Translate this page into:
Mass in Right Pulmonary Artery—Case Report
Ravi Kiran Muddada, DM Student Department of Cardiology Nizam's Institute of Medical Sciences, Punjagutta, Hyderabad, TS 500082 India ravikiran927@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
The authors present a case of mass in the right pulmoary artery in a 60-year-old female patient who had dyspnea on exertion for 1 month before admission. Two-dimensional echocardiography and computed tomography pulmonary angiogram revealed mass in the right pulmonary artery. There was no evidence of deep venous thrombosis. Though the final diagnosis was not made, the authors present this case mainly for identifying and differentiating pulmonary artery thrombosis from chronic thromboembolic pulmonary hypertension and tumor.
Keywords
deep venous thrombosis
pulmonary artery hypertension
pulmonary embolism
Introduction
Pulmonary embolism (PE) and deep venous thrombosis (DVT) are both considered manifestations of the same disease of venous thromboembolism. Virchow postulated that dysfunction of vessel walls, alternations in blood flow, and hypercoagulability of the blood triggered inappropriate thrombus formation.1 DVT most commonly occurs as local clot formation in the deep calf veins. PE arises when clots break off from a peripheral DVT and become lodged within the pulmonary arterial vasculature. PE is routinely diagnosed when filling defects are found in the pulmonary arteries on CTPA. Among the general population of patients presenting to emergency rooms, absence of DVT may occur in up to 57% of those diagnosed with PE.2 A high prevalence of isolated PE may suggest localized thrombus formation in the pulmonary arteries instead of embolization from peripheral clots. In situ thrombosis is not differentiated from emboli on CTPA. However, despite evidence for multiple possible origins for clots within the pulmonary arteries, PE is the default diagnosis for filling defects detected by CTPA in clinical practice.3 Here, we present a case of localized mass within the right pulmonary artery without any evidence of DVT whose pathology is not known.
Case Details
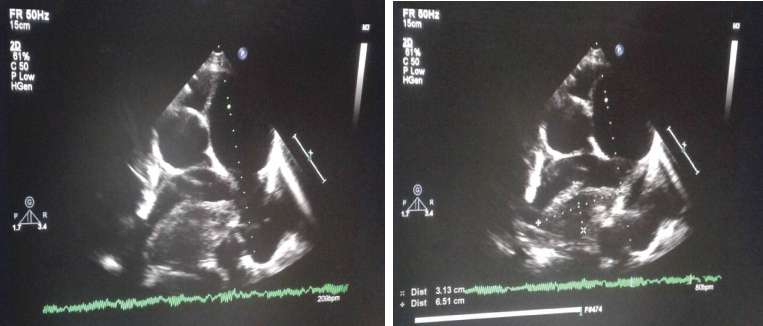
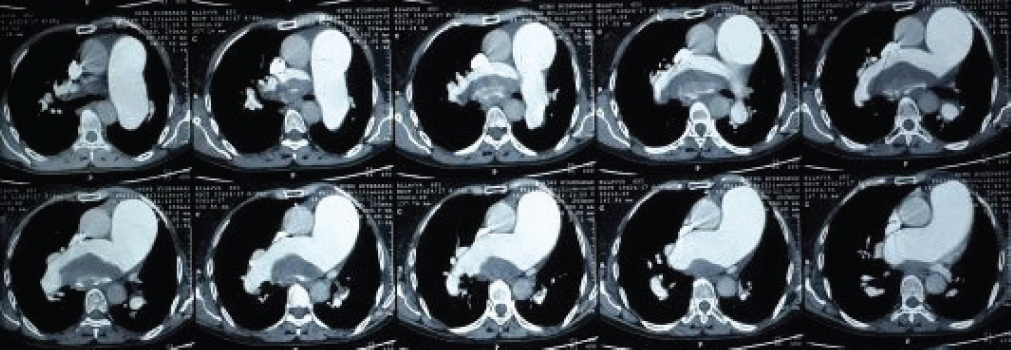
A 60-year-old woman came with complaints of shortness of breath on exertion for the past 1 month. There was no history of chest pain, palpitations, syncope, and hemoptysis. She has no history of hypertension and diabetes mellitus. At admission her pulse rate was 74 beats/min and blood pressure was 170/90 mm Hg. General and systemic examinations were normal except for loud pulmonary component of second heart sound. Hemoglobin was 10.4 g/dL, total leukocyte count (TLC) was 7,500 cells/mm3, platelet count was 1.8 lakhs/mm3, blood urea was 40 mg/dL, serum creatinine was 1 mg/dL, Na+ was 139 mmol/L, K+ was 4.6 mmol/L, and erythrocyte sedimentation rate (ESR) was 5 mm. Electrocardiogram (ECG) showed incomplete right bundle branch block (RBBB). Two-dimensional (2D) echocardiography showed no regional wall motion abnormality and good biventri cular function, dilated main pulmonary artery (MPA), right and left pulmonary arteries (RPA and LPA), large mass in RPA of size 6.5 × 3.1 cm (Fig. 1), mild tricuspid regurgitation, and severe pulmonary artery hypertension (PAH). Bilateral lower limb venous Doppler showed no evidence of DVT. Computed tomography pulmonary angiogram (CTPA) showed dilated MPA, RPA, and LPA with mass in RPA extending into proximal part of its descending branch (Fig. 2). There was no external impression noted at the origin of the ostia of the left coronary artery, mild narrowing noted of the ostium of left coronary artery. Coronary angiogram and right-sided heart catheterization showed mild narrowing of the ostium of the left main coronary artery and severe PAH. Considering her age, still the possibility of a tumor could not be ruled out and cardiac magnetic resonance imaging (MRI) was advised. The patient was lost to follow-up.
-
Fig. 1 Parasternal short-axis view showing mass in the RPA.
Fig. 1 Parasternal short-axis view showing mass in the RPA.
-
Fig. 2 CTPA showing mass in the RPA.
Fig. 2 CTPA showing mass in the RPA.
Discussion
Although pulmonary artery tumors are rare, they can be misdiagnosed as pulmonary embolism (PE) because of their similar clinical and radiologic features. The diagnosis is often delayed and it is difficult to avoid misdiagnosis. Because pulmonary artery tumor grows gradually, it usually has a long asymptomatic course and insidious onset of symptoms of pulmonary arterial obstruction. Pulmonary artery tumor is frequently confused with PE.
However, this case has severe PAH, but the cause of PAH is not known. In situ thrombosis of the peripheral pulmonary arterioles is occasionally encountered in primary pulmonary hypertension (PPH) and is likely due to endothelial cell injury creating a procoagulant environment.4 Development of large thrombi in the MPA, RPA, or LPA, however, is extremely rare in PPH. PPH causes a relatively uniform involvement of small muscular pulmonary arteries that manifests as loss of normal gravity-dependent attenuation gradient.5 This is in contrast to the patchy embolic occlusion of larger generation pulmonary arteries seen in chronic thromboembolic pulmonary arterial hypertension (CTEPH), which is responsible for the conspicuous mosaic pattern of lung attenuation.6 Other findings described in CTEPH include abrupt truncation or narrowing of the pulmonary arteries, webs, disparity in size of the segmental arteries, pulmonary infarcts, and bronchial collateral vessels.
First of all, this case had a low risk of developing deep vein thromboembolism, and there was no sign of unilateral swelling of the leg. Because deep venous thrombosis (DVT) is the major contributing factor of developing PE, the clinical probability of PE was low in this patient.
Second, this patient had different echocardiographic patterns. Her echocardiographic examination showed a bulging mass lesion impacted in the RPA, which was different from linear mass lesions usually shown in acute PE. When thrombi are visualized in the MPA in patients with acute PE, they are usually located in its distal part near the bifurcation. They extend to right and/or left pulmonary artery in many cases.7 8 The involvement of the pulmonary valves and the attachment to the right ventricular outflow tract (RVOT) were other differential findings suggesting a malignant mass with infiltration. Because transthoracic echocardiogram (TTE) has no harmful effect, the short-term follow-up echocardiographic examination can be an attractive method for the differential diagnosis.
Third, the computed tomography (CT) of the chest demonstrated an intraluminal filling defect occupying the entire lumen of the RPA. According to several studies on the role of CT in differentiating these two disease categories, the characteristics of CT findings that favor the diagnosis of pulmonary artery tumors rather than of PE include a low-attenuation filling defect, heterogeneous enhancement of mass occupying the entire luminal diameter of the main or the proximal pulmonary artery, and extravascular spread of the lesion.9
Fourth, pulmonary infarcts can occur in patients with PE. Complete absence of those infarcts with such a large thrombus is unlikely in PE. This is in favor the tumor, even though tumor embolization is known to occur. If this PAH was caused by chronic pulmonary thromboembolism, massive or submassive emboli, involving other branches of the pulmonary artery, were expected, which was not the condition in this case.
In conclusion, though the final diagnosis was not made in this case, it is crucial to identifying and differentiating in situ pulmonary artery thrombosis from CTEPH, as this requires a different therapeutic approach, and physicians should con sider the possibility of pulmonary artery tumor as a differential diagnosis of PE, especially in patients with low or intermediate probability of PE. The echocardiographic features, including proximal location of mass in the MPA, involvement of pulmonary valves, and no significant change in the short-term follow-up echocardiography, can give additional information in the differential diagnosis.
References
- The surgeon general's call to action to prevent deep vein thrombosis and pulmonary embolism. [cited February 15, 2014]
- [Publisher] [Google Scholar]
- 64-Multidetector-row spiral CT in pulmonary embolism with emphasis on incidental findings. Clin Imaging. 2008;32(05):335-341.
- [Google Scholar]
- Christopher Study Investigators. Effectiveness of managing suspected pulmonary embolism using an algorithm combining clinical probability, D-dimer testing, and computed tomographyJAMA. 2006;295(02):172-179.
- [Google Scholar]
- Primary pulmonary hypertension: a vascular biology and translational research “Work in progress”. Circulation. 2000;102(22):2781-2791.
- [Google Scholar]
- Density gradient of the lung parenchyma at computed tomographic scanning in patients with pulmonary hypertension and systemic sclerosis. Acad Radiol. 1996;3(09):724-730.
- [Google Scholar]
- Small-vessel diseases of the lung: CT-pathologic correlates. Radiology. 2002;225(03):639-653.
- [Google Scholar]
- Detection of central pulmonary artery thromboemboli by transesophageal echocardiography in patients with severe pulmonary embolism. J Am Soc Echocardiogr. 1992;5(05):515-524.
- [Google Scholar]
- Anatomic distribution of pulmonary emboli at pulmonary angiography: implications for cross-sectional imaging. Radiology. 1996;199(01):31-35.
- [Google Scholar]
- Computed tomography in pulmonary artery sarcoma: distinguishing features from pulmonary embolic disease. J Comput Assist Tomogr. 2004;28(01):34-39.
- [Google Scholar]







