Translate this page into:
Corynebacterium diphtheriae - Uncustomary Avatar in a Patient with Prosthetic Valves at an Unusual Age
*Corresponding author: Poongodi Santhana Kumarasamy, Department of Microbiology, Tirunelveli Medical College, Tirunelveli, Tamil Nadu, India. kodi68@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Santhana Kumarasamy P, Meena Kumari P, Jeyaraman A, Shanmugavelu M. Corynebacterium diphtheriae - Uncustomary Avatar in a Patient with Prosthetic Valves at an Unusual Age. Indian J Cardiovasc Dis Women. doi: 10.25259/ IJCDW_71_2024
Abstract
Corynebacterium diphtheriae is considered a re-emerging pathogen worldwide. There is a shift in the age in the incidence of diphtheria from children to adolescents and adults reported in India. The majority of the patients with C. diphtheriae endocarditis have prosthetic valves and present clinically as an acute fever, septic arthritis, and pharyngitis. In this background, here, we present a case of septic arthritis associated with bacteremia in an adult female with double-valve prosthetic replacement.
Keywords
Adult
Corynebacterium diphtheria
Infective endocarditis
Septic arthritis
INTRODUCTION
Although diphtheria has been sometimes overlooked, cases have been documented worldwide within the last several years. In 2015, India reported 2,365 cases of diphtheria which was higher than any other country.[1] Non-toxigenic and toxigenic strains may be present in the nasopharynx, skin, and other sites as asymptomatic carriers.[2] Similar to toxigenic variants, non-toxigenic Corynebacterium diphtheriae can cause infection in susceptible individuals with comorbid conditions. Furthermore, non-toxigenic variants can become toxigenic by bacteriophage-mediated lysogenesis. Together, the potential of non-toxigenic strains to obtain the tox gene exposes susceptible populations at risk for a diphtheria epidemic.[3] The majority of the patients with C. diphtheriae endocarditis have prosthetic valves, underlying heart conditions, or a history of intravenous drug use. Similar to Staphylococcus aureus, C. diphtheriae endocarditis presents as an aggressive and destructive illness with a high prevalence of complications, particularly in patients with underlying prosthetic valves.[4] The morphology of toxigenic and non-toxigenic strains is indistinct. Non-toxigenic variants are associated with less disease burden in terms of clinical severity and respiratory and disseminated infection. However, endocarditis, osteomyelitis, and septic arthritis may occur after an infection with non-toxigenic C. diphtheriae.[3] In this background, here, we present a case of septic arthritis associated with bacteremia in an adult female with double-valve prosthetic replacement.
CASE REPORT
We reported the case of a 49-year-old female with rheumatic heart disease involving the mitral valve and aortic valve prolapse and chronic atrial fibrillation. She had fever with chills on and off, giddiness, palpitation, easy fatigability, dyspnea, and swelling over the left knee joint for 3 days. She had a history of a left posterior cruciate ligament avulsion fracture 7 months back, fixed with an external cast. She underwent double-valve replacement 12 years back. On examination, she was afebrile with a pulse rate of 120/min, irregularly irregular with varying volume, a respiratory rate of 28/min, and blood pressure of 110/80 mmHg; SpO2 was 100%, her throat appeared normal, and cardiovascular examination revealed S1 and S2 sounds, though S1 was variable, while respiratory system assessment indicated normal vesicular breath sounds without any added sounds. The abdomen was soft and no organomegaly was noted.
Laboratory investigations included hemoglobin - 11.7 g% and platelet count - 80,000 lakhs/cumm, and thyroid function test was normal. Echocardiography showed post-aortic and mitral valve replacement with a dilated left atrium and ventricle, moderately severe left ventricular dysfunction, atrial fibrillation, global dyskinesia, aortic prosthetic valve dysfunction, normally functioning mitral valve, no paravalvular leak, and no tricuspid valve regurgitation.
Left knee lateral arthrotomy was done on the next day of admission under spinal anesthesia, and 100 mL pus was aspirated [Figure 1]. Direct Gram stain showed Gram-positive bacilli [Figure 2]. C. diphtheriae was isolated [Figure 3], which was sensitive to ciprofloxacin, erythromycin, clindamycin, linezolid, meropenem, and rifampin and resistant to penicillin, tetracycline, cefotaxime, and trimethoprim/sulfamethoxazole. BacT/Alert 3D system aerobic blood culture showed C. diphtheriae with the same sensitivity pattern. Bacterial identification by Matrix-assisted laser desorption/ionization- Time of flight (MALDI-TOF) was done with a score value of 1.95.

- Pus from the left knee joint.
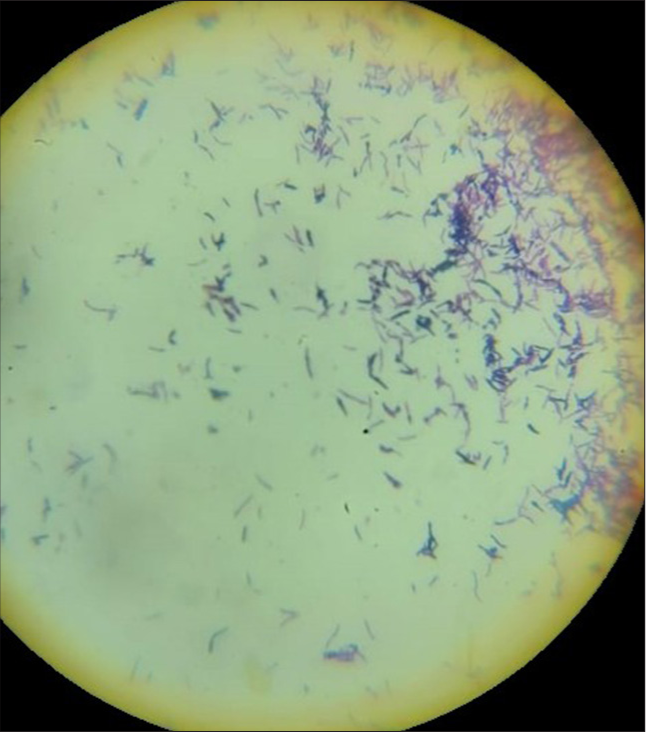
- Gram stain showing Gram-positive bacilli. 100× Oil immersion

- Culture plate showing Corynebacterium diphtheriae colony. Nutrient agar plate showing Corynebacterium diphtheria colonies
She was on T. warfarin 7 mg, T. digoxin 0.25 mg, T. Aldactone 25 mg, T. amiodarone, T. esomeprazole, Inj. ceftriaxone, and Inj. linezolid. She developed septic shock with acute renal failure after 2 days. Then, she was given Inj. piperacillin + tazobactam and Inj. vancomycin. Growth on the pus and blood culture were identified only after the 6th day of admission. The patient’s condition deteriorated despite appropriate higher antibiotics. The patient succumbed before the institution of the antidiphtheritic serum.
DISCUSSION
At present, C. diphtheriae is not only considered a re-emerging pathogen but also remains one of the most significant pathogens worldwide. Originally, it was considered a disease of children; now, there is a shift in the age in the incidence of diphtheria from children to adolescents and adults reported in India.[5]
Atypical presentation can occur with non-toxigenic strain. The pathogenesis of infection due to non-toxigenic C. diphtheriae is inconclusive and needs further studies. They can invade the tissue, cause fulminant infection, and appear to have a predilection for cardiac valvular endothelium and synovium.[6] Studies reported that 80% of endocarditis is due to non-toxigenic C. diphtheriae, and typically, previous valvular heart disease is an important risk factor, which is reported in 42–80% of cases, and left-sided endocarditis is more common. Non-toxigenic C. diphtheriae endocarditis presents clinically as an acute fever, septic arthritis, and pharyngitis.[7] Endocarditis without vegetations, though rare, can be diagnosed based on the modified Duke’s criteria.[8] Joint involvement and bacteremia due to C. diphtheriae were also reported.[6] Aspirated pus from joint and blood culture revealed C. diphtheriae in this case. The toxigenicity of the strain can be tested in vitro by Elek’s gel precipitation test, which requires quality control of reagents and a standardized procedure, hence performed only in reference laboratory. Polymerase chain reaction can be performed to demonstrate a subunit of diphtheria toxin, but does not necessarily indicate the toxin production.[9] A non-toxigenic toxin-gene bearing (NTTB) C. diphtheriae has been reported in many literatures. These NTTB strains produce challenges in public health management since it is unpredictable when they will revert to full toxicity.[10] The toxigenicity test or tox gene demonstration was not performed in this isolate.
Besides toxins, other virulence factors such as iron transport systems and fimbrial proteins are also reported.[1] Some multifunctional proteins such as DIP0733, DIP2093, and CDCE8392-081 are involved in establishing infections in the deeper parts of the body and invasion of the host cells. Astoundingly, the gene oxyR, which codes for global oxygen regulator of C. diphtheriae, affects the adherence patterns, invasion, intracellular survival in epithelial cells, and arthritogenic potential C. diphtheriae in mice. It is clear that C. diphtheriae evades the host immune system and persists in the host cells, proliferates, and enters the blood vessels, where they can bind with the erythrocytes (hemagglutination) and spreads throughout the body via the bloodstream. Further, it has a complex cell wall, a mycolic acid layer which is equivalent to outer membrane of Gram-negative bacteria. C. diphtheriae HCO4 strains show detrimental effect without being toxigenic and induce necrosis and apoptosis of host cells.[11]
Immunization with diphtheria, pertussis and tetanus vaccine (DPT) does not offer protection against the nontoxigenic strain of C. diphtheriae. Further, it does not prevent the carriage of C. diphtheriae, regardless of toxin production.[12] In highly immunized populations, toxigenic strains virtually disappear, although non-toxigenic strains may continue circulating. Antitoxin is only effective before the toxin reaches the cell; hence, it must be given as soon as possible.[13] The dose of antitoxin is calculated based on the site and severity of infection.[9] Numerous studies have revealed that the protective antibody levels against diphtheria have declined due to aging since the last vaccination, with the antibodies having an estimated half-life of 11 years.[1] Hence, Td is recommended during pregnancy and once in 10 years.[5]
Since the patient did not develop any membrane in her throat, C. diphtheriae was not anticipated and antidiphtheritic serum was not given. Atypical presentation due to C. diphtheriae should be suspected, especially in patients with prosthetic valves. In addition, it is becoming more common to find C. diphtheriae strains that are resistant to antibiotics. Fortunately, the isolates from the pus and blood in this patient were sensitive to most of the routinely used antibiotics. Antibiotic therapy kills the organisms, thus preventing further toxin production, slowing the spread of local infection, and reducing the transmission.[9]
Limitation
The toxigenicity of the isolate was not demonstrated.
CONCLUSION
Unusual presentation due to C. diphtheriae, particularly in patients with prosthetic valves, should be kept in mind and antidiphtheritic serum should be given as early as possible if it is a toxigenic strain. Infection can also occur in previously immunized patients. Despite continued global efforts and stable vaccination coverage, diphtheria is not eradicated and remains a problem today. Awareness among clinicians and microbiologists should be increased, and appropriate specimens should be collected, especially in patients with atypical presentation with prosthetic valves.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Pathogenesis of Corynebacterium diphtheriae and Available Vaccines: An Overview. Glob J Infect Dis Clin Res. 2017;3:20-4.
- [Google Scholar]
- Cutaneous Diphtheria in a German Man with Travel History. Acta Derm Venereol. 2012;92:179-80.
- [CrossRef] [PubMed] [Google Scholar]
- Cardiac Arrest Associated with Non-Toxigenic Corynebacterium diphtheria Strain: A Case Report. Front Med (Lausanne). 2023;9:1003193.
- [CrossRef] [PubMed] [Google Scholar]
- Corynebacterium diphtheriae Endocarditis: A Case Series and Review of the Treatment Approach. Int J Infect Dis. 2011;15:e584-8.
- [CrossRef] [PubMed] [Google Scholar]
- The First Case of Septicemia Due to Nontoxigenic Corynebacterium diphtheriae in Poland: Case Report. Ann Clin Microbiol Antimicrob. 2005;4:8.
- [CrossRef] [PubMed] [Google Scholar]
- Nontoxigenic Corynebacterium diphtheriae Endocarditis with Cardiogenic Shock and Severe Congestive Heart Failure. J Infect Dis Antimicrob Agents. 2015;32:135-9.
- [Google Scholar]
- Corynebacterium striatum Cardiac Device-Related Endocarditis: A Case Report. IDCases. 2022;27:e01371.
- [CrossRef] [PubMed] [Google Scholar]
- Household Transmission of NonToxigenic Diphtheria Toxin Gene-Bearing Corynebacterium diphtheriae Following a Cluster of Cutaneous Cases in a Specialist Outpatient Setting. J Med Microbiol. 2023;72:1-11.
- [CrossRef] [PubMed] [Google Scholar]
- Interactions between the Re-Emerging Pathogen Corynebacterium diphtheriae and Host Cells. Int J Mol Sci. 2022;23:3298.
- [CrossRef] [PubMed] [Google Scholar]
- Oregon Health Authority. Public Health Division. 2024. Acute and Communicable Disease Prevention. Available from: https://www.healthoregon.org/labtests [Last accessed on 2024 Oct 09]
- [Google Scholar]
- Immunobiology of Diphtheria. Recent Approaches for the Prevention, Diagnosis, and Treatment of Disease. Biotechnol Acta. 2013;6:43-62.
- [CrossRef] [Google Scholar]








