressure Research Council of Australia. Statement on COVID-19 and blood pressure medication. https://www.hbprca.com.au/statement-on-covid-19. Accessed March 18, 2020
- Altered lipid metabolism in recovered SARS patients twelve years after infection. Sci Rep. 2017;7(01):9110.
- [Google Scholar]
- Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents 2020 [Epub ahead of print]
- [CrossRef] [Google Scholar]
- American College of Cardiology. Ventricular Arrhythmia Risk Due to Hydroxychloroquine-Azithromycin Treatment For COVID-19. Available at: https://www.acc.org/latest-in-cardiology/articles/2020/03/27/14/00/. Accessed March 29, 2020
- Considerations for cardiac catheterization laboratory procedures during the COVID-19 pandemic. Cath Cardiovasc Interv 2020 [Epub ahead of print]
- [CrossRef] [Google Scholar]






