Translate this page into:
Infective Endocarditis Presenting as Endogenous Endophthalmitis and Multiple Cerebral Infarcts
*Corresponding author: Mansoor C. Abdulla, Department of General Medicine, Sultan Qaboos Hospital, Salalah, Oman. drcamans@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Abdulla MC. Infective Endocarditis Presenting as Endogenous Endophthalmitis and Multiple Cerebral Infarcts. Indian J Cardiovasc Dis Women. 2024;9:109-11. doi: 10.25259/IJCDW_4_2024
Abstract
A 60-year-old housewife as admitted with fever, pain and redness in her right eye for 2 days. She had right eye redness with haziness of the cornea, white fibrinous material in the anterior chamber, and vitreous in the posterior segment. She was evaluated and found to have Endogenous Endophthalmitis (EE) with multiple cerebral infarcts due to methicillin-sensitive coagulase-negative Staphylococcus endocarditis. The patient received intravitreal injections of vancomycin and ceftazidime. She received cefazolin 2 g thrice daily intravenously. The plan of vitrectomy was suggested as per the advice from the ophthalmologist but the relatives opted for conservative management. The patient went into multiorgan failure with disseminated intravascular coagulation and despite all efforts, she succumbed to her illness. Our patient had two extracardiac manifestations of IE together. The presence of any of these manifestations should raise suspicion of infective endocarditis (IE). We report a case of native mitral valve methicillin-sensitive coagulase-negative Staphylococcus endocarditis presenting with extracardiac manifestations. Our case reminds readers to be aware of endocarditis when evaluating patients with extracardiac manifestations like EE.
Keywords
Infective endocarditis
Endogenous endophthalmitis
Cerebral infarcts
INTRODUCTION
Infective endocarditis (IE) remains a major clinical problem, with high mortality rates due to the potential complications. Endophthalmitis is usually caused by ocular surgery or penetrating trauma. Endogenous endophthalmitis (EE) is due to the hematogenous spread of bacteria from a remote primary source. IE can present a wide range of manifestations and prompt recognition is essential for proper management and minimizing mortality. We present a case of IE presenting with EE and multiple cerebral infarcts.
CASE REPORT
A 60-year-old housewife was admitted with fever, pain, and redness in her right eye for 2 days. She had right lower limb pain with pustules over it 3 days before the onset of fever and eye pain. On the day of admission, she had two episodes of generalized tonic-clonic seizures. She had diabetes mellitus, hypertension, and diabetic nephropathy in the past. She had no sick contacts and had no history of addictions. On examination, she had a high-grade fever of 100° F, tachycardia, tachypnea, and normal blood pressure, and was maintaining oxygen saturation with room air. She had right eye redness with the haziness of the cornea [Figure 1a], white fibrinous material in the anterior chamber, and vitreous in the posterior segment. The right lower limb was swollen with a local rise of temperature, and tenderness, and had few pustules. She was fully conscious and oriented, was moving all four limbs, had bilateral extensor plantar response, and exaggerated deep tendon reflexes. The rest of the systemic examination was unremarkable.
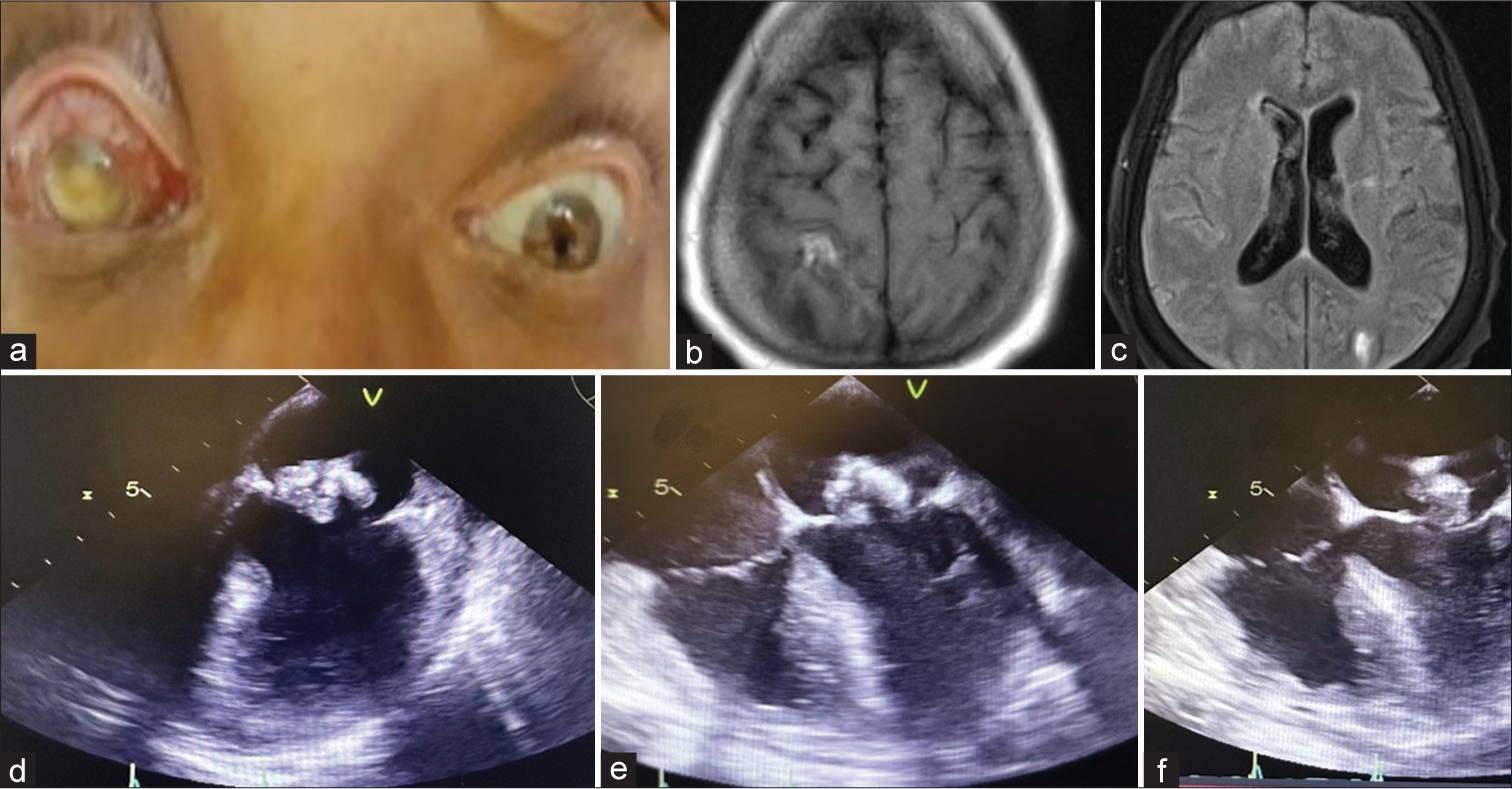
- (a) Right eye clinical photograph showing endophthalmitis, (b and c) Magnetic resonance imaging of the brain showing hyperintense areas in the right frontoparietal and left occipital regions in the fluid attenuated inversion recovery images. (d-f) Transesophageal echocardiogram showing vegetation over the mitral leaflet.
Hemoglobin was 12.7g/dL, total white blood cell count 20,500/μL with predominant neutrophils, platelet count 2.5 × 109/L, and C-reactive protein was 298 mg/L (normal range 0–5 mg/L). Urinalysis showed 2+ albuminuria, three leukocytes/high power field, five red blood cells, and no casts. Her creatinine was 4.4 mg/dL (reference 0.8 – 1.0 mg/dL), sodium 131 mmoL/l, and potassium 4.3 mmoL/l. The rest of the biochemical parameters were normal. Chest X-ray and electrocardiogram were normal. Ultrasonography abdomen was normal. Magnetic resonance imaging of the brain showed hyperintense areas in the right frontoparietal and left occipital regions in the T2-weighted and fluid-attenuated inversion recovery images with diffusion restriction suggesting infarcts [Figures 1b and c). The presence of EE, with multiple cerebral infarcts and bacteremia, suggested endocarditis. The transesophageal echocardiogram showed vegetation over the mitral leaflet with moderate mitral regurgitation [Figures 1d-f]. Cultures from the right eye’s blood, pus, and aqueous humor showed growth of methicillin-sensitive coagulase-negative Staphylococcus. The patient received intravitreal injections of vancomycin and ceftazidime. She received cefazolin 2 g thrice daily intravenously. The plan of vitrectomy was suggested as per the advice from the ophthalmologist, but the relatives opted for conservative management. The patient went into multiorgan failure with disseminated intravascular coagulation and despite all efforts, she succumbed to her illness.
DISCUSSION
Ocular manifestations of IE include Roth spots, conjunctival hemorrhages, chorioretinitis endophthalmitis, and Litten spots.[1] EE is a rare ocular manifestation of IE with high mortality rates that usually result in vision-threatening sequelae.[2] EE is caused by the metastatic spread of the infectious process from an extraocular site or following intravenous administration of a contaminated solution.[2] EE accounts for only 5–7% of endophthalmitis cases and has a high mortality rate of up to 29% with poor visual acuity outcomes.[3] EE is usually seen in patients with diabetes or cardiac diseases and malignancy.[4] IE is considered to be the most common primary site of infection leading to EE after meningitis. Patients with EE should undergo transesophageal echo to look for IE. Neurologic complications of IE include hemorrhagic and ischemic infarcts, microhemorrhages, mycotic aneurysms, infectious arteriopathy, meningitis, brain and spinal abscesses, and vertebral osteomyelitis.[5]
Our patient had two extracardiac manifestations of IE together. The presence of any of these manifestations should raise suspicion of IE. We report a case of native mitral valve methicillin-sensitive coagulase-negative Staphylococcus endocarditis presenting with extracardiac manifestations. This case highlights the importance of maintaining a high index of suspicion for IE in patients presenting with EE. Patients presenting with EE should undergo a transthoracic or transesophageal echocardiogram to look for IE.
CONCLUSION
Our patient had two extracardiac manifestations of IE together. The presence of any of these manifestations should raise suspicion of IE. We report a case of native mitral valve methicillin-sensitive coagulase-negative staphylococcus endocarditis presenting with extracardiac manifestations. Our case reminds readers to be aware of endocarditis when evaluating patients with extracardiac manifestations like EE.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Classical Eye Signs in Bacterial Endocarditis. QJM Int J Med. 2015;108:909-10.
- [CrossRef] [PubMed] [Google Scholar]
- More than Meets the Eye: Infective Endocarditis Presenting as Endogenous Endophthalmitis. Cureus. 2021;13:e14745.
- [CrossRef] [Google Scholar]
- Culture-proven Endogenous Endophthalmitis: Clinical Features and Visual Acuity Outcomes. Am J Ophthalmol. 2004;137:725-31.
- [CrossRef] [PubMed] [Google Scholar]
- Endogenous Bacterial Endophthalmitis. Report of a Ten-year Retrospective Study. Ophthalmology. 1994;101:832-8.
- [CrossRef] [PubMed] [Google Scholar]
- Neurologic Complications in Infective Endocarditis: Identification, Management, and Impact on Cardiac Surgery. Neurohospitalist. 2014;4:213-22.
- [CrossRef] [PubMed] [Google Scholar]







